Abstract
Background
Atrial fibrillation (AF) occurs frequently in patients with COPD. There are limited data about the impact of AF in hospitalized COPD patients on other serious health outcomes, such as acute organ dysfunction, severe sepsis, and respiratory failure. The aim of our study was to delineate the impact of AF in hospitalized COPD patients.
Methods
We defined COPD populations with and without AF from the National Health Insurance database in Taiwan. The control subjects (patients with COPD without AF) were selected from the population of COPD patients who had no history of AF and were matched to the COPD patients with AF by age (±1 year), gender, and the year of COPD diagnosis (±1 year). The primary outcome was the time to any first event, which included acute organ dysfunction, severe sepsis, respiratory failure, and death during the hospitalization period. Secondary outcomes, which also included acute organ dysfunction, severe sepsis, respiratory failure, and death, were estimated separately over time.
Results
The primary outcome probability was higher in COPD patients with AF than in COPD patients without AF, with an adjusted HR (aHR) of 1.169 (95% confidence interval [CI]: 1.034–1.320), and higher risks of acute organ dysfunction and respiratory failure were also observed in the former group, with aHRs of 1.179 (95% CI: 1.0370–1.339) and 1.176 (95% CI: 1.006–1.374), respectively.
Conclusion
Compared with COPD patients without AF, those with AF had a higher risk of hepatic dysfunction and respiratory failure.
Introduction
Atrial fibrillation (AF) is one of the most frequently noted arrhythmias in patients with COPD. There are many factors contributing to AF in the COPD population, including smoking, oxidative stress, and tissue hypoxia, as well as the effects of medications, including corticosteroids, theophylline, and beta-agonists.Citation1–Citation5 Our previous studyCitation6 showed that, compared with those without COPD, patients with COPD presented an adjusted HR (aHR) of 2.23 with a 95% confidence interval (CI) of 1.98–2.51. AF is an aging-associated disease with an incidence rate of 0.84 per 100,000 person-years in patients between 40 and 49 years old and an increased incidence rate of 5.23 per 100,000 person-years in those aged >70 years. A previous studyCitation7 enrolled 4,618 residents with AF that was first documented between 1980 and 2000; the results showed a trend of mortality after AF. After a mean follow-up of 5.3±5.0 years, the mortality HR was 9.62 within the first 4 months and 1.66 thereafter in the AF population with no evidence of changes in mortality during the 21 years. Another studyCitation8 investigated the long-term effects of AF in patients with pacemakers and found that mortality was significantly decreased during the last three decades. In addition, many studiesCitation9–Citation13 have shown that AF increases the risk of death, and the mortality rate was high in the first year of AF occurrence.Citation7 Due to different selection criteria and study periods, there is no consensus among researchers regarding the prognosis of AF in hospitalized patients. COPD and AF are common diseases and often coexist. A studyCitation14 enrolled 227 patients who had concomitant COPD and AF and found that COPD is an independent risk factor for the 1-year all-cause mortality in patients with AF. However, there is limited evidence regarding the influence of AF on the prognosis of COPD patients, such as organ dysfunction and respiratory failure in hospitalization. The aim of our study was to investigate the impact of AF on hospitalized COPD patients by using a nationwide analysis based on an insurance claims database in Taiwan.
Methods
Source of data
Taiwan started a single-payer National Health Insurance program on March 1, 1995 and enrolled >99.9% of Taiwan’s population. A medical claims database, the National Health Insurance Research Database (NHIRD), was created for research and includes outpatient and inpatient claims data. The database comprises patients’ age, gender, diseases, prescription drugs, and medical expenditures. This study was a population-based retrospective cohort one. Our data were retrieved from the Longitudinal Health Insurance Database, which comprises 1,000,000 beneficiaries collected from 1997 to 2013. In this observational and analytical study, the database was derived from NHIRD, and the data are de-identified secondary data released for research purposes. The study was reviewed and approved by the Institutional Review Board of Kaohsiung Medical University Hospital (KMUH-IRB-EXEMPT (II)-20170003). According to both the NHIRD and hospital regulations, the informed consent from patients was waived for this retrospective cohort study due to the information being de-identified secondary data. All procedures were in accordance with the principles of the Declaration of Helsinki.
Study population
We defined the COPD population according to the diagnostic guidelines of the International Classification of Diseases-9-Clinical Modification (ICD-9-CM) codes 490–492 and 496, A-codes A323 and A325, and at least one prescription of long-acting muscarinic antagonists, long-acting beta-agonists, or long-acting beta-agonists and inhaled corticosteroids between 1998 and 2012.
