Abstract
Psoriasis is a chronic inflammatory disease affecting up to 3% of the general population, associated with discomfort and impaired quality of life. In recent years, the pathogenic cytokine network of psoriasis has been extensively studied leading to the development of new treatments that provide greater efficacy. Interleukin 17A (IL-17A) has been recognized as a crucial cytokine that mediates immunopathogenesis of psoriasis. Ixekizumab – indicated for the treatment of adults with moderate-to-severe plaque psoriasis – is a subcutaneously administered humanized monoclonal antibody that targets IL-17A. A large percentage of patients affected by psoriasis achieved consistent benefits in terms of disease control and rapid onset of action during clinical trials. Overall, ixekizumab brought clinical improvement and a favorable safety profile in phase III trials. Ixekizumab is characterized by consistent efficacy and rapid onset of response; it is not influenced by previous exposure to biologics and has shown good results in areas that are difficult to treat and in severe clinical variants of psoriasis. Ixekizumab has shown significant improvements in the activity of the disease and in those physical functions that inhibit radiographic progression in patients with concomitant involvement of joints. Our data support ixekizumab as a successful therapeutic option for patients affected by moderate-to-severe plaque-type psoriasis.
Introduction
Psoriasis is a chronic inflammatory disease affecting up to 3% of the general population. It is clinically characterized by epidermal hyperproliferation leading to erythematous-squamous skin plaques. Up to 30% of psoriatic patients may also suffer from seronegative spondyloarthritis.Citation1
Psoriasis is nowadays considered a systemic disorder that needs a multidisciplinary approach and an appropriated treatment taking into account different comorbidities. Indeed, several studies demonstrated the association between psoriasis and a number of disease-related comorbidities including blood hypertension and cardiovascular diseases, obesity, type II diabetes, dyslipidemia – singularly or combined in order to configure the metabolic syndrome – nonalcoholic fatty liver disease, anxiety, depression, and inflammatory bowel disease.Citation2–Citation6
Psoriasis has been reported to have a notable impact on social relationships, mental health, and work-related activities.Citation6,Citation7 Although new molecules have been discovered in the last 2 decades leading to an improvement in the quality of life of patients as well as in skin and joint symptoms, the disease is still not controllable in many patients, in particular in case of long-term patients.Citation8
Recent discoveries regarding the pathogenesis of the disease have enabled the identification of some new promising targets for psoriasis treatment, particularly interleukin 17 (IL-17).Citation9,Citation10
This review will focus on ixekizumab, an anti-IL-17 human monoclonal antibody.
Role of IL-17 in the pathogenesis of plaque-type psoriasis
IL-17 is a family of proinflammatory cytokines first described by Yao et al and comprising IL-17A, IL-17B, IL-17C, IL-17D, IL-17E, and IL-17F secreted by T cells, natural killer cells, mast cells, and neutrophils.Citation11,Citation12 IL-17A represents the most investigated cytokine of this family. It is involved in host defense against infections and is implicated in various inflammatory disorders including autoimmune diseases, metabolic disorders, and cancer. IL-17A promotes many events that lead to inflammation, neutrophil recruitment, and host defense throughout the secretions of a multiplicity of molecules as cytokines, chemokines, acute-phase proteins, antimicrobial peptides, mucins, and matrix metalloproteinases.Citation12,Citation13
