Abstract
Background
Cyclophilin A (CyPA) is a secreted molecule that is regulated by inflammatory stimuli. Although inflammation has an important role in the pathogenesis of chronic obstructive pulmonary disease (COPD), little is known regarding the relationship between serum CyPA and COPD.
Methods
Ninety-three COPD patients with acute exacerbation were enrolled in the study and were reassessed during the convalescence phase. Eighty-eight controls were matched for age, gender, body mass index, smoking index and comorbidity. The basic clinical information and pulmonary function of all participants were collected. Serum levels of CyPA and other inflammation indexes were further measured.
Results
Serum CyPA was significantly increased in convalescent COPD patients compared to healthy controls, and further elevated in COPD patients with acute exacerbation. Serum CyPA positively correlated with serum interleukin-6, matrix metalloproteinase-9 and high-sensitivity C-reactive protein in both the exacerbation and convalescence phases of COPD. Furthermore, it negatively correlated with percent value of forced expiratory volume in 1 second (FEV1%) predicted and FEV1/forced vital capacity in convalescent COPD patients.
Conclusion
These results suggest that serum CyPA can be used as a potential inflammatory biomarker for COPD and assessment of serum CyPA may reflect the severity of inflammation in COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by irreversible airflow limitation, chronic airway inflammation, and emphysema. The morbidity and mortality rates of COPD constantly increase partly because of environmental pollution and an aging population.Citation1 It has become a challenging problem worldwide.
Several mechanisms have been involved in the pathogenesis of COPD, such as inflammation, oxidant–antioxidant imbalance, proteinase–antiproteinase imbalance, immunologic mechanisms, apoptosis, and ineffective repair.Citation2 The inflammatory response has played an important role in the progression of COPD.Citation3 Airway inflammation in COPD is characterized by the infiltration of T lymphocytes, macrophages, and neutrophils.Citation4 It has been shown that airway inflammation correlates with disease severity and pulmonary function in COPD, as they are able to induce tissue damage through the release of various oxidants and proteases.Citation5 Not only airway inflammation, but also systemic inflammation is now recognized as an integral part of COPD pathogenesis.Citation6 Serum C-reactive protein, a well-known systemic inflammatory marker, has been demonstrated to correlate with disease severity, acute exacerbation frequency, and prognosis of COPD.Citation7 It has also been reported that several other serum biomarkers are used to assess systemic inflammation during the clinical course of COPD.Citation8
Cyclophilin A (CyPA) is a ubiquitously expressed protein belonging to the immunophilin family, which shares peptidyl-prolylcis-trans isomerase activity and was first identified as a cytosolic binding protein of the immunosuppressant cyclosporin A in 1984.Citation9,Citation10 CyPA has been involved in a variety of physiologic and pathologic activities, including protein folding, trafficking, and T-cell activation.Citation11 Although CyPA has initially demonstrated activity as an intracellular protein, it can be secreted into the extracellular environment in various cell types under inflammatory stimuli and oxidative stress.Citation12 The increased serum levels of CyPA can be observed in patients with acute coronary syndrome, diabetes mellitus, and chronic kidney disease.Citation13–Citation15 Despite inflammation and oxidative stress playing important roles in the pathogenesis of COPD, little is known regarding the relationship between serum CyPA and COPD. Therefore, our present study was designed to investigate the alterations of serum CyPA during clinical recovery from COPD exacerbation as well as the correlations between serum CyPA and other inflammatory biomarkers.
Materials and methods
Reagents
CyPA, high-sensitivity C-reactive protein (hsCRP), interleukin-6 (IL-6), and matrix metalloproteinase-9 (MMP-9) enzyme-linked immunosorbent assay (ELISA) kits were all purchased from Yuanye Biological Technology Co. Ltd (Shanghai, People’s Republic of China). The detection limit of the kits is 0.1 ng/mL for CyPA, 0.1 mg/L for hsCRP, 1 pg/mL for IL-6, and 1 ng/mL for MMP-9.
