Abstract
Background
The diaphragmatic rapid shallow breathing index (D-RSBI), which is the ratio between respiratory rate (RR) and the ultrasonographic evaluation of diaphragmatic displacement (DD), is a new and promising tool to predict weaning outcome. Its accuracy in predicting weaning failure, in ready-to-wean acute exacerbation COPD (AECOPD) patients, needs to be evaluated.
Patients and methods
A prospective observational study was carried out on ready-to-wean AECOPD patients. During a T-tube spontaneous breathing trial (SBT) evaluation of the right hemidiaphragm displacement (ie, DD), M-mode ultrasonography to calculate the D-RSBI, as well as the RSBI (RR/tidal volume [VT]) were carried out simultaneously. Outcome of the weaning trial was recorded. Receiver operating characteristic (ROC) curves were used to evaluate the diagnostic accuracy of D-RSBI and RSBI.
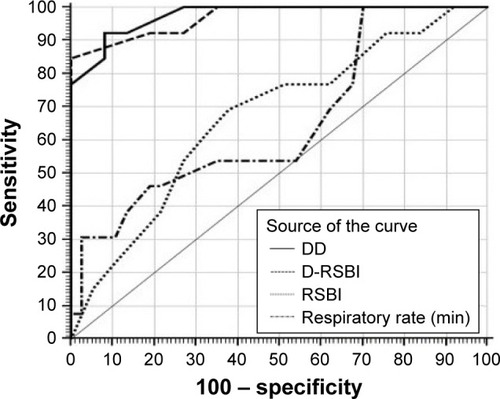
Results
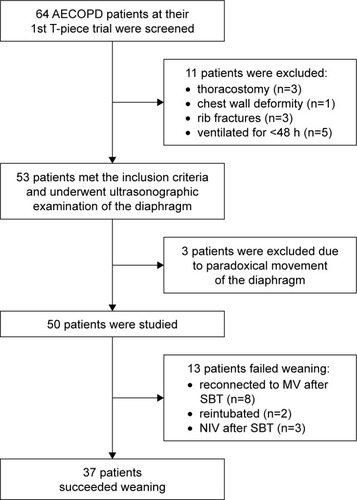
A total of 50 AECOPD patients requiring mechanical ventilation for more than 48 h who were ready to perform a SBT were included. Of these, 37 (74%) were successfully liberated from mechanical ventilation. Among the 13 patients who failed the weaning trial, 8 (62%) failed the SBT and reconnected to the ventilator, 2 (15%) were reintubated within 48 h of extubation and 3 (23%) required NIV support within 48 h of extubation. The areas under the ROC curves for D-RSBI and RSBI were 0.97 (p<0.001) and 0.67 (p<0.06), respectively.
Conclusion
D-RSBI (RR/DD) is superior to the traditional RSBI (RR/VT) in predicting weaning outcome in AECOPD patients.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Acute exacerbations of COPD (AECOPD) are a common cause of comorbidities and COPD-related mortality.Citation1–Citation3 Invasive ventilation (IV) is essential among AECOPD patients to treat acute respiratory failure. In such cases, strategies should be implemented to discontinue IV as soon as possible to avoid time-dependent complications that may arise as a result of prolonged IV.Citation4 Furthermore, extubation failure is associated with a risk of mortality, ranging from 40 to 50%.Citation5
Weaning failure is believed to be multifactorial. However, diaphragmatic dysfunction plays a major role in ventilator dependency,Citation6–Citation8 and diaphragmatic function is still poorly assessed among critically ill patients. Although useful for research purposes, direct measurements of diaphragmatic strength are invasive and need considerable expertise.Citation9 Diaphragmatic ultrasonography has recently been introduced as a non-invasive and bedside tool to measure diaphragmatic displacement (DD).Citation10,Citation11 Diaphragmatic dysfunction (defined as DD <10 mm) has been shown to be a good predictor of failure to wean from mechanical ventilation.Citation12
The rapid shallow breathing index (RSBI) (defined as the ratio of respiratory rate to tidal volume [RR/VT]) is one of the most widely used predictors of weaning outcome.Citation13 But unfortunately, it has variable sensitivity and specificity.Citation14–Citation16 So recently, Spadaro et alCitation17 introduced the diaphragmatic RSBI (D-RSBI) by substituting VT with DD in the RSBI (ie, D-RSBI = RR/DD). This avoids masking the underlying diaphragmatic dysfunction caused by the contribution of the accessory muscles in generating VT that could impair the diagnostic accuracy of the RSBI.Citation17
The aim of this study was to validate the D-RSBI as a new predictor of weaning outcome in patients with AECOPD and to compare its accuracy with that of the traditional RSBI.
