Abstract
Background
Measurement of quadriceps muscular force is recommended in individuals with COPD, notably during a pulmonary rehabilitation program (PRP). However, the tools used to measure quadriceps maximal voluntary contraction (QMVC) and the clinical relevance of the results, as well as their interpretation for a given patient, remain a matter of debate. The objective of this study was to estimate the minimally important difference (MID) of QMVC using a fixed dynamometer in individuals with COPD undergoing a PRP.
Methods
Individuals with COPD undergoing a PRP were included in this study. QMVC was measured using a dynamometer (MicroFET2) fixed on a rigid support according to a standard-ized methodology. Exercise capacity was measured by 6-minute walk distance (6MWD) and evaluation of quality of life with St George’s respiratory questionnaire (SGRQ) and Hospital Anxiety and Depression Scale (HADS) total scores. All measures were obtained at baseline and the end of the PRP. The MID was calculated using distribution-based methods.
Results
A total of 157 individuals with COPD (age 62.9±9.0 years, forced expiratory volume in 1 second 47.3%±18.6% predicted) were included in this study. At the end of the PRP, the patients had improved their quadriceps force significantly by 8.9±15.6 Nm (P<0.001), as well as 6MWD by 42±50 m (P<0.001), SGRQ total score by −9±17 (P<0.001) and HADS total score by −3±6 (P<0.001). MID estimation using distribution-based analysis was 7.5 Nm by empirical rule effect size and 7.8 Nm by Cohen’s effect size.
Conclusion
Measurement of QMVC using a fixed dynamometer is a simple and valuable tool capable of assessing improvement in quadriceps muscle force after a PRP. We suggest an MID of 7.5 Nm to identify beneficial changes after a PRP intervention.
Introduction
Along with limitations in respiratory capacity, peripheral or limb-muscle dysfunction is a widely recognized consequence of COPD,Citation1 causing particularly quadriceps-muscle weakness.Citation2,Citation3 A reduction of 30% in quadriceps muscular force among the patients with COPD has been observed when compared to healthy elderly volunteers.Citation4 This is mainly attributed to reduction in lean mass and a decrease in the cross-sectional area of the muscle,Citation5,Citation6 as well as decreased muscular endurance and increased susceptibility to fatigue,Citation7 further worsening a sedentary lifestyle. It has also been observed that despite the respiratory problems, individuals with COPD stop exercise, not due to the breathlessness, but rather due to the perception of leg fatigue.Citation8 The prevalence of reduced quadriceps strength has also been reported in other chronic diseases such as diabetesCitation9 and chronic heart failure (CHF),Citation10 serving as a predictor of mortality in the latterCitation11 and in COPD.Citation12 Moreover, quadriceps muscular force represents a valuable target to measure, as it allows identification of responders to a pulmonary rehabilitation program (PRP).Citation13 Among the different techniquesCitation14 to measure quadriceps strength, the use of a handheld dynamometerCitation15 for the evaluation of quadriceps maximal voluntary contraction (QMVC), where resistance is applied by the operator either directly on the deviceCitation16 or by the use of straps,Citation17 is known to be a simple and reproducible method.Citation18 The technique, though well known as a handheld method, also accepts the use of a stabilization belt to fix the dynamometer on a rigid support that limits operator-induced bias.Citation19 The simplicity of this method makes it possible to conduct this measurement in any clinical setting with minimal equipment. Despite its usage over rather a long time, we lack information on what an improvement in this measure really signifies for patients.
There have been previous studies on the evolution of quadriceps strength after a rehabilitation program in chronic diseases, such as diabetesCitation20 and CHF.Citation21 In COPD, a significant increase in quadriceps strength by 8% following aerobic training and 20% following combined aerobic and strength training have been identified.Citation22 Although differing in methodology of measurement, the study of change in quadriceps strength after an intervention of rehabilitation is of great value. However, its minimally important difference (MID) remains unknown. The MID is a useful expression defined as “the minimal amount of change required between two points in time to be confident that a patient has truly changed”.Citation23 A reduction of 4% in isometric force has been suggested as the minimal change to bring about a relevant difference in osteoarthritis of the knee.Citation24 Similarly, a preliminary result by Quessada et al suggested an MID of 33 Nm for QMVC in individuals with COPD undergoing exercise training.Citation25 As preliminary data from a small sample, these results and the insight on the technique of measurement remain to be confirmed in a larger population. From this perspective, we aimed to determine the MID for QMVC using a simple fixed dynamometer in individuals with COPD undergoing a PRP.
