Abstract
Introduction
The clinical benefit of continued supervised maintenance exercise programs following pulmonary rehabilitation in COPD remains unclear. This systematic review aimed to synthesize the available evidence on the efficacy of supervised maintenance exercise programs compared to usual care following pulmonary rehabilitation completion on health care use and mortality.
Methods
Electronic databases (MEDLINE, Embase, CINAHL, Cochrane Central Register of Controlled Trials, Web of Science, and PEDro) and trial registers (ClinicalTrials.gov and Current Controlled Trials) were searched for randomized trials comparing supervised maintenance exercise programs with usual care following pulmonary rehabilitation completion. Primary outcomes were respiratory-cause hospital admissions, exacerbations requiring treatment with antibiotics and/or systemic corticosteroids, and mortality.
Results
Eight trials (790 COPD patients) met the inclusion criteria, six providing data for meta-analysis. Continued supervised maintenance exercise compared to usual care following pulmonary rehabilitation completion significantly reduced the risk of experiencing at least one respiratory-cause hospital admission (risk ratio 0.62, 95% confidence interval [CI] 0.47–0.81, P<0.001). Meta-analyses also suggested that supervised maintenance exercise leads to a clinically important reduction in the rate of respiratory-cause hospital admissions (rate ratio 0.72, 95% CI 0.50–1.05, P=0.09), overall risk of an exacerbation (risk ratio 0.79, 95% CI 0.52–1.19, P=0.25), and mortality (risk ratio 0.57, 95% CI 0.17–1.92, P=0.37).
Conclusion
In the first systematic review of the area, current evidence demonstrates that continued supervised maintenance exercise compared to usual care following pulmonary rehabilitation reduces health care use in COPD. The variance in the quality of the evidence included in this review highlights the need for this evidence to be followed up with further high-quality randomized trials.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Pulmonary rehabilitation is defined as “a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors.”Citation1 Pulmonary rehabilitation has well-established benefits in improving exercise capacity, health-related quality life, and psychological well-being in chronic lung conditions such as COPD.Citation1,Citation2 The strength of the evidence for these benefits in COPD has led to calls for an end to randomized controlled trials comparing pulmonary rehabilitation with usual care.Citation3 However, the benefits of pulmonary rehabilitation have been shown to be short termCitation2 with the condition of most patients returning to baseline at 12 months.Citation4 Consequently, there is interest in exercise programs that may maintain the initial benefits of pulmonary rehabilitation.Citation5,Citation6
Supervised maintenance exercise programs after pulmonary rehabilitation in COPD appear to be more effective in preserving the improvements in exercise capacity up to 6 months but show no effects with respect to health-related quality of life postrehabilitation.Citation5,Citation7 Exacerbations and hospital admissions are the key events in the management of COPD, but the effects of exercise, particularly supervised maintenance programs following pulmonary rehabilitation, on these outcomes have received little attention. A recent systematic review has highlighted the role of pulmonary rehabilitation in reducing hospitalizations due to COPD exacerbations.Citation8 This supported a previous systematic review that showed a reduction in the risk of hospital readmission when completing pulmonary rehabilitation following exacerbation,Citation9 albeit the quality of this evidence has recently been downgraded due to inconsistencies in the estimates of effect.Citation10 There is increasing interest in assessing these outcomes in response to exercise interventions following pulmonary rehabilitation to identify if the duration of benefits from a pulmonary rehabilitation program alone can be prolonged or rather enhanced during the postrehabilitation period.Citation8 A previous systematic review of supervised maintenance exercise programs following pulmonary rehabilitation in COPD had included studies that reported health care use; however, data were not statistically combined to quantify effect size.Citation5 Despite the availability of new evidence in the area since this review, there remains no systematic review that has synthesized the evidence of the effects of supervised maintenance exercise training programs compared to usual care following pulmonary rehabilitation on outcomes related to health care use. Therefore, the aim of this systematic review was to collate and synthesize all of the available evidence from randomized controlled trials in order to estimate the size of the effect of supervised maintenance exercise programs following pulmonary rehabilitation on health care use.
Methods
The protocol for this study (CRD42016035509) was registered in advance on PROSPERO (International Prospective Register of Systematic Reviews; www.crd.york.ac.uk/PROSPERO/).
Selection criteria
Participants
Adults with a confirmed diagnosis of COPD (in line with national or international criteria, eg, British Thoracic Society, American Thoracic Society/European Respiratory Society, and Global Initiative for Chronic Obstructive Lung Disease) who had completed a pulmonary rehabilitation program.Citation11–Citation13
Intervention
Studies were included if patients were randomized to a supervised maintenance exercise training program following pulmonary rehabilitation.
Comparison
The comparator was any concurrent control group who had completed pulmonary rehabilitation and returned to “usual care.”
Outcomes
Primary outcomes were hospital admissions (respiratory cause), exacerbations requiring treatment with antibiotics and/or systemic corticosteroids, and all-cause mortality.
Secondary outcome measures were hospital admissions (all-cause), outpatient visits, length of hospital stay (respiratory or all-cause), and general practitioner (GP) visits.
Study design
Studies included in this review had to have adhered to the following study designs: parallel-group randomized controlled trials (allocation at individual or cluster level or using quasi-random method) or crossover randomized controlled trials (data up to point of crossover only).
