Abstract
Background
The aim of the present review is to systematically evaluate the efficacy and safety of pembrolizumab by analyzing survival outcomes and at the same time, to present evidence for future clinical applications of anti-programmed cell death protein 1 (anti-PD-1) antibodies by analyzing the efficacy and safety of pembrolizumab.
Methods
A comprehensive literature search of PubMed, Medline, and Embase was performed for all relevant clinical trials. In this study, adverse events of any grades and grades ≥3 were summarized and calculated for event rates. For controlled trials, odd ratios (ORs) were calculated to determine the role of pembrolizumab in adverse events. The Kaplan–Meier survival curves were extracted for hazard ratio (HR) calculation and survival outcomes were measured by progression-free survival (PFS).
Results
A total of 3,953 patients were included in safety analyses. The results indicated that the overall incidence of any treatment emergent adverse events was 74.3% (95% confidence interval [CI]: 0.671–0.805). The efficacy analysis involving 915 patients with advanced melanoma suggested that 10 mg/kg of pembrolizumab every 3 weeks could improve patients’ PFS (HR =0.73, 95% CI: 0.64–0.83).
Conclusion
Pembrolizumab is a promising therapeutic option that could bring better survival outcomes but, at the same time, leads to higher frequency of some adverse events.
Keywords:
Introduction
Cancer is one of the most lethal health problems worldwide.Citation1 One mechanism that prevents the initiation of effective antitumor responses in cancer microenvironment is immune evasion, which makes the treatment of advanced and refractory cancer difficult.Citation2,Citation3 Programmed cell death protein 1 (PD-1) is a highly expressed immune checkpoint receptor on lymphocytes and plays an important role in regulating T-cell responses to reduce damage to surrounding normal tissues.Citation4,Citation5 PD-1 is also highly expressed on intratumoral TREG cells and might enhance the immunosuppressive activity of these cells.Citation6–Citation9 This process requires the binding of PD-1 to its ligands, PD-L1 or PD-L2, to decrease the production of cytokines and the expression of antiapoptotic proteins, which ultimately suppresses cytotoxic T-cell functions.Citation9 However, PD-L1 is upregulated on many cancer cells, which makes it easier for cells to escape from immune surveillance by inhibiting T-cell responses.Citation10 For this reason, the therapy targeting at PD-1 to maintain T-cell activation is a promising area to be further explored.
Landmark studies have demonstrated the efficacy of anti-PD-1/PD-L1 therapies for patients with metastatic non-small-cell lung cancer (NSCLC), renal cell cancer, urothelial cancer, bladder cancer, colon cancer, and so on.Citation11–Citation20 The first antibodies against the immune checkpoint PD-1 receptors, nivolumab and pembrolizumab, have now been approved for clinical use. However, the preexisting studies only summarized data for certain types of cancersCitation21,Citation22 and the key factors associated with better clinical outcomes still remained unclear. In this study, we systematically evaluated the efficiency and safety of pembrolizumab in patients with tumors of different histological types, which hopefully could help present comprehensive evidence for future clinical applications of anti-PD-1 antibodies.
Methods
Search strategy
A comprehensive literature search of PubMed, Medline, and Embase was performed according to Cochrane guidelinesCitation23 for all relevant clinical trials on the safety and efficacy of pembrolizumab. The latest search was done on October 16, 2016. Keywords included pembrolizumab, safety, efficacy, and clinical trials. In order to ensure the completeness of the results, we also carried out further searches for relevant unpublished trials in the clinical trial registry.Citation24
Inclusion and exclusion criteria
We referred to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The eligible criteria included 1) any phase clinical trials evaluating the efficacy and safety of pembrolizumab whether they had control groups or not; 2) patients in clinical trials had been histologically confirmed of advanced or refractory cancer; and 3) survival or adverse events were reported in the results or available for calculation.
Studies were excluded based on any of the following conditions: 1) review articles, meta-analysis, laboratory articles, or letters; 2) studies of other therapies; and 3) articles not provided with English version. When two articles involved the same medical center and patient cohort, the one with a larger sample size was selected. Two authors independently selected studies, and any disagreements were resolved by consulting a third author.