IL-17A is produced predominantly by Th (T helper) 17 cells, a subset of CD4+ T cells. An aberrant production of IL-17A is strongly related to the pathogenesis of psoriasis and other autoimmune diseases such as rheumatoid arthritis, chronic noninfectious uveitis, and Crohn’s disease. The block of IL-17A represents a potential target in the treatment of a number of autoinflammatory disorders.Citation13 Furthermore, the role of IL-17 in the pathogenesis of psoriatic arthritis (PsA) was assumed when increased levels of IL-17 and tumor necrosis factor alpha (TNF-α) mRNA expression were observed in the synovial liquid of patients affected by rheumatoid arthritis.Citation14 Thereafter, several studies described the relation between IL-1–17, TNF-α, IL-6, IL-1, and IL-8 demonstrating that IL-17 enhances TNF-α-induced synthesis of interleukins 1, 6, and 8 in skin and synovial fibroblasts acting as a “fine-tuning cytokine” in a functional cooperation mediated by CCAAT/enhancer binding protein family members.Citation15–Citation19 Finally, it has been demonstrated that IL-17 induces cartilage collagen breakdown and is involved in osteoclastogenesis and bone resorption through the activation of nuclear factor kappa B ligand.Citation20–Citation22
Plaque-type psoriasis has been historically considered as a Th1-mediated disease despite increasing evidence suggesting the significance of the IL-23/T17 axis as a key pathogenic pathway.Citation23–Citation25 In particular, elevated levels of IL-17A, IL-17F, IL-22, and IL-23 were detected in human lesional skin,Citation26–Citation29 while circulating levels of T17 signature cytokines were higher in psoriatic patients compared to healthy subjects and correlated to the severity of disease.Citation30,Citation31
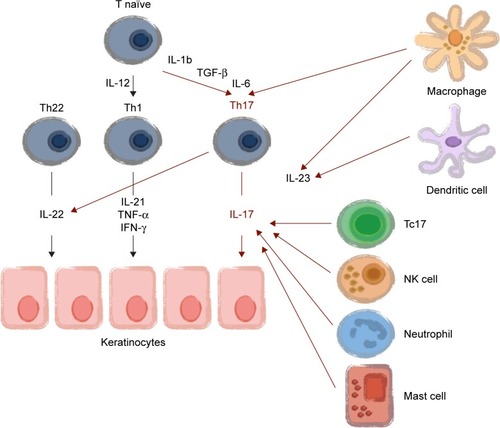
In brief, the main steps involving IL-17 in the pathogenesis of psoriasis are 1) naïve T cell differentiating into Th17 through interaction with activated dendritic cells (DCs) in the presence of IL-23; 2) Th17 producing IL-17A and IL-17F; and 3) keratinocyte stimulated by IL-17 ligands leading to aberrant differentiation and proliferation that promote the production of proinflammatory chemokines; and 4) angiogenic factors that stimulate further recruitment of inflammatory cells, setting up a positive feedback loop ().Citation32 In particular, it has been demonstrated that IL-23 produced by DCs and keratinocytes can induce IL-17A production by Th17 cells, Tc17 cells, γδ T cells, and innate cell subsets (mast cells and neutrophils). Furthermore, blood-derived ILC3 can produce IL-17A that activates fibroblasts to produce IL-6, IL-8, granulocyte colony-stimulating factor, and keratinocytes to produce IL-1β, IL-6, IL-8, IL-17A, and TNF-α, the latter being produced by several cell types including keratinocytes, DCs, and Th1 and Th17 cells. This cytokine cascade has an additive effect on keratinocytes leading to chemokines and AMP (including cathelicidin). Cathelicidin can bind to self-DNA- and self-RNA-forming complexes, which, respectively, trigger TLR9 and TLR7 activation in plasmacytoid DCs (pDCs). This is perceived as a danger signal, breaks immunological tolerance, and leads to the activation of pDCs and IFN-α secretion, and as a consequence, inflammasome and T-cell activation. IL-22 – produced among others by TH17/Th22 cells – contributes to the onset of psoriasis by inducing keratinocyte proliferation and maturation.Citation27,Citation30
Figure 1 IL-17 in the pathogenesis of plaque-type psoriasis. Copyright ©2014. Dove Medical Press. Modified from Lønnberg AS, Zachariae C, Skov L. Targeting of interleukin-17 in the treatment of psoriasis. Clin Cosmet Investig Dermatol. 2014;7:251–259.Citation32
Ixekizumab and IL-17A target therapies
Based on these observations on the role of Th17 cells in psoriasis and PsA, three targeted agents, namely secukinumab, ixekizumab, and brodalumab, were developed. Secukinumab is a fully human IgG1κ monoclonal antibody approved by the Food and Drug Administration and the European Medicines Agency for the treatment of plaque psoriasis, PsA, and ankylosing spondylitis.Citation33 Brodalumab is an IgG2 against IL-17 receptor, binding with high affinity to human IL-17RA, now undergoing phase III studies.Citation34
Ixekizumab is an anti-IL-17A hinge-modified humanized immunoglobulin G subclass-4 (IgG4) antibody indicated for the treatment of moderate-to-severe plaque-type psoriasis.Citation35,Citation36 This molecule was assembled as a humanized IgG4 isotype to decrease the potential risk of immunogenicity caused by repeated administrations.Citation36 Ixekizumab binds to human IL-17A at a conformational epitope, neutralizing the proinflammatory effect of IL-17A/F heterodimers in cell-based assays.Citation37 It is administered subcutaneously; its recommended dose is 160 mg at baseline, followed by 80 mg in weeks 2, 4, 6, 8, 10, and 12. After that, a maintenance dose of 80 mg is administered every 4 weeks. The mean elimination half-life is 10.5 days.Citation25
