Abstract
Introduction
Exercise tolerance testing is an integral part of the pulmonary rehabilitation (PR) management of patients with chronic obstructive pulmonary disease (COPD). The 6-minute stepper test (6MST) is a new, well-tolerated, reproducible exercise test, which can be performed without any spatial constraints.
Objective
The aim of this study was to compare the results of the 6MST to those obtained during a 6-minute walk test (6MWT) and cardiopulmonary exercise testing (CPET) in a cohort of COPD patients.
Methods
Ninety-one COPD patients managed by outpatient PR and assessed by 6MST, 6MWT, and CPET were retrospectively included in this study. Correlations between the number of steps on the 6MST, the distance covered on the 6MWT, oxygen consumption, and power at the ventilatory threshold and at maximum effort during CPET were analyzed before starting PR, and the improvement on the 6MST and 6MWT was compared after PR.
Results
The number of steps on the 6MST was significantly correlated with the distance covered on the 6MWT (r=0.56; P<0.0001), the power at maximum effort (r=0.46; P<0.0001), and oxygen consumption at maximum effort (r=0.39; P<0.005). Performances on the 6MST and 6MWT were significantly improved after PR (570 vs 488 steps, P=0.001 and 448 vs 406 m, respectively; P<0.0001). Improvements of the 6MST and 6MWT after PR were significantly correlated (r=0.34; P=0.03).
Conclusion
The results of this study show that the 6MST is a valid test to evaluate exercise tolerance in COPD patients. The use of this test in clinical practice appears to be particularly relevant for the assessment of patients managed by home PR.
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic lung disease marked by breathlessness on exertion, with systemic consequences and an increased risk of disability and death, especially as COPD is frequently associated with comorbidities (cardiovascular disease, obesity, and Type 2 diabetes).Citation1,Citation2 Pulmonary rehabilitation (PR), comprising exercise retraining, resumption of physical activity, therapeutic education, and psychosocial support, is an integral part of the management of COPD patients. This global management allows improvement of dyspnea, exercise tolerance, and quality of life.Citation3–Citation6
Various exercise tests are commonly used to assess the exercise tolerance of patients with lung disease in the context of PR. Cardiopulmonary exercise testing (CPET) is the standard test allowing investigation of the pathophysiological mechanisms responsible for dyspnea and evaluation of aerobic capacity.Citation7 However, CPET requires specialized and expensive equipment and qualified personnel, which limit its availability. The 6-minute walk test (6MWT) is a validated test for most chronic lung diseases; it is easy to perform and does not require any specific equipment. The 6MWT is sensitive and reproducible and is commonly used to evaluate the course of exercise tolerance in the context of out/inpatient PR with a well-defined minimal clinically important difference.Citation8–Citation11 According to the American Thoracic Society (ATS) guidelines,Citation12 the 6MWT must be performed in an unobstructed 30 m hallway, but such a space is rarely available in the patient’s homeCitation13 or in the physician’s office, or even in some respiratory medicine departments. A recent study has however proposed performing the 6MWT over a distance of 10 m.Citation14
To overcome these technical and spatial limitations, a 6-minute stepper test (6MST) has been proposed to evaluate exercise tolerance. This test requires only a limited amount of space and equipment and is feasible, easy to perform, sensitive, well tolerated, and reproducible in COPD patients.Citation15,Citation16 The 6MST has been used to assess exercise tolerance in the context of PR.Citation17,Citation18 However, the correlation between the 6MST and validated indices used to measure exercise capacity (6MWT and CPET) has not yet been established.
The primary objective of this study was to analyze the correlations between exercise tolerance data provided by the 6MST, 6MWT, and CPET in a population of COPD patients managed by outpatient PR. The secondary objective was to analyze and compare the course of exercise tolerance measured by 6MST and 6MWT before and after PR.
Material and methods
This monocentric retrospective study included COPD patients managed by outpatient PR. Patients included in this study were those who had completed the entire PR program and those for whom pre-rehabilitation 6MWT, 6MST, and CPET assessment data were available.
The severity of COPD was evaluated by Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage.Citation19 Patients were divided into two groups according to GOLD stage: mild-to-moderate COPD (Stages 1 and 2) and severe-to-very-severe COPD (Stages 3 and 4).
