Abstract
Background and objective
Despite the ongoing intense debate on the definition of airflow limitation by spirometry in the elderly population, there have only been few studies comparing the fixed ratio and the Z-score of forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) in terms of long-term mortalities. In this study, we aimed to identify the proper method for accurately defining the airflow limitation in terms of long-term mortality prediction in the elderly population.
Methods
Data were collected from the Third National Health and Nutrition Examination Survey in the US. Non-Hispanic Caucasians aged 65–80 years were included. The receiver operating characteristic (ROC) curves of both methods were plotted and compared for 10-year all-cause, respiratory, and COPD mortalities.
Results
Of 1,331 subjects, the mean age was 71.7 years and 805 (60.5%) were males. For the 10-year all-cause mortality, the area under the curve (AUC) of the fixed ratio was significantly greater than that of the Z-score of FEV1/FVC, but both showed poor prediction performance (0.633 vs 0.616, p<0.001). For the 10-year respiratory and COPD mortalities, both the fixed ratio and the Z-score of FEV1/FVC showed comparable prediction performance with greater AUCs (0.784 vs 0.778, p=0.160, and 0.896 vs 0.896, p=0.971, respectively). Interestingly, the conventional cutoff of 0.7 in the fixed ratio was consistently higher than the optimal for the 10-year all-cause, respiratory, and COPD mortalities (0.70 vs 0.69, 0.62, and 0.61, respectively), whereas that of −1.64 in the Z-score of FEV1/FVC was consistently lower than the optimal cutoff (−1.64 vs −1.31, −1.47, and −1.41, respectively).
Conclusion
In the elderly population, both the fixed ratio and the Z-score of FEV1/FVC showed comparable prediction performance for the 10-year respiratory and COPD mortalities. However, the conventional cutoff of neither 0.70 in the fixed ratio nor −1.64 in the Z-score of FEV1/FVC was optimal for predicting the long-term mortalities.
Introduction
COPD is a major cause of morbidity and mortality worldwide, and the socioeconomic burden of the disease is rapidly increasing.Citation1–Citation3 As the airflow limitation is a distinct feature of COPD, spirometry has been widely used for its diagnosis.Citation2–Citation7 However, the proper method for defining the airflow limitation by spirometry has yet to be fully established and is under intense debate, particularly regarding the elderly population.Citation8,Citation9
For example, the fixed ratio that defines the airflow limitation as the ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) less than a fixed cutoff, such as 0.70, has been used frequently due to the simplicityCitation3,Citation10–Citation12 but has been disputed because of the possibility of overdiagnosis, especially in the elderly population.Citation5,Citation7,Citation13–Citation16 On the other hand, the Z-score or lower limit of normal of FEV1/FVC have been considered as being less influenced by the age-related issues, because it defines the pathologic state by taking into account the age-adjusted normal reference.Citation5,Citation7,Citation13–Citation16 However, this method has been criticized as well because of the complexity and the risk of underdiagnosis.Citation17,Citation18
As there is no gold standard for defining the airflow limitation particularly in the elderly population, several studies have compared the fixed ratio and the Z-score or lower limit of normal of FEV1/FVC using various clinical outcomes such as respiratory symptoms, FEV1 declines, emergency department visits, and respiratory- or COPD-related hospitalizations.Citation19–Citation22 However, there have only been a few studies comparing both methods in terms of the long-term mortality, which is the most robust and reliable outcome in clinical studies.Citation23,Citation24 Therefore, we performed a study to identify the proper method for defining the airflow limitation in terms of long-term mortalities in the elderly population. In addition, because there is a lack of evidence that the conventional cutoffs of 0.70 in the fixed ratio and −1.64 in the Z-score of FEV1/FVC are the optimal values for predicting long-term mortalities in the elderly population, we also examined the optimality of the conventional cutoffs in both methods.