Clinical trials on plaque-type psoriasis
Phase I
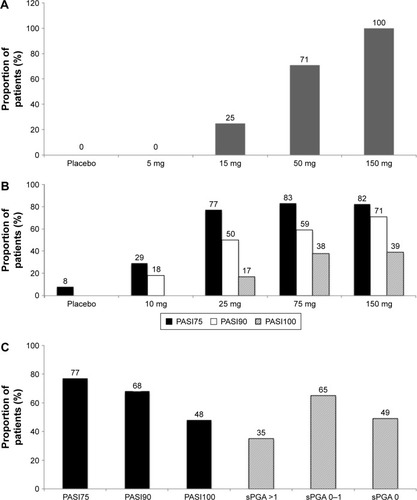
The first phase I, randomized, double-blind, placebo-controlled, dose-escalation study on the safety and possible efficacy of ixekizumab in chronic moderate-to-severe plaque-type psoriasis was published in 2012 by Krueger et al.Citation25 Ixekizumab was administered to 32 subjects with plaque psoriasis by subcutaneous injection across a range of doses from 5 to 150 mg in weeks 0, 2, and 4. Eight subjects received placebo injections at the same time points. Patients were evaluated both clinically and histologically by skin biopsies taken before treatment and in weeks 2 and 6. Histological evaluation demonstrated a marked reduction of both dermal infiltration of T cells and DCs and epidermal hyperplasia compared to baseline. Clinical efficacy, expressed as proportion of patients achieving a reduction in Psoriasis Area and Severity Index (PASI) score of at least 75% from baseline (PASI75), has been summarized in . In week 6, 25%, 71%, and 100% of patients receiving 15, 50, and 150 mg, respectively, achieved PASI75. None of the patients receiving ixekizumab 5 mg achieved the efficacy endpoint.
Figure 2 Efficacy of ixekizumab in phase I and phase II trials.
Abbreviations: PASI, Psoriasis Area and Severity Index; sPGA, static Physician Global Assessment.
Phase II
Two phase II trials investigated the efficacy and safety of ixekizumab in the treatment of plaque-type psoriasis. In 2012, Leonardi et al, evaluated 142 patients affected by chronic moderate-to-severe plaque psoriasis in a double-blind, multicenter, randomized, dose-ranging study. The subjects were randomly assigned to receive subcutaneous injections of placebo or 10, 25, 75, or 150 mg of ixekizumab in weeks 0, 2, 4, 8, 12, and 16.Citation38
The primary objectives were to assess whether ixekizumab was superior to placebo, by measuring the proportion of patients who achieved PASI75 in week 12, and to estimate the percentage of reduction in the PASI score in each treatment group. The secondary objective included the proportion of patients with a reduced PASI score of at least 90% or 100% over the baseline value (PASI90 and PASI100, respectively), and the evaluation of the static physician’s global assessment, joint pain visual analog scale, Nail Psoriasis Severity Index (NAPSI), and Psoriasis Scalp Severity Index (PSSI). The resulting efficacy outcomes of the study have been summarized in .
Subsequently, a multicenter, open-label extension (OLE) of this phase II, randomized, placebo-controlled trial (RCT) was designed to evaluate the long-term (52 weeks) efficacy and safety of ixekizumab.Citation39 Patients received ixekizumab (10, 25, 75, or 150 mg) or placebo subcutaneously in weeks 0, 2, 4, 8, 12, and 16 of the RCT. In week 20 of the RCT, patients who did not reach PASI75 were eligible to enter the OLE and initiate monthly ixekizumab treatment. All other patients entered a treatment-free period from week 20 to week 32 and became eligible to enter the OLE at the study visit if PASI75 was lost or in week 32 if PASI75 or higher improvement was maintained throughout the treatment-free period. All patients were administered 120 mg of ixekizumab subcutaneously every 4 weeks. Before entering the OLE, 69 of 120 (58%) patients had achieved PASI75 in week 20 of the RCT and entered a treatment-free period from week 20 to 32. Of these 69 patients, 45 (65%) maintained a PASI75 response through the treatment-free period and entered the OLE in week 32. Twenty-four (35%) patients entered the OLE before week 32 when their response was lower than PASI75. The remaining 51 patients were nonresponders in the RCT and entered the OLE in week 20. Efficacy was evaluated in week 52 through PASI and static Physician Global Assessment (sPGA). The observed results have been summarized in . Interestingly, the patients assigned to placebo during the RCT who did not achieve PASI75 were responsive during the OLE. In fact, a PASI75 response was observed in 95% (18 of 19), a PASI90 response was observed in 95% (18 of 19), and a PASI100 response was observed in 63% (12 of 19) of these patients.