From COPD population, we extracted patients with history of AF (ICD-9-CM code 427.3) as case group between 1998 and 2012. The index date was the date of the first diagnosis of COPD, and patients in the COPD and AF group (case group) were diagnosed with AF before the index date.
The control subjects (patients with COPD without AF) were selected from the COPD patients who had no history of AF and were matched to the COPD patients with AF by age (±1 year), gender, and the year of index date (±1 year). The AF-to-control ratio was 1:3.
Infection site and life-support treatments, including intensive care, vasopressor use, hemodialysis, and mechanical ventilation, were extracted from ambulatory visits and hospitalization data within a year before the index date by ICD-9-CM codes and history of medications. The comorbidities were identified from inpatient or outpatient diagnoses 1 year before the index date. Comorbidities included hypertension (ICD-9-CM codes 401–405), diabetes (ICD-9-CM code 250), hyperlipidemia (ICD-9-CM code 272), cerebrovascular accident (ICD-9-CM codes 430–438), congestive heart failure (ICD-9-CM code 428), or cancer (ICD-9-CM codes 140–208). The demographic characteristics that were evaluated included gender, age, urban living, and comorbidities in the case and control groups.
Outcome measures
The primary outcome was the time to any first event, including acute organ dysfunction, severe sepsis, respiratory failure, and death during the hospitalization period. Secondary outcomes, which also included acute organ dysfunction, severe sepsis, respiratory failure, and death, were estimated separately over time. We also divided acute organ dysfunction into different organ systems (cardiovascular, respiratory, renal, hepatic, neurologic, hematologic, and metabolic) for evaluation, and the diagnostic codes for acute organ dysfunction are listed in Table S1. Severe sepsis included patients with bacterial or fungal infections and acute organ dysfunction during hospitalization, and the diagnostic criteria have been described in previous studies.Citation15,Citation16 Respiratory failure followed ICD-9-CM codes 518.81, 518.83, and 518.84 obtained from ambulatory visits and hospitalization data.
Statistical analysis
We sought to describe the demographics and clinical characteristics, including age, gender, urban living, comorbidities, infection sites, and life-support treatments including intensive care, vasopressor use, hemodialysis, and mechanical ventilation in COPD patients with and without AF.
Continuous variables are presented as the means and SDs and were compared between the case and control groups with Student’s t-tests. Discrete variables are presented as counts and percentages and were compared between the case and control groups with chi-square tests. Values of P<0.05 were considered statistically significant in all statistical analyses.
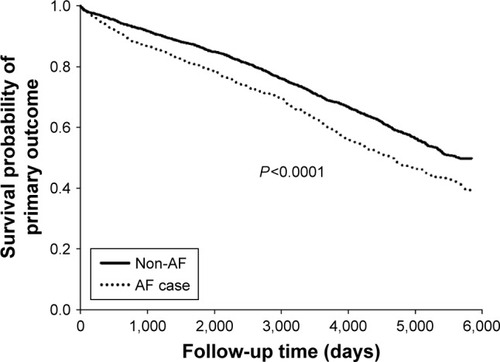
The effects of AF were examined in COPD patients during a 14-year follow-up. Each case was followed until the first occurrence of one of the primary outcome measures (acute organ dysfunction, severe sepsis, respiratory failure, or death) or until the end of December 31, 2013. All cases in which no predefined outcomes or death occurred during the follow-up were not included in the analysis. A Cox proportional hazards model was used to assess the association of outcomes with case and control groups during the follow-up period. Univariate and multivariate models were used to estimate HRs in the Cox proportional hazards model to assess the associations of primary and secondary outcomes in COPD patients with AF during the follow-up period. Models were adjusted for age, gender, urban living, comorbidities, infection sites, and life-support treatments. Kaplan–Meier estimates were used to generate time-to-event curves for the primary outcome. We used Kaplan–Meier analyses to estimate the time to primary outcome, including acute organ dysfunction, severe sepsis, respiratory failure, and death, in COPD patients with and without AF during the observed period. All data processing and statistical analyses were performed using the SAS® software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
We enrolled 882 patients with COPD and AF and 2,646 patients with COPD without AF. shows the demographic characteristics, comorbidities, infection sites, and life-support measures in COPD patients with and without AF. The mean age of patients with COPD and AF was 67.3 years. Approximately 50% of the patients with COPD and AF were aged >70 years, and male patients comprised 63.5% of this group. COPD patients with AF tended to have a higher prevalence of comorbidities, including hypertension (68.3% vs 46.3%), diabetes (22.8% vs 16.5%), hyperlipidemia (19.5% vs 14.7%), cerebrovascular accident (25.3% vs 16.9%), and congestive heart failure (20% vs 8.4%) than COPD patients without AF. Infections occurred more frequently in COPD patients with AF than in COPD patients without AF. Compared with COPD patients without AF, COPD patients with AF required more life-support resources, including admission to the intensive care unit, vasopressor administration, hemodialysis, and mechanical ventilation.