Patients and control subjects
COPD patients with acute exacerbation phase were admitted to the Department of Respiratory and Critical Care Medicine of The Second Affiliated Hospital of Xi’an Jiaotong University, between January 2016 and December 2016. The diagnosis criteria of COPD and acute exacerbation phase were according to the Global Initiative for Chronic Obstructive Lung Disease.Citation16 Patients who had asthma, bronchiectasis, pneumonia, sleep apnea syndrome, cancer, coronary artery disease, diabetes mellitus, and autoimmune diseases were excluded by medical history inquiry, physical examination, biochemical parameters determination (including autoantibodies and tumor markers), pulmonary function, electrocardiogram, ultrasonic cardiogram, and computed tomography. All enrolled patients were followed until the individual was medically stable enough to leave the hospital and not prone to acute exacerbation again. Patients who had adverse clinical outcomes were also excluded, including death from any cause in hospital, requiring mechanical ventilation and length of hospitalization time shorter than 1 day or longer than 30 days. Finally, 93 cases met the required inclusion and exclusion criteria, and were further evaluated 8 (interquartile range [IQR]: 7–11) days after the onset of exacerbation when they were convalescent. Healthy controls were recruited from the health examination center of the hospital, and 88 controls were matched with COPD patients for age, gender, body mass index, and smoking index. The present research was approved by the Research Committee of Human Investigation of Medical College of Xi’an Jiaotong University. All participants gave written informed consent.
Treatments of COPD
The routine treatments for exacerbated COPD during hospitalization were as follows: atomization inhalation of corticosteroids, β2-agonists, and anticholinergics, and intravenous infusions of methylprednisolone (with an initial dose of 40 mg daily), aminophylline, and expectorants. Antibiotics were administered if a bacterial infection was suspected and adjusted according to clinical symptoms and signs, sputum culture tests, and biochemical inflammatory markers. Oxygen was provided in order to maintain oxygen saturation $90%. Nebulized bronchodilators were prescribed for maintenance therapy upon discharge from the hospital.
Clinical variables
Variables including demographic data, smoking habits, course of disease, comorbidity condition, and respiratory symptoms were recorded on the day of admission. In consideration of severe breathing difficulties, exacerbated COPD patients did not perform pulmonary function examination. When they were stable enough to perform the spirometer maneuver before leaving the hospital, pulmonary function was assessed by an experienced technician. The basic clinical information and pulmonary function of healthy controls were also collected.
Sample collection and measurement
Venous blood samples of COPD patients were collected at the beginning of hospitalization (exacerbation) and at the end of hospitalization (convalescence). In addition, samples of healthy controls were collected upon healthy examination. Blood samples were centrifuged at 1000× g at 4°C for 20 min. And then serum was separated and stored at −80°C until further analysis. Routine blood testing was conducted for determining white blood cells (WBC) and neutrophil% by an autoanalyser (Sysmex XE-2100, Kobe, Japan) in the clinical laboratory. Serum concentrations of CyPA, hsCRP, IL-6, and MMP-9 were determined by commercial sandwich ELISA kits according to the manufacturer’s instructions. All the samples from each participant were measured in the same assay to reduce interassay variability.
Statistical analysis
Statistical analyses were conducted with SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA). All data were examined with Kolmogorov–Smirnov test for normal distribution. Continuous variables were presented as mean ± SD or median (interquartile range) according to the distribution state. Categorical variables were presented as a percentage. Normally distributed data were analyzed using Student’s t-tests, non-normally distributed data were compared using Wilcoxon–Mann–Whitney test, and categorical variables were compared with χ2 test. Correlation coefficients between CyPA levels and other laboratory values were analyzed by partial correlation with age, body mass index, and course of disease as continuous variables, and gender, smoking status, and presence of hypertension as dichotomous variables. Multivariate linear regression analysis was used to assess the relationship between CyPA and age, gender, body mass index, smoking status, course of disease, hypertension, and disease status. A value of P<0.05 was considered significant.