Phase III
Three major multicenter, randomized, double-blind, placebo-controlled, parallel-group phase III studies have been published, namely UNCOVER-1, UNCOVER-2, and UNCOVER-3.Citation40 Of these, UNCOVER-1 evaluated ixekizumab versus placebo, while UNCOVER-2 and UNCOVER-3 had an active comparator (etanercept). In these trials, investigators randomly assigned 1,296 patients to UNCOVER-1, 1,224 patients to UNCOVER-2, and 1,346 patients to UNCOVER-3.
UNCOVER-1 was a prospective, double-blind, multicenter trial investigating the efficacy of ixekizumab on inducing psoriasis clearance in 12 weeks on 1,296 patients. Subjects were randomly distributed in a 1:1:1 ratio to receive placebo or 80 mg ixekizumab every 2 weeks (Q2W), 80 mg ixekizumab every 4 weeks (Q4W) after an initial dose of 160 mg at week 0, respectively. Response to ixekizumab during the 12-week induction period has been summarized in .
Figure 3 Efficacy of ixekizumab in phase III trials.
Abbreviations: Q2W, every 2 weeks; Q4W, every 4 weeks; PASI, Psoriasis Area and Severity Index; sPGA, static Physician Global Assessment; ETA, etanercept.
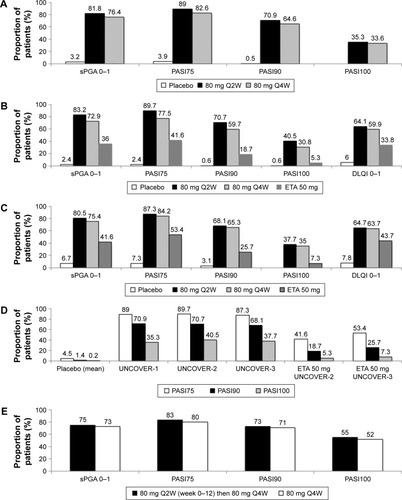
In week 12, ixekizumab-responsive patients (sPGA 0 or 1) were randomly reassigned to receive placebo, 80 mg of ixekizumab Q4W, or 80 mg of ixekizumab every 12 weeks up to week 60.
UNCOVER-2 was a prospective, double-blind, multi-center 12-week study on 1,224 patients randomly distributed in a 2:2:2:1 ratio to receive subcutaneous placebo, etanercept (50 mg twice weekly), or one injection of 80 mg ixekizumab every 2 weeks, or every 4 weeks after a 160 mg starting dose. In addition to the co-primary endpoints of UNCOVER-1 (PASI75, 90, and 100, and sPGA 0 or 1 at week 12), this trial evaluated itch numeric rating scale and Dermatology Life Quality Index as secondary endpoints. The above-mentioned study design was repeated in the UNCOVER-3 trial for the first 12 weeks. Efficacy data in week 12 of UNCOVER-2 and UNCOVER-3 trials have been summarized in , respectively. A summary of ixekizumab 12-week efficacy observed in UNCOVER-1 and UNCOVER-2 trials is presented in .
In addition, UNCOVER-1 and UNCOVER-2 designs have an adjunctive randomized withdrawal period analysis from week 12 to week 60, while patients in the UNCOVER-3 trial received continuous treatment of ixekizumab from week 0 to 60. The latter data have been summarized in .