Methods
Subjects
Patients were included in the study if they fulfilled the inclusion criteria of a diagnosis of COPD according to the Global initiative for Chronic Obstructive Lung Disease (GOLD) recommendations,Citation26 having completed a PRP including exercise training and education component as recommended,Citation27 and written consent signed by the patient prior to the beginning of the program. Patients from Nantes were included in the cohort RehaEffort from the Institut de Recherche en Santé Respiratoire des Pays de la Loire and patients from North Brittany were from the Centre Hospitalier des Pays de Morlaix. Exclusion criteria were the presence of a lower-limb lesion hampering the measurement of quadriceps strength and the presence of joint limitations. The patients were recruited in three different centers in two cities of France: the University Hopsital of Nantes and the Tourmaline Medical Centre in Nantes and the Centre Hospitalier des Pays de Morlaix in Morlaix. In Nantes, the study was conducted by the RehaEffort cohort group from the Institut de Recherche en Santé Respiratoire des Pays de la Loire, for which approval was obtained from the ethical board (Comité de Protection des Personnes [CPP] – 2009/17) and the Comité Consultatif sur le Traitement de l’Information en Matière de Recherche dans le Domaine de la Santé [CCTIRS] (07.207 bus). Patients from the Centre Hospitalier des Pays de Morlaix signed a written informed consent in accordance with the Declaration of Helsinki and the current guidelines for Good Clinical Practice after approval by the institutional medical ethics committees (CPP Ouest 6 – CPP803, 2013-A01180-45).
Study design
All patients included went through a complete outpatient or inpatient evaluation in the institutions to assess individual deficiency, incapacity, and social disadvantage, as recommended.Citation27 Pulmonary function tests, including spirometry, plethysmography, and diffusion capacity, were conducted according to European Respiratory Society and American Thoracic Society task-force recommendations.Citation28,Citation29 All patients performed a cardiopulmonary exercise test using a progressive 10 W incremental test on an electromagnetically braked cycle ergometer up to exhaustion, as recommended.Citation30 A 6-minute walk test (6MWT) was also performed, and dyspnea was assessed using the Modified Medical Research Council (mMRC) scale. Evaluation of health-related quality of life (HRQoL) was done with St George’s respiratory questionnaire (SGRQ) total score, and anxiety and depression with Hospital Anxiety and Depression Scale (HADS) total score. Along with these, nutritional assessment, evaluation of comorbidities, and treatments were done. Evaluation of exercise capacity, dyspnea, HRQoL, anxiety, and depression were conducted at baseline and the end of the PRP.
Pulmonary rehabilitation
All the centers included in the study followed the standard-ized PRP as per the recommendations,Citation31 with variations in their modalities, including home-based, center-based, and outpatient-based programs in Nantes and center-based or outpatient-based programs in Morlaix. A further description of the PRP content is provided in the Supplementary material.
Quadriceps maximal voluntary contraction
For measurement of QMVC, an adaptation of the well-established method using a MicroFET2 dynamometer (Hoggan Scientific, Salt Lake City, UT, USA) was used.Citation19 To ensure proper measurement, the patient sat comfortably on the examination table with a high-density triangular corner cushion under the knees, in order to guarantee alignment of the femur and provide countersupport at the knees. Hip and knee were positioned at 90° flexion.Citation32 The device was fixed on the leg of the examination table with a strap to prevent any operator bias. A second strap was then used to fix the leg to the device. The point of application of force was 5 cm above the medial malleolus of the tibia. The moment of force was calculated with measurement of the lever arm between the knee-joint center and the point of application of force. As the measure of QMVC is known to have a learning effect,Citation33 a minimum of three measures was obtained for each leg. The best value obtained was then taken as the absolute value. These measurements are expressed in Newton meters.