All data were collected prospectively and were entered into our rehabilitation computerized medical records. The study protocol was approved by the Observational Research Protocol Evaluation Committee of the French Language Society of Pulmonology, France. As the study data was collected as part of a pulmonary rehabilitation program prior to this retrospective study commencing the Observational Research Protocol Evaluation Committee advised written informed consent did not need to be obtained from the patients.
Pulmonary function tests
Spirometry was performed before PR in clinically stable patients, according to European guidelines.Citation20,Citation21
Cardiopulmonary exercise testing
CPET was performed according to an incremental protocol on a cycle ergometer (Ergometrics 800; ergoline, Bitz, Germany), with blood pressure and electrocardiographic monitoring (Medcard; Medisoft®, Dinant, Belgium), according to the usual guidelines.Citation22,Citation23 The protocol included a 3-minute rest period, a 3-minute unloaded pedaling period, an incremental ramp exercise (10–15 W/min) pursued to a symptom-limited end point, and a 3-minute recovery time. Inspired and expired gases were collected by a mouthpiece connected to a gas analyzer (Ergocard, Medisoft®). Maximal oxygen consumption (VO2 max) and oxygen consumption at the ventilatory threshold (VT) were expressed in mL/min/kg. VT was defined by a nonlinear increase in ventilation (VE) during exercise and was determined by the level of effort at which carbon dioxide production (VCO2) increased more rapidly than VO2,Citation24 or by an increase in the respiratory equivalent for oxygen (VE/VO2) with no increase in the respiratory equivalent for carbon dioxide (VE/VCO2).Citation25 All CPET were limited by dyspnea, fatigue, or both and provided at least one objective criterion of maximum among the following: breathing reserve <15%, peak heart rate >90% of predicted, peak lactate >7 mEq/L, peak exercise partial pressure of oxygen (PaO2) in arterial blood <55 mmHg, or peak VE/VO2 >35.Citation22
Six-minute walk test
The 6MWT was performed over a “rectangular” distance of 70 m in the respiratory medicine department. With the exception of this point, the ATS guidelines for 6MWT were followed.Citation12 After resting for 5 minutes, continuous monitoring of transcutaneous oxygen saturation (SpO2) and heart rate by a pulse oximeter (Oxymontre 3100; Nonin®, Plymouth, MN, USA) were performed.
Six-minute stepper test
The 6MST aims at measuring the number of steps performed on a stepper in 6 minutes using a protocol that is equivalent to the 6MWT protocol. A step was defined as a single complete movement of raising one foot and putting it down. The stepper (Go Sport®, Grenoble, France)Citation16 was placed on the ground facing a wall to allow patients to maintain their balance by placing their fingers on the wall. The step height was set at 20 cm. Before starting the test, patients got accustomed to the stepper for 2 minutes. The protocol included a 3-minute rest period and a 6-minute stepping period. Patients received standardized instructions adapted from the 6MWT ATS instructions,Citation15 advising them to make the most number of steps they could in 6 minutes. The number of steps performed in 6 minutes was recorded. Monitoring of heart rate and SpO2 by a pulse oximeter (Oxymontre 3100; Nonin) was performed each minute. An investigator, a member of the paramedical team, remained behind the patient throughout the test.
The 6MST and 6MWT were conducted by the same team to avoid between-investigator variability.
Pulmonary rehabilitation
Patients completed a 6-week course of outpatient PR at a rate of four sessions per week, 3 hours per session, comprising a combination of exercise retraining, therapeutic education, and psychosocial support.Citation6,Citation17
Statistical analysis
Statistical analysis was performed with PRISM software (GraphPad®, La Jolla, CA, USA) and SAS version 9.3 software (SAS Institute, Cary, NC, USA). Quantitative parameters were expressed in terms of mean and standard deviation. Qualitative parameters were expressed in terms of frequencies and percentages. The distribution of quantitative parameters was verified graphically and by a Shapiro–Wilk test.
Pearson’s or Spearman’s correlation coefficient was used to evaluate the correlation between the results of the various tests performed by the patients (CPET, 6MWT, and 6MST). A linear regression was performed to analyze the independent correlation between the 6MST (dependent variable) and the 6MWT distance according to age, body mass index, forced expiratory volume in one second/forced vital capacity (independent variables).