Methods
Study design and population
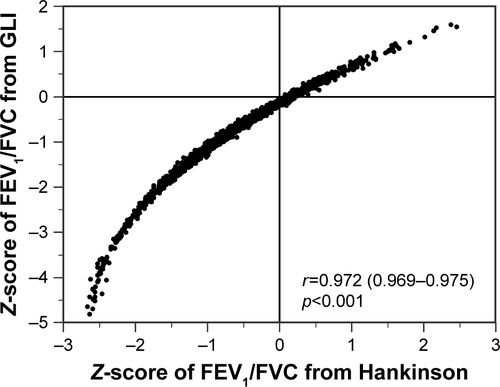
We used the data from the Third National Health and Nutrition Examination Survey in the US (US NHANES III), which were utilized in our previous study.Citation25 Briefly, non-Hispanic Caucasians (aged 17–80 years) with three or more acceptable spirometry results were included in our previous study.Citation25 Among them, subjects who were aged ≥65 years were included and those with possible restrictive disease defined as both FVC <80% of predicted value and FEV1/FVC ≥0.70 were excluded from the study ().
Figure 1 Flowchart of subject selection from the US NAHNES III.
The spirometry results and mortality status of the subjects during 10-year of follow-up were collected in addition to the demographic data including age, sex, height, smoking history, and comorbidities. The cause of death was assessed in each fatal case, and the mortality was reclassified into 10-year all-cause, respiratory, and COPD mortalities. For these outcomes, the receiver operating characteristic (ROC) curves of both the fixed ratio and the Z-score of FEV1/FVC were plotted. The preferred method was assessed by comparing the areas under the curve (AUCs) of both methods for the long-term mortalities.
The optimal cutoff that shows the highest Youden index (sensitivity + specificity − 1) was assessed in each ROC curve and compared to the conventional cutoffs – 0.70 in the fixed ratio and −1.64 in the Z-score of FEV1/FVC – as appropriate. Performance indices such as sensitivity, specificity, positive likelihood ratio (LR+), and negative likelihood ratio (LR−) were also calculated and compared at both the conventional and optimal cutoffs.
The study was approved by the institutional review board of Asan Medical Center (approval number: 2016-0198). Since the data of US NHANES III were de-identified and freely open to the public, no US institutional review board approval was required.
Spirometry results
We performed the study using the data from the US NHANES III, and the manner of the spirometry measurement used in the survey was described previously.Citation25,Citation26 Briefly, each subject attempted to perform at least five FVC maneuvers and was requested to meet the acceptability and reproducibility criteria of the American Thoracic Society (ATS). Bronchodilators were not used for the spirometry. The spirometry system had been independently tested and proved to be qualified for the spirometry equipment recommendations of the ATS.
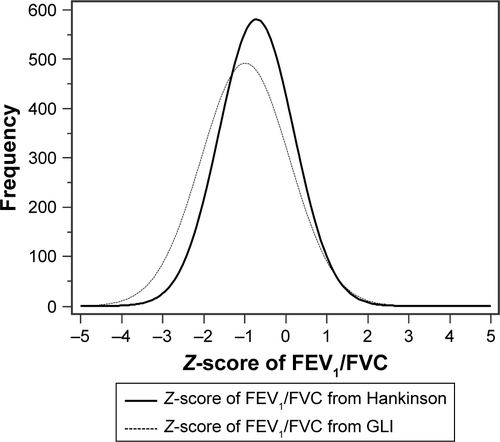
The Z-scores of spirometry values were calculated using the lambda-mu-sigma (LMS) method, by which the spirometry values of median (mu), coefficient of variation (sigma), and skewness (lambda) were modeled.Citation25,Citation27,Citation28 The reference spirometry values obtained from Hankinson were preferred in this study, since they were derived from the US NHANES III as well.Citation26 In addition, we repeated the analyses using the reference spirometry values from the Global Lung Function Initiative (GLI), which is available at the official website of GLI (http://www.ers-education.org/guidelines/global-lung-function-initiative.aspx).Citation29,Citation33
Mortality data
The US NHANES III provided mortality data based on the National Death Index, and we reclassified them into 10-year all-cause, respiratory, and COPD mortalities. Respiratory and COPD mortalities were defined using the 10th revision of the International Classification of Diseases (ICD-10) codes J10–J98 and J40–J47, respectively. The codes for asthma, J45 and J46, were included in the respiratory mortality but excluded from the COPD mortality.