Statistical analysis
All results are presented as means ± SD or percentages. Comparison of baseline characteristics among the three centers was done by one-way analysis of variance (ANOVA). Variables that changed significantly from baseline to the end of the PRP were identified by paired t-tests in cases of normality of distribution of values or the Wilcoxon test if not normally distributed. All statistical analyses were performed using SigmaPlot 11.0 and SPSS Statistics 19 (IBM, Armonk, NY, USA). QMVC and the 6-minute walk distance (6MWD) measurements were standardized using z-scores. A z-score gives a quantified distance from the normative data in the SD in respect to the average reference performance of the population selected, which means that z-scores help us to compare the observed value of measurement to a normal population. A z-score of −1.64 signifies that the value measured lies in the fifth percentile.
The equation used was z-score = (Observed value – Predicted value)/SD. The predicted value for QMVC was taken from Hogrel et alCitation34 and for 6MWD from Troosters et al.Citation35 Statistical significance of comparisons was set at P<0.05.
Calculation of MID
For MID estimation, distribution- and anchor-based methods were used.Citation36 The distribution-based method uses the distribution of observed values in a given sample to estimate MID. Distribution-based methods used in this study were empirical rule effect size (0.08×6×SDend–baseline) and Cohen’s effect size (0.5×SDend–baseline). The anchor-based method uses an external indicator with its known MID in the target population. In this study, the possible anchors were 6MWD, with its MID of 30 m,Citation37 and SGRQ total score, with its MID of −4 points.Citation38 For a potential anchor to be selected using this approach as per recommendations, the change from baseline must correlate with the change in QMVC with a correlation coefficient ≥0.3 and P<0.05.Citation36
Results
A total of 157 eligible individuals with COPD were included in the study from February 2014 to January 2016. The characteristics of the subjects included are given in . Comparison of baseline characteristics among the three centers is given in Table S1.
Table 1 Baseline characteristics of the patients
Responsiveness to PRP
Changes in parameters between baseline and the end of the PRP are given in . Subjects improved quadriceps force, 6MWD, and HRQoL significantly. Comparison of the intervention effect on the parameters evaluated at baseline and the end of the PRP at the three centers is given in Table S2.
Table 2 Changes in parameters measured at baseline and end of PRP
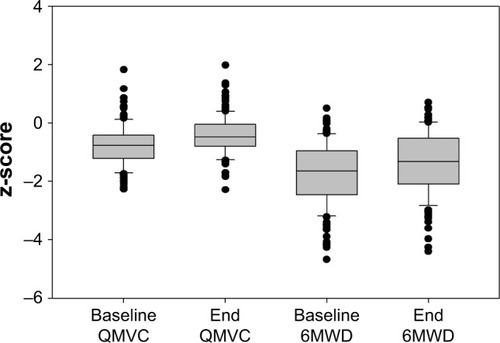
Evolution of QMVC and 6MWD z-scores
There was significant evolution in QMVC and 6MWD z-scores between baseline and the end of the PRP (−0.8±0.7 to −0.4±0.7 [P<0.001] for QMVC and −1.7±1.1 to −1.4±1.0 [P<0.001] for 6MWD; ). At the end of the PRP, subjects had improved their 6MWD, and average z-score (−1.4±1.0) was found to be within the 90th percentile.
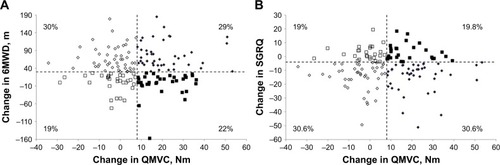
Determination of MID
Using distribution-based methods, the MID for QMVC was 7.5 Nm for empirical rule effect size and 7.8 Nm for Cohen’s effect size. The change in QMVC failed to correlate with either the change in 6MWD (r=−0.032, P=0.686) or with change in SGRQ total score (r=0.006, P=0.937). As such, no anchor could be identified in this analysis. The distribution of the subjects with the changes in 6MWD and SGRQ total scores in terms of the MID of 7.5 Nm in QMVC and MIDs of 30 m for 6MWD and −4 points for the SGRQ is given in .
