Abstract
Purpose
The unpredictable trajectory of COPD can present challenges for patients when faced with a decision regarding a do-not-resuscitate (DNR) directive. The current retrospective analysis was conducted to investigate factors associated with an early DNR decision (prior to last hospital admission) and differences in care patterns between patients who made DNR directives early vs late.
Patients and methods
Electronic health records (EHR) were reviewed from 271 patients with terminal COPD who died in a teaching hospital in Taiwan. Clinical parameters, patterns of DNR decisions, and medical utilization were obtained. Those patients who had a DNR directive earlier than their last (terminal) admission were defined as “Early DNR” (EDNR).
Results
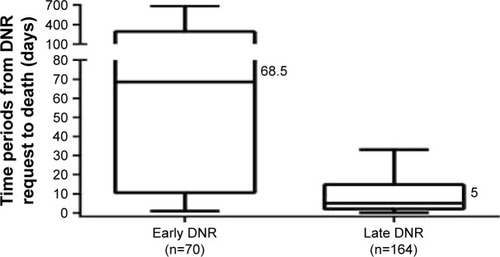
A total of 234 (86.3%) patients died with a DNR directive, however only 30% were EDNR. EDNR was associated with increased age (OR=1.07; 95% CI: 1.02–1.12), increased ER visits (OR=1.22; 95% CI: 1.10–1.37), rapid decline in lung function (OR=3.42; 95% CI: 1.12–10.48), resting heart rate ≥100 (OR=3.02; 95% CI: 1.07–8.51), and right-sided heart failure (OR=2.38; 95% CI: 1.10–5.19). The median time period from a DNR directive to death was 68.5 days in EDNR patients and 5 days in “Late DNR” (LDNR) patients, respectively (P<0.001). EDNR patients died less frequently in the intensive care unit (P<0.001), received less frequent mechanical ventilation (MV; P<0.001), more frequent non-invasive MV (P=0.006), and had a shorter length of hospital stay (P=0.001).
Conclusions
Most patients with terminal COPD had DNR directives, however only 30% of DNR decisions were made prior to their last (terminal) hospital admission. Further research using these predictive factors obtained from EHR systems is warranted in order to better understand the relationship between the timing associated with DNR directive decision making in patients with terminal COPD.
Introduction
COPD is a chronic illness that presents as a chronic productive cough and progressive shortness of breath.Citation1 COPD was the seventh leading cause of death in Taiwan in 2015 and estimates suggest it will be the third leading cause of death worldwide in 2030.Citation2,Citation3 Patients with advanced COPD often have a poor prognosisCitation4; however, advanced COPD patients receive intensive care more frequently compared with patients diagnosed with lung cancer.Citation5–Citation9 Patients with advanced COPD have increased comorbidities, spend more days in the hospital, have more invasive procedures, are more likely to die in the intensive care unit (ICU) and are less likely to have a do-not-resuscitate (DNR) directive.Citation10–Citation13
Cardiopulmonary resuscitation (CPR) performed in patients with a terminal illness is often ineffective and is associated with a reduction in quality of end-of-life care.Citation14 A DNR directive indicates a patient’s refusal to accept CPR when suffering from cardiac or respiratory arrest and is one of the most commonly discussed advance directives in palliative care.Citation15,Citation16
In 2000, the Hospice Palliative Care Act (HPCA) became a law in Taiwan, with amendments following in 2002, 2012, and 2013.Citation17,Citation18 People who suffer from a terminal illness, when certified by two physicians, have the right to refuse CPR.Citation18 According to the HPCA, a DNR directive can be made in one of two ways: signed by a competent terminally ill patient (DNR will) or by a close relative (DNR consent) when the patient is no longer capable of making that decision for himself/herself.Citation19
Other international guidelines have emphasized the importance of advance care directives being made early in patients with late stage COPDCitation1,Citation20; however, several barriers have been identified. COPD has an unpredictable disease trajectory.Citation21,Citation22 It is difficult to predict the death of a patient with COPD within six months.Citation23,Citation24 Common parameters for prognostic criteria include measures of lung function, degree of hypoxia, history of hospitalization, and recent ventilator support – all of which have been found to be unreliable.Citation25–Citation28 Therefore, the timing of decisions regarding DNR directives in most patients with COPD may occur closer to death than not, and that decision may not be made by the patient themselves.