Table 1 Demographic characteristics and comorbidities in COPD patients with and without AF
shows the impact of AF on the outcome risks in patients with COPD during the follow-up period. The primary outcome probability was higher in COPD patients with AF than in those without AF, with an aHR of 1.169 (95% CI: 1.034–1.320), and a higher risk of acute organ dysfunction and respiratory failure was also observed in the former group, with aHRs of 1.179 (95% CI: 1.0370–1.339) and 1.176 (95% CI: 1.006–1.374), respectively. There was no significant difference between the patient groups in the occurrence of severe sepsis or death.
Table 2 Effects of AF on the risk of outcomes in patients with COPD
In , we further stratified the acute organ dysfunction and found that COPD patients with AF had a higher risk of respiratory failure and hepatic dysfunction than COPD patients without AF, with aHRs of 1.213 (95% CI: 1.041–1.414) and 1.882 (95% CI: 1.113–3.181), respectively, after adjusting for age, gender, comorbidities, urban living, infection status, and life-support measures.
Table 3 Acute organ dysfunction in COPD patients with and without AF stratified by diseases
shows the aHRs for factors associated with the risk of primary outcome events and acute organ dysfunction during the follow-up period. AF, age, male sex, diabetes, cerebrovascular accident, congestive heart failure, infection at any one site, genitourinary infection, and treatment with mechanical ventilation were the factors associated with a higher risk of primary outcome events in COPD patients. AF, age, male sex, hypertension, diabetes, hyperlipidemia, cerebrovascular accident, congestive heart failure, infection at any one site, and treatment with mechanical ventilation were the factors associated with a higher risk of acute organ dysfunction in COPD patients.
Table 4 Adjusted HRs for factors associated with the risk of primary outcome and acute organ dysfunction in the follow-up period
shows the Kaplan–Meier curves of the primary outcome (time to any first event, including acute organ dysfunction, severe sepsis, respiratory failure, and death during the hospitalization period) in COPD patients with and without AF (P<0.001).
Discussion
To our knowledge, this is the first nationwide study to demonstrate the impact of AF in COPD patients admitted to a hospital.
A study using the Spanish National Hospital Discharge DatabaseCitation17 to compare the incidence of hospitalization for AF in patients with and without COPD found that COPD is a common comorbidity in patients hospitalized for AF. In addition, the incidence of hospitalization for AF was twice as high in COPD patients than in those without COPD, and the presence of comorbidities, the length of hospital stays, and the in-hospital mortality rate were significantly higher in AF patients with COPD than in those without COPD.
Our study had similar results. Patients with COPD and AF had a higher prevalence of comorbidities and more frequent infections and were more likely to receive intensive care, vasopressor treatment, hemodialysis, and mechanical ventilation. However, the previous study did not mention the outcomes of acute organ dysfunction, severe sepsis, or respiratory failure. We found in our study that, compared with COPD patients without AF, COPD patients with AF had a higher risk of acute organ dysfunction and respiratory failure. Cardiovascular diseases are frequently comorbid with COPD and may have an impact on the prognosis and mortality. A previous study showedCitation18 that, compared with patients with congestive heart failure and no COPD, patients with congestive heart failure and COPD had an increased risk of hospitalization but not of mortality. COPD also increases the morbidity and mortality among patients with ischemic heart disease.Citation19 Cardiac arrhythmia frequently occurs in patients with COPD. AF and ventricular arrhythmias are risk factors of death within 1 year of COPD acute exacerbation and admission to a hospital.Citation20 The mechanisms of arrhythmia include delayed afterdepolarizations, altered cardiac repolarization, increased sympathetic tone, or reduced vagal tone resulting in triggered activity, prolonged QT phase, and heart rate variability.Citation21 Other authors found that AF was independently associated with 1-year and 5-year mortality rates after multivariate analysis in patients hospitalized for COPD, with HRs of 1.54 (95% CI: 1.01–2.35) and 1.37 (95% CI: 1.05–1.78), respectively.Citation22 Our study followed patients for 14 years and found that AF increased not only the incidence of acute organ dysfunction but also that of respiratory failure.