Search strategy
Searches were conducted to identify any relevant completed or ongoing systematic reviews using the following sources: Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, and PROSPERO. Published trials were identified through searches on the following bibliographic databases: MEDLINE, Embase, CINAHL, Cochrane Central Register of Controlled Trials, Web of Science, and PEDro. Searches of ongoing trial registers, such as ClinicalTrials.gov and Current Controlled Trials, were also undertaken. Gray literature was also searched via EThOS (British Library) and Conference Proceedings Index (Web of Science Core Collection). Searches were conducted from database inception to August 2017. No limits were set on language or publication status. Search terms were structured around the population (eg, “Lung Diseases, Obstructive”, “COPD”), intervention (eg, “Exercise Therapy”, “exercis* N3 supervi* OR training OR maintenance OR program*”), and study type (eg, “randomised”, “randomized”, “controlled”). An example of a full search strategy for CINAHL is presented in Table S1. Database searching was supplemented by contact with study authors and research groups, forward and backward citation tracking from included studies or previous relevant reviews, with further Internet searching via Google Scholar until August 2017.
Search results were collated using EndNote (Clarivate Analytics, Philadelphia, PA, USA). Duplicate citations were removed prior to independent screening of title and abstracts according to inclusion criteria by two reviewers. Full-text articles were obtained for all studies that were unable to be excluded based on title and abstract, before further independent screening to decide on final eligibility. Discrepancies in study eligibility were resolved through discussion between reviewers.
Data extraction and quality appraisal
Data extraction took place using a modified Cochrane Data Extraction Template including elements adapted from a taxonomy form previously used in randomized controlled trials.Citation14 Data were extracted by one reviewer and checked for accuracy by a second reviewer. List of characteristics extracted from studies is available in the Supplementary materials.
Two reviewers independently assessed the risk of bias for included studies using the Cochrane Risk of Bias Tool with the following domains: random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias.Citation15 Each domain was classified as low, unclear, or high with the risk of bias for each study classified using the following criteria: 1) low risk of bias (all criteria were deemed low), 2) medium risk of bias (one criterion graded as high or two criteria graded as unclear), and 3) high risk of bias (more than one criterion was deemed high or more than two criteria graded unclear). Disagreements between reviewers were resolved through further discussion.
Data analysis
All analyses were performed using Review Manager Version 5.3. The primary measures of effect were treated as dichotomous data (defined as the total number of participants in each group who had been hospitalized for respiratory cause, treated for an exacerbation, or died [all-cause]) and interpreted as risk ratios. Rate ratio of hospital admissions (respiratory-cause) and exacerbations was also calculated using the incidence rate in the intervention groups divided by the incidence rate in the control groups. Secondary outcomes of hospital admissions (all-cause), GP visits (all-cause), and outpatient visits were treated as dichotomous outcomes only and were interpreted as risk ratios. Length of hospital admissions (respiratory and all-cause) were analyzed as a continuous outcome and expressed as the between-groups difference in means. All primary and secondary outcomes were analyzed using raw data provided by authors rather than mean values presented in publications. If studies reported the same outcome measures, data were combined statistically using a random-effects meta-analysis. We contacted study authors to obtain missing numerical outcome data, and in cases where studies only reported certain outcomes of health care use, we verified that no additional data were available. The generic inverse-variance random-effects model for rates of hospitalization (respiratory) and exacerbation included the (natural) logarithms of the rate ratios and the standard error of the rate ratio.Citation15 Statistical heterogeneity was assessed by the I2 value. Data were not pooled if heterogeneity was found to be moderate (I2>30%). If heterogeneity was identified, potential sources were explored. Prespecified subgroup analyses included the setting, frequency, and delivery (training level of supervisor, combined with education) of supervised maintenance exercise programs. To test the robustness of findings in primary outcome measures, planned prespecified sensitivity analyses involved the removal of studies categorized as medium or high risk of bias within the Cochrane Risk of Bias Tool.
Results
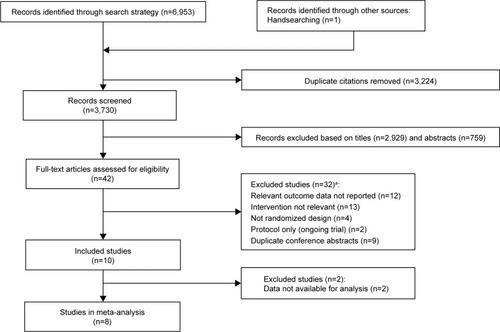
After the removal of duplicates, searches identified 3,730 records to be screened, of which 3,688 records were excluded based on title and abstract (). Full texts were obtained for the remaining 42 records. Information on excluded texts and reasons for these can be found in Table S2. Ten records (eight studies) met the inclusion criteria (), of which six studies had data available for meta-analysis. Two studies were excluded from the meta-analysis due to data not being available in the appropriate formatCitation16 and outcome definitions (eg, exacerbation) not meeting review eligibility criteria.Citation17
Table 1 Characteristics of included studies
Characteristics of included studies
The eight included studies were published between 2002 and 2017 (). The eight studies, in total, randomized 790 COPD patients (64% males), with study sample sizes ranging between 40 and 164. All stages of COPD severity (airflow limitation) were represented across included studies. All studies, except Moullec et al,Citation23,Citation24 randomized patients to either a control group (usual care) or a supervised maintenance exercise program following pulmonary rehabilitation. Moullec et alCitation23,Citation24 used a quasi-random method, whereby patients were consecutively assigned following pulmonary rehabilitation discharge. All supervised maintenance exercise interventions lasted between 9 and 12 months except for Guell et alCitation25 who provided a program for 36 months. Ringbaek et alCitation19 and Ries et alCitation16 had 6- and 12-month observation periods, respectively, following the completion of supervised maintenance exercise, data for which were not relevant for analysis in this review. Intervention procedures varied considerably between studies with one study providing an intense program of 3.5 h of supervised maintenance exercise a week,Citation23,Citation24 whereas another study provided one supervised maintenance session every 3 months.Citation20,Citation21 More details on interventions for all of the studies are given in .