Student’s t-test for paired data or Wilcoxon signed rank test was used to compare the course of the 6MST and 6MWT results before and after PR, according to the distribution of the variables. All tests were initially performed on the overall population, and then according to the severity of COPD exclusively for the 6MST and 6MWT results. The significance level was set at 5%.
Results
One hundred seventy-seven COPD patients were managed by outpatient PR between January 2010 and December 2014. Ninety-one (51%) of these patients completed a pre-rehabilitation assessment comprising all three tests (6MST, 6MWT, and CPET) and were included in this study. Another 86 patients (49%) were excluded due to missing CPET (n=39) or 6MWT data (n=21), or because a stress test rather than CPET was performed (n=26). The characteristics of the 91 patients are presented in .
Table 1 Patient characteristics (n=91)
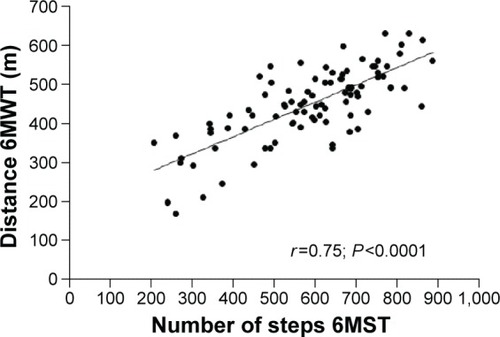
A statistically significant correlation was observed between the number of steps on the 6MST and the distance covered on the 6MWT (r=0.56; P<0.0001; ), independent of the severity of COPD (). This correlation was observed in patients with mild-to-moderate COPD and in patients with severe-to-very-severe COPD (). The number of steps on the 6MST was correlated with power (W) at the VT and at maximum effort, and VO2 max ( and ). Similarly, the distance covered on the 6MWT was correlated with power and VO2 at the VT and at VO2 max (). A linear regression showed that the 6MST was related to the 6MWT distance and peak exercise power, independent of age, lung function, and body mass index ().
Table 2 Test results before PR and correlations
Table 3 Test results before PR according to the severity of COPD and correlations with the 6MST
Table 4 Linear regression using the 6MST as a dependent variable
Figure 1 Correlation between the number of steps on the 6MST and the distance covered on the 6MWT before PR.
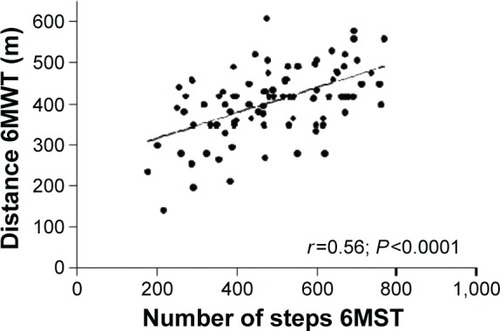
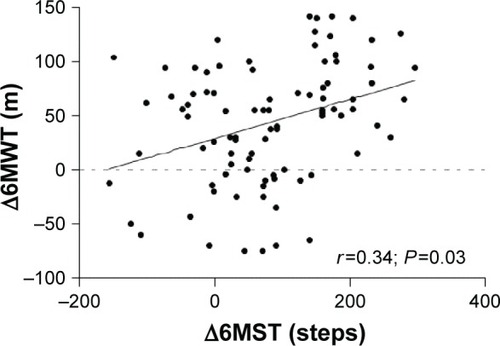
For the overall population, a significant improvement of the 6MWT distance was observed, increasing from 406±86 m before PR to 448±95 m after PR (P<0.0001), together with a significant increase in the number of steps on the 6MST, increasing from 488±149 steps before PR to 570±161 steps after PR (P<0.0001). A statistically significant correlation was observed for all patients between the number of steps on the 6MST and the distance covered on the 6MWT after PR (r=0.75; P<0.0001; ). Subgroup analysis revealed similar results for patients with mild-to-moderate COPD (r=0.77; P<0.0001) and patients with severe-to-very-severe COPD (r=0.76; P<0.0001). As shown in , improvement of the 6MST after PR was correlated with improvement of the 6MWT in all patients (absolute values: r=0.34; P=0.03; ; percentage change: r=0.32; P=0.001).