Although the mechanisms of AF and fatty liver disease are not clear, there are two studiesCitation23,Citation24 that found an association between nonalcoholic fatty liver disease and AF, and the authors speculated that this association is causal and two-way. A studyCitation25 used transient elastography to detect liver stiffness in an elderly Finnish population and found an association between AF and liver stiffness after adjusting for body mass index, age, gender, alcohol intake, smoking, insulin resistance, and systolic blood pressure.
Reactive oxygen species play an important role in the essential steps in initiating liver fibrosis by inducing hepatic stellate cell activation and hepatocyte apoptosis.Citation26 Angiotensin II and atrial stretch can activate NADPH oxidase as a potential enzymatic source for reactive oxygen species production in AF patients.Citation27 Galectin-3 concentrations are higher in patients with heart failure and AF and are associated with an increased risk of AF,Citation28 but there is no statistically significant after-adjustment for the risk factor of AF. Galectin-3 is associated with cardiometabolic comorbidities, and its production is not triggered by abnormal heart rhythm.Citation29 The role of galectin-3 is associated with fibroblast proliferation, transformation, adhesion, differentiation, and angiogenesis, as well as cell apoptosis in connection to liver cirrhosis and myocardial fibrosis.Citation30
COPD is characterized by systemic inflammation as well as increased amounts of reactive oxygen species, and this may drive the pathophysiology in hepatic dysfunction. Other factors include iatrogenic causes or medications attributed to liver dysfunction which needs to be further investigated. Our study found that COPD patients with AF have a higher risk of hepatic dysfunction, but a prospective cohort study is required to delineate the association and investigate the molecular pathways between liver disease and AF in COPD population.
There are some limitations to our study. Our database lacks laboratory data and images, such as pulmonary function tests and echocardiograms, making it difficult to further analyze the study population. There may be doubt about the coding of the diseases in database. In general, the disease coding has been validated and found to be convincing and appears to be a valid resource for further research.Citation31 Otherwise, additional prerequisites such as medication use can help define the diseases and can enhance the data reliability.
Conclusion
COPD patients with AF had more comorbidities than did COPD patients without AF. After admission to a hospital, there was no statistically significant risk of sepsis, but hepatic dysfunction and respiratory failure were higher in COPD patients with AF than in COPD patients without AF. The relationship between AF and liver dysfunction requires further study because, compared with COPD patients without AF, COPD patients comorbid with AF are more vulnerable to liver disease, which should not be ignored.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This work was supported by a grant from the Chi Mei Medical Center, Chiali (CCFHR10601), and supported by a grant from the Kaohsiung Medical University Research Foundation (KMU-M107020).
Supplementary material
Table S1 Diagnostic codes for acute organ dysfunction
Disclosure
The authors report no conflicts of interest in this work.