Primary and secondary outcomes of this review were determined by either self-reporting of events by patientsCitation16,Citation17 or self-report validated through examination of health records.Citation18–Citation25 Health care use was reported as a secondary outcome in the majority of studiesCitation16–Citation24 with the publication of one study not reporting relevant outcomes.Citation25 Contact with authors of this study provided unpublished data relevant to this review. None of the studies had outcome data for all planned meta-analyses.
The risk of bias assessment was hindered by poor study reporting. Some studies presented with several unclear risks of bias domains, leading to overall high risk of bias. Due to high attrition rates, the risk of bias in four of the included studies in the meta-analyses was classified as high (). The only study with a low risk of bias was unable to be included in meta-analyses due to the lack of availability of data.Citation16
Table 2 Risk of bias assessment
Primary outcomes
Hospital admissions (respiratory cause)
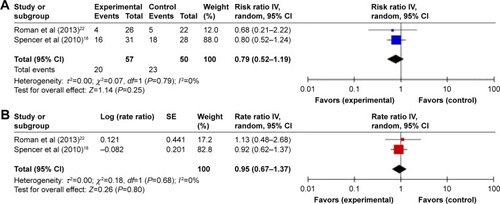
Meta-analysis of five trialsCitation18,Citation20,Citation22–Citation25 demonstrated a statistically significant reduction in the risk of experiencing at least one respiratory-cause hospital admission with continued supervised maintenance exercise following pulmonary rehabilitation (risk ratio 0.62, 95% confidence interval (CI) 0.47–0.81, P<0.001) (). There were no indications of heterogeneity in the findings (I2=0%).
Figure 2 Trial-level data, effect estimates, and forest plot of comparison for the overall risk (of experiencing at least one event) (A) and incidence rates (B) of respiratory-cause hospitalization.
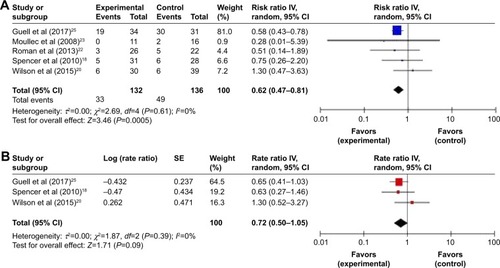
Three trials provided data on incidence rates,Citation18,Citation20,Citation25 whereby the overall estimate of the average effect suggested a reduction in the rate of respiratory-cause hospital admissions with supervised maintenance exercise (rate ratio 0.72, 95% CI 0.50–1.05, P=0.09, I2=0%) ().
Exacerbations requiring treatment with antibiotics and/or systemic corticosteroids
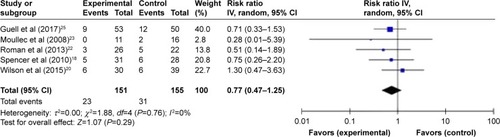
Meta-analysis of two trialsCitation18,Citation22 suggested a reduction in the risk of experiencing at least one exacerbation with supervised maintenance exercise (risk ratio 0.79, 95% CI 0.52–1.19, P=0.25, I2=0%) (). Synthesis of the incidence rates of exacerbations in these studies suggested a minimal effect of supervised maintenance exercise (rate ratio 0.95, 95% CI 0.67–1.37, P=0.80, I2=0%) ().
Mortality
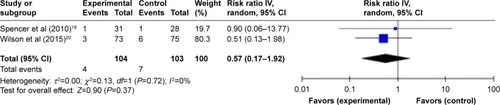
Meta-analysis of two trialsCitation18,Citation20 suggested a reduction in the risk of all-cause mortality with supervised maintenance exercise, but this was not statistically significant (risk ratio 0.57, 95% CI 0.17–1.92, P=0.37, I2=0%) (). The trial by Roman et alCitation22 was omitted from this analysis due to no events occurring in either group during the trial.Citation15
Secondary outcomes
Hospital admissions (all-cause)
Meta-analysis of three trialsCitation19,Citation20,Citation23 suggested a greater risk of experiencing at least one all-cause hospital admission with supervised maintenance exercise (risk ratio 1.14, 95% CI 0.80–1.62, P=0.48, I2=0%) (Figure S1).
Length of stay (respiratory cause and all-cause)
One trial provided data for length of hospital stay due to respiratory causeCitation18 (mean difference −1.60, 95% CI −4.73 to 1.53, P=0.32), and one trial provided data for length of hospital stay due to all-causeCitation19 (mean difference −0.20, 95% CI −2.31 to 1.91, P=0.85) with both favoring a shorter length of stay with supervised maintenance exercise.
Outpatient visits
Only one trial provided data for outpatient visits.Citation20 The overall estimate of effect suggested a nonsignificant reduction in the risk of experiencing at least one outpatient visit with supervised maintenance exercise (risk ratio 0.78, 95% CI 0.53–1.14, P=0.20).
GP visits
Meta-analysis of three trialsCitation18,Citation20,Citation22 suggested a minimal reduction in the number of patients making at least one GP visit with supervised maintenance exercise (risk ratio 0.92, 95% CI 0.75–1.11, P=0.38, I2=0%) (Figure S2).