Statistical analysis
Results for continuous variables were expressed as mean ± standard deviation and those for categorical variables were expressed as absolute frequency and percentage. The AUCs were expressed with 95% confidence interval, and DeLong’s method was used for the comparison. A p-value of <0.05 was considered as statistically significant. All statistical analyses were completed using SPSS version 21.0 for Windows (IBM Corporation, Armonk, NY, USA) and MedCalc, version 17.5.5 for Windows (MedCalc Software bvba, Ostend, Belgium).
Results
Subject characteristics
Among 1,331 subjects included in the study, the mean age was 71.7±4.5 years and 805 (60.5%) were males. In all, 808 (60.7%) subjects had smoking history. The mean value of FEV1/FVC was 0.68±0.10 and that of Z-score of FEV1/FVC was −0.71±0.91 (). During the 10-year follow-up, mortality from any cause occurred in 490 (36.8%) subjects, while 48 (3.6%) and 29 (2.2%) mortalities were related to the respiratory and COPD causes, respectively.
Table 1 Baseline characteristics of the subjects
Prediction performance of the fixed ratio and the Z-score of FEV1/FVC for the mortalities in the elderly population
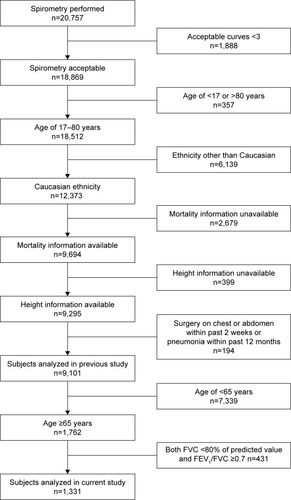
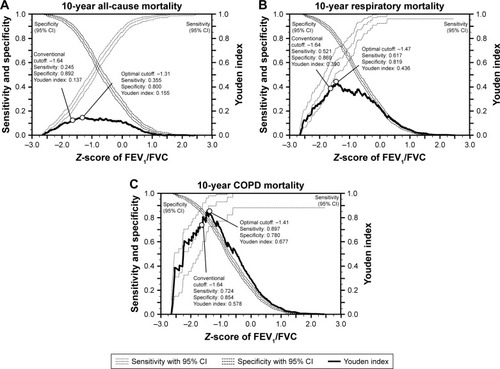
For 10-year all-cause mortality, the AUC of the fixed ratio was significantly greater than that of the Z-score of FEV1/FVC (0.633 [0.607–0.659] vs 0.616 [0.589–0.642], p<0.001, respectively; ). For 10-year respiratory and COPD mortalities, the fixed ratio and the Z-score of FEV1/FVC showed comparable prediction performance with greater AUCs (0.784 [0.761–0.806] vs 0.778 [0.755–0.800], p=0.160, for 10-year respiratory mortality and 0.896 [0.878–0.912] vs 0.896 [0.878–0.912], p=0.971, for 10-year COPD mortality, respectively; ). In the analysis using the reference values from GLI, both the fixed ratio and the Z-score of FEV1/FVC showed similar results (0.633 [0.606–0.659] vs 0.607 [0.581–0.634], p<0.001, for 10-year all-cause mortality; 0.784 [0.761–0.806] vs 0.774 [0.751–0.796], p=0.073, for 10-year respiratory mortality; and 0.896 [0.878–0.912] vs 0.895 [0.877–0.911], p=0.844, for 10-year COPD mortality, respectively; Figure S1).
Figure 2 Comparison of the prediction performance of the fixed ratio and the Z-score of FEV1/FVC for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the elderly population.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; AUC, area under the curve.