Figure 2 Distribution of subjects.
Abbreviations: QMVC, quadriceps maximal voluntary contraction; 6MWD, 6-minute walk distance; MIDs, minimally important differences; SGRQ, St George’s respiratory questionnaire.
Discussion
In this study, we report the MID for QMVC in individuals with COPD undergoing a PRP. Our findings suggest 7.5 Nm to be the minimal change in QMVC attributed to the intervention of a PRP. Even though the measure of QMVC has been in place for a long time, a question remains as to what this measure actually means with regard to meaningful improvement for a patient and how the person perceives this muscular force in daily life. The diminution in muscular force with disease progression is common among individuals with COPD. Therefore, the assessment of quadriceps force seems relevant, especially if the interest is to evaluate the effect of such an intervention as a rehabilitation program. The measure of quadriceps force appears of interest along with the evaluation of daily activity in chronic diseases, as movement like getting up from a chair and moving around involves the use of quadriceps muscles. We previously found a significant correlation between changes in QMVC after a PRP and 1-minute sit-to-stand test,Citation39 which involves repeated contractions of quadriceps muscles for a longer time, requiring force and endurance capacities. Apart from activities of daily living, good quadriceps muscular force can also reduce the risk of falls in these patients. Studies have shown strong correlations between lower-limb-muscle weakness and increased fall incidence among elderly people.Citation40 In COPD, an increased risk of falls is associated with quadriceps weakness resulting from exacerbation and related hospitalization.Citation41 This further adds to the interest of QMVC measurement in COPD. The evaluation of QMVC by dynamometer in our study was performed by fixing the device with a strap to the leg of the examination table to avoid operator-influenced bias. It is important to note that the handheld method using this device is known to be influenced by the strength of the operator when applied manually.Citation42
Our study estimated the MID of QMVC in individuals with COPD. To our knowledge, this is the first study to address MID calculation for QMVC in COPD. There have been a few studies that focused on the evolution of quadriceps strength after an intervention. Nishitani et al provided evidence of an improvement in muscle strength in individuals with diabetes mellitus after cardiac rehabilitation of 6 months following coronary artery-bypass grafting.Citation20 Similarly, in individuals with CHF and COPD, evolution of quadriceps strength was compared between an exercise rehabilitation of 7 weeks and usual care. There was no difference between groups, perhaps because the exercise program included mainly endurance training, as justified by the authors.Citation21 Ber-nard et al showed a significant increase of 20% in quadriceps strength following aerobic and strength training in COPD.Citation22 Despite studies including quadriceps-strength measurement in COPD and pulmonary rehabilitation, a possible MID has been less explored. All these studies also differed in the method of evaluation of quadriceps strength. We found a preliminary report on MID for QMVC in COPD by Ques-sada et al, where the technique of measurement was not provided in detail and thus cannot be presumed to be totally comparable.Citation25
The estimation of MID in our study was done using distribution-based methods only, as the change in QMVC and the possible anchors failed to correlate. In this study, we chose the 6MWD and SGRQ as possible anchors, due to their known MID and relevance in the COPD population undergoing a PRP. QMVC expresses maximal strength of the muscle, whereas the 6MWD is an aerobic functional test. The reorganization of muscle-fiber type in COPD, as per Gosker et al,Citation43 could also result in differences in performance during these two evaluations, suggesting that they evaluate different dimensions of functional capacity. Quadriceps force has been identified as a determinant of 6MWD,Citation44 but it should be noted that our interest lies in the comparison between the change measured in each of these evaluations. The low correlation between changes in QMVC and 6MWD suggests that evolution of either of the evaluations is not correlated with the other, further confirming a difference in the dimensions that they measure. Similarly, variability in the correlation between a physical performance and QoL has previously been shown,Citation45 which could agree with our nonsignificant correlation between QMVC and SGRQ. It is however usual for MID calculation to be based on the distribution of observed scores. Similar methods have been used to calculate MIDs for exercise tests in COPD, such as the 6MWT and 6-minute stepper test.Citation46,Citation47 These statistical methods, based on distribution of values, resulted in variation in MID from 7.5 Nm to 7.8 Nm. Taking these MID ranges into account, >50% of subjects were able to improve their quadriceps force after the PRP. It should also be noted that our study focused on the minimally significant change for an improvement in QMVC and not deterioration. The interpretation of improvement and deterioration may not be likely to be similar when presented in a patient-reported outcome, which is often used in the anchor-based MID estimation. This variation could result in different MIDs for improvement and deterioration of a measure.Citation48 The MID estimation, however, in our study gives a cutoff value for improvement of quadriceps strength.