Results
summarizes the clinical characteristics of all study participants. The groups were well matched with respect to age, gender, body mass index, and smoking index. The proportion of subjects with hypertension was similar between COPD patients and healthy controls (P=0.672). The course of COPD was 10 (IQR: 4.5–13.5) years and median hospitalization time of those patients with exacerbated COPD was 8 (IQR: 7–11) days.
Table 1 Basic characteristics of the study population
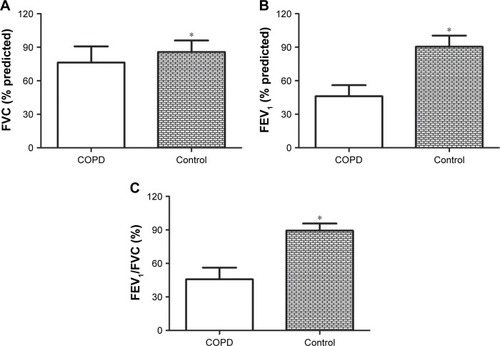
shows the parameters of pulmonary function including forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and FEV1/FVC ratio. Compared to healthy controls, FVC% predicted and FEV1% predicted in the convalescent COPD patients were both significantly decreased (76.4±14.4 versus 85.7±10.3 and 46.1±9.92 versus 90.4±10.0, respectively, both P<0.001). The ratio of FEV1/FVC in convalescent COPD patients was lower than that in the healthy control group (45.8±10.4 versus 89.3±6.40, P<0.001).
Figure 1 Pulmonary function of convalescent COPD patients (n=93) and healthy controls (n=88).
Abbreviations: COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
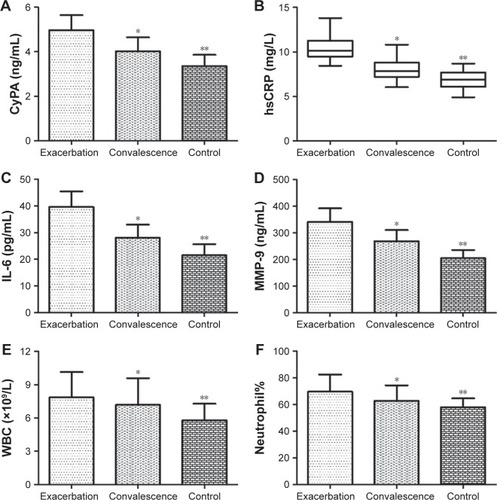
Serum concentration of CyPA in COPD patients with exacerbation phase was significantly higher than in the convalescence phase (4.97±0.68 versus 4.02±0.63 ng/mL, P<0.001). Moreover, CyPA serum concentration in convalescent COPD patients was notably increased compared to healthy controls (4.02±0.63 versus 3.36±0.51 ng/mL, P<0.001, ). Serum levels of hsCRP were 10.2 (IQR: 9.47–11.3) mg/L in exacerbated COPD, 7.86 (IQR: 7.20–8.80) mg/L in convalescent COPD, and 6.89 (IQR: 6.07–7.68) mg/L in healthy controls, and all the differences were significant (P<0.001, ). Serum concentrations of IL-6 and MMP-9 in the exacerbation phase of COPD were significantly higher than those in the convalescence phase (39.6±5.81 versus 28.1±4.93 pg/mL and 341±51.5 versus 269±41.6 pg/mL, respectively, both P<0.001). Compared to healthy controls, serum levels of IL-6 and MMP-9 in the convalescent COPD patients were also higher (28.1±4.93 versus 21.5±4.13 pg/mL and 269±41.6 versus 205±30.5 pg/mL, respectively, both P<0.001, ). In addition, there was a significant decline in WBC and neutrophil% from the exacerbation to the convalescence phase of COPD (P=0.047 and P<0.001, respectively). Furthermore, the values of WBC and neutrophil% further decreased in healthy controls (both P<0.001, ).
Figure 2 Inflammation indexes in COPD patients with exacerbation and convalescence phases (n=93) and healthy controls (n=88).