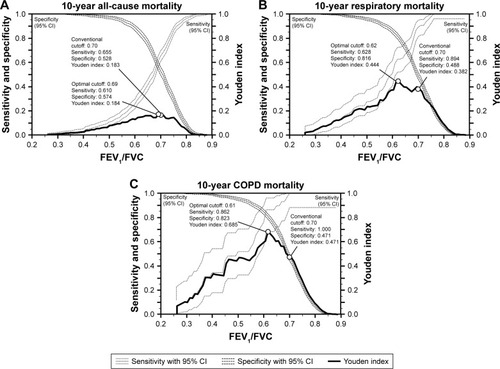
Cutoffs and performance indices of the fixed ratio for the mortalities in the elderly population
For 10-year all-cause, respiratory, and COPD mortalities, the optimal cutoffs of the fixed ratio were 0.69, 0.62, and 0.61, respectively, and the conventional cutoff of 0.70 was consistently higher than the optimal values ( and ). Interestingly, regardless of the mortalities, the sensitivity of the conventional cutoff was consistently higher than that of the optimal cutoff (0.655 vs 0.610 for 10-year all-cause mortality, 0.894 vs 0.628 for 10-year respiratory mortality, and 1.000 vs 0.862 for 10-year COPD mortality, respectively). On the other hand, the specificity of the conventional cutoff was consistently lower than that of the optimal cutoff (0.528 vs 0.574 for 10-year all-cause mortality, 0.488 vs 0.816 for 10-year respiratory mortality, and 0.471 vs 0.823 for COPD mortality, respectively; and ).
Table 2 Conventional and optimal cutoffs and the performance indices of fixed ratio for 10-year all-cause, respiratory, and COPD mortalities in the elderly population
Figure 3 Comparison of the conventional and the optimal cutoffs and the performance indices of the fixed ratio for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the elderly population.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; CI, confidence interval.
Cutoffs and performance indices of the Z-score of FEV1/FVC for the mortalities in the elderly population
For 10-year all-cause, respiratory, and COPD mortalities, the optimal cutoffs of the Z-score of FEV1/FVC were −1.31 (9th–10th percentile), −1.47 (7th–8th percentile), and −1.41 (7th–8th percentile), respectively; in contrast to the fixed ratio, the conventional cutoff of −1.64 (5th percentile) was consistently lower than the optimal values ( and ). For the performance indices, the sensitivity of the conventional cutoff was consistently lower than that of the optimal cutoffs (0.245 vs 0.355 for 10-year all-cause mortality, 0.521 vs 0.617 for 10-year respiratory mortality, and 0.724 vs 0.897 for 10-year COPD mortality, respectively). On the other hand, the specificity of the conventional cutoff was consistently higher than that of the optimal cutoff (0.892 vs 0.800 for 10-year all-cause mortality, 0.869 vs 0.819 for 10-year respiratory mortality, and 0.854 vs 0.780 for 10-year COPD mortality, respectively; and ). When the reference values from GLI were used for the analysis, the optimal cutoffs of the Z-score of FEV1/FVC for 10-year mortalities were “left shifted” and were −1.76 (3rd–4th percentile) for both 10-year all-cause and respiratory mortalities and −1.58 (5th–6th percentile) for 10-year COPD mortality (Figure S2).
Table 3 Conventional and optimal cutoffs and the performance indices of the Z-score of FEV1/FVC for 10-year all-cause, respiratory, and COPD mortalities in the elderly population
Figure 4 Comparison of the conventional and the optimal cutoffs and the performance indices of the Z-score of FEV1/FVC for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the elderly population.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; CI, confidence interval.
Subgroup analysis by sex
In male elderly population (n=805), the AUCs of the fixed ratio for 10-year all-cause and respiratory mortalities were significantly greater than those of the Z-score of FEV1/FVC (0.633 [0.599–0.667] vs 0.624 [0.589–0.657], p<0.001, for 10-year all-cause mortality and 0.794 [0.764–0.821] vs 0.786 [0.756–0.814], p<0.001, for 10-year respiratory mortality, respectively). For 10-year COPD mortality, the fixed ratio and the Z-score of FEV1/FVC showed comparable prediction performance with greater AUCs (0.898 [0.875–0.918] vs 0.895 [0.872–0.916], p=0.415). The optimal cutoffs of the fixed ratio for 10-year all-cause, respiratory, and COPD mortalities were 0.71, 0.62, and 0.61, respectively and those of the Z-score of FEV1/FVC were −0.53 (29th–30th percentile), −1.41 (7th–8th percentile), and −1.41 (7th–8th percentile), respectively (Figure S3).