It appears important to distinguish the different MID calculations and to analyze their advantages and limits. Copay et alCitation49 listed three limitations of MID determinations: each method estimates a different MID value, MID calculation does not consider the cost of the treatment (further studies are necessary to investigate this point), and the change in patient-reported outcome depends on the baseline status of the patient. Along with these, the study had some limitations. The first is the absence of a control group. The findings of this study could have been strengthened with a control group. The second limitation is the difference in duration of the PRP among the centers. A center effect is not excluded, but probably limited here by the fact that the subjects recruited in all three centers had similar baseline characteristics, which made it possible to combine the observed values. This approach justifies the interest of a multicenter study. Although there were some differences in duration, the program content was as per the recommendations in all the centers, thus leading to similar changes observed after the PRP whatever the origin of the patients. Moreover, our results showed that all PRPs produced significant improvements, which is comparable to previous studies.Citation50,Citation51 The third limitation is the absence of follow-up data after the PRP. Further studies are required to investigate the long-term maintenance of muscle-strength improvement.
Conclusion
Assessment of QMVC using a fixed dynamometer is a simple evaluation of quadriceps muscular force and capable of assessing improvement after a PRP among COPD patients. A gain of at least 7.5 Nm represents a meaningful improvement in quadriceps force after a PRP.
Acknowledgments
The authors would like to acknowledge colleagues from the following teams who were involved in taking care of the patients in pulmonary rehabilitation and assisting with inclusion: Véronique Jean from the Pulmonary Rehabilitation Department in Saint-Jacques Hospital, University Hospital of Nantes and François Dessables from the Tourmaline Medical Center in Nantes.
Supplementary materials
Pulmonary rehabilitation
The home-based pulmonary rehabilitation program (PRP) was conducted for 12 weeks, 2 days per week, center-based PRP for 4 weeks, 3 days per week, outpatient-based PRP for 6 weeks, 3 days per week in the centers in Nantes, and center-based or outpatient PRP in Morlaix for 4 weeks, 5 days per week. The standardized PRP in all the centers included aerobic exercise on a cycle ergometer and/or treadmill with a target intensity of 60% peak work rate regarded as minimum and resistance training of the upper-and lower-limb muscles for 30–45 minutes.Citation1,Citation2 Along with these, respiratory physiotherapy, a therapeutic educational program, dietary counseling, a smoking-cessation program and sociopsychological support were also included in the PRP.
Table S1 Baseline characteristics of the patients from three centers
Table S2 Comparison of the changes in parameters measured at baseline and the end of PRP in the three centers
References
- BoltonCEBevan-SmithEFBlakeyJDBritish Thoracic Society guideline on pulmonary rehabilitation in adultsThorax201368Suppl 2ii1ii3023880483
- BernardSRibeiroFMaltaisFSaeyDPrescribing exercise training in pulmonary rehabilitation: a clinical experienceRev Port Pneumol20142029210024480488
- TroostersTGosselinkRDecramerMSix minute walking distance in healthy elderly subjectsEur Respir J199914227027410515400
Disclosure
The authors report no conflicts of interest in this work.