Patients and methods
Patients
This prospective observational study was carried out in the Respiratory ICU of the Chest Department, Zagazig University Hospitals during the period from December 2016 to May 2017. It included all patients with AECOPD at their first spontaneous breathing trial (SBT). The exclusion criteria were 1) age <18 years; 2) presence of thoracostomy, pneumothorax or pneumomediastinum; 3) presence of rib fractures; 4) neuromuscular disease; 5) use of muscle-paralyzing agents within 48 h before the study and 6) history or new detection of paralysis or paradoxical movement of a single hemidiaphragm on diaphragmatic ultrasonography.
The study was approved by the Faculty of Medicine, Zagazig University Ethics Committee. Written informed consent was obtained from all patients.
Methods
All studied patients were subjected to the following:
A thorough medical history.
Full clinical examination (general and local examination).
Plain chest X-ray (posteroanterior or anteroposterior view according to circumstances).
Routine laboratory investigations:
complete blood picture (CBC)
liver functions
kidney functions
serum electrolytes (Na, K, Cl).
Arterial blood gases analysis (ABGs).
Diagnosis of AECOPD according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria: NHLBI/WHO (GOLD) supported by spirometric evidence of airflow obstruction (forced expiratory volume in 1 s [FEV1]/forced vital capacity [FVC] <0.70) when clinically stable; with clinical criteria of exacerbation including (increased dyspnea, increased sputum volume or sputum purulence).Citation18
Calculation of Simplified Acute Physiology Score (SAPS) IICitation19 and assessment of cough strength and amount of endotracheal secretions.Citation20
Patients intubated and mechanically ventilated for more than 48 h were considered ready for SBT (ie, spontaneous ventilation through a T-tube with the FiO2 set at the same level used during mechanical ventilation) if they met all of the following criteria: 1) clinical improvement of the underlying acute cause of respiratory failure; 2) favorable cough reflex; 3) absence of excessive and/or purulent tracheobronchial secretion; 4) stable cardiovascular status (ie, heart rate <120 beats/min; systolic blood pressure, 90–160 mmHg; and no vasopressor use); 5) stable metabolic status (ie, electrolytes and blood sugar within normal range, temperature <38°C, hemoglobin ≥8–10 g/dL); 6) adequate oxygenation (ie, arterial oxygen saturation (SaO2) >92% with inspiratory oxygen fraction (FiO2) ≤0.5 with positive end expiratory pressure (PEEP) ≤8 cmH2O) and 7) adequate pulmonary function (ie, RR ≤30 breaths/min with VT ≥5 mL/kg ideal body weight (IBW) and no significant respiratory acidosis).Citation17
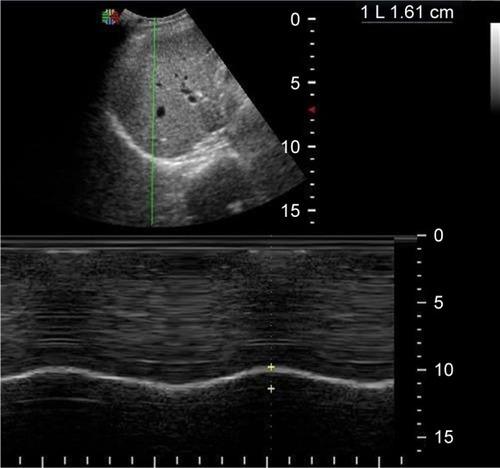
Ultrasonographic scanning of the right hemidiaphragm after 30 min. from the beginning of the SBT. The patients were lying in the semi recumbent position, with the head of the bed elevated at an angle between 30° and 45°. Diaphragmatic movement was measured using a 3.5-MHz US probe placed over one of the lower intercostal spaces in the right anterior axillary line with a SonoScape ultrasound machine (SonoScape SSI-4000, SonoScape Medical Corp., Guangdong, China; EC REP SonoScape Europ S.R.L, Rome, Italy). With the probe fixed on the chest wall during respiration, the ultrasound beam was directed to the hemidiaphragmatic dome