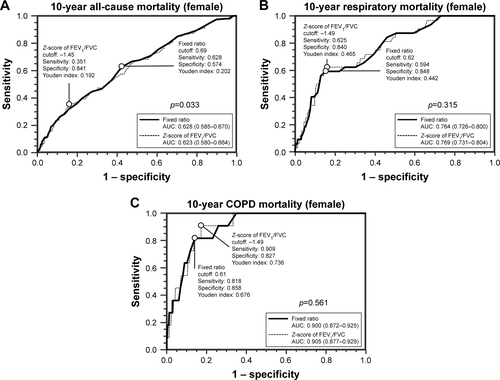
In the female elderly population (n=526), the AUC of the fixed ratio for 10-year all-cause mortality was significantly greater than that of the Z-score of FEV1/FVC (0.628 [0.585–0.670] vs 0.623 [0.580–0.664], p=0.033). For 10-year respiratory and COPD mortalities, the fixed ratio and the Z-score of FEV1/FVC showed comparable prediction performance with greater AUCs (0.764 [0.726–0.800] vs 0.769 [0.731–0.804], p=0.315, for 10-year respiratory mortality and 0.900 [0.872–0.925] vs 0.905 [0.877–0.929], p=0.561, for 10-year COPD mortality, respectively). The optimal cutoffs of the fixed ratio for 10-year all-cause, respiratory, and COPD mortalities were 0.69, 0.62, and 0.61, respectively, and those of the Z-score of FEV1/FVC were −1.45 (7th–8th percentile), −1.49 (6th–7th percentile), and −1.49 (6th–7th percentile), respectively (Figure S4).
Discussion
Although mortality is the most robust and reliable outcome of clinical studies on COPD, it has been rarely used for the comparison of the fixed ratio and the Z-score or lower limit of normal of FEV1/FVC because it requires high patient numbers and extended study duration.Citation23,Citation24 In this study, we compared the prediction performance of the fixed ratio and the Z-score of FEV1/FVC for 10-year all-cause, respiratory, and COPD mortalities, particularly in the elderly population, which is at the center of the debate on the definition of airflow limitation by spirometry. We found that both methods show comparable prediction performance for 10-year respiratory and COPD mortalities in the elderly population regardless of the reference values ( and S1B and C). These results suggest that the fixed ratio and the Z-score or lower limit of normal of FEV1/FVC can both be used to define the airflow limitation in the elderly population and can be chosen according to the physician’s preference. Considering the advantage of the simplicity of the fixed ratio, we assume that the fixed ratio might be more favored in clinical settings, which is in line with the perspective of the Global Initiative for Chronic Obstructive Lung Disease (GOLD).Citation3
On the other hand, for 10-year all-cause mortality, the fixed ratio consistently showed better prediction performance than the Z-score of FEV1/FVC in the elderly population ( and S1A). However, we believe that it needs to be interpreted with caution because the low AUCs of both methods – 0.633 in the fixed ratio and 0.616 (or 0.607 with the reference values from GLI) in the Z-score of FEV1/FVC – indicate subpar prediction performance. These might stem from the heterogeneity of all-cause mortality. Since we limited the study population to those aged between 65 and 80 years, the subjects had a substantial number of comorbidities, including hypertension, diabetes, cancer, heart attack, and heart failure, that might influence the all-cause mortality (). Therefore, there might be a substantial number of mortalities independent of the pulmonary function, and the spirometry itself might be insufficient for predicting 10-year all-cause mortality in this high-comorbid population.
We also investigated the optimality of the conventional cutoffs for predicting 10-year all-cause, respiratory, and COPD mortalities in the elderly population. Although the conventional cutoffs – 0.70 in the fixed ratio and −1.64 in the Z-score of FEV1/FVC (5th percentile in the lower limit of normal) – have been widely used in clinical studies and practices, both cutoffs were defined as arbitrary by experts.Citation16 We found that, regardless of mortalities, the conventional cutoff of 0.70 in the fixed ratio was consistently higher than the optimal cutoff with a higher sensitivity and a lower specificity ( and ). This is in line with the criticism that the fixed ratio may be prone to overdiagnosing the airflow limitation in the elderly population.Citation5,Citation7,Citation13–Citation16 On the other hand, the conventional cutoff of −1.64 in the Z-score of FEV1/FVC was consistently lower than the optimal cutoff with a lower sensitivity and a higher specificity ( and ). This also correlates well with the criticism that the Z-score or lower limit of normal of FEV1/FVC may be prone to under-diagnosing the airflow limitation in the elderly population.Citation17,Citation18 Thus, the conventional cutoffs of both the fixed ratio and the Z-score of FEV1/FVC may be biased in the elderly population and the over- and underdiagnosis of the airflow limitation might be affected by not only the innate characteristics of each method but also the biased cutoffs. However, we could not determine a single best cutoff from our study because the optimal cutoffs varied with the outcomes and because there was no consensus regarding the desirable clinical outcome for the comparison. Nevertheless, we believe that our findings are meaningful since they raise the awareness of the uncertain optimality of the conventional cutoffs.