Sensitivity analyses
As all studies included in the meta-analyses were assessed to have a medium or high risk of bias, we were unable to perform our prespecified sensitivity analyses. However, we deemed that a sensitivity analysis was required on our outcome of the risk of respiratory-cause hospital admissions due to the presence of one studyCitation25 that had a substantially longer intervention (and follow-up period) (36 months).
Assessing the number of patients suffering one or more exacerbation between groups (ie, risk ratio) will show the direction of the intervention effect, but it is heavily influenced by the duration of the trial.Citation26 Pooled analyses excluding Guell et alCitation25 led to the loss of statistical significance and reduction in the overall effect of supervised maintenance exercise on the overall risk of experiencing at least one respiratory-cause admission (risk ratio 0.81, 95% CI 0.43–1.52, P=0.51) (). Admission data were also retrieved from the study authors for the 1 year follow-up of this study, to allow further scrutiny of the effect of the duration of follow-up. Pooled analyses including the 12-month follow-up of Guell et alCitation25 also led to loss of statistical significance and reduction in the overall effect of supervised maintenance exercise on the overall risk of experiencing at least one respiratory-cause hospital admission (risk ratio 0.77, 95% CI 0.47–1.25, P=0.29) (). Due to limited number of completed trials, it was not possible to perform meaningful synthesis of prespecified subgroups on our primary outcomes.
Figure 5 Sensitivity analyses on trial-level data, effect estimates, and forest plot of comparison for the risk of hospital admission for a respiratory cause excluding Guell et al.Citation25
Abbreviations: CI, confidence interval; IV, inverse variance.
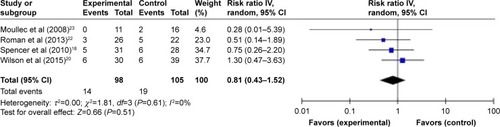
Figure 6 Sensitivity analyses on trial-level data, effect estimates, and forest plot of comparison for the risk of hospital admission for a respiratory cause including 0–12 months follow-up of Guell et al.Citation25
Discussion
To our knowledge, this is the first systematic review to identify eight completed randomized trials that compared the efficacy of supervised maintenance exercise following pulmonary rehabilitation with usual care on health care use in COPD, six of which had relevant data to be synthesized using meta-analysis.
Summary of main findings
Data synthesis of five trialsCitation18,Citation20,Citation22–Citation25 suggests that, on average, supervised maintenance exercise following pulmonary rehabilitation significantly reduces the risk of experiencing at least one respiratory-cause hospital admission by 38%. The current available evidence is heavily weighted by one trial,Citation25 whereby the magnitude of the point estimate is sensitive to the inclusion of this trial (due to length of follow-up). Synthesized data from three trialsCitation18,Citation20,Citation25 suggest that, on average, supervised maintenance exercise may also have an effect on multiple admissions by reducing the rate of respiratory-cause admissions by 28%. While pooling of studies for other primary measures in this review (relative risk reduction in exacerbations requiring treatment with antibiotics and/or systemic corticosteroids and all-cause mortality of 21% and 43%, respectively) did not translate to statistically significant changes, the point estimates of effect do surpass proposed thresholds of clinical significance.Citation26,Citation27 There is currently no evidence that supervised maintenance exercise following pulmonary rehabilitation has an effect on the risk of all-cause hospital admission or GP visits. Furthermore, there are insufficient data to synthesize the effect of supervised maintenance exercise on outpatient visits or duration of hospital stay following respiratory-cause and all-cause admission.
Strengths and limitations of the review
A strength of this review is that it is the first to conduct comprehensive searches and synthesis of published and unpublished data on health care use during supervised maintenance exercise programs compared to usual care following pulmonary rehabilitation. This review followed a preset, publicly available protocol detailing specific methodology. When the protocol for this review was written however, we did not anticipate the inclusion of trials with substantial differences in study follow-up. The recent study of Guell et alCitation25 has received plaudits for conducting such a long follow-up period of postpulmonary rehabilitation maintenance.Citation28 We feel that this deviation from our protocol in performing sensitivity analysis was strongly justified on the basis that studies with a longer observation period are likely to impact the robustness of our findings.
Extensive efforts were made to contact all trial authors to obtain additional data when outcomes did not appear in the available reports. The retrieval of additional data (beyond the published literature) reflects a key strength of our review. We, however, recognize that two studiesCitation16,Citation17 that met review eligibility criteria were not included in our meta-analyses; hence, this must be noted as a limitation. We identified inconsistencies in how our review outcomes were reported. The majority of the studies were limited by expressing hospitalizations/exacerbations as mean number of events per study group only and simply interpreted as a difference in means. However, a small minority of patients who experience multiple events can heavily influence this measure of effect, and the interpretation of such estimates is not as informative as when discrete (count) data are analyzed as ratios. From a statistical point of view, a strength of our review is that our measures of effect make full use of the data that have been collected in the included studies. Clinically, we allow health care practitioners and other relevant stakeholders to be able to interpret the effect of supervised maintenance exercise on the risk of whether a patient experiences an exacerbation and the efficacy of the intervention in reducing multiple events in the same patient.
The proposed minimal clinically important difference in COPD exacerbation frequency is 20%.Citation26,Citation27 As the entire range of the confidence interval for the effect of supervised maintenance exercise on hospitalization rates (ie, severe exacerbation) or risk of an exacerbation treated with antibiotics and/or systemic corticosteroids does not exceed the threshold of clinical usefulness, we cannot exclude the possibility that the reduction is of a magnitude not considered clinically worthwhile. Hence, the available evidence can be considered consistent with either an increase or a decrease in hospitalization rates (ie, severe exacerbation) or risk of an exacerbation as a result of the intervention.