at an angle of not less than 70°. During inspiration, the normal diaphragm contracts and moves caudally toward the transducer; this is recorded as an upward motion of the M-mode tracing. The amplitude of excursion was measured on the vertical axis of the tracing from the baseline to the point of maximum height of inspiration on the graph. Six measurements were recorded and averaged. All measurements were performed during tidal breathing at 6–12 mL/kg, excluding smaller or deeper breaths. The whole US examination was accomplished in 5 min. Negative excursion was an indicator of paradoxical diaphragmatic movement.Citation12 M-mode ultrasonography of the diaphragm of a patient with a conserved right hemidiaphragm function (DD = 16 mm) is shown in . Diaphragmatic ultrasonography was performed for all patients by two independent operators to measure the DD. All patients’ recordings were analyzed twice by both operators. All measurements were tested for intraobserver and interobserver reproducibility.
Measurement of RR and VT during the SBT using a portable spirometer (Spirotube PC Spirometer, Thor Laboratories, Budapest, Hungary). This PC spirotube has an ultrasonic respiratory sensor with automatic internal calibration.
Calculation of RSBI (RR/VT)Citation13 and D-RSBI (RR/DD).Citation17
Assessment of weaning outcome. A successful weaning trial was reported when patients were extubated and breathed spontaneously for more than 48 h. The reinstitution of mechanical ventilation during or at the end of the SBT, reintubation within 48 h or the use of non-invasive ventilation (NIV) within 48 h of extubation were reported as a failed weaning trial.
Figure 1 M-mode ultrasonography of the diaphragm of a patient with a conserved right hemidiaphragm function (DD = 16 mm).
Abbreviation: DD, diaphragmatic displacement.
Statistical analysis
In Spadaro et al’sCitation17 study, the area under receiver operating characteristic curve (AUROC) for D-RSBI was 0.89. Accordingly, assuming that the null hypothesis for AUROC was 0.5 at a power of 80%, confidence limit of 95%, and a prevalence of 39% weaning failure in COPD,Citation21 a sample size of 41 patients was considered adequate. After estimating a 10% dropout (refusal or interruption of the measurement), we choose a sample size of 45 patients.
Continuous variables were expressed as the mean ± SD, and the categorical variables were expressed as a number (percentage). Continuous variables were checked for normality by using the Shapiro–Wilk test. Independent samples Student’s t-tests were used to compare between two groups of normally distributed variables. Percent of categorical variables were compared using Pearson’s chi-square test or Fisher’s exact test as appropriate. Receiver operating characteristic (ROC) curve analysis was used to identify optimal cutoff values of DD, RSBI and DSBI with maximum sensitivity and specificity for prediction of weaning failure. The AUROC was also calculated, criteria to qualify for AUC were as follows: 0.90–1 = excellent, 0.80–0.90 = good, 0.70–0.80 = fair, 0.60–0.70 = poor and 0.50–0.60 = fail. The optimal cutoff point was established at the point of maximum accuracy. All tests were two sided. A p-value <0.05 was considered significant. All statistics were performed using SPSS 22.0 for windows (IBM Corporation, Armonk, NY, USA) and MedCalc windows (MedCalc Software bvba 13, Ostend, Belgium).