In the analysis using the reference values from GLI, however, the optimal cutoffs of the Z-score of FEV1/FVC for 10-year mortalities were “left shifted” and those for both 10-year all-cause and respiratory mortalities were less than the current cutoff (−1.76 vs −1.64 for both mortalities; Figure S2). Considering the “left-shifted” distribution of the Z-scores of FEV1/FVC with the reference values from GLI in this elderly Caucasian population (Figures S5 and S6), we assume that the “left-shifted” optimal cutoffs might be influenced by the “left-shifted” distribution of the Z-scores. The geographic and time differences between the US NHANES III and GLI and the extreme age distribution of the subjects might contribute to these results, but we believe that the details should be investigated in further studies.
Since the study population was predominantly males, we performed the subgroup analysis by sex. Overall, the results were similar between the groups, but the optimal cutoffs of the fixed ratio and the Z-score of FEV1/FVC for 10-year all-cause mortality in male elderly population were “right shifted” with the optimal cutoffs of 0.71 in the fixed ratio and −0.53 in the Z-score of FEV1/FVC (Figure S3A). Considering that the male elderly subjects are prone to have comorbidities that might influence the mortalities, we assume that the spirometry itself might be insufficient for predicting 10-year all-cause mortality, particularly in male elderly population.
This study has several limitations. First, we evaluated the prediction performance of each method for defining the airflow limitation by spirometry using retrospectively collected mortality data. Although mortality is the most robust and reliable outcome in the clinical studies,Citation24 the retrospective data on mortality might be confounded by inherent statistical biases.Citation30,Citation31 Second, although the ICD-10 codes were used for classifying the cause of death, there might be a potential error that may have influenced the results. However, the mortality status and cause of death of the subjects of the US NHANES III have been extensively validated in previous studies;Citation18,Citation25,Citation28 therefore, we assume that the effect of potential error on the results of this study is minimal. Third, whereas post-bronchodilator spirometry is required for strict diagnostic criteria of both the fixed ratio and the Z-score of FEV1/FVC, it was not available in this general population-based survey. However, as Soriano and ManninoCitation32 indicated, the clinical significance of bronchodilator responsiveness is not universally accepted and the importance of the post-bronchodilator spirometry is being challenged. Finally, since we only included Caucasian subjects aged 65–80 years, the general application of the results to other age or ethnic groups might be limited. However, considering that the debate on defining airflow limitation by spirometry is mainly over the elderly population, we believe that the investigation limited to this age group is necessary and has a distinct significance.
Conclusion
In the elderly population, both the fixed ratio and the Z-score of FEV1/FVC showed comparable prediction performance for 10-year respiratory and COPD mortalities. These suggest that both the fixed ratio and the Z-score or lower limit of normal FEV1/FVC can be used to define the airflow limitation in the elderly population, although we assume that the convenient fixed ratio might be favored by clinicians due to its simplicity.
In addition, the conventional cutoffs – 0.70 in the fixed ratio and −1.64 in the Z-score of FEV1/FVC – seem to provide biased results in the elderly population in that they may contribute to over- and underdiagnosis of the airflow limitation, respectively. Further investigation for defining a single best cutoff for each method is required.
Acknowledgments
This study was supported by the National Health Clinical Research (NHCR) from the Ministry of Health and Welfare, Republic of Korea (HC16C2254). We thank Dr Joon Seo Lim from the Scientific Publications Team at Asan Medical Center for his editorial assistance in preparing this manuscript.
