Abstract
Background
Although studies have examined the relationship between metabolic syndrome (MetS) and COPD, the incidence of MetS in individuals with COPD has not specifically been investigated. This study aimed to evaluate the incidence of MetS in subjects with airway obstruction using data from a community-based cohort.
Patients and methods
Data representing 4 years of follow-up from the Ansung–Ansan cohort were analyzed; a total of 6,184 adults, who were ≥40 years of age and underwent spirometry, were enrolled in this study. Airway obstruction was defined as forced expiratory volume in 1 s/forced vital capacity ratio <70%, and MetS was determined according to the National Cholesterol Education Program Adult Treatment Panel III guidelines.
Results
A total of 419 patients were newly diagnosed with MetS, based on the National Cholesterol Education Program Adult Treatment Panel III guidelines, during follow-up. MetS was more frequent in COPD subjects, relative to non-COPD subjects, in both sexes (14.7% vs 11.0% [men] and 14.7% vs 11.8% [women]). In men subjects, the risk for MetS was higher in subjects with airflow obstruction than in subjects without obstruction, after adjusting for age, body mass index, and smoking status.
Conclusion
The incidence of MetS was higher in men with airflow obstruction than in healthy subjects.
Keywords:
Introduction
COPD is characterized by persistent air-flow limitation that is typically progressiveCitation1 and is a major cause of morbidity and mortality worldwide.Citation2 Metabolic syndrome (MetS) has been associated with several diseases, including cardiovascular disease, as well as with increased exacerbation of underlying disease and mortality risk.Citation3–Citation5 As COPD and MetS both constitute major public health problems, more precise and informative epidemiological data are needed regarding the relationship between COPD and MetS.
Previous studies have evaluated the prevalence of MetS in COPD patients and normal subjects.Citation6,Citation7 In addition, a Korean study reported a relatively higher prevalence of MetS in patients with COPD, compared with healthy subjects.Citation8,Citation9 However, there have been no community-based cohort studies investigating the incidence of MetS in COPD patients.
Many of the previous studies regarding MetS in COPD were cross-sectional and primarily focused on the prevalence, rather than the incidence, of MetS in patients with COPD. Thus, the present study aimed to evaluate the incidence and characteristics of MetS in COPD patients using data from a large community-based cohort.
Patients and methods
Study population
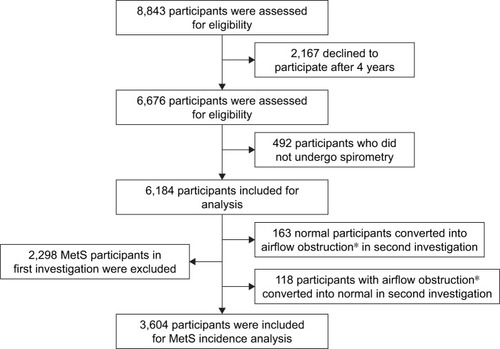
Prospectively collected data from the Ansung–Ansan cohort were used for this analysis. The Ansung–Ansan cohort is a community-based sample that was evaluated in the Korean Genome and Epidemiology study (KoGES). The KoGES cohort included subjects from both the Ansan (urban) and Anseong (rural) areas of Korea for prospective investigation. Detailed information regarding the study design and protocols has been previously published.Citation10 The baseline survey of the Ansung–Ansan cohort was conducted between May 2001 and February 2003; the present study included 8,843 eligible adults who were 40–69 years of age. Follow-up examinations were performed biennially. Of these subjects, 6,676 were reevaluated after 4 years, corresponding with a follow-up rate of 75.4% in the secondary survey (2005–2006). Subjects who did not undergo pulmonary function testing at baseline and follow-up after 4 years (n = 492) were excluded. Of the remaining 6,184 subjects, a further 2,298 were excluded because they exhibited MetS in the baseline survey. Although subjects were diagnosed with COPD at the time of the baseline survey, those exhibiting normal pulmonary function results in the secondary survey were excluded (n = 118), as were participants with normal lung function who exhibited COPD in the second investigation (n = 163). Ultimately, a total of 3,604 subjects were included in the final analysis ().
