Abstract
Rationale
Readmissions are common following acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and are partially responsible for increased morbidity and mortality in COPD. Numerous factors have been shown to predict readmission of patients previously admitted to hospital for AECOPD; however, factors related to readmission in patients who are triaged in emergency departments (EDs) and sent directly home are poorly understood. We postulate that patients seen in the ED for AECOPD and directly sent home have a high readmission rate, and we suspect that inadequate management and follow-up contribute to this high readmission rate.
Methods
We conducted a 1-year retrospective study of all patients seen in the ED for AECOPD at an inner-city tertiary care hospital; 30- and 90-day readmission rates for COPD and all-cause admissions to the ED and hospital were determined. Patients discharged directly home from the ED were compared with those admitted to hospital for management. Patient, treatment, and system variables that could potentially impact readmission were documented. Multivariate Poisson regression models were used to determine which factors predicted readmissions.
Results
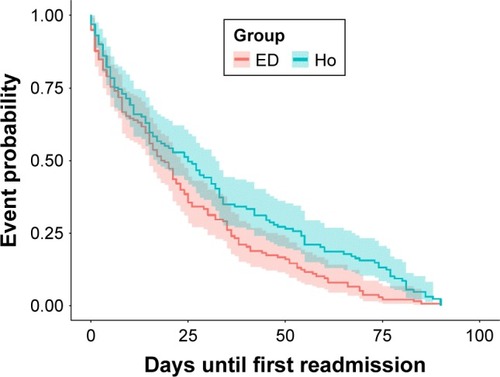
The readmission rates in the ED group (n=240) were significantly higher than that in the hospitalized group (n=271): 1) the 90-day ED readmissions (1.29 vs 0.51, p<0.0001) and 30-day ED readmissions (0.54 vs 0.20, p<0.0001) (ED vs hospitalized groups) were significantly higher in the ED group; 2) the time to first readmission was significantly shorter in the ED group than in the hospitalized group (24.1±22 vs 31.8±27.8 days; p<0.05). Cardiovascular comorbidities (p<0.00001), substance abuse disorder (p<0.001), and mental illness (p<0.001) were the strongest predictors of readmission in the ED group. Age (p<0.01), forced expiratory volume in 1 second (p<0.001), and cardiovascular comorbidities (p<0.05) were the best predictors for both 30- and 90-day COPD readmission rates in the ED group. Only 50% of the ED group patients received bronchodilators, oral steroids, and antibiotics inclusively, and only 68% were referred for community follow-up. The need for oral steroids to treat AECOPD predicted future 90-day COPD readmissions in the ED group (p<0.003).
Conclusion
Patients discharged directly home from EDs have a significantly higher risk of readmission to EDs than those who are hospitalized. One possible reason for this is that COPD management is variable in EDs with <50% receiving appropriate therapy.
Introduction
Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) is defined as an acute worsening of respiratory symptoms beyond baseline level including dyspnea, cough, and sputum production that require a change in medication in mild cases and emergency department (ED) visits or hospitalization in more severe cases.Citation1 AECOPD is associated with an increased morbidity and mortality in COPD patients with an increased frequency of exacerbation leading to higher mortality,Citation2 lower quality of life,Citation3 an accelerated decline in lung function,Citation4 and future adverse events.Citation5 In the period up to 3 months following an acute exacerbation, there is a higher risk for subsequent exacerbations,Citation6 mortality,Citation7 and indication that even then some patients do not have full recovery in lung function.Citation8 Furthermore, there are high health care costsCitation9 for COPD exacerbations with acute care and ED readmissions contributing the largest amount of readmissions in Canada.Citation10
The importance of AECOPD management has been emphasized due to the adverse effect on patient outcome and the burden to the health care system these events have. Therefore, the goal of AECOPD treatment is to minimize the impact of the exacerbation in order to reduce the frequency of future events.Citation1 Thus, many studies have looked at the factors that are associated with exacerbation frequency to find which can be modifiable. Certain disease factors (severity of disease [forced expiratory volume in 1 second {FEV1}],Citation11,Citation12,Citation19,Citation20 exacerbation history,Citation12,Citation14,Citation15,Citation18,Citation19 comorbidities,Citation11,Citation15,Citation16,Citation18,Citation20 body mass index,Citation13 previous surgeries,Citation13 long-term oxygen therapyCitation14), social factors (smoking,Citation12,Citation19 drug addiction, living without a partner/spouse,Citation11 quality of life,Citation12,Citation14 socioeconomic statusCitation13,Citation16,Citation17), patient factors (age,Citation12,Citation15 physical activity,Citation14 compliance with treatmentCitation20), and management factors (intervention programs, treatmentCitation13,Citation14,Citation21,Citation22) have previously been shown to predict exacerbations and readmission of patients admitted to the hospital for AECOPD. Decision support algorithms incorporating the above-mentioned variables have been reported to assist physicians to determine whether hospital admission or ED management and observation with discharge home from the ED in AECOPD are appropriate.Citation23–Citation26 However, the adoption and utility of these tools are unclear and are complicated for practical use in a busy ED, and decisions to admit patients with COPD are often and mostly based on clinical judgment of the attending physician. Numerous factors have been associated with readmissions following AECOPD;Citation12–Citation22 however, readmission rates in patients seen in the ED for AECOPD and directly sent home are understudied, particularly the factors that predict readmissions in this population.