Discussion
This study shows that the number of steps on the 6MST was significantly correlated with the distance covered on the 6MWT, VO2 max, and power at VT and at maximum effort, independent of the severity of COPD. These results also show a significant correlation between improvements of performances on the 6MWT and 6MST after outpatient PR.
Assessment of exercise tolerance is an integral part of the evaluation of COPD patients during PR.Citation4,Citation6 Despite the demonstrated value of the 6MWT, its technical constraints do not always allow use and regular repetition of this test during patient follow-up, especially in the physician’s or physiotherapist’s office, or at the patient’s home.Citation12,Citation13 Consequently, various teams have developed alternatives to these tests, including the 6MST.
In line with previous studies,Citation15,Citation26 our results demonstrated a significant correlation between the number of steps on the 6MST and the distance covered on the 6MWT. These correlations were independent of the severity of COPD. Delourme et alCitation26 also showed that these correlations remained significant independent of the type of interstitial lung disease (ILD). All of these results indicate that the 6MST can be used in a wide range of patients with varying degrees of severity of chronic lung disease (COPD and ILD).
The 6MWT is considered to be a submaximal test, as the subject is free to walk at his or her own rate, but it has been shown that the most severe COPD patients achieve an identical VO2 to that observed at the end of a cycle ergometer test, by the third minute of walking.Citation27–Citation30 McGavin et alCitation31 have previously validated the 12MWT in COPD patients based on the significant correlation (r=0.52) between the distance covered and VO2 max, as also confirmed by Carter et alCitation32 and, more recently, by Luxton et alCitation33 (r=0.54 and r=0.63, respectively). Similar results have been reported in patients with heart failure (r=0.42) and respiratory insufficiency (r=0.57).Citation34,Citation35 This study demonstrated identical correlations between maximum values obtained during CPET and the distance covered on the 6MWT, as well as the number of steps on the 6MST.
Other clinical tests have been proposed in the literature, such as the stair climbing test,Citation36,Citation37 the sit-to-stand test,Citation38 and the step test (walking up and down a 20 cm platform for a determined duration). Citation39 In a population of COPD patients, the performance on the step test is correlated with the performance on CPET, and the distance covered on the 12MWTCitation40 and the 6MWT.Citation41 We decided to perform this test on a stepper device rather than on a 20 cm platform, because the stepper allows the patient to maintain balance by lightly placing the fingers on the wall, which is more reassuring for elderly patients and/or patients with balance disorders.
Many studies have demonstrated the good sensitivity of the 6MWT at assessing the efficacy of outpatient or home PR in COPD patients.Citation4,Citation6 Lacasse et alCitation3,Citation42 reported gains of 56 and 48 m for outpatient PR and home PR, respectively. No consensus has been reached concerning the minimal clinically important difference (MCID) of the 6MWT: 54 m in the study by Redelmeier et alCitation8 and 35 m9 and 26 m11 in more recent studies. A 14% relative improvement has also been proposed, but appears to be less sensitive than an absolute value of 25 m.Citation10 The gain of 42 m observed in this study is consistent with the data of the literature.Citation8–Citation11 Furthermore, a significant increase in the number of steps on the 6MST (from 488 to 570) was observed not only after outpatient PR (in agreement with previously published results in 30 COPD patients),Citation16 but also after home PR in a population of patients with idiopathic pulmonary fibrosis,Citation43 unselected patients with more severe chronic lung disease (80% on long term oxygen therapy and/or noninvasive ventilation),Citation17 and in COPD patients.Citation18 The mean improvement of 79 steps on the 6MST in this study is superior to the 40-step MCID proposed by Pichon et alCitation44 based on the analysis of the results of 62 COPD patients managed by inpatient PR. The performances on the two clinical exercise tolerance tests were significantly improved after PR: 79 steps on the 6MST and 42 m on the 6MWT, and these improvements were significantly correlated with each other. Coquart et alCitation16 suggested that familiarization with the 6MWT would have an impact on improved performance on the 6MST after PR due to a possible learning effect. However, it should be stressed that the patients in this study did not use the stepper as a retraining tool. The improvements observed on the 6MST were consequently the result of improvement of the subject’s aerobic and muscular capacities. These results suggest that, like the 6MWT,Citation4,Citation6 the 6MST is a sensitive clinical exercise test to assess the efficacy of a PR program on the exercise tolerance of COPD patients.