Results
The flow chart of the study is illustrated in . Initially, 64 patients were screened. A total of 53 of them met the inclusion criteria, while 11 were excluded due to thoracostomy (3 patients), chest wall deformity (1 patient), rib fractures (2 patients) and ventilation for less than 48 h (5 patients). Additionally, three more patients were excluded because of hemidiaphragm paralysis detected by paradoxical movement of the hemidiaphragm during diaphragmatic ultrasonography. So finally, 50 patients were included and analyzed. Of these, 37 (74%) were successfully liberated from mechanical ventilation. Among the 13 patients who failed the weaning trial, 8 (62%) failed the SBT and reconnected to the ventilator, 2 (15%) were reintubated within 48 h of extubation and 3 (23%) required NIV support within 48 h of extubation.
Figure 2 Flow chart of the study.
shows no statistically significant differences in preweaning parameters between weaning success and weaning failure groups as regard all demographic and clinical characteristics of the studied patients.
Table 1 Demographic and clinical characteristics of all studied patients
shows the SBT ventilatory parameters among all the studied population. RR, DD and D-RSBI differed significantly between patients who were successfully weaned and those who failed the weaning trial (p=0.03, <0.001 and <0.001, respectively).
Table 2 Spontaneous breathing trial ventilatory parameters in all studied patients
and reported the overall results of the ROC analysis regarding the available weaning predictors: D-RSBI, RSBI, DD and RR. D-RSBI showed the best diagnostic accuracy (AUROC = 0.97; p<0.001). A cutoff of D-RSBI >1.9 breaths/min/mm yielded 84.6% sensitivity, 100% specificity, 100% positive predictive value (PPV), 94.9% negative predictive value (NPV) and 96% accuracy.
Table 3 Accuracy of DD, D-RSBI, RSBI and RR in predicting weaning failure
Discussion
Mechanical ventilation is a life-saving modality of intervention that is essential for many critically ill patients, including those with AECOPD, but it is associated with a lot of complications as well as patient discomfort.Citation22 So, early safe and effective liberation of patients from mechanical ventilation remains a challenge for clinicians. It is needed, whenever the underlying condition that led to mechanical ventilation has adequately resolved and the patient can breathe spontaneously with sufficient gas exchange.Citation23
Two large weaning trials illustrated that clinicians frequently underestimate the ability of patients to breathe spontaneously when liberated from the ventilator.Citation24,Citation25 Furthermore, available weaning predictors; like the RSBI lack adequate predictive value to render them routinely used to judge the capability of patients to wean, particularly those at high risk of extubation failure including patients with hypercapnia, COPD or congestive heart failure.Citation25 Moreover, due to the complexity of the derangement of the mechanical properties of the respiratory system, COPD patients probably need different weaning indices or different threshold values compared to a general ICU population.Citation26
Results of this study confirm the superiority of the diaphragmatic-RSBI (D-RSBI), a new index first adopted by Spadaro and coworkers,Citation17 over the traditional RSBI in predicting weaning outcome; even in patients with AECOPD who are at increased risk of extubation failure.
The present work supports the evidence that substitution of VT with DD in calculating RSBI could represent an accurate weaning predictor in a special population of ICU patients, ie, COPD patients with acute exacerbation.
Weaning failure is multifactorial. So, an accurate predictive tool should reflect all pathophysiological determinants of failure, including increased mechanical workload applied on the respiratory muscles, diaphragmatic dysfunction, weaning-induced cardiac failure and a reduced ability to clear secretions and to maintain open airways. Most of the above-mentioned pathways lead to rapid shallow breathing. Hence, Yang and TobinCitation13 developed the RSBI which quantitates the extent of rapid shallow breathing taking into account the ratio between RR and VT.