The aim of this study was to investigate factors associated with an early DNR decision (prior to last [terminal] hospital admission) and differences in care patterns between patients who made DNR directives early vs late. The timing of DNR decisions, who made the DNR decision, and the medical utilization of patients with COPD who died in a medical center in Taiwan were analyzed. Factors associated with early DNR decisions as obtained from hospital electronic health records (EHR) were also analyzed to provide additional insight for physicians, patients and their families to support their decision making when faced with a decision regarding a DNR directive.
Methods
Consecutive patients whose primary or secondary cause of death was COPD (based on ICD, ninth revision, Clinical Modification [ICD-9-CM] coding) between 2011 and 2015, and whose death occurred in Taichung Veterans General Hospital (TCVGH), Taiwan, were included in this retrospective observational cohort study. Subjects with fewer than two TCVGH visits for the management of the symptoms associated with their COPD in the last year of life were excluded. TCVGH is a tertiary teaching hospital and the only public medical center located in central Taiwan. Patient demographics, diagnostic test results, treatment history, including palliative care, at TCVGH, was collected using the EHR system. The study protocol was fully reviewed and approved by the Institutional Review Board of the Taichung Veterans General Hospital (TCVGH-IRB) Taiwan (IRB number: CE17017A, date of approval: 11/22/2016). The requirement for informed patient consent was waived by the TCVGH internal review board considering the retrospective study design and the availability of all data via electronic medical records. Only de-identified patient data was used in this study.
Study population
EHRs from a total of 271 patients were included in the analysis. Eligible patients were ≥40 years of age, had been diagnosed with COPD (ICD-9-CM codes 491.x, 492.x, and 496.x), had been admitted to the hospital for acute care, and died in the hospital between June 1, 2011 and December 31, 2015. Patients who met the inclusion criteria but were discharged in critical condition or terminal status were also included in the analysis.
Operational definitions of outcome measures
All subjects were validated according to the official criteria for “terminal status in COPD.”Citation29 Terminal status in COPD refers to having symptoms of dyspnea at rest, a progressive condition, and any of the following conditions: 1) Respiratory insufficiency (with or without oxygen support [PaO2 ≤55 mmHg, PaCO2 ≥50 mmHg, or O2 saturation ≤88%]); 2) FEV1 ≤30% of predicted; 3) FEV1 declined ≥40 mL/year; 4) Weight loss ≥10% in 6 months; 5) Resting heart rate ≥100/min; 6) Right-sided heart failure; and 7) Multiple comorbidities: (eg, cachexia, recurrent infection, depression, or multiple comorbidities).Citation8,Citation9
Patients with COPD or their surrogates who had a DNR directive prior to their last (terminal) admission to the hospital were classified as Early DNR (EDNR). Whereas, Late DNR (LDNR) patients were those who implemented a DNR directive during their last admission.
Assessment
We collected data on patient age, gender, pulmonary function test results (FEV1/FVC ratio and FEV1%), heart function (two-dimensional echocardiography), medical utilization (number of emergency room (ER) visits and hospitalizations), and any CPR (cardiac pulmonary resuscitation) within 1 year prior to death. Additional information obtained during the last (terminal) hospital admission included whether admitted from the ER, died on the service of a pulmonologist, died in the ICU, or experienced mechanical ventilation (such as invasive and non-invasive mechanical ventilation). The frequency of each criterion met by each patient with COPD was calculated. Furthermore, timing of a signed DNR directive and the patient status (terminal or not terminal) was also recorded. The total number of days from each patient’s signed DNR consent until their deaths, as well as the number of days from physician confirmed terminal status to patient death were analyzed.
Statistical analysis
Statistical analyses were completed using SPSS version 22.0 (International Business Machines Corp, Armonk, NY, USA). For nonparametric distribution data, differences between groups were assessed using a Mann–Whitney U test and results were presented as median and interquartile range (IQR). The categorical variables were presented as frequency and percentage and analyzed using the chi-squared test. Factors associated with EDNR were assessed using univariate analysis and those with significant difference were assessed using multivariate analysis. The strength of association was presented as the odds ratio (OR) and 95% confidence intervals (CI). All results with P<0.05 were deemed to be statistically significant.