Abbreviations: COPD, chronic obstructive pulmonary disease; CyPA, cyclophilin A; hsCRP, high-sensitivity C-reactive protein; IL-6, interleukin-6; MMP-9, matrix metalloproteinase-9; WBC, white blood cells.
The partial correlation coefficients of serum CyPA with other laboratory parameters after adjustment for age, gender, body mass index, smoking index, course of disease, and comorbidity are presented in and . During the exacerbation and convalescence phases of COPD, serum CyPA values positively correlated with hsCRP (r=0.442 and 0.441, both P<0.05), IL-6 (r=0.343 and 0.307, both P<0.05), and MMP-9 (r=0.749 and 0.778, both P<0.05). Serum CyPA was also positively correlated with WBC and neutrophil% in exacerbated COPD patients (r=0.386 and 0.254, both P<0.05), but there were no statistical correlations between CyPA and WBC as well as neutrophil% in convalescent COPD patients (r=0.197 and 0.164, both P>0.05). During the convalescence phase of COPD, there was no statistical correlation between CyPA and FVC% predicted (r=−0.154, P=0.154). In addition, CyPA negatively correlated with FEV1% predicted (r=−0.271, P=0.011) and FEV1/FVC (r=−0.291, P=0.006) in convalescent COPD patients.
Table 2 Partial correlation coefficients of CyPA with laboratory parameters in exacerbated COPD
Table 3 Partial correlation coefficients of CyPA with laboratory parameters in convalescent COPD
Multivariate linear regression analysis with CyPA as the dependent variable showed that COPD disease status was the only major influence factor affecting CyPA (unadjusted r2=0.400, adjusted r2=0.376), while age, gender, body mass index, smoking status, course of disease, and hypertension did not appear to be significant factors influencing CyPA ().
Table 4 Multivariate linear regression of COPD patients with CyPA as the dependent variable
Discussion
CyPA is evolutionarily well conserved and expressed in all cells of organisms in both prokaryotes and eukaryotes.Citation17 It is mainly localized in the cytoplasm and shows a variety of intracellular functions, including intracellular signaling, protein trafficking, and the regulation of other protein activities.Citation11 CyPA can also be secreted into the extracellular environment from various cell types in response to infection, hypoxia, and oxidative stress.Citation18–Citation20 However, the concrete mechanism by which CyPA is secreted from cells is still unclear and may be associated with the acetylation of CyPA.Citation21 The secreted form of CyPA is known to function as an autocrine/paracrine factor, which mediates intercellular signal communication.Citation22
Current studies have demonstrated that CyPA is involved in the pathogenesis of several human diseases, such as cardiovascular disease, rheumatoid arthritis, sepsis, viral infection, cancer, nervous system degeneration, asthma, and periodontitis.Citation18,Citation23–Citation29 Proteomic analysis has found that the expression of CyPA is upregulated in smokers and particularly notable in COPD smokers.Citation30 However, alterations of serum CyPA in COPD patients remain unclear. Our present study showed that serum CyPA levels were increased in convalescent COPD patients compared to healthy controls, and further elevated in COPD patients with acute exacerbation. The major reason for the upregulation of serum CyPA concentration in COPD patients may be due to the inflammatory stimuli and oxidative stress. In addition, it has been reported that extracellular CyPA binds to extracellular matrix metalloproteinase inducer (EMMPRIN, CD147) and thereby initiates a cascade of inflammatory processes such as leucocyte chemotaxis and induction of MMP-9 and IL-6 expression.Citation31,Citation32 Therefore, we further evaluated serum concentrations of IL-6 and MMP-9 in COPD patients. Serum levels of IL-6 and MMP-9 were also increased in convalescent COPD patients and further increased in exacerbated COPD patients. Correlation analysis showed that CyPA positively correlated with IL-6 and MMP-9 in COPD patients with acute exacerbation and convalescence phases, suggesting that CyPA can strengthen its effect through the induction of IL-6 and MMP-9 expression.