Data extraction
Data extracted from all eligible articles included 1) the basic information of studies: first author, year of publication, sample size, treatment regime, and study phase; 2) the types of adverse events of any grades and grades ≥3, which were graded according to the National Cancer Institute (Washington, DC, USA) Common Toxicity Criteria, Version 3.0; 3) the number of patients with adverse events in treatment groups and control groups; and 4) hazard ratios (HRs) for progression-free survival (PFS) or overall survival (OS).
Statistical analysis
The safety analysis and efficacy analysis were performed on Comprehensive Meta-Analysis program 2 (Biostat, Englewood, NJ, USA) and Review Manager 5.2 (The Cochrane Collaboration, Copenhagen, Sweden), respectively. For single-arm studies, we calculated the proportion and the corresponding 95% confidence intervals (CIs) of major adverse events (AEs) (both all grades and grade ≥3). For controlled trials, the odds ratio (OR) was calculated to determine the role of pembrolizumab in adverse events’ occurrence. A random-effect model (Der Simonian and Laird method) was applied if heterogeneity was observed (P<0.10 or I2>50%), otherwise the fixed-effect model was used.Citation25 All P-values were two sided, and a P-value of <0.10 was considered to be statistically significant.
Results
Literature search results
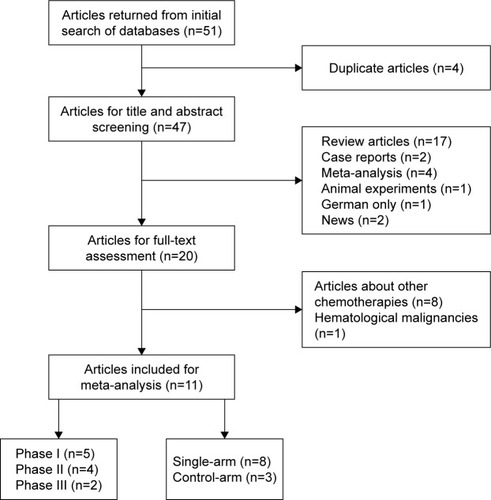
A total number of 51 potentially relevant articles were returned from initial search of PubMed, Medline, and Embase on October 16, 2016, and 47 articles were obtained after the removal of duplicates. After title and abstract screening, 27 articles were excluded as they were review articles, case reports, meta-analysis, animal experiments, or not in English. We then went through full-text screening of the remaining articles. Eight articles were excluded for their concentration on the safety and efficacy of other drugs, and one study about Hodgkin’s lymphoma was also excluded because our analysis was based on solid tumors only. Eleven eligible studiesCitation11,Citation17,Citation26–Citation34 were ultimately enrolled. Studies of the same first authors but with different study designs were enrolled. The flow diagram of the study selection process is provided in .
Study characteristics
Eligible articles included five Phase I, four Phase II, and two Phase III randomized controlled trials or, in another classification, eight single-arm studies and three control-arm studies. Enrolled malignancies were melanoma (six trials), NSCLC (two trials), nonspecific tumors (two trials), and Merkel cell carcinoma (one trial). The baseline characteristics of the 11 included articles are presented in .
Table 1 Basic information of eligible articles
As for single-arm trials, we calculated the incidence of adverse events. As for control-arm studies, two studies with the same treatment regime in treatment groups and analyses of the same cancer type were enrolled in survival meta-analysis to test the efficacy of pembrolizumab. Ribas et alCitation32 set melanoma patients into two groups (pembrolizumab at a dose of 2 or 10 mg/kg every 3 weeks versus investigator-choice chemotherapy). Similarly, Robert et alCitation34 made comparison between pembrolizumab at a dose of 10 mg/kg every 2 or 3 weeks and control therapy to determine the contribution of pembrolizumab in adverse events.
Safety analysis
Overall analysis
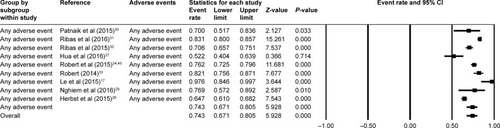
A total number of 3,922 patients were included in the analysis. After investigating all grades and grade ≥3 adverse events, we found that the most frequently occurred events included rash, pruritus, diarrhea, nausea, myalgia, arthralgia, and pneumonitis. The pooled estimate for overall incidence of any treatment emergent adverse events (TEAEs) was 74.3% (95% CI: 0.671–0.805) ().