This study was mainly limited by its retrospective nature. However, there were only a few data missing, and most of the variables were objective measurements collected from standardized tests. Almost half the patients were excluded from the study because all the required examinations were not performed on them. Although this could introduce a selection bias, there was no statistical difference between excluded and included patients concerning demographic, clinical, comorbidities, and pulmonary function data (data not shown).
Conclusion
This study demonstrates not only a correlation between the number of steps on the 6MST and the distance covered on the 6MWT, but also a correlation with power and VO2 max of the CPET for COPD patients regardless of their stage of severity. The improvements on the 6MST and 6MWT observed after PR were also correlated, confirming the value of this new, sensitive, and reproducible test, which is easy to perform without any spatial constraints, for assessment of exercise tolerance in COPD patients, in routine respiratory medicine practice, and especially, before and after short- and long-term PR management.
Disclosure
JM Grosbois received financial support from Adair, France Oxygène, Homeperf, LVL, Orkyn, Santélys, SOS Oxygène, Sysmed, and VitalAire for home-based PR program. The authors report no other conflicts of interest in this work.
References
- VanfleterenLESpruitMAGroenenMClusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2013187772873523392440
- Van RemoortelHHornikxMLangerDRisk factors and comorbidities in the preclinical stages of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20131891303824219412
- LacasseYGoldsteinRLassersonTJMartinSPulmonary rehabilitation for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20064CD00379317054186
- Société de Pneumologie de Langue FrançaiseRecommandations pour la pratique clinique. Prise en charge de la BPCO [Recommendation for the clinical practice management of COPD]Rev Mal Respir201027Suppl 1S1S76IXXXI French20931674
- van RanstDOttenHMeijerJWvan’t HulAJOutcome of pulmonary rehabilitation in COPD patients with severely impaired health statusInt J Chron Obstruct Pulmon Dis2011664765722162650
- SpruitMASinghSJGarveyCAn official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitationAm J Respir Crit Care Med20131888e13e6424127811
- AguilaniuBWallaertBEFX: De L’interprétation à La Décision MédicaleParis, FranceMargaux Orange2015
- RedelmeierDABayoumiAMGoldsteinRSGuyattGHInterpreting small differences in functional status: the six minute walk test in chronic lung disease patientsAm J Respir Crit Care Med19971554127812829105067
- PuhanMAMadorMJHeldUGoldsteinRGuyattGHSchünemannHJInterpretation of treatment changes in 6-minute walk distance in patients with COPDEur Respir J200832363764318550610
- HollandAEHillCJRasekabaTLeeANaughtonMTMcDonaldCFUpdating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary diseaseArch Phys Med Rehabil201091222122520159125
- PuhanMAChandraDMosenifarZThe minimal important difference of exercise tests in severe COPDEur Respir J201137478479020693247
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function LaboratoriesATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med2002166111111712091180
- HollandAERasekabaTFioreJFBurgeATLeeALThe 6-minute walk distance cannot be accurately assessed at home in people with COPDDisabil Rehabil201537121102110625176002
- BeekmanEMestersIGosselinkRThe first reference equations for the 6-minute walk distance over a 10 m courseThorax201469986786824764113
- BorelBFabreCSaisonSBartFGrosboisJ-MAn original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper testClin Rehabil2010241829320053721
- CoquartJBLemaîtreFCastresISaisonSBartFGrosboisJ-MReproducibility and sensitivity of the 6-minute stepper test in patients with COPDCOPD201512553353825526322
- GrosboisJ-MLe RouzicOMongeEBartFWallaertBComparison of home-based and outpatient, hospital-based, pulmonary rehabilitation in patients with chronic respiratory diseasesRev Pneumol Clin20136911017 French23305933