Approximately half of the patients seen in the ED for AECOPD are hospitalized. Of concern, adherence to guidelines for AECOPD management in the ED is typically low in the USA and Canada.Citation27 Previous studies have examined the factors that predict relapse, admission frequency, poor outcomes, and hospital admission after an ED visit for AECOPD, few have specifically looked at patients who were directly sent home, and none looked at readmissions up to 90 days or compared the patient group treated just in the ED with those who are hospitalized.Citation28–Citation36 We hypothesize that readmission rates are higher in patients with AECOPD discharged directly from the ED compared with patients managed in the hospital.
This study was designed to compare the readmission rates and patient population demographics of patients visiting the ED for AECOPD and discharged directly from the ED, to patients visiting the ED and who are then hospitalized for AECOPD. We were also interested to determine the factors that predict readmission of the patients directly discharged from the ED with the primary diagnosis of AECOPD. The primary outcome measure was the total all-cause and COPD-related readmissions at 30 and 90 days post-index visit/admission for COPD. The secondary outcomes were patient factors (disease and social factors) and system factors (ED management) or variables associated with readmission.
Methods
Patient population
This was a 1-year (March 2012 to March 2013) retrospective study of all patients who were seen and managed in an inner-city tertiary hospital for AECOPD (St Paul’s Hospital, Vancouver, Canada). All patients were seen and managed in the ED and either directly sent home after stabilization or admitted to hospital for further management. The attending physician made the diagnosis of AECOPD based on clinical acumen. To be included in this analysis, the principal diagnosis of the ED visit had to be AECOPD. The index admission in both the groups was defined as the first admission for AECOPD (to ED in ED group and to hospital in hospitalized group) after the set start date.
Study design
Patient data were retrospectively collected by using patient charts and hospital’s electronic databases (that include dictations, laboratory records, radiology reports, and lung function reports). To ensure that readmissions to other hospitals or deaths were not missed, a provincial-wide electronic database was used to cross-check the data (patients who were documented as “not resident” to the area were excluded from analysis). All patients were assigned a unique study number, and all research-related information collected was attached to this number to protect patient confidentiality. No personal information that could identify a patient has been or will be used in presentations or publications. All information and data collected were kept secure, and only the principal investigator or his/her designate had access to personal information or any information that could potentially identify the patients. Ethics approval for this retrospective chart review study was obtained from the University of British Columbia and Providence Health Care Research Institute Research Ethics Board. No personal consent from the patients included in the study was obtained or required by the ethics board.
The management of the AECOPD was done by the attending physician (emergency physician in the ED group and either general internist or respirologist in the hospitalized group). The in-hospital management of AECOPD in all patients was guided by a standardized hospital-wide admission protocol for the management of AECOPD based on the GOLD strategic document.Citation1 The AECOPD in the ED group was managed by the attending emergency physician. As there is no standardized protocol for ED management of AECOPD, specific data regarding patient assessment (investigations such as imaging, laboratory tests, and other diagnostics), patient treatment (medication given and prescribed on discharge), and patient follow-up (referrals for further testing and interventions such as pulmonary rehabilitation or follow-up by the patient’s family physician or respirologist) were collected.