Definition of MetS and airflow obstruction
MetS was defined clinically based on the presence of ≥3 of the following modified Adult Treatment Panel III revised guidelines:Citation11 central obesity (with waist circumference cutoff points of >90 cm for men and >80 cm for women); an elevated triglyceride level (≥1.7 mmol/L or undergoing drug treatment for elevated triglyceride levels); a reduced high-density lipoprotein cholesterol (HDL-C) level (<1.0 mmol/L [men], <1.3 mmol/L [women], or drug treatment for reduced HDL-C); elevated blood pressure (≥130 mmHg systolic, ≥85 mmHg diastolic, or antihypertensive drug treatment in patients with a history of hypertension); and an elevated fasting plasma glucose concentration (≥5.6 mmol/L or drug treatment for diabetes).
Lung function tests were performed by a skilled technician using a portable spirometer (Vmax-2130, Sensor Medics, Yorba Linda, CA, USA) in accordance with stan-dardized protocols from the American Thoracic Society.Citation12 All participants underwent pulmonary function testing during each visit (at baseline as well as the first and second follow-up visits). Calibration and quality control of spiro-metric examinations were performed regularly, based on American Thoracic Society guidelines.Citation12 Airflow obstruction was defined as a prebronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of <0.7.
Statistical analysis
All values are expressed as mean ± standard deviation. Continuous and categorical variables were compared using Student’s t-test and the chi-squared/Fisher’s exact test, respectively. Logistic regression analyses were performed to estimate odds ratios (ORs) with 95% confidence intervals (CIs) for MetS development, after adjusting for other confounding variables; P < 0.05 was considered to be statistically significant. Statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Ethics approval
The Korean Centers for Disease Control and Prevention obtained written informed consent from all participants, and the Institutional Review Board of Severance Hospital (Seoul, South Korea) approved the study protocol (4-2016-0458). The data accessed from the KoGES cohort study is anonymous.
Results
Baseline patient characteristics
describes the baseline characteristics of all patients who were included in the analysis. In total, 3,604 subjects (51.1% men, 45.9% women) were included in our analysis. The mean age of the patients was 50.5 ± 8.4 years. There was an age difference between men and women (50.8 ± 8.5 vs 50.0 ± 8.3, P = 0.004). Among all included subjects, 23.1% and 4.3% exhibited hypertension and diabetes mellitus, respectively. The proportion of current smokers was 44.1% of male subjects and 2.5% of female subjects (P < 0.001).
Table 1 Baseline characteristics of men and women subjects included in the study
The average body mass index (BMI) was 23.9 kg/m2, with female subjects exhibiting a relatively lower mean BMI than male subjects (24.0 kg/m2 vs 23.8 kg/m2, P = 0.015). There were no differences in lung function or physical activity between male and female subjects. At baseline, 252 of 3,604 (7.0%) subjects exhibited airflow obstruction. The proportion of male subjects with COPD was significantly higher than the proportion of female subjects with COPD (11.8% vs 1.9%, P < 0.001). The median follow-up duration was 4 years (interquartile range: 3.0–4.0 years).
Incidence of MetS
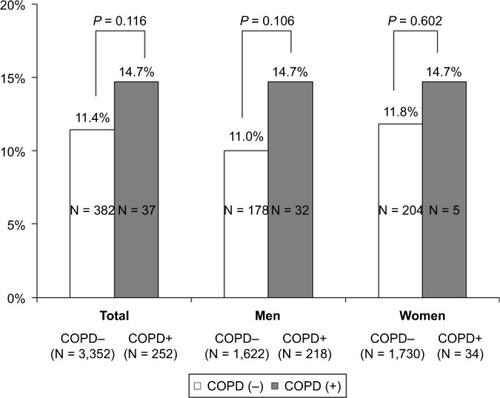
During the follow-up period, 11.6% (n = 419) of patients developed MetS based on the National Cholesterol Education Program Adult Treatment Panel III guidelines.Citation11 The incidence of MetS was higher in patients with COPD, relative to those without COPD, for both sexes (11.0% vs 14.7% [men] and 11.8% vs 14.7% [women]) (). shows the result of a multivariate logistic regression analysis of risk factors for MetS. After adjusting for confounding variables, such as age, BMI, and smoking, male patients with airflow obstruction were 1.76-fold (95% CI 1.04–2.96, P = 0.028) more likely to develop MetS, relative to normal subjects. Thus, the risk for MetS in subjects with airway obstruction was higher in the subgroup of male subjects, following adjustment for age, BMI, smoking, and physical activity.