The proportion of missing outcome data compared to observed outcome data in some of the trialsCitation20–Citation25 is enough to induce a clinically relevant bias in the observed intervention effects. There is no consensus on how to handle participants in a meta-analysis for whom data are not available.Citation15 We opted for an available case analysis as opposed to intention to treat analysis using imputation. Although our findings do provide an analysis of efficacy, the lack of intention to treat approach precludes an effectiveness analysis of the supervised maintenance exercise.Citation29
Effects estimated from published studies only may be inflated due to bias toward the nonpublication of studies with nonsignificant effects. The fact that all of the included published studies did not report significant effects of supervised maintenance exercise on health care use mitigates concerns about publication bias. All of the trials included in the meta-analyses were classified as having an overall medium or high risk of bias. Therefore, the quality of the overall evidence presented in this review is low. There were many individual domains where the risk of bias was unclear, primarily due to incomplete reporting. It is important to consider that this may not be poor reporting per se, and rather limitations in study design.Citation30 Also, as commonly found in COPD trials, especially those >6 months in duration, many studies were classified as having high attrition bias.Citation31
Comparison with other reviews
No previous systematic review has synthesized data from randomized controlled trials assessing the effects of supervised maintenance exercise following pulmonary rehabilitation on health care use. There were three previous systematic reviews in COPD that had synthesized the available evidence on supervised maintenance programs following pulmonary rehabilitation, but meta-analyses were limited to exercise capacity and quality of life outcomes.Citation5,Citation7,Citation32 Similarities, with regard to the benefits of exercise in our review, can be seen with Moore et alCitation8 where data from randomized controlled trials on health care use following pulmonary rehabilitation alone were synthesized. However, this review did not focus on interventions aiming to maintain exercise regimens following pulmonary rehabilitation but instead evaluated the short- and long-term benefits of initial pulmonary rehabilitation programs on exacerbations compared to no treatment. It was concluded that the delivery of pulmonary rehabilitation to stable COPD patients or patients following acute exacerbations results in reduced rates of hospitalizations compared to usual care. Our findings suggest that continuing maintenance exercise in a supervised manner following pulmonary rehabilitation may further enhance the benefit on certain health care use outcomes.
Implications for clinical practice
Based on the evidence presented in this review, it would currently be unwise to make specific recommendations on clinical care within this area. Due to the low precision (wide confidence intervals) in our effect estimates, only one of our meta-analyses translated to a statistically significant difference in health care use as a result of supervised maintenance exercise. However, early indications are promising, whereby the current point estimates of effect in some of the outcomes (eg, exacerbation rate) would be large enough to be classified as clinically significant. These clinically significant findings could have large implications for future postrehabilitation care. While there are proposals that “one size does not fit all” with pulmonary rehabilitation maintenance,Citation28 supervised maintenance exercise will likely play an important part in future practice recommendations. Arguably, the funding and reimbursement of supervised maintenance programs may largely depend on evaluations of cost-effectiveness. In theory, offering continued supervised maintenance exercise programs following pulmonary rehabilitation may not be cost-effective in the short term due to the initial outlay of setting up a program;Citation21,Citation33 however, the potential reductions in health care use in the medium to long term seen within this review may be large enough to produce a favorable cost–benefit ratio to health care budgets. This review highlights the importance of this active area of research and upon completion of further studies, its influence on future clinical practice.
Implications for future research
The findings of our meta-analyses must be interpreted in relation to quality and quantity of available evidence. The low precision of the individual study estimates (as a result of small sample sizes and hence low number of events) widens the confidence intervals for the point estimates of effect, highlighting the important impact that further research could have.
Further randomized trials addressing the current uncertainty about the effects of supervised maintenance exercise versus usual care on outcomes such as mortality and risk of exacerbation would need to be large (in sample size and/or a duration of follow-up ≥12 months). None of the included studies reported an a priori sample size calculation to determine the effect of supervised maintenance exercise on outcomes related to health care use.Citation18,Citation20,Citation22,Citation25 Future studies should include an appropriately powered sample size calculation based on proposed minimal clinically important differences. These studies should also adopt proper statistical analysis of outcomes (particularly exacerbations). Typical distribution of COPD exacerbations data and recommended statistical approaches have been discussed elsewhere.Citation34,Citation35 To facilitate critical appraisal and interpretation, future randomized trials would also benefit from adhering to Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Our findings have general applicability to all stable COPD patients referred to pulmonary rehabilitation. As none of the included trials stratified randomization by COPD severity, it is unclear whether our findings are equally applicable to all stages of COPD severity or exacerbation status. Further research is required to ascertain the effects of supervised maintenance exercise programs following early rehabilitation programs where patients are inherently considered to have a greater baseline risk of health care use. Similarly, our review was limited to patients with a diagnosis of COPD; efficacy of exercise maintenance options for other chronic respiratory conditions requires attention.