Outcomes
The primary outcomes were both 30 and 90 days post-ED index and hospitalized index admission and were determined for all-cause and COPD readmissions.
Secondary outcomes were factors that predict ED read-missions after discharge from the ED for AECOPD.
Data analysis
All analyses were performed by using RStudio (Version 1.0.153 © 2009–2017; RStudio, Inc., https://www.rstudio.com/). Tests employed were two-tailed and p-values <0.05 were considered significant. Statistical tests to compare the demographics of the ED index admission and the hospitalized index admission groups were chosen depending on whether the variable was continuous or proportional and whether the data were normally distributed. Continuous variables were first tested for normality using the Shapiro–Wilk test and if not normally distributed, the Wilcoxon ranked-sum test (also called Mann–Whitney U test) was used to determine whether means were significantly different between the two groups. For proportional variables, the chi-squared tests were used to determine whether the index admission group was associated with a variable. The Yates’ correction for continuity was not applied as sample sizes were large and there were no expected frequencies less than five. Readmission rates and average time until first readmission between the ED group and hospitalized group were compared again using the Wilcoxon ranked-sum test.
Multivariate Poisson regression models were used to determine the factors that predict readmissions of patients seen in the ED for AECOPD. RStudio was used to run automated stepwise regressions, which uses lowest Akaike information criterion to determine the best model by using both forward selection and backward elimination approaches. Two types of models were created; one for patient factors and one for system factors that relate to both 30- and 90-day all-cause or COPD admissions. The regression coefficient (β) was converted to an incidence rate ratio (IRR) (X=eβ), implicating the change in the rate at which events occur with one unit change in the predictor variable.
Results
Demographics
Eligibility criteria were met for 240 patients in the ED index admission group and for 271 patients in the hospital index admission group. The demographic comparison between the two groups is shown in . The ED index admission group compared with the hospitalized index admission group was significantly younger by about 10 years (p<0.001), with milder COPD severity (as indicated by higher FEV1; p=0.001). There were 26% more current smokers (p<0.001), 13% more ever smokers (p=0.001), and 30% more substance abusers (p<0.001) in the ED group versus hospital group. Furthermore, the ED group had a higher mean number of comorbidities (p<0.001) and had 20% more mental health comorbidities (p<0.001) than the hospitalized group. The ED group had a high proportion of patients living without a partner (88.8%) and high prevalence of cardiovascular comorbidity (43.8%).
Table 1 Demographic data
Readmissions of ED versus hospitalized patients (primary outcome)
Readmission rates of the two groups are shown in . The 90-day ED readmissions (1.29 vs 0.51, p<0.001) and 30-day ED readmissions (0.54 vs 0.20, p<0.001) were significantly higher in the ED group. The 30- and 90-day hospital readmissions were not significantly different between the two groups. In the ED group, 31% of the 90-day readmissions were COPD related and 33% of the 30-day readmissions were COPD related. Time to the first all-cause readmission was significantly shorter in the ED group compared with the hospitalized group (24.21 vs 31.85 days, p<0.01) ().
Table 2 Readmission rates between ED- and hospital-managed AECOPD
Factors predicting readmissions in ED-managed patients (secondary outcome)
Mental health and cardiovascular comorbidities were the strongest variables associated with both 30- and 90-day read-missions in the ED group (). Thirty-day readmissions were associated with younger age (IRR =0.98, p<0.01), lack of a partner/spouse (IRR =0.37, p=0.010 or p<0.01), mental illness (IRR =1.76, p<0.01), cardiovascular comorbidities (IRR =1.42, p<0.05), and an increase in total number of comorbidities (IRR =1.05, p<0.05) (). Ninety-day readmission rates were associated with substance abuse disorder (IRR =1.53, p<0.001), mental illness (IRR =1.53, p<0.001), cardiovascular comorbidities (IRR =1.62, p<0.001), and the number of comorbidities (IRR =1.09, p<0.001). Patients who had stopped smoking (past smokers) had 52% lower risk of all-cause readmissions (p<0.001). summarizes the risk factors associated with COPD-specific admissions. Factors with the strongest association with COPD readmissions in the ED-managed group were younger age, cardiovascular comorbidities, and FEV1.