References
- KinoshitaMHergesRMHodgeDORole of smoking in the recurrence of atrial arrhythmias after cardioversionAm J Cardiol2009104567868219699344
- KorantzopoulosPKolettisTMGalarisDGoudevenosJAThe role of oxidative stress in the pathogenesis and perpetuation of atrial fibrillationInt J Cardiol2007115213514316764958
- OgiHNakanoYNiidaSIs structural remodeling of fibrillated atria the consequence of tissue hypoxia?Circ J20107491815182120631454
- SalpeterSROrmistonTMSalpeterEECardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysisChest200412562309232115189956
- ChristiansenCFChristensenSMehnertFCummingsSRChapurlatRDSørensenHTGlucocorticoid use and risk of atrial fibrillation or flutter: a population-based, case-control studyArch Intern Med2009169181677168319822824
- LiaoKMChenCYIncidence and risk factors of atrial fibrillation in Asian COPD patientsInt J Chron Obstruct Pulmon Dis2017122523253028883719
- MiyasakaYBarnesMEBaileyKRMortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based studyJ Am Coll Cardiol200749998699217336723
- AsbachSOlschewskiMFaberTSZehenderMBodeCBrunnerMMortality in patients with atrial fibrillation has significantly decreased during the last three decades: 35 years of follow-up in 1627 pacemaker patientsEuropace200810439139418326852
- StewartSHartCLHoleDJMcMurrayJJA population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley studyAm J Med2002113535936412401529
- KirchhofPAuricchioABaxJCrijnsHOutcome parameters for trials in atrial fibrillation: executive summaryEur Heart J200728222803281717897924
- BenjaminEJWolfPAD’AgostinoRBSilbershatzHKannelWBLevyDImpact of atrial fibrillation on the risk of death: the Framingham Heart StudyCirculation199898109469529737513
- VidailletHGranadaJFChyouPOA population-based study of mortality among patients with atrial fibrillation or flutterAm J Med2002113536537012401530
- RuigómezAJohanssonSWallanderMAGarcía RodríguezLARisk of mortality in a cohort of patients newly diagnosed with chronic atrial fibrillationBMC Cardiovasc Disord20022511897013
- HuangBYangYZhuJClinical characteristics and prognostic significance of chronic obstructive pulmonary disease in patients with atrial fibrillation: results from a multicenter atrial fibrillation registry studyJ Am Med Dir Assoc201415857658124894999
- LiaoKMLinTCLiCYYangYHDementia increases severe sepsis and mortality in hospitalized patients with chronic obstructive pulmonary diseaseMedicine (Baltimore)20159423e96726061334
- ShenHNLuCLLiCYDementia increases the risks of acute organ dysfunction, severe sepsis and mortality in hospitalized older patients: a National Population-Based StudyPLoS One20127e4275122905169
- Méndez-BailónMLopez-de-AndrésAde Miguel-DiezJChronic obstructive pulmonary disease predicts higher incidence and in hospital mortality for atrial fibrillation. An observational study using hospital discharge data in Spain (2004–2013)Int J Cardiol201723620921528190617
- CanepaMStraburzynska-MigajEDrozdzJCharacteristics, treatments and 1-year prognosis of hospitalized and ambulatory heart failure patients with chronic obstructive pulmonary disease in the European Society of Cardiology Heart Failure Long-Term RegistryEur J Heart Fail201820110011028949063
- OnishiKTotal management of chronic obstructive pulmonary disease (COPD) as an independent risk factor for cardiovascular diseaseJ Cardiol201770212813428325523
- FusoLIncalziRAPistelliRPredicting mortality of patients hospitalized for acutely exacerbated chronic obstructive pulmonary diseaseAm J Med19959832722777872344
- LahousseLNiemeijerMNvan den BergMEChronic obstructive pulmonary disease and sudden cardiac death: the Rotterdam studyEur Heart J201536271754176125920404
- García-SanzM-TCánive-GómezJCSenín-RialLOne-year and long-term mortality in patients hospitalized for chronic obstructive pulmonary diseaseJ Thorac Dis20179363664528449471
- KarajamakiAJPatsiOPSavolainenMKesaniemiYAHuikuriHUkkolaONon-alcoholic fatty liver disease as a predictor of atrial fibrillation in middle-aged population (OPERA Study)PLoS One20151011e014293726571029
- TargherGValbusaFBonapaceSNon-alcoholic fatty liver disease is associated with an increased incidence of atrial fibrillation in patients with type 2 diabetesPLoS One201382e5718323451184
- KäräjämäkiAJKettunenOLepojärviSPresence of atrial fibrillation is associated with liver stiffness in an elderly Finnish populationPLoS One2017123e017385528288202
- LiangSKisselevaTBrennerDAThe role of NADPH oxidases (NOXs) in liver fibrosis and the activation of myofibroblastsFront Physiol201671726869935
- YounJYZhangJZhangYOxidative stress in atrial fibrillation: an emerging role of NADPH oxidaseJ Mol Cell Cardiol201362727923643589
- HoJEYinXLevyDGalectin 3 and incident atrial fibrillation in the communityAm Heart J2014167572973424766984
- KornejJSchmidlJUeberhamLGalectin-3 in patients with atrial fibrillation undergoing radiofrequency catheter ablationPLoS One2015104e012357425875595
- LiLCLiJGaoJFunctions of galectin-3 and its role in fibrotic diseasesJ Pharmacol Exp Ther2014351233634325194021
- ChengCLLeeCHChenPSLiYHLinSJYangYHValidation of acute myocardial infarction cases in the National Health Insurance Research Database in TaiwanJ Epidemiol201424650050725174915