During our searches, we identified two protocols of randomized trials (based in the USA and Canada) that meet our eligibility criteria (Table S3).Citation36,Citation37 Compared to usual care following pulmonary rehabilitation, one studyCitation36 is randomizing patients to Tai Chi classes, or a walking group for a 6-month period, while another studyCitation37 is randomizing patients to a 12-month community exercise program. An update on the synthesis of the available evidence would be encouraged upon completion of the trials. For the design and delivery of new trials, research teams should note recent recommendations from the Australian and New Zealand Pulmonary Rehabilitation GuidelinesCitation6 that maintenance programs of monthly or three monthly supervised exercises (or less frequently) are insufficient to maintain exercise capacity or quality of life. It is reasonable to suggest that this frequency of supervised maintenance exercise compared with usual care is also unlikely to benefit outcomes related to health care use. However, we recognize that there is growing interest in different approaches to maintain the benefits of pulmonary rehabilitation, for example, telerehabilitation,Citation38 telecoaching,Citation39 and pedometer feedback.Citation40
Conclusion
This systematic review and meta-analysis suggests that supervised maintenance exercise programs compared to usual care following pulmonary rehabilitation may be beneficial in reducing health care use. However, the quality of the available evidence was variable. This outlines the requirement for methodologically sound and large studies to provide more precise estimates for the effects of postpulmonary rehabilitation maintenance.
Acknowledgments
We acknowledge the cooperation of authors (Rosa Guell, Pilar Cejudo Ramos, Lissa Spencer, Miguel Roman, Magdalena Esteva, Thomas Ringbaek, Ed Wilson, and Greg Moullec) of the included studies in this review for providing data in a format appropriate for analyses. We also thank Marilyn Moy, Laura Desveaux, and Dina Brooks for providing updates on their current ongoing trials related to this review. This review was conducted during Alex R Jenkins’ PhD studentship, which was part of the Doctoral Training Alliance Applied Biosciences for Health Programme.
Supplementary materials
Methods
Data extraction
The following study characteristics were extracted: methods of the study (date/title of the study, aim of study, study design, unit of allocation, duration of study, duration of intervention, primary outcome, secondary outcomes, and funding source), participants (population description, demographics, inclusion criteria, exclusion criteria, method of recruitment of participants, total number randomized, clusters, baseline imbalances, withdrawal and exclusions, and subgroups reported), intervention and where relevant comparator (group name, number randomized to group-sample size, description, venue numbers/locations, duration and frequency of maintenance exercise training period, delivery, providers, co-interventions, compliance/adherence, and defined parameters of usual care), and outcomes (outcome name, outcome type, outcome definition, person measuring/reporting, unit of measurement, scales [upper and lower limits], outcome tool validation, imputation of missing data, assumed risk estimate, and level of power).
Figure S1 Trial-level data, effect estimates, and forest plot of comparison for the risk of all-cause hospital admission.
Abbreviations: CI, confidence interval; IV, inverse variance.
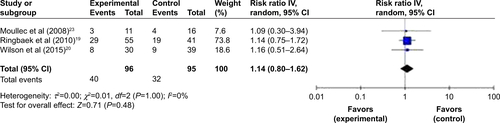
Figure S2 Trial-level data, effect estimates, and forest plot of comparison for the risk of GP visits.
Abbreviations: CI, confidence interval; GP, general practitioner; IV, inverse variance.
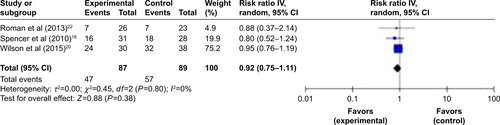
Table S1 Example search strategy of a bibliographic database (CINAHL)
Table S2 Characteristics of excluded studies
Table S3 Ongoing studies
References
- AndrewsSMCarterMDeoghareHMillsPKvan GundyKJainVVPulmonary rehabilitation maintenance program prevents accelerated FEV1 decline and may prevent exacerbations in patients with severe COPDAm J Respir Crit Care Med2015191A2013
- BernocchiPScalviniSBarattiDA multidisciplinary telehealth program in patients with combined chronic obstructive pulmonary disease and chronic heart failure: study protocol for a randomized controlled trialTrials201617146227659741
- BerryMJRejeskiWJAdairNEEttingerWHZaccaroDJSevickMAA randomized, trolled trial comparing long-term and short-term exercise in patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil200323606812576914
- BertoliniGNRamosDLeiteMREffects of a home-based exercise program after supervised resistance training in patients with chronic obstructive pulmonary diseaseMedicina201649331337
- BrooksDKripBMangovski-AlzamoraSGoldsteinRSThe effect of postrehabilitation programmes among individuals with chronic obstructive pulmonary diseaseEur Respir J200220202912166571
- BrownePOliveSStauntonLThe effects of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary diseaseThorax201368Suppl 3A16