Table 2 Association between metabolic syndrome and lung function impairment at 4 years of follow-up
Figure 2 Incidence of metabolic syndrome in patients with COPD at 4 years of follow-up.
Discussion
This is the first study to confirm the incidence of Mets in COPD patients via data from a large community-based cohort. The incidence of MetS was higher in the airflow obstruction group, even after adjustment for other confounding factors, including age, BMI, smoking, and physical activity, in male subjects. This finding is consistent with previous studies that have reported an increased prevalence of MetS in patients with COPD. However, clinical implication of the present study is that it was the first to evaluate and compare the incidence of MetS between patients with and without airflow obstruction.
In the present study, incidence of MetS was higher in patients with impaired lung function. However, a strength of our study was that we defined the airflow obstruction group according to airflow limitation, rather than FEV1 quartile or changes in FVC. Previously, Kim et al investigated the incidence of MetS in patients with impaired lung function.Citation13 In that study, changes in vital capacity over a 6-year period were associated with development of MetS, which itself was associated with obesity and abdominal obesity. However, the patients included in that study did not exhibit COPD, nor were they enrolled from a community-based sample. Another group attempted to characterize the incidence of MetS using 2-year follow-up data from Health Screening Centers in Taiwan.Citation14 In contrast to the present study, the follow-up duration in the Taiwan-based study was short and the target group was divided according to FEV1, rather than airflow limitation; furthermore, the target group was not a community-based cohort. There is significant disparity between the present study and previous studies regarding the accuracy of the definition of airflow obstruction.
Some studies have reported an association between COPD and MetS. Recent reviews revealed that the mean prevalence of MetS in patients with COPD was 32% (range 23%–58%), compared with 30% (range 17%–54%) in controls. Moreover, the average reported prevalence of MetS varies among different regions, with a lower prevalence in studies from Asia (28%), relative to European (41%) and American studies (53%).Citation6 Furthermore, the difference in MetS prevalence between COPD patients and controls was small, which may be related to the inclusion of subjects without COPD, but with other comorbidities, in the control group. In this study, we confirmed the prevalence of MetS in both populations (34.8%), relative to the control group (28.4%). The rates revealed in the present study are consistent with other recent reports. Additionally, the 4-year incidence of MetS was higher in the airflow obstruction group, relative to the control group. Several groups have investigated the incidence of MetS using different diagnostic methods, including spirometry and health care databases.Citation15–Citation17 A study by Breyer et al revealed that the prevalence of MetS was higher in patients with COPD.Citation18 Similarly, in a study involving Asian subjects, the risk for MetS was higher in individuals with airflow obstruction, relative to individuals without obstruction, even after adjustment for potential confounders.Citation19 Additionally, a Korean study that used data from a nationwide survey reported that the risk for MetS was higher in sarcopenic males with COPD;Citation8 notably, the prevalence of MetS was also higher.Citation9 Previous studies, however, have sought to evaluate the relationship between COPD and MetS primarily through measurement of the prevalence of MetS. The findings from our study are unique in that we are the first to report the incidence of MetS in patients with COPD using data from a large community-based cohort. In contrast to other studies, the present study involved repeated measurements of pulmonary function and participants were more accurately categorized according to airflow obstruction, which differs from the methods used in previous investigations.
Many studies have investigated the relationship between COPD and the presence of comorbidities. In patients with COPD and MetS, cardiovascular comorbidities are more prevalent and are associated with an increased mortality, largely related to the aggravation of underlying disease.Citation20,Citation21 A possible explanation for higher incidence of MetS among COPD patients may be that COPD patients with MetS are physically less active and exhibit increased levels of systemic inflammation relative to healthy patients.Citation22,Citation23 However in this study, these particular differences were not clearly observed, perhaps because the number of patients with MetS was insufficient; moreover, patients with severe and very severe airflow obstruction were not included in the analysis.