Table 3 Factors predicting all-cause readmission in the ED group
Table 4 Factors predicting COPD readmission in ED-managed patients
ED management
shows the ED management of AECOPD, demonstrating both the investigation conducted to exclude other potential causes for the patients’ symptoms and the treatment provided. Chest X-ray was requested in the majority of patients (92.9%), 55.8% of patients had workup for potential cardiovascular causes for dyspnea, and 74.1% had an infectious workup. Only 49.1% received bronchodilators, antibiotics, and steroids inclusively, and 68% of patients were referred for additional follow-up by their family physician, respirologist, or respiratory therapist for puffer training or pulmonary rehabilitation.
Table 5 ED management (investigations and treatment) of AECOPD
Interestingly, the emergency physicians’ decision to conduct an infectious workup (IRR =1.34, p<0.05) was associated with an increase in the 90-day readmission rate and a cardiovascular workup with a 90-day (IRR =1.34, p<0.01) and 30-day (IRR =1.39, p<0.05) all-cause readmission rate. Receiving bronchodilators was associated with a 47% (p<0.001) 90-day and 36% (p<0.001) 30-day reduction in all-cause readmissions. Thirty-(IRR =1.93, p<0.05) and 90-day (IRR =1.93, p<0.007) COPD readmissions were associated with the need to do a cardiovascular workup. The need to use systemic steroids was associated with an increase in 90-day COPD-related readmissions (IRR =2.13, p<0.001).
Discussion
AECOPDs are a major source of ED visits in North America and are associated with substantial morbidity and mortality.Citation5 Many patients with AECOPD return for a repeated ED visit following discharge.Citation6 In the present study, we showed that on average patients experience another 0.7 admissions to the ED within 30 days and 1.7 admissions within 90 days of discharge from the index ED visit. Interestingly, these rates are significantly higher than those experienced by patients who are hospitalized for their AECOPD and are subsequently discharged home although ED-discharged patients were significantly younger and had better lung function than those discharged from hospital wards.
Although the exact reasons for the higher rates of readmissions in the ED-discharged patients are not fully known, there were several important observations in our study that deserve emphasis. First, the ED-discharged patients were more likely to be current smokers and have more comorbidities (and especially substance abuse disorders and mental illnesses). Substance abuse disorder has been identified as a strong predictor for readmission following hospitalization.Citation22 Comorbidities are common in COPD patients and adversely impact disease outcome because of many sharing risk factors and compounding effects on disease severity.Citation37,Citation38 Cardiovascular comorbidities were present in 44% of the patients in the ED group. Cardiovascular comorbidities have been shown to be important in COPD patients because of their prevalence and negative effects on patient outcomes.Citation39–Citation45 In particular, in terms of AECOPD, underlying cardiovascular diseases are associated with a higher risk for exacerbation.Citation46,Citation47 In addition, cardiovascular events are often triggered by AECOPD (heart failure, myocardial damage, and arrhythmia such as atrial fibrillation).Citation48–Citation53 This combination tends to make exacerbations more severe/complicated and raises the need for hospitalization,Citation52,Citation54,Citation55 resulting in lengthened recovery timesCitation56,Citation57 and increased mortality.Citation45,Citation58 Acute exacerbation of COPD may also trigger acute coronary syndrome, myocardial infarction (heart attack), stroke, and sudden cardiac death.Citation57,Citation58 The strong association of underlying cardiovascular comorbidities in our ED group and its association with increased readmission rates suggest that ED management of AECOPD should always include a workup for potential associated cardiovascular events.