- Carrieri-KohlmanVNguyenHQDonesky-CuencoDDemir-DevirenSNeuhausJStulbargMSImpact of brief or extended exercise training on the benefit of a dyspnea self-management program in COPDJ Cardiopulm Rehabil20052527528416217231
- CejudoPGaldizBPuyCEvaluation of a maintenance 3-year follow-up pulmonary rehabilitation programEur Respir J201444170825142478
- CejudoPGaldizBPuyCOutcomes evaluation of a maintenance 3-year follow-up pulmonary rehabilitation programmeAm J Respir Crit Care Med2014189A3645
- CruzJMarquesABrooksDWalk2Bactive: a randomized controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary diseaseChron Respir Dis2016131576626703921
- DesveauxLBeauchampMKLeeAIversNGoldsteinRBrooksDEffects of a community-based, post-rehabilitation exercise program in COPD: protocol for a randomized controlled trial with embedded process evaluationJMIR Res Protoc201652e6327169436
- du MoulinMTaubeKWegscheiderKBehnkeMvan den BusscheHHome-based exercise training as maintenance after outpatient pulmonary rehabilitationRespiration200977213914518667807
- EisnerBvan StratenJThe decline in acute hospitalizations for COPD patients in a pulmonary rehab maintenance programPresented at the National COPD ConferenceArlington, VA, USANovember 14–15, 2003
- ElliottMWatsonCWilkinsonEMuskAWLakeFRShort- and long-term hospital and community exercise programmes for patients with chronic obstructive pulmonary diseaseRespirology20049334535115363006
- FuJJMinJYuPMMcDonaldVMMaoBStudy design for a randomised controlled trial to explore the modality and mechanism of Tai Chi in the pulmonary rehabilitation of chronic obstructive pulmonary diseaseBMJ Open201668e011297
- GomezARomanMLarrazCEfficacy of respiratory rehabilitation on patients with moderate COPD in primary care and maintenance of benefits at 2 yearsAten Primaria200638423023316978561
- GuellRCasanPBeldaJLong-term effects of outpatient rehabilitation of COPD: a randomized trialChest2000117497698310767227
- HeppnerPSMorganCKaplanRMRiesALRegular walking and long-term maintenance of outcomes after pulmonary rehabilitationJ Cardiopulm Rehabil2006261445316617228
- HillCMcDonaldCA maintenance program post pulmonary rehabilitation improved exercise tolerance in patients with COPDRespirology20049A8
- KotrachHDajczmanEBaltzanMAA randomized controlled pilot study using a virtual game system (VGS) as a home-based exercise modality following pulmonary rehabilitation (PR) in patients with COPDAm J Respir Crit Care Med2016193A4530
- LinnebergARasmussenMBuchTFA randomised study of the effects of supplemental exercise sessions after a 7-week chronic obstructive pulmonary disease rehabilitation programClin Respir J20126211211921651747
- MartinezGThogersenJBrondumERingbaekTLangePEffect of maintenance training after 7 weeks rehabilitation programmeBerlinEuropean Respiratory Society Annual Congress2008
- MoyMLWaynePMLitrownikDLong-term exercise after pulmonary rehabilitation (LEAP): design and rationale of a randomized controlled trial of Tai ChiContemp Clin Trials201545Pt B45846726362690
- PerumalSDNiNO’DriscollMFJoyceRMcTJEfficacy of a maintenance programme on patients with COPD following pulmonary rehabilitationIrish J Med Sci2010179S482
- PleguezuelosEPerezMEGuiraoLImproving physical activity in patients with COPD with urban walking circuitsRespir Med20131071948195623890958
- RiesALMakeBJReillyJJPulmonary rehabilitation in emphysemaProc Am Thorac Soc2008552452918453366
- RingbaekTBroendumEMartinezGThoegersenJLangePEffect of maintenance training after 7-weeks rehabilitation programme on hospitalisationViennaEuropean Respiratory Society Annual Congress2009
- Rodriguez-TrigoGCejudoPPuyCLong term pulmonary rehabilitation programs for chronic obstructive pulmonary disease (COPD). Two years follow-upEur Respir J2011383645
- ScalviniSBernocchiPBarattiDMultidisciplinary telehealth program for patients affected by chronic heart failure and chronic obstructive pulmonary diseaseEur J Heart Fail2016189426663216
- SpencerLAlisonJMcKeoughZMaintenance of exercise capacity following pulmonary rehabilitation in COPD: a randomised controlled trialStockholmEuropean Respiratory Society Annual Congress2007
- SpencerLMAlisonJAMcKeoughZJDo supervised weekly exercise programs maintain functional exercise capacity and quality of life, twelve months after pulmonary rehabilitation in COPD?BMC Pulm Med200977
- SwertsPMKretzersLMTerpstra-LindemanEVerstappenFTWoutersEFExercise reconditioning in the rehabilitation of patients with chronic obstructive pulmonary disease: a short- and long-term analysisArch Phys Med Rehabil19907185705732369292
- van WeteringCRHoogendoornMMolSJRutten-van MolkenMPScholsAMShort- and long-term efficacy of a community-based COPD management programme in less advanced COPD: a randomised controlled trialThorax201065171319703824
- VasilopoulouMPapaioannouAIKaltsakasGHome-based maintenance tele-rehabilitation reduces the risk for AECOPD, hospitalizations and emergency department visitsEur Respir J2017495160212928546268
Disclosure
The authors report no conflicts of interest in this work.