Supplementary materials
Figure S1 Comparison of the prediction performance of the fixed ratio and the Z-score of FEV1/FVC for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the elderly population using the reference values from GLI.
Note: Youden index is defined as sensitivity + specificity − 1.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; GLI, Global Lung Function Initiative; AUC, area under the curve.
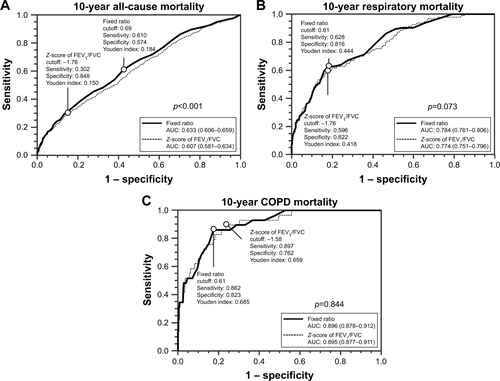
Figure S2 Comparison of the conventional and the optimal cutoffs and the performance indices of the Z-score of FEV1/FVC for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the elderly population using the reference values from GLI.
Note: Youden index is defined as sensitivity + specificity − 1.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; GLI, Global Lung Function Initiative; CI, confidence interval.
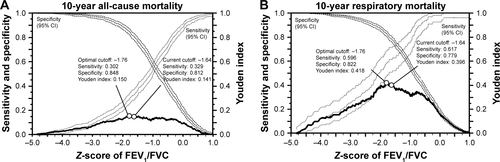
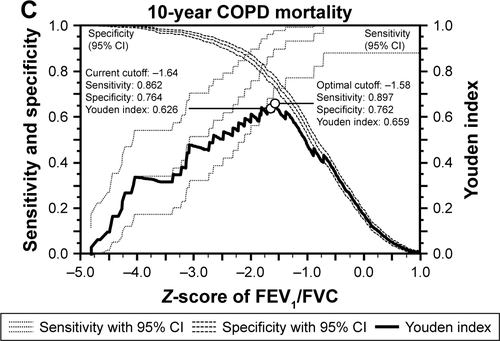
Figure S3 Comparison of the prediction performance of the fixed ratio and the Z-score of FEV1/FVC for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the male elderly population.
Note: Youden index is defined as sensitivity + specificity − 1.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; AUC, area under the curve.
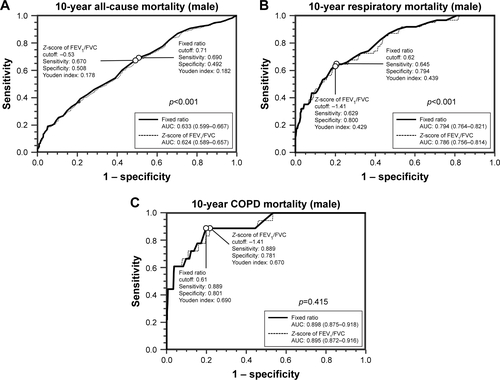
Figure S4 Comparison of the prediction performance of the fixed ratio and the Z-score of FEV1/FVC for 10-year all-cause mortality (A), 10-year respiratory mortality (B), and 10-year COPD mortality (C) in the female elderly population.
Note: Youden index is defined as sensitivity + specificity − 1.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; AUC, area under the curve.
Disclosure
The authors report no conflicts of interest in this work.