Results
Characteristics of COPD deaths
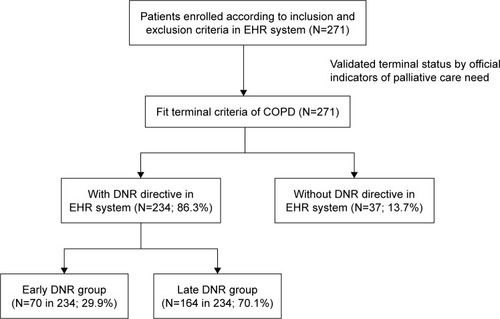
A total of 271 deaths due to COPD fit the enrollment criteria. Patient characteristics and the study flow chart are summarized in and . Patients with COPD who died in the hospital were aged, predominately male, and experienced frequent ER visits and hospitalizations. Most patients (94.5%) were admitted from the ER on their last (terminal) admission to the hospital, 59.8% of patients died while being treated by a pulmonologist, and 32.5% died in the ICU. Despite 86.3% of patients having a DNR directive, 83.0% still experienced mechanical ventilation (MV) and 67.5% experienced invasive MV. Only 11.1% had been documented as being terminal by the attending physician, and almost 80% of these were documented during the last admission when the patient was near death. Although 86.3% of patients had expressed an interest in establishing a DNR directive by themselves or via their family surrogates, greater than 70% of the DNR directives were made during the last admission prior to death.
Table 1 Demographic characteristics of patients with COPD who died in a medical center over a period of 5 years (2011–2015) (N=271)
Figure 1 Study flow chart.
Abbreviations: DNR, do-not-resuscitate; EHR, Electronic health records.
Validated official criteria for “terminal status in COPD”
Since only 11.1% of COPD deaths were documented as terminal status near death, the terminal condition according to the official criteria required validation.Citation29,Citation30 In our retrospective analysis, all patients fit the official criteria for “terminal status in COPD.”Citation29 The top three criteria were respiratory insufficiency (94.1%), multiple comorbidities (89.7%), and resting heart rate greater than 100 bpm (78.2%; ).
Table 2 The official indicators of “terminal status in COPD” in Taiwan
“Early DNR,” “Late DNR,” and patterns of care during the last admission for COPD
EDNR patients were aged, had more frequent ER visits and hospitalizations, and met the criteria for “terminal status” more frequently than LDNR patients (all P<0.05; ). The EDNR group had an increased frequency of rapid declines in lung function (P=0.014), resting heart rate ≥100 bpm (P=0.024) and right-sided heart failure (P=0.003). EDNR patients died less frequently in the ICU (P<0.001), used less invasive mechanical ventilation (MV) (P<0.001), used non-invasive MV more frequently (P=0.006) and had shorter lengths of stay before death (P=0.001). The amount of time between DNR request to death was also significantly longer in the EDNR group compared with the LDNR group (median: 68.5 days and 5 days, respectively, P<0.001; and ).
Table 3 Comparison of care pattern and terminal criteria between “Early DNR” and “Late DNR”
Factors associated with EDNR
Factors associated with EDNR are shown in . Using a univariate analysis, older age (odds ratio; OR=1.08; 95% CI: 1.04–1.13, P<0.001), frequent ER visits (OR=1.25; 95% CI: 1.13–1.38, P<0.001), meeting more clinical indicators for palliative care (OR=1.32; 95% CI: 1.09–1.60, P=0.005), rapid decline in pulmonary function (OR=2.23; 95% CI: 1.22–4.10, P=0.009), resting heart rate ≥100 bpm (OR=2.56; 95% CI: 1.18–5.59, P=0.018), and right-sided heart failure (OR=2.49; 95% CI: 1.40–4.42, P=0.002) were associated with EDNR. “Terminal status documented by a physician” was not correlated with an early DNR directive (OR=1.97; 95% CI: 0.90–4.32, P=0.09). Multivariate analysis was applied to those factors found to be significant with univariate analysis. The multivariate analysis showed that older age (OR=1.07; 95% CI: 1.02–1.12, P=0.005), frequent ER visits (OR=1.22; 95% CI: 1.10–1.37, P<0.001), rapid decline in pulmonary function (OR=3.42; 95% CI: 1.12–10.48, P=0.031), resting heart rate ≥100 bpm (OR=3.02; 95% CI: 1.07–8.51, P=0.036), and right-sided heart failure (OR=2.38; 95% CI: 1.10–5.19, P=0.028) were significantly associated with early DNR requests. However, when using a multivariate analysis, age remained a significant factor and numbers of clinical indicators was not a significant factor (OR=0.68; 95% CI: 0.44–1.06, P=0.091).