References
- MaltaisFDecramerMCasaburiRAn official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20141899e15e6224787074
- SeymourJMSpruitMAHopkinsonNSThe prevalence of quadriceps weakness in COPD and the relationship with disease severityEur Respir J2010361818819897554
- KharbandaSRamakrishnaAKrishnanSPrevalence of quadriceps muscle weakness in patients with COPD and its association with disease severityInt J Chron Obstruct Pulmon Dis2015101727173526366065
- ManWDSolimanMGNikoletouDNon-volitional assessment of skeletal muscle strength in patients with chronic obstructive pulmonary diseaseThorax200358866566912885979
- AgustiASorianoJBCOPD as a systemic diseaseCOPD20085213313818415812
- MarquisKDebigaréRLacasseYMidthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2002166680981312231489
- EvansRAKaplovitchEBeauchampMKIs quadriceps endurance reduced in COPD? A systematic reviewChest2015147367368425340989
- KillianKJLeblancPMartinDHSummersEJonesNLCampbellEJExercise capacity and ventilatory, circulatory, and symptom limitation in patients with chronic airflow limitationAm Rev Respir Dis199214649359401416421
- VolpatoSBianchiLLauretaniFRole of muscle mass and muscle quality in the association between diabetes and gait speedDiabetes Care20123581672167922596176
- HarringtonDAnkerSDChuaTPSkeletal muscle function and its relation to exercise tolerance in chronic heart failureJ Am Coll Cardiol1997307175817649385904
- KamiyaKMasudaTTanakaSQuadriceps strength as a predictor of mortality in coronary artery diseaseAm J Med2015128111212121926169888
- SwallowEBReyesDHopkinsonNSQuadriceps strength predicts mortality in patients with moderate to severe chronic obstructive pulmonary diseaseThorax200762211512017090575
- WalshJRMorrisNRMckeoughZJYerkovichSTParatzJDA simple clinical measure of quadriceps muscle strength identifies responders to pulmonary rehabilitationPulm Med2014201478270224672721
- MossCLWrightPTComparison of three methods of assessing muscle strength and imbalance ratios of the kneeJ Athl Train1993281555816558207
- SaeyDTroostersTMeasuring skeletal muscle strength and endurance, from bench to bedsideClin Invest Med2008315307311
- BohannonRWHand-held dynamometry: adoption 1900–2005Percept Mot Skills200610313417037637
- WhiteleyRJacobsenPPriorSSkazalskiCOttenRJohnsonACorrelation of isokinetic and novel hand-held dynamometry measures of knee flexion and extension strength testingJ Sci Med Sport201215544445022424705
- O’SheaSDTaylorNFParatzJDMeasuring muscle strength for people with chronic obstructive pulmonary disease: retest reliability of hand-held dynamometryArch Phys Med Rehabil2007881323617207672
- BohannonRWKindigJSaboGDuniAECramPIsometric knee extension force measured using a handheld dynamometer with and without belt-stabilizationPhysiother Theory Pract201228756256822191509
- NishitaniMShimadaKMasakiMEffect of cardiac rehabilitation on muscle mass, muscle strength, and exercise tolerance in diabetic patients after coronary artery bypass graftingJ Cardiol201361321622123332345
- EvansRASinghSJCollierRLokeISteinerMCMorganMDGeneric, symptom based, exercise rehabilitation: integrating patients with COPD and heart failureRespir Med2010104101473148120650624
- BernardSWhittomFLeblancPAerobic and strength training in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1999159389690110051269
- StratfordPWBinkleyJMRiddleDLGuyattGHSensitivity to change of the Roland-Morris Back Pain Questionnaire: part 1Phys Ther19987811118611969806623
- RuhdorferAWirthWEcksteinFRelationship between isometric thigh muscle strength and minimum clinically important differences in knee function in osteoarthritis: data from the osteoarthritis initiativeArthritis Care Res (Hoboken)201567450951825303012
- QuessadaANellessenAGBiscaGWMinimal important difference of quadriceps femoris muscle strength after high-intensity exercise training in patients with COPD: preliminary resultsEur Respir J201444Suppl 58P1286