Second, adherence to national and international guidelines for managing AECOPD in the ED was relatively low in the present study, consistent with another study in the USA and Canada.Citation27 We found that while nearly 90% of ED patients were treated with bronchodilators, 63% with antibiotics, and 71% with a course of steroids for their AECOPD in the ED and/or prescribed to complete at home, only 49.1% received all three treatment modalities. This relative under-treatment of AECOPD may contribute to the high recurrence and readmissions rates. Interestingly, if the emergency physician deems it necessary to do a workup for potential underlying infection (complete blood count, C-reactive protein, and blood or sputum cultures) or a cardiovascular reason for dyspnea (electrocardiogram, troponin, and brain natriuretic protein), these interventions predict future readmissions. ED management analysis suggests that the patients with comorbidities (predominantly cardiovascular) and more severe COPD were correctly identified in the ED and given appropriate tests and treatment. Yet the higher readmission rates among these patients indicate that the management plan was not sufficient to prevent future exacerbations or readmissions. Better follow-up and community support are needed to monitor treatment, to do counseling on smoking cessation, to provide action plans and puffer training, and to address other factors such as substance abuse.Citation22 Interestingly, the use of bronchodilators in the ED and at home was strongly associated with fewer readmissions (all-cause and COPD readmissions), underlying recent studies that showed the importance of proper use of bronchodilators, specifically long-acting bronchodilators in reducing AECOPD.Citation1 The need for systemic steroids to treat AECOPD also predicts future COPD readmissions, and we suspect that the need for steroids may be just a surrogate marker for the severity of AECOPD.
There were several notable limitations in this study. Our study population is from the inner city with a large fraction of the study patients of low socioeconomic status with high prevalence of substance abuse and mental illness (more so in the ED group); therefore, the results of the study are limited in their generalizability to the wider COPD population. Since this is a retrospective study, not all variables were available for all patients. Furthermore, the ED management of AECOPD is currently not protocolized with inconsistent documentation in the discharge summary as to whether all patients received a COPD action plan or whether current smokers received smoking cessation counseling.
Conclusion
We conclude that patients managed in the ED for AECOPD and discharged directly home have a higher 30- and 90-day readmission rate than patients admitted for in-hospital management. Factors that contribute to this higher readmission rate are underlying cardiovascular disease, mental illness, and substance abuse disorder. We also identify weaknesses in the management of the patients in the ED, specifically as only 50% were given bronchodilators, steroids, and antibiotics inclusively. Other important interventions such as smoking cessation counseling, providing an action plan and referral to appropriate follow-up services such as pulmonary rehabilitation, or a respiratory specialist, were lacking. We postulate that a protocolized management plan for AECOPD in the busy ED could reduce short-term readmissions.
Disclosure
Doctor SF van Eeden is the GlaxoSmithKline-Canadian Institutes of Health Research Professor in COPD. The authors report no other conflicts of interest in this work.
References
- VogelmeierCFCrinerGJMartinezFJGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2017 report: GOLD executive summaryAm J Respir Crit Care Med2017195555758228128970
- Soler-CatalunaJJMartinez-GarciaMARoman SanchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- SeemungalTADonaldsonGCPaulEABestallJCJeffriesDJWedzichaJAEffect of exacerbation on quality of life in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med19981575 Pt 1141814229603117
- MakrisDMoschandreasJDamianakiAExacerbations and lung function decline in COPD: new insights in current and ex-smokersRespir Med200710161305131217112715
- HurstJRVestboJAnzuetoASusceptibility to Exacerbation in Chronic Obstructive Pulmonary DiseaseN Engl J Med2010363121128113820843247
- HurstJRDonaldsonGCQuintJKGoldringJJBaghai-RavaryRWedzichaJATemporal clustering of exacerbations in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2009179536937419074596