COPD is characterized not only by local pulmonary inflammation, but also by systemic inflammation.Citation33 Various systemic inflammatory markers, including WBC, neutrophil%, mean platelet volume, erythrocyte sedimentation rate, hsCRP, D-dimer, cystatin C, and inflammatory cytokines have been used for the assessment of inflammation during COPD progression.Citation7,Citation8,Citation34–Citation36 This study found that hsCRP, WBC, and neutrophil% were significantly increased in both the exacerbation and convalescence phases of COPD, indicating that the inflammatory response persists through the convalescence phase. Correlation analysis showed that serum CyPA positively correlated with hsCRP during the exacerbation and convalescence phases of COPD, and negatively correlated with FEV1% predicted and FEV1/FVC in the convalescence phase. These results suggested that serum CyPA may be another inflammatory marker for COPD. In addition, the results of multivariate linear regression analysis suggested that age, gender, body mass index, smoking status, course of disease, and complication with hypertension did not significantly affect serum CyPA concentration, and COPD disease status was found to be the only major factor.
The strengths of our present study are the well-matched controls and direct comparison of CyPA at different phases of COPD. As diabetes mellitus and coronary artery disease affect serum CyPA expression,Citation13,Citation14 we ruled out these comorbidities in this study. It has also been reported that plasma CyPA level is influenced by essential hypertension,Citation37 so the patients and controls were well matched for hypertension proportion in the present study. Moreover, our results first suggest that serum CyPA may be a potential inflammatory biomarker for COPD. However, we should confirm that there are some limitations in this study. First, treatments of COPD patients may influence the statistical results among the three groups. Second, the pulmonary function of exacerbated COPD patients is absent. Third, the sample size in this study was not large. Finally, our study excluded COPD patients with comorbidities, so the results may not be generalized to all COPD patients.
In conclusion, this study shows that serum CyPA levels were increased in convalescent COPD patients compared to healthy controls, and further elevated in COPD patients with acute exacerbation. Moreover, serum CyPA positively correlated with hsCRP, IL-6, and MMP-9 in COPD with convalescence and exacerbation phases, and negatively correlated with FEV1% predicted and FEV1/FVC in convalescent COPD patients. Serum CyPA may be a reliable biomarker for assessing the systemic inflammatory response in COPD progression.
Acknowledgments
This study was supported by the National Nature Science Foundation of China (No 81600030), Natural Science Basic Research Project of Shaanxi Province (No 2016JQ8048), and Research Funds of The Second Affiliated Hospital of Xi’an Jiaotong University (No RC(XM)201604).
Disclosure
The authors report no conflicts of interest in this work.
References
- Lopez-CamposJLTanWSorianoJBGlobal burden of COPDRespirology2016211142326494423
- VijayanVKChronic obstructive pulmonary diseaseIndian J Med Res2013137225126923563369
- CazzolaMPageCPCalzettaLMateraMGEmerging anti-inflammatory strategies for COPDEur Respir J201240372474122496331
- TetleyTDInflammatory cells and chronic obstructive pulmonary diseaseCurr Drug Targets Inflamm Allergy20054660761817305517
- GompertzSBayleyDLHillSLStockleyRARelationship between airway inflammation and the frequency of exacerbations in patients with smoking related COPDThorax2001561364111120902
- BarnesPJCelliBRSystemic manifestations and comorbidities of COPDEur Respir J20093351165118519407051
- KaradenizGPolatGSenolGBuyuksirinMC-reactive protein measurements as a marker of the severity of chronic obstructive pulmonary disease exacerbationsInflammation201336494895323547018