References
- SpruitMSinghSGarveyCAn official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitationAm J Respir Crit Care Med201318881364
- McCarthyBCaseyDDevaneDMurphyKMurphyELacasseYPulmonary rehabilitation for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20152CD00379325705944
- LacasseYCatesCJMcCarthyBThis Cochrane Review is closed: deciding what constitutes enough research and where next for pulmonary rehabilitation in COPDCochrane Database Syst Rev201511ED00010726593129
- MadorMJPatelANNadlerJEffects of pulmonary rehabilitation on activity levels in patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil20113115259
- BeauchampMKEvansRJanaudis-FerreiraTGoldsteinRSBrooksDSystematic review of supervised exercise programs after pulmonary rehabilitation in individuals with COPDChest201314441124113323429931
- AlisonJAMcKeoughZJJohnstonKAustralian and New Zealand pulmonary rehabilitation guidelinesRespirology20172280081928339144
- BusbyAKReeseRLSimonSRPulmonary rehabilitation maintenance interventions: a systematic reviewAm J Health Behav201438332133024636028
- MooreEPalmerTNewsonRMajeedAQuintJKSoljakMAPulmonary rehabilitation as a mechanism to reduce hospitalizations for acute exacerbations of COPD: a systematic review and meta-analysisChest2016150483785927497743
- PuhanMAGimeno-SantosEScharplatzMPulmonary rehabilitation following exacerbations of chronic obstructive pulmonary diseaseCochrane Database Syst Rev201110CD00530521975749
- PuhanMAGimeno-SantosECatesCJPulmonary rehabilitation following exacerbations of chronic obstructive pulmonary diseaseCochrane Database Syst Rev201612CD00530527930803
- British Thoracic SocietyChronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and ManagementLondonBritish Thoracic Society2011
- American College of Physicians, American College of Chest Physicians, American Thoracic SocietyDiagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory SocietyAnn Intern Med2011155317919121810710
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal Strategy for the Diagnosis, Management, and Prevention of COPD – 2016 Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/Accessed December 12, 2017
- LambSEBeckerCGillespieLDReporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventionsTrials20111212521586143
- HigginsJPTGreenS webpage on the InternetCochrane Handbook for Systematic Reviews of Interventions Version 5.0.2. The Cochrane Collaboration2009 [updated September 2009]. Available from: http://handbook.cochrane.org/v5.0.2/Accessed April 18, 2017
- RiesALKaplanRMMyersRMaintenance after pulmonary rehabilitation in chronic lung diseaseAm J Respir Crit Care Med2003167688088812505859
- BrooksDKripBMangovski-AlzamoraSGoldsteinRSThe effect of postrehabilitation programmes among individuals with chronic obstructive pulmonary diseaseEur Respir J200220202912166571
- SpencerLAlisonJAMcKeoughZJMaintaining benefits following pulmonary rehabilitation: a randomised controlled trialEur Respir J201035357157719643944
- RingbaekTBrondumEMartinezGLong-term effects of 1-year maintenance training on physical functioning and health status in patients with COPDJ Cardiopulm Rehabil20103014752
- WilsonAMBrownePOliveSThe effects of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomised controlled trialBMJ Open201553e005921
- BurnsDKWilsonECFBrownePThe cost effectiveness of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: an economic evaluation alongside a randomised controlled trialAppl Health Econ Health Policy201614110511526346590
- RomanMLarrazCGomezAEfficacy of pulmonary rehabilitation in patients with moderate chronic obstructive pulmonary disease: a randomized controlled trialBMC Fam Pract2013142123399113
- MoullecGNinotGVarrayADesplanJHayotMPrefautCAn innovative maintenance follow-up program after a first inpatient pulmonary rehabilitationRespir Med2008102455656618164191
- MoullecGNinotGAn integrated programme after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: effect on emotional and functional dimensions of quality of lifeClin Rehabil201024212213620026578
- GuellMRCejudoPOrtegaFBenefits of long-term pulmonary rehabilitation maintenance program in severe COPD patients: 3 year follow-upAm J Respir Crit Care Med2017195562262927611807
- WedzichaJAMiravitllesMHurstJRManagement of COPD exacerbations: a European Respiratory Society/American Thoracic Society guidelineEur Respir J2017493160079128298398
- JonesPWBeehKMChapmanKRMinimally clinically important differences in pharmacological trialsAm J Respir Crit Care Med2014189325025524383418
- RochesterCSpruitMMaintaining the benefits of pulmonary rehabilitation. The Holy GrailAm J Respir Crit Care Med2017195554855128248138
- AaronSDFergussonDMarksGBCounting, analysing and reporting exacerbations of COPD in randomised controlled trialsThorax200863812212817702790
- KjaergardLLVillumsenJGluudCReported methodologic quality and discrepancies between large and small randomized trials in meta-analysesAnn Intern Med20011351198298911730399
- WelshEJCatesCJPoolePCombination inhaled steroid and long-acting beta2-agonist versus tiotropium for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20135CD00789123728670
- SoysaSMcKeoughZSpencerLEffects of maintenance programs on exercise capacity and quality of life in chronic obstructive pulmonary diseasePhys Ther Rev201217335345
- GriffithsTLPhillipsCJDaviesSBurrMLCampbellIACost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programmeThorax2001561077978411562517
- KeeneONJonesMRLanePWAndersonJAnalysis of exacerbation rates in asthma and chronic obstructive pulmonary disease: example from the TRISTAN studyPharm Stat200762899717230434
- KeeneONCalverleyPMJonesPWVestboJAndersonJAStatistical analysis of exacerbation rates in COPD: TRISTAN and ISOLDE revisitedEur Respir J2008321172418591336
- MoyMLWaynePMLitrownikDLong-term exercise after pulmonary rehabilitation (LEAP): design and rationale of a randomized controlled trial of Tai ChiContemp Clin Trials20154545846726362690
- DesveauxLBeauchampMKLeeAIversNGoldsteinRBrooksDEffects of a community-based, post-rehabilitation exercise program in COPD: protocol for a randomized controlled trial with embedded process evaluationJMIR Res Protoc201652e6327169436
- VasilopoulouMPapaioannouAIKaltsakasGHome-based maintenance tele-rehabilitation reduces the risk for AECOPD, hospitalizations and emergency department visitsEur Respir J2017495160212928546268
- NguyenHQGillDPWolpinSSteeleBGBendittJOPilot study of a cell phone-based exercise persistence intervention post-rehabilitation for COPDInt J Chron Obstruct Pulmon Dis2009430131319750190
- CruzJBrooksDMarquesAWalk2Bactive: a randomised controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary diseaseChron Respir Dis2016131576626703921