- SuissaSDell’AnielloSErnstPLong-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortalityThorax2012671195796322684094
- SeemungalTADonaldsonGCBhowmikAJeffriesDJWedzichaJATime course and recovery of exacerbations in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200016151608161310806163
- MittmannNKuramotoLSeungSJHaddonJMBradley-KennedyCFitzgeraldJMThe cost of moderate and severe COPD exacerbations to the Canadian healthcare systemRespir Med2008102341342118086519
- Discharge Abstract Database, Canadian Institute for Health Information, Fichier des hospitalisations MED-ÉCHO, ministère de la Santé et des Services sociaux du QuébecAll-Cause Readmission to Acute Care and Return to the Emergency RoomOttawa, ONCanadian Institute for Health Information2012
- WongAWMGanWQBurnsJSinDDvan EedenSFAcute exacerbation of chronic obstructive pulmonary disease: influence of social factors in determining length of hospital stay and readmission ratesCan Respir J200815736136418949105
- GuerraBGaveikaiteVBianchiCPuhanMAPrediction models for exacerbations in patients with COPDEur Respir Rev20172614316006128096287
- AmalakuhanBKiljanekLParvathaneniAHesterMCheriyathPFischmanDA prediction model for COPD readmissions: catching up, catching our breath, and improving a national problemJ Community Hosp Intern Med Perspect20122110
- BahadoriKFitzGeraldJMRisk factors of hospitalization and readmission of patients with COPD exacerbation – systematic reviewInt J Chron Obstruct Pulmon Dis20072324125118229562
- SantibáñezMGarrastazuRRuiz-NuñezMPredictors of hospitalized exacerbations and mortality in chronic obstructive pulmonary diseasePLoS One2016116e015872727362765
- CoventryPAGemmellIToddCJPsychosocial risk factors for hospital readmission in COPD patients on early discharge services: a cohort studyBMC Pulm Med2011114922054636
- ChanFWKWongFYYYamCHKRisk factors of hospitalization and readmission of patients with COPD in Hong Kong population: Analysis of hospital admission recordsBMC Health Serv Res20111118621831287
- MüllerováHShuklaAHawkinsARisk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort studyBMJ Open2014412e006171
- Montserrat-CapdevilaJGodoyPMarsalJRBarbéFGalvánLRisk factors for exacerbation in chronic obstructive pulmonary disease: a prospective studyInt J Tuberc Lung Dis201620338939527046722
- AlexopoulosECMalliFMitsikiEBaniaEGVarounisCGourgoulianisKIFrequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study)Int J Chron Obstruct Pulmon Dis2015102665267426715845
- LemmensKMNieboerAPHuijsmanRA systematic review of integrated use of disease-management interventions in asthma and COPDRespir Med2009103567069119155168
- AdamsonSLBurnsJCampPGSinDDvan EedenSFImpact of individualized care on readmissions after a hospitalization for acute exacerbation of COPDInt J Chron Obstruct Pulmon Dis201611617126792986
- Garcia-GutierrezSQuintanaJMBarrioIIRYSS-COPD Appropriateness Study (IRYSS-CAS) GroupApplication of appropriateness criteria for hospitalization in COPD exacerbationIntern Emerg Med20138434935723508735
- RezaeeMEWardCENuanezBRezaeeDADitkoffJHalalauAExamining 30-day COPD readmissions through the emergency departmentInt J Chron Obstruct Pulmon Dis20171310912029343950
- Garcia-GutierrezSQuintanaJMBilbaoAIRYSS-COPD Appropriateness Study (IRYSS-COPD) GroupValidity of criteria for hospital admission in exacerbations of COPDInt J Clin Pract201468782082925077290
- LippmannSJYeattsKBWallerAEHospitalizations and return visits after chronic obstructive pulmonary disease ED visitsAm J Emerg Med20133191393139623910071
- CydulkaRKRoweBHClarkSEmermanCLCamargoCAJrMARC Investigators. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease in the elderly: the Multicenter Airway Research CollaborationJ Am Geriatr Soc200351790891612834509
- KimSEmermanCLCydulkaRKRoweBHClarkSCamargoCAMARC InvestigatorsProspective multicenter study of relapse following emergency department treatment of COPD exacerbationChest2004125247348114769727
- RoweBHVilla-RoelCGuttmanAPredictors of hospital admission for chronic obstructive pulmonary disease exacerbations in Canadian emergency departmentsAcad Emerg Med200916431632419298621
- HasegawaKTsugawaYTsaiCLBrownDFCamargoCAJrFrequent utilization of the emergency department for acute exacerbation of chronic obstructive pulmonary diseaseRespir Res2014154024717062