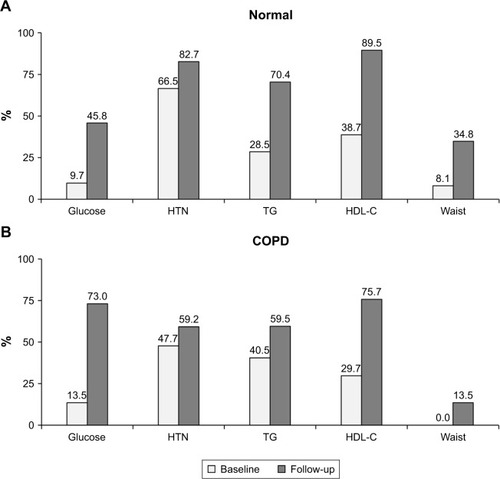
Although pathophysiological consequences of MetS remain controversial, insulin resistance may play a crucial role.Citation24 Findings of the present study regarding airflow obstruction and occurrence of insulin resistance, which was defined as increased fasting plasma glucose levels, are generally consistent with previous studies.Citation14 For example, Lawlor et alCitation25 observed an inverse association between insulin resistance and lung function, following adjustment for important confounding factors. In addition, Lazarus et alCitation26 reported that decreased lung function at baseline predicted insulin resistance over 20 years of follow-up, independent of age, BMI, waist-to-hip ratio, or cigarette smoking status. Additional studies have demonstrated that patients with impaired lung function carry an increased risk for developing insulin resistance and type 2 diabetes mellitus.Citation27–Citation29 Consistent with these findings, we found that the percentage change in glucose level was higher in patients with COPD, suggesting that insulin resistance may be an independent risk factor for the incidence of MetS among COPD patients ().
Figure 3 Individual components of metabolic syndrome in normal and COPD patients. (A) Individual component changes (expressed as percentage) in metabolic syndrome in normal subjects. (B) Individual component changes (expressed as percentage) in metabolic syndrome in subjects with COPD.
According to the International Diabetes Federation, the prevalence of MetS is largely affected by abdominal obesity. Indeed, patients with obstructive lung disease exhibit more visceral fat mass, relative to healthy subjects.Citation30 In the present study, these findings are indirectly confirmed by the observation that the incidence of MetS was higher in individuals with a higher BMI (25.5 kg/m2 vs 23.7 kg/m2). It remains unclear why abdominal obesity is more prevalent in COPD patients than in healthy subjects; however, various factors, including poor nutrition and inactive lifestyle, may play an important role.Citation30 Future longitudinal studies with larger sample sizes are required to further investigate the causal relationship between COPD and MetS.
Our study has several strengths. To our knowledge, this was the first study to evaluate the incidence of MetS in patients with airflow obstruction. Second, we evaluated the risk for MetS using a relatively large community-based population with a relatively long duration of follow-up. Third, we accurately classified patients as COPD or non-COPD through repeated pulmonary function tests; moreover, we obtained MetS data via laboratory tests and accurate medical history, rather than through patient interviews.
Our study also included multiple limitations. First, we could not analyze other important comorbidities, such as cardiovascular disease and malignancies, because of the absence of objective data regarding both factors. Second, most patients with airway obstruction were classified as exhibiting mild or moderate disease; the exclusion of patients with severe disease, therefore, may have influenced our results. Third, the incidence of MetS was higher in only male subjects, which might be influenced by smoking status and low event number in female subjects (n = 5). Further, large prospective studies are needed to more clearly elucidate the relationship between airflow obstruction and the incidence of MetS in the general population.
Conclusion
The incidence of MetS was higher in COPD patients, relative to controls, and was most influenced by fasting blood glucose level and high blood pressure. The incidence of MetS was higher in older, male COPD subjects, who exhibited higher BMI and more severe smoking status. Future longitudinal and interventional studies are needed to elucidate the relationship between airflow obstruction and the incidence of MetS in the general population.
Author contributions
All authors contributed toward data analysis, drafted and critically revised the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Data availability
The data are not available for public access because of patient privacy concerns.
Disclosure
The authors report no conflicts of interest in this work.