Table 4 Factors associated with EDNR
Discussion
Three major findings were demonstrated in the current study. First, the official criteria for “terminal status in COPD” was validated – all enrolled COPD patients (N=271) fit the official criteria for terminal COPD. To the best of our knowledge, this is the first research to validate the official criteria for “terminal COPD” using real-world data from Taiwan.
Second, a gap of DNR decisions and the identification of terminal COPD status between patients/their surrogates and physicians was observed. In this cohort, 234 of the 271 patients with COPD (86.3%) had signed a DNR directive before they died; however, only 30 of the 271 patients with COPD (11.1%) had been confirmed and documented as being terminal status by physicians. Of the 234 cases with a DNR order, 233 cases were from family surrogates and only one patient made their own decision. According to the “Hospice Palliative Care Act” in Taiwan, two scenarios are possible when making a decision regarding a DNR directive.Citation17,Citation18 1) It could be made by a patient themselves (DNR signed by patient), or 2) by their surrogate (DNR signed by surrogate).Citation19 In this case it is possible the physicians had initiated conversations with family surrogates prior to last admission. Previous studies in Taiwan suggested patients who understand the prognosis of their disease or have previous discussions about a DNR order tend to have a DNR directive, however, in a real-world setting a family surrogate often needs to make a DNR directive on behalf of patients who cannot express their intention at end of life.Citation16 In a local survey of 201 nursing home residents in Taiwan, the result showed that 16.4% had DNR directives, and 91% of these DNR directives were signed by family surrogates.Citation31 This situation is the same as reports from Europe and North America that older patients prefer to make their final DNR directives by themselves.Citation32,Citation33 The current data not only reflect the unmet need for early advance care planning in COPD even when the “Hospice Palliative Care Act” is taken into account, but also show the uncertainty of physicians in identifying terminal status in patients with COPD. This phenomenon may contribute to the important barriers, such as poor communication between patients and physicians and the unpredictable trajectory of COPD when initiating DNR decisions.Citation34–Citation36 Third, we have identified factors associated with executing a DNR early by patients and/or their surrogates. EDNR patients had less intensive care, died less frequently in the ICU, and had shorter lengths of stay in the hospital in the last admission before they died when compared with the LDNR group. These results suggest that obtaining an early DNR directive (by patients or their surrogates) changed the attitude and treatment strategy of physicians. Only 11% of terminal patients with COPD were documented as in terminal status by physicians.
It is difficult to predict the death of patients with COPD within 6 months.Citation22–Citation24 Although pulmonary function tests (PFT) were important indicators of the prognosis for COPD,Citation12,Citation35 in the current study, only 35.4% (96 of 271 patients) had a PFT within 1 year prior to death. Heart failure is one of the most common comorbid conditions in COPD.Citation37,Citation38 The presence of pulmonary hypertension and right-sided heart failure doubles the mortality in patients with COPD.Citation39,Citation40 In our data, severe COPD accompanied by documented right-sided heart failure was significantly associated with early DNR directives (OR=2.49; 95% CI: 1.40–4.42). We suggest that an annual follow-up PFT and heart function surveys are important in helping physicians to evaluate the disease progression of COPD.