A subanalysis of UNCOVER studies focused on scalp psoriasis demonstrated that in patients with moderate-to-severe psoriasis with baseline scalp involvement, PSSI 90 and 100 were achieved in week 12 in a higher percentage of patients treated with ixekizumab Q2W (81.7% and 74.6%) or ixekizumab Q4W (75.6% and 68.9%) compared with patients treated with placebo (7.6% and 6.7%; P<0.001 each ixekizumab arm vs placebo) or etanercept (55.5% and 48.1%; P<0.001 each ixekizumab arm vs etanercept). These outcomes were maintained in week 60 of the maintenance period of UNCOVER-1 and UNCOVER-2 trials.Citation41
Similar results have been reported when a subanalysis focused on nail psoriasis was performed.Citation42 In week 12, ixekizumab Q2W or Q4W resulted in a greater improvement in nail psoriasis than placebo or etanercept, as measured by NAPSI reduction percentage (ixekizumab Q2W 39% improvement, ixekizumab Q4W 40%, etanercept 28%, placebo −4.7%). In week 24, a lot more patients receiving ixekizumab showed no signs of nail involvement (34% and 30% in ixekizumab Q2W for 12 weeks then Q4W and ixekizumab Q4W, respectively).Citation42,Citation43
In addition to classical efficacy measures, a revision of UNCOVER trials data by Armstrong et al described the effect of ixekizumab on work productivity, measured by the Work Productivity and Activity Impairment–Psoriasis (WPAI-PSO).Citation44 The WPAI-PSO questionnaire was administered at baseline, at week 12 and at weeks 24, 36, 52, and 60. The results of the questionnaire demonstrated that ixekizumab-treated patients had less impairment in work productivity than placebo-treated patients, and, within some items, less impairment than etanercept-treated patients.
Finally, UNCOVER-J was a phase III, multicenter, single-arm, open-label, long-term Japanese study. Eighty milligrams Q2W of ixekizumab was administered after a first dose of 160 mg. Subsequently, a maintenance dose of 80 mg Q4W ixekizumab was administered. A total of 91 patients were enrolled, including 78 affected by moderate-to-severe plaque psoriasis, eight by erythrodermic psoriasis, and five by generalized pustular psoriasis. UNCOVER-J confirmed the efficacy in Japanese patients of ixekizumab (98.7% of patients achieved PASI75) and suggest that ixekizumab could be clinically useful in patients with less common forms of psoriasis. However, the study population and the absence of controls represent a limit for this study.Citation45
Clinical trials on PsA
Phase III data from the SPIRIT-P1 study showed that ixekizumab is safe and effective for the treatment of PsA, even though the included patients were naïve to biologics, including TNF-α inhibitors.Citation46 The ongoing SPIRIT-P2 trial will provide data on patients previously exposed to biologics.
The SPIRIT-P1 study is a 3-year, phase III, randomized, double-blind, placebo-controlled and active-controlled trial, comparing two different regimens of ixekizumab with an active reference arm treated with adalimumab. The trial involved 417 patients randomized up to 24 weeks in four arms: 1) placebo (N=106); 2) adalimumab 40 mg biweekly (N=101); 3) ixekizumab 80 mg biweekly (N=103); or 4) 80 mg every 4 weeks (N=107) following 160 mg initial dose. Among the 417 included subjects, 382 patients completed the 24-week study. Results demonstrated the significant efficacy of ixekizumab 80 mg biweekly and ixekizumab 80 mg every 4 weeks versus placebo in terms of ACR 20, ACR50, ACR70, and PASI 75/90/100 both after 12 and 24 weeks (P<0.01). Furthermore, both ixekizumab regimens were effective versus placebo in reducing dactylitis after 12 and 24 weeks. Furthermore, the authors observed a significant improvement of disease activity and physical function, and the inhibition of PsA radiographic progression (modified Total Sharp Score [mTSS]).