Individual analysis
In single-arm trials, no significant heterogeneity was found in some of all-grade AEs, so the fixed-effects model was applied (). Among them, dry mouth occurred in 10.0% (95% CI: 0.045–0.206) of participants and 9.8% (95% CI: 0.087–0.111) of patients were observed with decreased appetite. Other AEs of which I2>50 were analyzed with the random-effects model (). Rash (14.8%, 95% CI: 0.102–0.204), pain (13.7%, 95% CI: 0.011–0.689), pruritus (17.7%, 95% CI: 0.128–0.240), arthralgia (11.3%, 95% CI: 0.082–0.153), and vitiligo (11.0%, 95% CI: 0.089–0.169) were common in random-effects model. By comparison, severe events (grade ≥3) were rare. The most frequently presented grade ≥3 TEAEs were hyponatremia (7.5%, 95% CI: 0.031–0.167, fixed model) () and elevation in alanine transaminase (2.6%, 95% CI: 0.006–0.101, random model) ().
Figure 3 Forest plot of all-grade adverse events in single-arm trials.
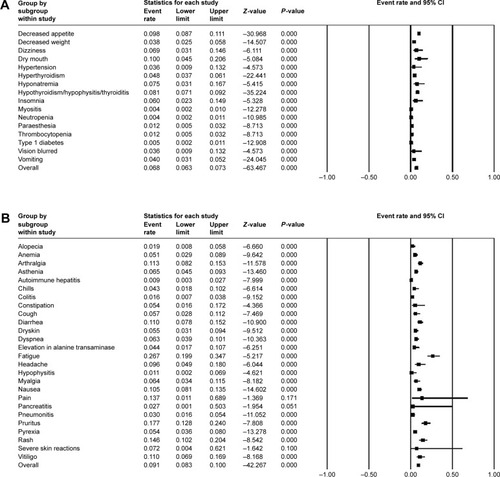
Figure 4 Forest plot of grade ≥3 adverse events in single-arm trials.
Abbreviation: CI, confidence interval.
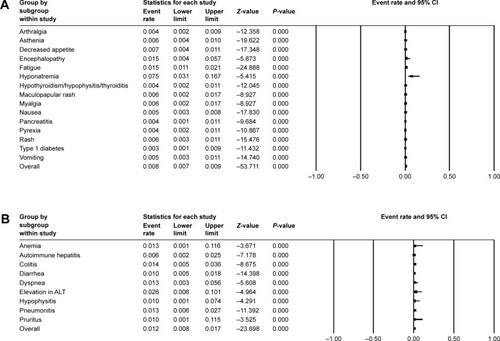
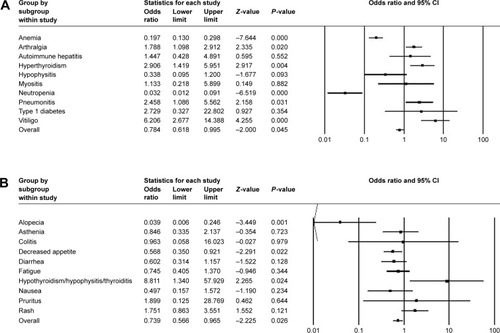
For three control-arm studies, fixed model was applied in all-grade anemia, arthralgia, autoimmune hepatitis, and so on, with OR values () while random model was used in all-grade alopecia, asthenia, colitis, and so on (). Of all the adverse events mentioned earlier, the most frequently occurred events included pruritus (OR =1.899, 95% CI: 0.125–8.769) and rash (OR =1.751, 95% CI: 0.863–3.551). The frequency of hypothyroidism/hypophysitis/thyroiditis was significantly higher in patients treated with control therapy (OR =8.811, 95% CI: 1.340–7.929). Vitiligo of all grades also occurred significantly more often in the pembrolizumab cohort (OR =6.206, 95% CI: 2.677–14.388). Similar trends were observed for event rates of hyperthyroidism (OR =2.906, 95% CI: 1.419–5.951), pneumonitis (OR =2.458, 95% CI: 1.086–5.562), and arthralgia (OR =1.788, 95% CI: 1.098–2.912). Pembrolizumab might have a dominant effect on vitiligo with the highest OR value. Similarly, grade ≥3 adverse events were relatively rare and none demonstrated statistically significant ORs (). Autoimmune hepatitis (OR =2.764, 95% CI: 0.482–15.859) and pneumonitis (OR =2.085, 95% CI: 0.562–7.736) contained 1.0 in their 95% CIs. We were, therefore, unable to determine the effect of pembrolizumab on these events.