References
- PauwelsRARabeKFBurden and clinical features of chronic obstructive pulmonary disease (COPD)Lancet2004364943461362015313363
- QaseemAWiltTJWeinbergerSEDiagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory SocietyAnn Intern Med2011155317919121810710
- VogelmeierCFCrinerGJMartinezFJGlobal strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summaryAm J Respir Crit Care Med2017195555758228128970
- MillerMRHankinsonJBrusascoVStandardisation of spirometryEur Respir J200526231933816055882
- PellegrinoRViegiGBrusascoVInterpretative strategies for lung function testsEur Respir J200526594896816264058
- HoggJCPathophysiology of airflow limitation in chronic obstructive pulmonary diseaseLancet2004364943570972115325838
- BakkePSRonmarkEEaganTRecommendations for epidemiological studies on COPDEur Respir J20113861261127722130763
- EnrightPBrusascoVCounterpoint: should we abandon FEV(1)/FVC <0.70 to detect airway obstruction? YesChest2010138510401042 discussion 1042–104421051394
- CelliBRHalbertRJPoint: should we abandon FEV(1)/FVC <0.70 to detect airway obstruction? NoChest201013851037104021051393
- Chronic Obstructive Pulmonary DiseaseNational clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary careThorax200459suppl 11232
- TunksMMillerDCanadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease–2008 update–highlights for primary careCan Respir J2008154219 author reply 219
- National Clinical Guideline C. National Institute for Health and Clinical Excellence: guidanceChronic Obstructive Pulmonary Disease: Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary CareLondonRoyal College of Physicians (UK) National Clinical Guideline Centre – Acute and Chronic Conditions201022673 Available from: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0033903/Access date February 13, 2018
- SwanneyMPRuppelGEnrightPLUsing the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstructionThorax200863121046105118786983
- RobertsSDFarberMOKnoxKSFEV1/FVC ratio of 70% misclassifies patients with obstruction at the extremes of ageChest2006130120020616840402
- HardieJABuistASVollmerWMEllingsenIBakkePSMorkveORisk of over-diagnosis of COPD in asymptomatic elderly never-smokersEur Respir J20022051117112212449163
- BrusascoVSpirometric definition of COPD: exercise in futility or factual debate?Thorax201267756957022467708
- ManninoDMSonia BuistAVollmerWMChronic obstructive pulmonary disease in the older adult: what defines abnormal lung function?Thorax200762323724117090573
- ManninoDMDiaz-GuzmanEInterpreting lung function data using 80% predicted and fixed thresholds identifies patients at increased risk of mortalityChest20121411738021659434
- CerveriICorsicoAGAccordiniSUnderestimation of airflow obstruction among young adults using FEV1/FVC <70% as a fixed cut-off: a longitudinal evaluation of clinical and functional outcomesThorax200863121040104518492741
- Garcia-RioFSorianoJBMiravitllesMOverdiagnosing subjects with COPD using the 0.7 fixed ratio: correlation with a poor health-related quality of lifeChest201113951072108021183609
- GuderGBrennerSAngermannCEGOLD or lower limit of normal definition? A comparison with expert-based diagnosis of chronic obstructive pulmonary disease in a prospective cohort-studyRespir Res20121311322309369
- AkkermansRPBerrevoetsMASmeeleIJLung function decline in relation to diagnostic criteria for airflow obstruction in respiratory symptomatic subjectsBMC Pulm Med2012121222439763
- van DijkWDGuptaNTanWCBourbeauJClinical relevance of diagnosing COPD by fixed ratio or lower limit of normal: a systematic reviewCOPD201411111312023862613
- GlaabTVogelmeierCBuhlROutcome measures in chronic obstructive pulmonary disease (COPD): strengths and limitationsRespir Res2010117920565728
- LeeSWKimHKBaekSDevelopment of a spirometry T-score in the general populationInt J Chron Obstruct Pulmon Dis20161136937926966359
- HankinsonJLOdencrantzJRFedanKBSpirometric reference values from a sample of the general U.S. populationAm J Respir Crit Care Med199915911791879872837
- StanojevicSWadeAStocksJReference ranges for spirometry across all ages: a new approachAm J Respir Crit Care Med2008177325326018006882
- Vaz FragosoCAConcatoJMcAvayGThe ratio of FEV1 to FVC as a basis for establishing chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2010181544645120019341
- QuanjerPHStanojevicSColeTJMulti-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equationsEur Respir J20124061324134322743675
- SuissaSEffectiveness of inhaled corticosteroids in chronic obstructive pulmonary disease: immortal time bias in observational studiesAm J Respir Crit Care Med20031681495312663327
- SuissaSBarnesPJInhaled corticosteroids in COPD: the case againstEur Respir J2009341131619567599
- SorianoJBManninoDMReversing concepts on COPD irreversibilityEur Respir J200831469569618378779
- Global Lung Function Initiative Available from: http://www.ers-education.org/guidelines/global-lung-function-initiative.aspxAccessed February 08, 2018