Safety
Ixekizumab has been reported to be generally well tolerated without any organ toxicity. Severe adverse events were reported in <2% of treated patients considering all the published studies.Citation38–Citation49 There were no deaths, and overall, an equal safety profile was observed between biologic-naïve and biologic-experienced patients.Citation40,Citation50 Severe adverse events were uncommon, with nasopharyngitis and upper-respiratory-tract infections as the most commonly reported. Nevertheless, they were equal among all treatment groups, indicating no added risk of these events attributable to ixekizumab. One major adverse cardiovascular event (MACE) was described in an ixekizumab-treated patient; similar adverse events were reported also in an etanercept-treated patient and in a placebo-treated patient.Citation40 These observations suggest that there is no specific risk for MACE determined by ixekizumab. One rectal cancer was reported in the long-term phase II trial.Citation39 Furthermore, one patient experienced worsening of ulcerative colitis and one reported a new onset Crohn’s disease during the first 12 weeks of treatment.Citation48
There have been no suicides in psoriasis patients treated with ixekizumab; in contrast, two cases of suicide occurred in Brodalumab trials.Citation40 Consistently with basic science data, Candida mucocutaneous infections have occurred in ixekizumab-treated patients, as observed with other anti-IL-17A agents.Citation51 Fungal infection seems to be related with higher doses of ixekizumab. They have been reported to be easily manageable with standard antimicrobial drugs; thus, none of the patients withdrew from the ixekizumab therapy.Citation40 In summary, the safety profile of ixekizumab is encouraging and consistent with its mechanism of action.Citation49
Use in therapy and conclusion
Since their introduction in clinical practice, biologics have raised the bar of therapeutic outcomes in psoriasis even though they are not effective in every case and a loss of response over time has been reported, particularly for monoclonal antibodies.Citation51
Ixekizumab has proved to be significantly more effective than the soluble anti-TNF-α receptor in clearing plaque-type psoriasis with effects that are maintained in time.Citation40,Citation49,Citation51,Citation52
The rapid onset of response determines a substantial gain in the patients’ quality of life and work productivity.Citation40,Citation44 Furthermore, its efficacy has been confirmed also in difficult-to-treat areas (ie, scalp and nails)Citation44–Citation46 and severe clinical variants of psoriasis (ie, erythrodemic psoriasis).Citation41–Citation43,Citation45 Besides, ixekizumab has shown significant improvements in the activity of skin disease and in inhibiting radiographic progression in patients with concomitant iarthritis.Citation46
The efficacy of ixekizumab is high both in patients with and without previous exposure to biologics.Citation51 In particular, after switching to ixekizumab a substantial proportion of patients with moderate-to-severe psoriasis who did not respond to etanercept experienced rapid and durable improvement.Citation48
It is difficult to estabilish an algorithm for sequential treatment in psoriasis patients since there are limited data on the efficacy of an anti-IL-17 agent in patients experiencing anti-TNF-alpha failure in real life.Citation52,Citation53 Nevertheless, currently available phase I–III data indicate that ixekizumab is a promising drug, although long-term data on the efficacy and safety and real-world data are needed before ixekizumab and other IL-17-targeting agents can find their place in clinical practice.Citation49,Citation52
Ixekizumab is an effective drug with a good safety profile and multiple target profile. It could be useful in patients with severe forms and multiple previous failures (second-/third-line biologic) as well as a first-line biologic agent for the treatment of moderate-to-severe plaque-type psoriasis in patients unresponsive or contraindicated to conventional systemic agents.
Disclosure
A Giunta has served as a consultant and a speaker for Abbvie, Pfizer. MS Chimenti has served as a consultant and a speaker for Abbvie and Pfizer. M Esposito has served as a consultant and a speaker for Abbvie, Biogen, Novartis, Eli-Lilly, Pfizer. L Bianchi has served as a consultant, speaker, and a board member for Abbvie, Celgene, Janssen, Novartis, Pfizer, and UCB. A Ventura reports no conflicts of interest in this work.