Efficacy analysis
Five single-arm trials reported median survival time or survival rates in patients with different types of tumors, demonstrating the antitumor effect of pembrolizumab to some degree without comparison with control groups ().
Table 2 Five single-arm trials demonstrating the efficacy of pembrolizumab without comparison with control groups
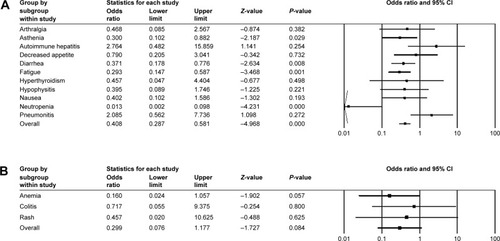
The efficacy of pembrolizumab was analyzed with two controlled trials, which investigated the PFS of 915 patients with advanced melanoma. All patients in treatment groups were treated with pembrolizumab 10 mg/kg every 3 weeks, and we chose 12 months as the endpoint of their survival outcome observations. Robert et alCitation34 reported that the estimated median PFS of patients receiving pembrolizumab was 4.1 months (95% CI: 2.9–6.9) and the HR was 0.58 (95% CI: 0.47–0.72; P<0.001) for pembrolizumab compared to the control therapy. Meanwhile, the study of Ribas et alCitation32 showed significant improvement in PFS, with an HR of 0.50 (95% CI: 0.39–0.64) for 10 mg/kg compared to traditional chemotherapy (P<0.0001). In addition, this effect was likely to be dose dependent, as they observed that, with the same frequency of administration, HR for pembrolizumab 10 mg/kg compared to 2 mg/kg was 0.91 (95% CI: 0.71–1.16). Overall, in comparison with control groups, both high and low doses of pembrolizumab exhibited improvement in patients’ PFS.
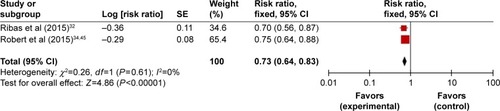
We then carried out meta-analysis based on these two articles. No significant heterogeneity was detected in the comparisons so the fixed-effects model was used (P<0.00001; I2=0). Our exploratory subgroup analyses showed that 10 mg/kg of pembrolizumab every 3 weeks could improve patients’ PFS (HR =0.73, 95% CI: 0.64–0.83) (). Further large-scale studies are still expected to assess the PFS of patients with other types of cancer.
Discussion
The remarkable benefits brought by PD-1 agents pembrolizumab and nivolumab in terms of PFS and OS had been well described, and pembrolizumab has now been considered as front-line therapy in melanoma.Citation35 However, the high cost of these agents should also be taken into consideration. According to the report by Tartari et al,Citation36 the estimated costs associated with the use of pembrolizumab in patients with melanoma and NSCLC were 145,010 $ and 130,511 $ respectively, accounting for the highest per patient costs. Therefore, in order to establish more practical and beneficial clinical strategies, for the first time, we provided in our study the efficacy and safety analysis of pembrolizumab in patients with cancers of different histological types, by analyzing the largest sample size we could reach, and thus offered the most robust summary up to date of adverse events both in pembrolizumab administration groups and control groups.
There are several factors to take into account regarding the addition of pembrolizumab into traditional therapies. First, the genetic mutation was an important factor associated with AEs since the working mechanism of pembrolizumab was based on the interaction between anti-PD-1 antibodies and PD-1.Citation3 Snyder et alCitation37 found that a higher mutational load was related to better survival in patients receiving PD-1 blockade therapy against cutaneous melanoma. Similar results were observed in patients with metastatic melanoma by George et al.Citation47 Meanwhile, Zhang et alCitation38 verified the hypothesis that PD-L1 expression and smoking history were correlated with improved clinical outcomes of anti-PD-1/PD-L1 therapies. Additionally, one potential mechanism of responses to PD-1 inhibition might be related to the specific tumor microenvironment. Tumeh et alCitation39 discovered that patients with higher densities of CD8-positive T cells and higher expression of the T-cell receptors in tumor microenvironment were more likely to present objective responses. However, PD-1 expression on T cells serves as a symbol for T-cell exhaustion, consistent with the observation that the function of tumor-infiltrating lymphocytes expressing PD-1 has been largely reduced.Citation40 Another factor might be the existence of other inhibitory receptors, such as LAG3, TIM3, BTLA, CD160, and CD244.Citation5,Citation13 As a result, blocking PD-1 alone might not be able to fully realize the antitumor function of T cells.