In contrast, patients who failed the weaning attempt in this study had a lower RSBI (76.15±13.10 breaths/min/L) than the cutoff value of 105 to predict weaning failure originally described by Yang and Tobin.Citation13 Also, several other studies have documented a wide range of predictive values for RSBI, which could reflect differences in methodology, classification of outcomes, and study populations.Citation27,Citation28
The present study found that the D-RSBI was significantly higher in COPD patients who failed SBT compared to those who succeeded to wean (3.27±0.84 versus 1.43±0.32, respectively), while the traditional RSBI was not significantly different between the two studied groups (p=0.082). Also, the D-RSBI predicted weaning failure accurately at a threshold value more than 1.9 (AUROC=0.97, p<0.001). Although, the cutoff value for the D-RSBI reported by Spadaro and his colleaguesCitation17 was lower (ie, >1.3) than this study. This could be explained by the difference in the study population, as the present work included only COPD patients who usually show a lower degree of diaphragmatic excursion.Citation29
The D-RSBI was speculated to be more accurate than the RSBI because DD reflects more closely the diaphragmatic function as compared to VT. In the presence of diaphragmatic dysfunction, the diaphragm movement is depressed and the accessory muscles of inspiration assume a greater role in generating VT, but for a limited period of time as they are less efficient and easily fatigable.Citation28,Citation30 In these situations, the VT is less linked to the function of the diaphragm than DD, which reflects the ability of the diaphragm to generate inspiratory volume.Citation31
Ultrasound examination of the diaphragm is a non-invasive, easy to do and bedside tool that does not require patient collaboration.Citation10,Citation32,Citation33 Diaphragmatic M-mode ultrasonography has been recently applied to measure the amount of diaphragmatic excursion (ie, DD) during either spontaneous or assisted breathing.Citation11,Citation12,Citation34 Herein, the DD was significantly higher in the successfully weaned than in the failed to wean COPD patients. Furthermore, the diagnostic accuracy of DD was superior to that of RSBI but still lower than that of the D-RSBI. These results confirm the superiority of D-RSBI in assessing both diaphragmatic function and prediction of extubation outcome.
Finally, many experts consider that clinical judgment, based upon careful inspection, is superior to and more accurate than available predictors of weaning outcome.Citation24–Citation26 However, integrating this clinical judgment with a relatively easy to do bedside index like the D-RSBI may at least help intensivists in their decision to extubate.Citation17
Regarding limitations of the current work. First, the reported cutoff value of D-RSBI in the studied COPD patients cannot be generalized to all ICU population and future studies should be done to confirm the validity of the D-RSBI in predicting the weaning outcome in different clinical situations. Second, one can say that ultrasonography is an operator dependent and measurements of DD might change between operators, but in the current work, interobserver and intraobserver reproducibility were tested.
Conclusion
D-RSBI (RR/DD) is a new and promising tool that is superior to the traditional RSBI (RR/VT) in predicting weaning outcome in COPD patients with acute exacerbation.
Author contributions
AA and SE were responsible for the study design. AA and MW were responsible for patient selection, data collection and performing diaphragmatic ultrasonography for all selected patients according to the adopted protocol.
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We wish to thank all the medical staff on the respiratory ICU, Zagazig University, Egypt.
Disclosure
The authors report no conflicts of interest in this work.
References
- HigginsMWThomTIncidence, prevalence and mortality: intra- and inter-country differenceHensleyMJSaundersNAClinical Epidemiology of Chronic Obstructive Pulmonary DiseaseNew YorkMarcel Dekker19902343
- ConnorsAFJrDawsonNVThomasCOutcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment)Am J Respir Crit Care Med19961544 Pt 19599678887592
- FusoLIncalziRAPistelliRPredicting mortality of patients hospitalized for acutely exacerbated chronic obstructive pulmonary diseaseAm J Med19959832722777872344
- SongYChenRZhanQThe optimum timing to wean invasive ventilation for patients with AECOPD or COPD with pulmonary infectionInt J Chron Obstruct Pulmon Dis20161153554227042042
- ThilleAWHarroisASchortgenFBrun-BuissonCBrochardLOutcomes of extubation failure in medical intensive care unit patientsCrit Care Med201139122612261821765357