References
- ParisiRSymmonsDPGriffithsCEAshcroftDMIdentification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project teamGlobal epidemiology of psoriasis: a systematic review of incidence and prevalenceJ Invest Dermatol20131332 377 38523014338
- GordonKBStroberBEUnderstanding therapeutic pathways and comorbidities in psoriasisSemin Cutan Med Surg2014332 Suppl 2 S20 S2324979540
- DavidoviciBBSattarNPrinzJPsoriasis and systemic inflammatory diseases: potential mechanistic links between skin disease and co-morbid conditionsJ Invest Dermatol20101307 1785 179620445552
- GottliebABDannFComorbidities in patients with psoriasisAm J Med200912212 1150.e1 e9
- GisondiPFerrazziAGirolomoniGMetabolic comorbidities and psoriasisActa Dermatovenerol Croat2010184 297 30421251450
- EspositoMSaracenoRGiuntaAMaccaroneMChimentiSAn Italian study on psoriasis and depressionDermatology20062122 123 12716484818
- EspositoMFaleriSBabinoGFrom patients’ needs to treatment outcomes in psoriasis: results from the pSORRIDI experienceJ Int Med Res2016441 Suppl 95 9927683149
- JacobsARosumeckSNastASystematic review on the maintenance of response during systemic antipsoriatic therapyBr J Dermatol20151734 910 92126280365
- ParkHLiZYangXOA distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17Nat Immunol2005611 1133 114116200068
- CaiYFlemingCYanJDermal γδ T cells–a new player in the pathogenesis of psoriasisInt Immunopharmacol2013163 388 39123499509
- YaoZPainterSLFanslowWCHuman IL-17: a novel cytokine derived from T cellsJ Immunol199515512 5483 54867499828
- GaffenSLJainRGargAVCuaDJThe IL-23-IL-17 immune axis: from mechanisms to therapeutic testingNat Rev Immunol2014149 585 60025145755
- GaffenSLThe role of interleukin-17 in the pathogenesis of rheumatoid arthritisCurr Rheumatol Rep2009115 365 37019772832
- KirkhamBWLassereMNEdmondsJPSynovial membrane cytokine expression is predictive of joint damage progression in rheumatoid arthritis: a two-year prospective study (the DAMAGE study cohort)Arthritis Rheum2006544 1122 113116572447
- KatzYNadivOBeerYInterleukin-17 enhances tumor necrosis factor alpha-induced synthesis of interleukin 1, 6 and 8 in skin and synovial fibroblasts: a possible role as a “fine-tuning cytokine” in inflammation processArthritis Rheum2001449 2176 218411592383
- ChabaudMFossiezFTaupinJLMiossecPEnhancing effect of IL-17 on IL-1-induced IL-6 and leukemia inhibitory factor production by rheumatoid arthritis synoviocytes and its regulation by Th2 cytokinesJ Immunol19981611 409 4149647250
- JovanovicDVDi BattistaJAMartel-PelletierJIL-17 stimulates the production and expression of proinflammatory cytokines, IL-1beta and TNF alpha, by human macrophagesJ Immunol19981607 3513 35219531313
- ChabaudMMiossecPThe combination of tumor necrosis factor alpha blockade with interleukin-1 and interleukin-17 blockade is more effective for controlling synovial inflammation and bone resorption in an ex vivo modelArthritis Rheum2001446 1293 130311407688
- RuddyMJWongGCLiuXKFunctional cooperation between interleukin-17 and tumor necrosis factor-α is mediated by CCAAT/enhancer binding protein family membersJ Biol Chem20042794 2559 256714600152
- LubbertsEIL-17/Th17 targeting: on the road to prevent chronic destructive arthritis?Cytokine2008412 84 9118039580
- BenderdourMTardifGPelletierJPInterleukin 17 (IL-17) induces collagenase-3 production in human osteoclastic chondrocytes via AP-1 dependent activation: differential activation of AP-1 members by IL-17 and IL-1betaJ Rheum20022921 1262 127212064845
- KoshyPJHendersonNLoganCLifePFCawstonTERowanADInterleukin 17 induces cartilage collagen breakdown: novel synergistic effects in combination with proinflammatory cytokinesAnn Rheum Dis2002618 704 71312117676
- ChiricozziAPathogenic role of IL-17 in psoriasis and psoriatic arthritisActas Dermosifiliogr2014105Suppl 1 9 2025398488
- LowesMARussellCBMartinDATowneJEKruegerJGThe IL-23/T17 pathogenic axis in psoriasis is amplified by keratinocyte responsesTrends Immunol2013344 174 18123291100
- KruegerJGFretzinSSuárez-FariñasMIL-17A is essential for cell activation and inflammatory gene circuits in subjects with psoriasisJ Allergy Clin Immunol20121301 145.e9 154.e922677045
- JohansenCUsherPAKjellerupRBLundsgaardDIversenLKragballeKCharacterization of the interleukin-17 isoforms and receptors in lesional psoriatic skinBr J Dermatol20091602 319 32419016708