There are some limitations to this study. First, the retrospective design collected data in a hospital. Therefore, it was possible to have missed patients due to inappropriate ICD-9-CM coding, underreporting, and/or incorrect electronic medical records diagnoses. Second, the care continuity of these COPD patients would be challenged for the missing data of medical utilizations. Since we have excluded subjects with fewer than two physician visits for COPD in TCVGH in their last year of life and the most critical COPD patients will be referred to TCVGH in central Taiwan, we could lower the impact of these two limitations. Third, we could not obtain the view point of patients and their surrogates due to the limitations of the study design. Fourth, the uncertainty of a clear definition of COPD terminal status would be a limitation for physicians expected to certify this status for their patients with COPD within an electronic medical record. Fifth, the results were based on a single medical center, so they may not represent the situation in other places or countries.
Conclusion
In this study, we currently report that despite 86.3% of patients with terminal COPD having DNR directives, only 11.1% had their terminal status documented by a physician, and 70% of DNR directives were made in the last admission before death. The major decision makers for the DNR directives were not the patients themselves, rather family surrogates. The time gap between “Early DNR” and “Late DNR” was nearly 60 days before death. By using information from EHRs, “Early DNR” was associated with older age, more ER visits, rapid decline in lung function, tachycardia and right-sided heart failure. Further research to routinely capture these predictive factors in existing EHR databases to help patients, their surrogates, and primary care physicians to share decision making in advanced COPD is warranted in the future.
Author contributions
The authors listed in the article meet conditions as following: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
The authors thank the Clinical Informatics Research & Development Center and Taichung Veterans General Hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
- VogelmeierCFCrinerGJMartinezFJGlobal strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 Report. GOLD Executive SummaryAm J Respir Crit Care Med2017195555758228128970
- 2015 statistical results on causes of death in Taiwan2017 Available from: http://www.mohw.gov.tw/mp-2.htmlAccessed October 12, 2017
- Global surveillance, prevention and control of chronic respiratory diseases – A comprehensive approach2007 Available from: http://www.who.int/respiratory/publications/global_surveillance/en/Accessed October 12, 2017
- JoshiMJoshiABartterTSymptom burden in chronic obstructive pulmonary disease and cancerCurr Opin Pulm Med20121829710322262138
- TsimSDavidsonSEnd-of-life care in a general respiratory ward in the United KingdomAm J Hosp Palliat Care201431217217423503567
- CurtisJREngelbergRYoungJPAn approach to understanding the interaction of hope and desire for explicit prognostic information among individuals with severe chronic obstructive pulmonary disease or advanced cancerJ Palliat Med200811461062018454614
- AuDHUdrisEMFihnSDMcDonellMBCurtisJRDifferences in health care utilization at the end of life among patients with chronic obstructive pulmonary disease and patients with lung cancerArch Intern Med2006166332633116476873
- CurtisJRPalliative and end-of-life care for patients with severe COPDEur Respir J200832379680317989116
- HyasatKSriramKBEvaluation of the patterns of care provided to patients with COPD compared to patients with lung cancer who died in hospitalAm J Hosp Palliat Care201633871772225987648
- ClaessensMTLynnJZhongZDying with lung cancer or chronic obstructive pulmonary disease: insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of TreatmentsJ Am Geriatr Soc2000485 SupplS146S15310809468
- GoodridgeDLawsonJDugglebyWMarciniukDRennieDStangMHealth care utilization of patients with chronic obstructive pulmonary disease and lung cancer in the last 12 months of lifeResp Med20081026885891
- ChouWCLaiYTHuangYCChangCLWuWSHungYSComparing end-of-life care for hospitalized patients with chronic obstructive pulmonary disease and lung cancer in TaiwanJ Palliat Care2013291293523614168
- BrownCEEngelbergRANielsenELCurtisJRPalliative care for patients dying in the intensive care unit with chronic lung disease compared with metastatic cancerAnn Am Thorac Soc201613568468926784137