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- SpruitMASinghSJGarveyCAn official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitationAm J Respir Crit Care Med20131888e13e6424127811
- MillerMRHankinsonJBrusascoVStandardisation of spirom-etryEur Respir J200526231933816055882
- WangerJClausenJLCoatesAStandardisation of the measurement of lung volumesEur Respir J200526351152216135736
- American Thoracic Society, American College of Chest PhysiciansATS/ACCP statement on cardiopulmonary exercise testingAm J Respir Crit Care Med2003167221127712524257
- SpruitMAPittaFMcauleyEZuwallackRLNiciLPulmonary rehabilitation and physical activity in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2015192892493326161676
- BachassonDVilliot-DangerEVergesSMaximal isometric voluntary quadriceps strength assessment in COPDRev Mal Respir201431876577025391511
- ReinkingMFBockrath-PuglieseKWorrellTKegerreisRLMiller-SayersKFarrJAssessment of quadriceps muscle performance by hand-held, isometric, and isokinetic dynamometry in patients with knee dysfunctionJ Orthop Sports Phys Ther19962431541598866274
- HogrelJYPayanCAOllivierGDevelopment of a French isometric strength normative database for adults using quantitative muscle testingArch Phys Med Rehabil200788101289129717908571
- TroostersTGosselinkRDecramerMSix minute walking distance in healthy elderly subjectsEur Respir J199914227027410515400
- RevickiDHaysRDCellaDSloanJRecommended methods for determining responsiveness and minimally important differences for patient-reported outcomesJ Clin Epidemiol200861210210918177782
- HollandAESpruitMATroostersTAn official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory diseaseEur Respir J20144461428144625359355
- JonesPWInterpreting thresholds for a clinically significant change in health status in asthma and COPDEur Respir J200219339840411936514
- VaidyaTde BisschopCBeaumontMIs the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPDInt J Chron Obstruct Pulmon Dis2016112609261627799759
- MorelandJDRichardsonJAGoldsmithCHClaseCMMuscle weakness and falls in older adults: a systematic review and meta-analysisJ Am Geriatr Soc20045271121112915209650
- RoigMEngJJRoadJDReidWDFalls in patients with chronic obstructive pulmonary disease: a call for further researchRespir Med200910391257126919419852
- WikholmJBBohannonRWHand-held dynamometer measurements: tester strength makes a differenceJ Orthop Sports Phys Ther199113419119818796845
- GoskerHRvan MamerenHvan DijkPJSkeletal muscle fibre-type shifting and metabolic profile in patients with chronic obstructive pulmonary diseaseEur Respir J200219461762511998989
- GosselinkRTroostersTDecramerMPeripheral muscle weakness contributes to exercise limitation in COPDAm J Respir Crit Care Med199615339769808630582
- de TorresJPPinto-PlataVIngenitoEPower of outcome measurements to detect clinically significant changes in pulmonary rehabilitation of patients with COPDChest200212141092109811948037
- PuhanMAChandraDMosenifarZThe minimal important difference of exercise tests in severe COPDEur Respir J201137478479020693247
- PichonRCouturaudFMialonPResponsiveness and minimally important difference of the 6-minute stepper test in patients with chronic obstructive pulmonary diseaseRespiration201691536737327216848
- GuyattGHOsobaDWuAWWyrwichKWNormanGRMethods to explain the clinical significance of health status measuresMayo Clin Proc200277437138311936935
- CopayAGSubachBRGlassmanSDPollyDWSchulerTCUnderstanding the minimum clinically important difference: a review of concepts and methodsSpine J20077554154617448732
- LavioletteLBourbeauJBernardSAssessing the impact of pulmonary rehabilitation on functional status in COPDThorax200863211512117901158
- MaddocksMKonSSCanavanJLPhysical frailty and pulmonary rehabilitation in COPD: a prospective cohort studyThorax2016711198899527293209