- GrosboisJMGicquelloALangloisCLong term evaluation of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2015102037204426445534
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2007176653255517507545
- QuanjerPHTammelingGJCotesJEPedersenOFPeslinRYernaultJCLung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory SocietyEur Respir J Suppl1993165408499054
- MillerMRHankinsonJBrusascoVStandardisation of spirometryEur Respir J200526231933816055882
- AguilaniuBRichardRCostesFMéthodologie et Pratique de l’Exploration Fonctionnelle à l’eXercice (EFX) [Cardiopulmonary exercise testing]Rev Mal Respir2007243 Pt 22S1112S160 French17389842
- American Thoracic SocietyAmerican College of Chest PhysiciansATS/ACCP statement on cardiopulmonary exercise testingAm J Respir Crit Care Med2003167221127712524257
- BeaverWLWassermanKWhippBJA new method for detecting anaerobic threshold by gas exchangeJ Appl Physiol 19851986606202020273087938
- WassermanKWhippBJKoylSNBeaverWLAnaerobic threshold and respiratory gas exchange during exerciseJ Appl Physiol19733522362434723033
- DelourmeJStervinou-WemeauLSalleronJGrosboisJMWallaertBSix-minute stepper test to assess effort intolerance in interstitial lung diseasesSarcoidosis Vasc Diffuse Lung Dis201229210711223461072
- TroostersTVilaroJRabinovichRPhysiological responses to the 6-min walk test in patients with chronic obstructive pulmonary diseaseEur Respir J200220356456912358329
- TurnerSEEastwoodPRCecinsNMHillmanDRJenkinsSCPhysiologic responses to incremental and self-paced exercise in COPD: a comparison of three testsChest2004126376677315364755
- CasasAVilaroJRabinovichREncouraged 6-min walking test indicates maximum sustainable exercise in COPD patientsChest20051281556116002916
- CoteCGPinto-PlataVMMarinJMNekachHDordellyLJCelliBRThe modified BODE index: validation with mortality in COPDEur Respir J20083251269127418579541
- McGavinCRGuptaSPMcHardyGJTwelve-minute walking test for assessing disability in chronic bronchitisBr Med J1976160138228231260350
- CarterRHolidayDBStocksJGrothuesCTiepBPredicting oxygen uptake for men and women with moderate to severe chronic obstructive pulmonary diseaseArch Phys Med Rehabil20038481158116412917855
- LuxtonNAlisonJAWuJMackeyMGRelationship between field walking tests and incremental cycle ergometry in COPDRespirology200813685686218811884
- GuyattGHSullivanMJThompsonPJThe 6-minute walk: a new measure of exercise capacity in patients with chronic heart failureCan Med Assoc J198513289199233978515
- GuyattGHThompsonPJBermanLBHow should we measure function in patients with chronic heart and lung disease?J Chronic Dis19853865175244008592
- PollockMRoaJBendittJCelliBEstimation of ventilatory reserve by stair climbing. A study in patients with chronic airflow obstructionChest19931045137813838222791
- Villiot-DangerEA stairclimbing test in COPD patients assessmentRev Mal Respir2009265530536 French19543172
- JonesSEKonSSCanavanJLThe five-repetition sit-to-stand test as a functional outcome measure in COPDThorax201368111015102023783372
- Dal CorsoSDuarteSRNederJAA step test to assess exercise-related oxygen desaturation in interstitial lung diseaseEur Respir J200729233033617050559
- SwinburnCRWakefieldJMJonesPWPerformance, ventilation, and oxygen consumption in three different types of exercise test in patients with chronic obstructive lung diseaseThorax19854085815864035628
- PessoaBVArcuriJFLabadessaIGCostaJNSentaninACDi LorenzoVAValidity of the six-minute step test of free cadence in patients with chronic obstructive pulmonary diseaseBraz J Phys Ther201418322823625003275
- LacasseYWongEGuyattGHKingDCookDJGoldsteinRSMeta-analysis of respiratory rehabilitation in chronic obstructive pulmonary diseaseLancet19963489035111511198888163
- RammaertBLeroySCavestriBWallaertBGrosboisJ-MHome-based pulmonary rehabilitation in idiopathic pulmonary fibrosisRev Mal Respir2011287e52e5721943547
- PichonRBeaumontMLe Ber-MoyCPéranLCouturaudFDétermination d’une différence minimale importante pour le stepper-test de six minutes chez les patients atteints de BPCO [Determination of a significant minimal difference for the 6 minute stepper-test in patients with COPD]Rev Mal Respir201532A75 French