- ZafarWGhafoorIJamshedAGulSHafeezHOutcomes of in-hospital cardiopulmonary resuscitation among patients with cancerAm J Hosp Palliat Care201734321221626589879
- MentzelopoulosSDSlowtherAMFritzZEthical challenges in resuscitationIntensive Care Med201844670371629748717
- FangYCPaiMCWangLCFactors influencing family surrogates’ intention with regard to do-not-resuscitate directive for patients with dementiaClin Gerontol20181019
- ChangHTLinMHChenCKChouPChenTJHwangSJTrends of do-not-resuscitate consent and hospice care utilization among noncancer descendents in a tertiary hospital in Taiwan between 2010 and 2014: a hospital-based observational studyMedicine20169546e539427861375
- Hospice Palliative Care Act2013 Available from: http://law.moj.gov.tw/Eng/LawClass/LawContent.aspx?PCODE=L0020066Accessed May 29, 2018
- LiangYHWeiCHHsuWHDo-not-resuscitate consent signed by patients indicates a more favorable quality of end-of-life care for patients with advanced cancerSupport Care Cancer201725253353927704261
- LankenPNTerryPBDelisserHMAn official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnessesAm J Respir Crit Care Med2008177891292718390964
- SteelAGoldringJEnd-of-life care in patients with chronic obstructive pulmonary diseaseBr J Hosp Med2015761C10C13
- SpathisABoothSEnd of life care in chronic obstructive pulmonary disease: in search of a good deathInt J Chron Obstruct Pulmon Dis200831112918488426
- The SUPPORT Principal InvestigatorsA controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT)JAMA199527420159115987474243
- CoventryPAGrandeGERichardsDAToddCJPrediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic reviewAge Ageing200534321822715863407
- Hansen-FlaschenJChronic obstructive pulmonary disease: the last year of lifeResp Care20044919097
- SeneffMGWagnerDPWagnerRPZimmermanJEKnausWAHospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary diseaseJAMA199527423185218577500534
- BenzoRSiemionWNovotnyPFactors to inform clinicians about the end of life in severe chronic obstructive pulmonary diseaseJ Pain Symptom Manage2013464994491499
- McGhanRRadcliffTFishRSutherlandERWelshCMakeBPredictors of rehospitalization and death after a severe exacerbation of COPDChest200713261748175517890477
- Palliative care services open to terminally ill non-cancer patients in eight newly added categories Officially Covered by National Health Insurance since September 1st, 20092009 Available from: https://www.nhi.gov.tw/english/News_Content.aspx?n=996D1B4B5DC48343&sms=F0EAFEB716DE7FFA&s=37BA73280DCC9628Accessed May 29, 2018
- HsuNCLinYFShuCCYangMCWjKNoncancer palliative care: the lost pieces in an acute care setting in TaiwanAm J Hosp Pall Care2013304334338
- LoYTWangJJLiuLFWangCNPrevalence and related factors of do-not-resuscitate directives among nursing home residents in TaiwanJ Am Med Dir Assoc201011643644220627185
- AgårdAHermerénGHerlitzJShould cardiopulmonary resuscitation be performed on patients with heart failure? The role of the patient in the decision-making processJ Intern Med2000248427928611086637
- FrankCHeylandDKChenBFarquharDMyersKIwaasaKDetermining resuscitation preferences of elderly inpatients: a review of the literatureCMAJ2003169879579914557319
- CurtisJREngelbergRANielsenELAuDHPatrickDLPatient-physician communication about end-of-life care for patients with severe COPDEur Respir J200424220020515332385
- JanssenDJCurtisJRAuDHDhAPatient-clinician communication about end-of-life care for Dutch and US patients with COPDEur Respir J201138226827621233263
- MomenNHadfieldPKuhnISmithEBarclaySDiscussing an uncertain future: end-of-life care conversations in chronic obstructive pulmonary disease. A systematic literature review and narrative synthesisThorax201267977778022802331
- BrownJPMartinezCHChronic obstructive pulmonary disease comorbiditiesCurr Opin Pulm Med201622211311826814720
- CamiciottoliGBigazziFMagniCPrevalence of comorbidities according to predominant phenotype and severity of chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2016112229223627695310
- Oswald-MammosserMWeitzenblumEQuoixEPrognostic factors in COPD patients receiving long-term oxygen therapy. Importance of pulmonary artery pressureChest19951075119311987750305
- ShujaatAMinkinREdenEPulmonary hypertension and chronic cor pulmonale in COPDInt J Chron Obstruct Pulmon Dis20072327328218229565