References
- VogelmeierCFCrinerGJMartinezFJGlobal Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD executive summaryAm J Respir Crit Care Med2017195555758228128970
- ManninoDMBuistASGlobal burden of COPD: risk factors, prevalence, and future trendsLancet2007370958976577317765526
- AlbertiKGZimmetPShawJMetabolic syndrome – a new worldwide definition. A consensus statement from the International Diabetes FederationDiabet Med200623546948016681555
- IsomaaBAlmgrenPTuomiTCardiovascular morbidity and mortality associated with the metabolic syndromeDiabetes Care200124468368911315831
- LakkaHMLaaksonenDELakkaTAThe metabolic syndrome and total and cardiovascular disease mortality in middle-aged menJ Am Med Assoc20022882127092716
- Cebron LipovecNBeijersRJvan den BorstBDoehnerWLainscakMScholsAMThe prevalence of metabolic syndrome in chronic obstructive pulmonary disease: a systematic reviewCOPD201613339940626914392
- BaffiCWWoodLWinnicaDMetabolic syndrome and the lungChest201614961525153426836925
- ChungJHHwangHJHanCHSonBSKimDHParkMSAssociation between sarcopenia and metabolic syndrome in chronic obstructive pulmonary disease: the Korea National Health and Nutrition Examination Survey (KNHANES) from 2008 to 2011COPD2015121828924914701
- ParkBHParkMSChangJChronic obstructive pulmonary disease and metabolic syndrome: a nationwide survey in KoreaInt J Tuberc Lung Dis201216569470022410468
- ShinCAbbottRDLeeHKimJKimmKPrevalence and correlates of orthostatic hypotension in middle-aged men and women in Korea: the Korean Health and Genome StudyJ Hum Hypertens2004181071772315116144
- GrundySMCleemanJIDanielsSRDiagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific StatementCirculation2005112172735275216157765
- Standardization of spirometry, 1994 update. American Thoracic SocietyAm J Respir Crit Care Med19951523110711367663792
- KimSKBaeJCBaekJHDecline in lung function rather than baseline lung function is associated with the development of metabolic syndrome: a six-year longitudinal studyPLoS One2017123e017422828346522
- HsiaoFCWuCZSuSCBaseline forced expiratory volume in the first second as an independent predictor of development of the metabolic syndromeMetabolism201059684885320006363
- FordESCunninghamTJMercadoCILung function and metabolic syndrome: findings of National Health and Nutrition Examination Survey 2007–2010J Diabetes20146660361326677470
- Diez-ManglanoJBarquero-RomeroJAlmagroPCOPD patients with and without metabolic syndrome: clinical and functional differencesIntern Emerg Med20149441942523645508
- ChoiJHParkSShinYHKimMYLeeYJSex differences in the relationship between metabolic syndrome and pulmonary function: the 2007 Korean National Health and Nutrition Examination SurveyEndocr J201158645946521502707
- BreyerMKSpruitMAHansonCKPrevalence of metabolic syndrome in COPD patients and its consequencesPLoS One201496e9801324950070
- LamKBJordanREJiangCQAirflow obstruction and metabolic syndrome: the Guangzhou Biobank Cohort StudyEur Respir J201035231732319574332
- ManninoDMThornDSwensenAHolguinFPrevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPDEur Respir J200832496296918579551
- DivoMCoteCde TorresJPComorbidities and risk of mortality in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2012186215516122561964
- WaschkiBKirstenAHolzOPhysical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort studyChest2011140233134221273294
- WatzHWaschkiBKirstenAThe metabolic syndrome in patients with chronic bronchitis and COPD: frequency and associated consequences for systemic inflammation and physical inactivityChest200913641039104619542257
- SchmidtAMInsulin resistance and metabolic syndrome: mechanisms and consequencesArterioscler Thromb Vasc Biol2012328175322815339
- LawlorDAEbrahimSSmithGDAssociations of measures of lung function with insulin resistance and type 2 diabetes: findings from the British Women’s Heart and Health StudyDiabetologia200447219520314704837
- LazarusRSparrowDWeissSTBaseline ventilatory function predicts the development of higher levels of fasting insulin and fasting insulin resistance index: the Normative Aging StudyEur Respir J19981236416459762793
- LinWYYaoCAWangHCHuangKCImpaired lung function is associated with obesity and metabolic syndrome in adultsObesity (Silver Spring)20061491654166117030977
- EngstromGHedbladBNilssonPWollmerPBerglundGJanzonLLung function, insulin resistance and incidence of cardiovascular disease: a longitudinal cohort studyJ Intern Med2003253557458112702035
- FordESManninoDMProspective association between lung function and the incidence of diabetes: findings from the National Health and Nutrition Examination Survey Epidemiologic Follow-up StudyDiabetes Care200427122966297015562215
- van den BorstBGoskerHRKosterAThe influence of abdominal visceral fat on inflammatory pathways and mortality risk in obstructive lung diseaseAm J Clin Nutr201296351652622811442