Our study provided information about 3,953 patients from preexisting clinical trials to investigate the increasing risk for the potential adverse events. All-grade rash (14.8%, 95% CI: 0.102–0.204), pain (13.7%, 95% CI: 0.011–0.689), pruritus (17.7%, 95% CI: 0.128–0.240), vitiligo (11.0%, 95% CI: 0.089–0.169), arthralgia (11.3%, 95% CI: 0.082–0.154), and dry mouth 10.0% (95% CI: 0.045–0.206) could happen in patients treated with pembrolizumab-based therapies, while severe event (grade ≥3) rates of rash, pruritus, and arthralgia decreased down to 0.6, 1.0, and 0.4%, respectively. Similarly, control-arm analysis revealed that immune-mediated adverse events mainly affected the skin, musculoskeletal, endocrine, and gastrointestinal systems, including rash, diarrhea, myalgia, and pneumonitis. As for control-arm study, significantly higher risks of all-grade events were observed in pembrolizumab cohort. Thyroid dysfunction was the most common event and was manageable with thyroid hormone replacement therapy. The underlying mechanism of thyroid dysfunction was further unraveled by de Filette et al, by measuring thyroid autoantibodies and analyzing 18F-fluorodeoxyglucose (18FDG)-positron emission tomography/computed tomography imaging. It was suggested that thyroid autoantibodies were present in nearly half of the patients with thyroid dysfunction and, at the same time, increasing 18FDG uptake in the thyroid gland was found in all patients suspected of pembrolizumab-associated thyroiditis.Citation41 However, none of the ORs for severe grade adverse events appeared to be statistically significant, which was consistent with results of previous safety meta-analyses.Citation12,Citation42
We found that the most common events of pembrolizumab therapy were cutaneous adverse effects including rash (14.8%), pruritus (17.7%), and less frequently vitiligo (11.0%). These adverse effects were generally manageable and did not require discontinuation of therapy.Citation43 The exact mechanism of these cutaneous eruptions had not been completely elucidated. The histological findings of Shi et alCitation44 were consistent among two anti-PD-1 agents, nivolumab and pembrolizumab, indicating that the cutaneous reaction might be a targeted effect of the PD-1/PD-L1 pathway rather than a nonspecific hypersensitivity reaction. An alternative explanation was that the administration of anti-PD-1 drug might stimulate immune response to medication that was previously tolerated.
The efficacy analysis was conducted with two controlled trials including 915 patients, of which the treatment group (pembrolizumab 10 mg/kg every 3 weeks) had presented improved PFS (HR =0.73, 95% CI: 0.64–0.83). Similar HRs were observed for PFS in each of the two trials, a finding that reinforces the superiority of pembrolizumab over control therapy. Two recent studies have reported an improvement in OS in patients with BRAFV600 wild-type melanoma receiving nivolumab (another PD-1 blockade therapy) compared to chemotherapy.Citation45 Combined with this finding, our pooled analysis confirmed the remarkable effect of anti-PD-1 therapy on the survival of patients with advanced melanoma. However, given the relatively small number of articles, the evaluation of this effect demanded further research.
To the best of our knowledge, our study is the most up-to-date meta-analysis to assess the efficacy and safety of pembrolizumab in patients with tumors of different histological types including melanoma, NSCLC, Merkel cell carcinoma, and other solid tumors, which hopefully would be applied in future anti-PD-1/PD-L1 immunotherapy practice. PD-1 checkpoint inhibitors are currently under rapid development. Pembrolizumab is one of the earliest US Food and Drug Administration-approved PD-1 checkpoint inhibitors. It is a new, innovative paradigm and has been confirmed of its merits in improving patients’ survival with less toxicity.Citation46 All the included clinical trials were published in the last 2 years, reflecting the popularity of pembrolizumab. Furthermore, in order to avoid selective reporting bias and the incompleteness of included trials, we reviewed all the materials (including supplementary data and relevant publications mentioned). Most included articles were multicentre, international (Australia, Canada, France, and the USA), randomized clinical trials, which offers great credibility in future application.