- MacNeeWSystemic inflammatory biomarkers and co-morbidities of chronic obstructive pulmonary diseaseAnn Med201345329130023110517
- WangPHeitmanJThe cyclophilinsGenome Biol20056722615998457
- HandschumacherREHardingMWRiceJDruggeRJSpeicherDWCyclophilin: a specific cytosolic binding protein for cyclosporin AScience198422646745445476238408
- NigroPPompilioGCapogrossiMCCyclophilin A: a key player for human diseaseCell Death Dis20134e88824176846
- NigroPSatohKO’DellMRCyclophilin A is an inflammatory mediator that promotes atherosclerosis in apolipoprotein E-deficient miceJ Exp Med20112081536621173104
- YanJZangXChenRThe clinical implications of increased cyclophilin A levels in patients with acute coronary syndromesClin Chim Acta20124137–869169522209965
- RamachandranSVenugopalAKuttyVRPlasma level of cyclophilin A is increased in patients with type 2 diabetes mellitus and suggests presence of vascular diseaseCardiovasc Diabetol2014133824502618
- LiuMCLeeYWLeePTCyclophilin A is associated with peripheral artery disease and chronic kidney disease in geriatrics: the Tianliao Old People (TOP) studySci Rep20155993725909510
- VestboJHurdSSAgustiAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- SchlegelJArmstrongGSRedzicJSZhangFEisenmesserEZCharacterizing and controlling the inherent dynamics of cyclophilin-AProtein Sci200918481182419319933
- ZhouDMeiQLiJHeHCyclophilin A and viral infectionsBiochem Biophys Res Commun2012424464765022814107
- SekoYFujimuraTTakaHMinekiRMurayamaKNagaiRHypoxia followed by reoxygenation induces secretion of cyclophilin A from cultured rat cardiac myocytesBiochem Biophys Res Commun2004317116216815047162
- SatohKNigroPMatobaTCyclophilin A enhances vascular oxidative stress and the development of angiotensin II-induced aortic aneurysmsNat Med200915664965619430489
- SoeNNSowdenMBaskaranPAcetylation of cyclophilin A is required for its secretion and vascular cell activationCardiovasc Res2014101344445324293519
- QuXWangCZhangJQieGZhouJThe roles of CD147 and/or cyclophilin A in kidney diseasesMediators Inflamm2014201472867325580061
- SatohKShimokawaHBerkBCCyclophilin A: promising new target in cardiovascular therapyCirc J201074112249225620962430
- WangLWangCHJiaJFContribution of cyclophilin A to the regulation of inflammatory processes in rheumatoid arthritisJ Clin Immunol2010301243319789967
- TegederISchumacherAJohnSElevated serum cyclophilin levels in patients with severe sepsisJ Clin Immunol19971753803869327337
- LeeJRole of cyclophilin a during oncogenesisArch Pharm Res201033218118720195816
- AvramutMAchimCLImmunophilins in nervous system degeneration and regenerationCurr Top Med Chem20033121376138212871169
- StemmyEJBalsleyMAJurjusRADamskerJMBukrinskyMIConstantSLBlocking cyclophilins in the chronic phase of asthma reduces the persistence of leukocytes and disease reactivationAm J Respir Cell Mol Biol201145599199821493785
- LiuLLiCXiangJDongWCaoZOver-expression and potential role of cyclophilin A in human periodontitisJ Periodontal Res201348561562223441725
- HuROuyangQDaiATanSXiaoZTangCHeat shock protein 27 and cyclophilin A associate with the pathogenesis of COPDRespirology201116698399321585617
- YurchenkoVZybarthGO’ConnorMActive site residues of cyclophilin A are crucial for its signaling activity via CD147J Biol Chem200227725229592296511943775
- YuanWGeHHeBPro-inflammatory activities induced by CyPA-EMMPRIN interaction in monocytesAtherosclerosis2010213241542121035802
- BarnesPJCellular and molecular mechanisms of chronic obstructive pulmonary diseaseClin Chest Med2014351718624507838
- ZhangMLiYYangXSerum cystatin c as an inflammatory marker in exacerbated and convalescent COPD patientsInflammation201639262563126613760
- ZhangMLiYZhangJMean platelet volume is elevated in exacerbated and convalescent COPD patientsClin Chim Acta2015451Pt B22723126436484
- ZhangMZhangJZhangQD-dimer as a potential biomarker for the progression of COPDClin Chim Acta2016455555926826394
- ChangCSSuSLChangCCCyclophilin-A: a novel biomarker for untreated male essential hypertensionBiomarkers201318871672024164594