- McCoolFDTzelepisGEDysfunction of the diaphragmN Engl J Med20123661093294222397655
- JaberSPetrofBJJungBRapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humansAm J Respir Crit Care Med2011183336437120813887
- HermansGAgtenATestelmansDDecramerMGayan-RamirezGIncreased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational studyCrit Care2010144R12720594319
- DoorduinJvan HeesHWvan der HoevenJGHeunksLMMonitoring of the respiratory muscles in the critically illAm J Respir Crit Care Med20131871202723103733
- MatamisDSoilemeziETsagouriasMSonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applicationsIntensive Care Med201339580181023344830
- BoussugesAGoleYBlancPDiaphragmatic motion studied by M-mode ultrasonographyChest2009135239140019017880
- KimWYSuhHJHongSBKohYLimCMDiaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilationCrit Care Med201139122627263021705883
- YangKLTobinMJA prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilationN Engl J Med199132421144514502023603
- LeeKHHuiKPChanTBTanWCLimTKRapid shallow breathing (frequency tidal volume ratio) did not predict extubation outcomeChest199410525405438306759
- SaviATeixeiraCSilvaJMfor the Gaúcho Weaning Study GroupWeaning predictors do not predict extubation failure in simple-to-wean patientsJ Crit Care2012272221.e1e8
- HuangCTYuCJConventional weaning parameters do not predict extubation outcome in intubated subjects requiring prolonged mechanical ventilationRespir Care20135881307131423307826
- SpadaroSGrassoSMauriTCan diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing indexCrit Care201620130527677861
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) for the diagnosis, management strategy and prevention of chronic obstructive lung disease (updated 2016) [homepage on the Internet] Available at: http://www.goldcopd.comAccessed December 18, 2016
- Le GallJRLemeshowSSaulnierFA new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter studyJAMA199327024295729638254858
- KhamieesMRajuPDeGirolamoAAmoateng-AdjepongYManthousCAPredictors of extubation outcome in patients who have successfully completed a spontaneous breathing trialChest200112041262127011591570
- Abu YoussefHAShalabyAEOAbd El HafizAMShabanMMHamedHAGPredictive value of rapid shallow breathing index in relation to the weaning outcome in ICU patientsEgypt J Chest Dis Tuberculosis2016652465472
- SchmidtGAGirardTDKressJPLiberation from mechanical ventilation in critically ill adults. Executive Summary of an Official American College of Chest Physicians/American Thoracic Society Clinical Practice GuidelineChest2017151116016527818329
- OuelletteDRPatelSGirardTDLiberation from mechanical ventilation in critically ill adults: an Official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline. Inspiratory pressure augmentation during spontaneous breathing trials, protocols minimizing sedation, and noninvasive ventilation immediately after extubationChest2017151116618027818331
- BrochardLRaussABenitoSComparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilationAm J Respir Crit Care Med199415048969037921460
- EstebanAFrutosFTobinMJA comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative GroupN Engl J Med199533263453507823995
- AlvisiRVoltaCARighiniERPredictors of weaning outcome in chronic obstructive pulmonary disease patientsEur Respir J200015465666210780755
- VallverduICalafNSubiranaMNetABenitoSManceboJClinical characteristics, respiratory functional parameters, and outcome of a two hour T-piece trial in patients weaning from mechanical ventilationAm J Respir Crit Care Med19981586185518629847278
- YanSLichrosIZakynthinosSMacklemPTEffect of diaphragmatic fatigue on control of respiratory muscles and ventilation during CO2 rebreathingJ Appl Physiol1993753136413708226552
- UnalOArslanHUzunKOzbayBSakaryaMEEvaluation of diaphragmatic movement with MR fluoroscopy in chronic obstructive pulmonary diseaseClin Imaging200024634735011368935
- YanSSliwinskiPGauthierAPLichrosIZakynthinosSMacklemPTEffect of global inspiratory muscle fatigue on ventilatory and respiratory muscle responses to CO2J Appl Physiol1993753137113778226553
- UmbrelloMFormentiPLonghiDDiaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical studyCrit Care20151916125886857
- GoligherECLaghiFDetskyMEMeasuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validityIntensive Care Med201541464264925693448
- TestaASoldatiGGiannuzziRBerardiSPortaleGGentiloni SilveriNUltrasound M-mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjectsUltrasound Med Biol2011371445221144957
- DemouleAJungBProdanovicHDiaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact—a prospective studyAm J Respir Crit Care Med2013188221321923641946