- RocheNZureikMSoussanDNeukirchFPerrotinDThe Urgence BPCO (COPD Emergency) Scientific Committee and InvestigatorsPredictors of outcomes in COPD exacerbation cases presenting to the emergency departmentEur Respir J200832495396118508819
- AaronSDVandemheenKLHebertPOutpatient oral prednisone after emergency treatment of chronic obstructive pulmonary diseaseN Engl J Med2003348262618262512826636
- LauACYamLYPoonEHospital re-admission in patients with acute exacerbation of chronic obstructive pulmonary diseaseRespir Med2001951187688411716201
- MurataGHGorbyMSKapsnerCOChickTWHalperinAKA multivariate model for the prediction of relapse after outpatient treatment of decompensated chronic obstructive pulmonary diseaseArch Intern Med1992152173771728932
- DahlénIJansonCAnxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary diseaseChest200212251633163712426264
- StehrDEKleinBJMurataGHEmergency department return visits in chronic obstructive pulmonary disease: the importance of psychosocial factorsAnn Emerg Med19912010111311161928884
- FabbriLMLuppiFBeghéBRabeKFComplex chronic comorbidities of COPDEur Respir J200831120421218166598
- SorianoJBVisickGTMuellerovaHPayvandiNHansellALPatterns of comorbidities in newly diagnosed COPD and asthma in primary careChest200512842099210716236861
- MüllerovaHAgustiAErqouSMapelDWCardiovascular comorbidity in COPD: systematic literature reviewChest201314441163117823722528
- MascarenhasJLourençoPLopesRAzevedoABettencourtPChronic obstructive pulmonary disease in heart failure. Prevalence, therapeutic and prognostic implicationsAm Heart J2008155352152518294490
- BhattSPDransfieldMTChronic obstructive pulmonary disease and cardiovascular diseaseTransl Res2013162423725123727296
- LangePMarottJLVestboJPrediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general populationAm J Respir Crit Care Med20121861097598122997207
- HøisethADNeukammAKarlssonBDOmlandTBrekkePHSøysethVElevated high-sensitivity cardiac troponin T is associated with increased mortality after acute exacerbation of chronic obstructive pulmonary diseaseThorax201166977578121653926
- DalalAAShahMLunacsekOClinical and economic burden of patients diagnosed with COPD with comorbid cardiovascular diseaseRespir Med2011105101516152221684731
- PapaioannouAIBartziokasKLoukidesSCardiovascular comorbidities in hospitalised COPD patients: a determinant of future risk?Eur Respir J201546384684925882807
- MatamisDTsagouriasMPapathanasiouATargeting occult heart failure in intensive care unit patients with acute chronic obstructive pulmonary disease exacerbation: effect on outcome and quality of lifeJ Crit Care2014292315.e7315.e14
- MacDonaldMIShafuddinEKingPTChangCLBardinPGHancoxRJCardiac dysfunction during exacerbations of chronic obstructive pulmonary diseaseLancet Respir Med20164213814826781000
- TerzanoCRomaniSContiVPaoneGOrioloFVitarelliAAtrial fibrillation in the acute, hypercapnic exacerbations of COPDEur Rev Med Pharmacol Sci201418192908291725339486
- AbusaidGHBarbagelataATueroEMahmoodASharmaGDiastolic dysfunction and COPD exacerbationPostgrad Med20091214768119641273
- AbrougFOuanes-BesbesLNciriNAssociation of left-heart dysfunction with severe exacerbation of chronic obstructive pulmonary disease: diagnostic performance of cardiac biomarkersAm J Respir Crit Care Med2006174999099616840745
- El-ShabrawyaMEldamanhorASStudy of cardiovascular diseases in hospitalized AECOPD patientsEgypt J Chest Dis20176611725
- LarattaCRvan EedenSAcute exacerbation of chronic obstructive pulmonary disease: cardiovascular linksBioMed Res Int2014201452878924724085
- PatelARCKowlessarBSDonaldsonGCCardiovascular risk, myocardial injury, and exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201318891091109924033321
- PatelARCDonaldsonGCMackayAJWedzichaJAHurstJRThe impact of ischemic heart disease on symptoms, health status, and exacerbations in patients with COPDChest2012141485185721940771
- ChangCLRobinsonSCMillsGDBiochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPDThorax201166976476821474497
- DonaldsonGCHurstJRSmithCJHubbardRBWedzichaJAIncreased risk of myocardial infarction and stroke following exacerbation of COPDChest201013751091109720022970
- LahousseLNiemeijerMNvan den BergMEChronic obstructive pulmonary disease and sudden cardiac death: the Rotterdam studyEur Heart J201536271754176125920404
- AdrishMNannakaVBCanoEJBajantriBDiaz-FuentesGSignificance of NT-pro-BNP in acute exacerbation of COPD patients without underlying left ventricular dysfunctionInt J Chron Obstruct Pulmon Dis2017121183118928458528