However, some details of our study need to be further refined. Pembrolizumab is a relatively new kind of drug, which leads to the insufficiency of clinical trials for pooled safety analysis. For the same reason, publication bias and sensitivity analyses were not performed. High levels of heterogeneity existed in several adverse events, which might be the result of the heterogeneity of patients’ profiles and treatment backgrounds. Finally, included trials failed to separate outcomes by patients’ characteristics. We were therefore unable to detect the potential correlation between survival and patients’ gender, age, or pembrolizumab dosages by subgroup analyses.
Conclusion
Pembrolizumab is a promising therapeutic option and was shown, in our analysis, to cause higher frequency of some adverse events. The questions addressed in this meta-analysis could currently not be answered with preexisting data. Future studies, therefore, are needed to draw definitive conclusions about the efficacy and safety of pembrolizumab, which could in turn help inform decision-making in clinical practice.
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRLMillerKDJemalACancer statistics, 2015CA Cancer J Clin2015651 5 2925559415
- HanahanDWeinbergRAHallmarks of cancer: the next generationCell2011144 646 67421376230
- MellmanICoukosGDranoffGCancer immunotherapy comes of ageNat Clin Pract Oncol20112 480 489
- NishimuraHNoseMHiaiHMinatoNHonjoTDevelopment of lupus-like autoimmune diseases by disruption of the PD-1 gene encoding an ITIM motif-carrying immunoreceptorImmunity199911 14110485649
- PardollDMThe blockade of immune checkpoints in cancer immunotherapyNat Rev Cancer201212 25222437870
- FranciscoLMSagePTSharpeAHThe PD-1 pathway in tolerance and autoimmunityImmunol Rev2010236 219 24220636820
- OkazakiTChikumaSIwaiYFagarasanSHonjoTA rheostat for immune responses: the unique properties of PD-1 and their advantages for clinical applicationNat Immunol201314 1212 121824240160
- FifeBTPaukenKEEagarTNInteractions between PD-1 and PD-L1 promote tolerance by blocking the TCR-induced stop signalNat Immunol20091011 1185 119219783989
- FreemanGJPaukenKEEagarTNEngagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activationJ Exp Med2000192 1027 103411015443
- DongHStromeSESalomaoDRTumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasionNat Med200288 793 80012091876
- GaronEBRizviNAHuiRPembrolizumab for the treatment of non–small-cell lung cancerN Engl J Med2015372 2018 202825891174
- GettingerSNHornLGandhiLOverall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non–small-cell lung cancerJ Clin Oncol20153318 200425897158
- BergerRRotem-YehudarRSlamaGPhase I safety and pharmacokinetic study of CT-011, a humanized antibody interacting with PD-1, in patients with advanced hematologic malignanciesClin Cancer Res20081410 3044 305118483370
- ArmandPNaglerAWellerEADisabling immune tolerance by programmed death-1 blockade with pidilizumab after autologous hematopoietic stem-cell transplantation for diffuse large B-cell lymphoma: results of an international phase II trialJ Clin Oncol20113133 4199 4206
- HamanishiJMandaiMIkedaTSafety and antitumor activity of anti–PD-1 antibody, nivolumab, in patients with platinum-resistant ovarian cancerJ Clin Oncol20153334 4015 402226351349
- AnsellSMLesokhinAMBorrelloIPD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphomaN Engl J Med20153724 311 31925482239
- LeDTUramJNWangHPD-1 blockade in tumors with mismatch-repair deficiencyCôlon Rectum201537226 2509
- MotzerRJRiniBIMcDermottDFNivolumab for metastatic renal cell carcinoma: results of a randomized phase II trialJ Clin Oncol20153313 1430 143725452452
- McDermottDFDrakeCGSznolMSurvival, durable response, and long-term safety in patients with previously treated advanced renal cell carcinoma receiving nivolumabJ Clin Oncol20153318 2013 202025800770
- PowlesTEderJPFineGDMPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancerEur Urol2014515 558 562
- JiaMFengWKangSEvaluation of the efficacy and safety of anti-PD-1 and anti-PD-L1 antibody in the treatment of non-small cell lung cancer (NSCLC): a meta-analysisJ Thorac Dis201573 455 46125922725
- YangYPangZDingNThe efficacy and potential predictive factors of PD-1/PD-L1 blockades in epithelial carcinoma patients: a systematic review and meta analysisOncotarget2015745 74350 74361
- DaiHQiAAnalysis of performance of reinforced concrete frame structure with staircase based on ETABSJ Earthq Eng Eng Vib200929 136 142
- RichyFScarpignatoCLanasAReginsterJYEfficacy and safety of piroxicam revisited: a global meta-analysis of randomised clinical trialsPharmacol Res2009604 254 26319467328
- DersimonianRLairdNMeta-analysis in clinical trials revisitedContemp Clin Trials201545pt A 139 14526343745
- HerbstRSBaasPKimDWPembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trialLancet201510 1540
- HuaCBoussemartLMateusCAssociation of vitiligo with tumor response in patients with metastatic melanoma treated with PembrolizumabJAMA Dermatol20161521 45 5126501224
- KarydisIChanPYWheaterMArriolaESzlosarekPWOttensmeierCHClinical activity and safety of Pembrolizumab in ipilimumab pre-treated patients with uveal melanomaOncoimmunology201655 e114399727467964
- NghiemPTBhatiaSLipsonEJPD-1 blockade with Pembrolizumab in advanced merkel-cell carcinomaN Engl J Med201637426 2542 255227093365
- PatnaikAKangSPRascoDPhase I study of Pembrolizumab (MK-3475; anti–PD-1 monoclonal antibody) in patients with advanced solid tumorsClin Cancer Res20152119 4286 429325977344
- RibasAHamidODaudAAssociation of Pembrolizumab with tumor response and survival among patients with advanced melanomaJAMA201631515 1600 160927092830
- RibasAPuzanovIDummerRPembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trialLancet Oncol2015168 908 91826115796
- RobertCRibasAWolchokJDAnti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trialLancet20143849948 1109 111725034862
- RobertCSchachterJLongGVKEYNOTE-006 InvestigatorsPembrolizumab versus ipilimumab in advanced melanomaN Engl J Med201537226 2521 253225891173
- ShoushtariANMunhozRRKukDThe efficacy of anti-PD-1 agents in acral and mucosal melanomaCancer201612221 3354 336227533633
- TartariFSantoniMBurattiniLMazzantiPOnofriABerardiREconomic sustainability of anti-PD-1 agents nivolumab and Pembrolizumab in cancer patients: recent insights and future challengesCancer Treat Rev201648 20 2427310708
- SnyderAMakarovVMerghoubTGenetic basis for clinical response to CTLA-4 blockade in melanomaN Engl J Med2015372 783
- ZhangTXieJAraiSThe efficacy and safety of anti-PD-1/PD-L1 antibodies for treatment of advanced or refractory cancers: a meta-analysisOncotarget2016745 73068 7307927683031
- TumehPCHarviewCLYearleyJHPD-1 blockade induces responses by inhibiting adaptive immune resistanceNature20145157528 568 57125428505
- MedinaPJAdamsVRPD-1 pathway inhibitors: immuno-oncology agents for restoring antitumor immune responsesPharmacotherapy2016363 317 33426822752
- de FiletteJJansenYSchreuerMIncidence of thyroid-related adverse events in melanoma patients treated with PembrolizumabJ Clin Endocrinol Metab201610111 4431 443927571185
- WestinJRChuFZhangMSafety and activity of PD1 blockade by pidilizumab in combination with rituximab in patients with relapsed follicular lymphoma: a single group, open-label, phase 2 trialLancet Oncol2014151 69 7724332512
- RizviNAMazièresJPlanchardDActivity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trialLancet Oncol2015163 25725704439
- ShiVJRodicNGettingerSClinical and histologic features of lichenoid mucocutaneous eruptions due to anti-programmed cell death 1 and anti-programmed cell death ligand 1 immunotherapyJAMA Dermatol201615210 1128 113627411054
- RobertCLongGVBradyBNivolumab in previously untreated melanoma without BRAF mutation – NEJMN Engl J Med20153724 320 33025399552
- RamelyteESchindlerSADummerRThe safety of anti PD-1 therapeutics for the treatment of melanomaExpert Opin Drug Saf2017161 41 5327737598
- GeorgeSMiaoDDemetriGDLoss of PTEN is associated with resistance to anti-PD-1 checkpoint blockade therapy in metastatic uterine leiomyosarcomaImmunity2017462 197 20428228279