- LowesMAKikuchiTFuentes-DuculanJPsoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cellsJ Invest Dermatol20081285 1207 121118200064
- LiJChenXLiuZYueQLiuHExpression of Th17 cytokines in skin lesions of patients with psoriasisJ Huazhong Univ Sci Technolog Med Sci2007273 330 33217641855
- Guttman-YasskyELowesMAFuentes-DuculanJLow expression of the IL-23/Th17 pathway in atopic dermatitis compared to psoriasisJ Immunol200818110 7420 742718981165
- KagamiSRizzoHLLeeJJKoguchiYBlauveltACirculating Th17, Th22, and Th1 cells are increased in psoriasisJ Invest Dermatol20101305 1373 138320032993
- CaproniMAntigaEMelaniLVolpiWDel BiancoEFabbriPSerum levels of IL-17 and IL-22 are reduced by etanercept, but not by acitretin, in patients with psoriasis: a randomized-controlled trialJ Clin Immunol2009292 210 21418763027
- LønnbergASZachariaeCSkovLTargeting of interleukin-17 in the treatment of psoriasisClin Cosmet Investig Dermatol20147 251 259
- RichPSigurgeirssonBThaciDSecukinumab induction and maintenance therapy in moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled, phase II regimen-finding studyBr J Dermatol20131682 402 41123362969
- RussellCBRandHBiglerJGene expression profiles normalized in psoriatic skin by treatment with brodalumab, a human anti-IL-17 receptor monoclonal antibodyJ Immunol20141928 3828 383624646743
- GenoveseMCVan den BoschFRobersonSALY2439821, a humanized anti-interleukin-17 monoclonal antibody, in the treatment of patients with rheumatoid arthritis: a phase I randomized, double-blind, placebo-controlled, proof-of-concept studyArthritis Rheum2010624 929 93920131262
- ChanACCarterPJTherapeutic antibodies for autoimmunity and inflammationNat Rev Immunol2010105 301 31620414204
- LiuLLuJAllanBWGeneration and characterization of ixekizumab, a humanized monoclonal antibody that neutralizes interleukin 17AJ Inflamm Res20169 39 5027143947
- LeonardiCMathesonRZachariaeCAnti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasisN Engl J Med201236613 1190 119922455413
- GordonKBLeonardiCLLebwohlMA 52-week, open-label study of the efficacy and safety of ixekizumab, an anti-interleukin-17A monoclonal antibody, in patients with chronic plaque psoriasisJ Am Acad Dermatol2014716 1176 118225242558
- GordonKBBlauveltAPappKAUNCOVER-1 Study Group; UNCOVER-2 Study Group; UNCOVER-3 Study GroupPhase 3 trials of Ixekizumab in moderate-to-severe plaque psoriasisN Engl J Med20163754 345 35627299809
- ReichKLeonardiCLebwohlMSustained response with ixekizumab treatment of moderate-to-severe psoriasis with scalp involvement: results from three phase 3 trials (UNCOVER-1, UNCOVER-2, UNCOVER-3)J Dermatolog Treat2016 1 6
- DennehyEBZhangLAmatoDGoldblumORichPIxekizumab is effective in subjects with moderate to severe plaque psoriasis with significant nail involvement: results from UNCOVER 3J Drugs Dermatol2016158 958 96127537996
- van de KerkhofPGuentherLGottliebABIxekizumab treatment improves fingernail psoriasis in patients with moderate-to-severe psoriasis: results from the randomized, controlled and open-label phases of UNCOVER-3J Eur Acad Dermatol Venereol2017313 477 48227910156
- ArmstrongAWLyndeCWMcBrideSREffect of Ixekizumab treatment on work productivity for patients with moderate-to-severe plaque psoriasis: analysis of results from 3 randomized phase 3 clinical trialsJAMA Dermatol20161526 661 66926953848
- SaekiHNakagawaHNakajoKJapanese Ixekizumab Study GroupEfficacy and safety of ixekizumab treatment for Japanese patients with moderate to severe plaque psoriasis, erythrodermic psoriasis and generalized pustular psoriasis: results from a 52-week, open-label, phase 3 study (UNCOVER-J)J Dermatol2017444 355 36227726163
- MeasePJvan der HeijdeDRitchlinCTSPIRIT-P1 Study GroupIxekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naive patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo-controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1Ann Rheum Dis2017761 79 8727553214
- GriffithsCEReichKLebwohlMUNCOVER-2 and UNCOVER-3 investigatorsComparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trialsLancet20153869993 541 55126072109
- BlauveltAPappKAGriffithsCEEfficacy and safety of switching to Ixekizumab in Etanercept non-responders: a subanalysis from two phase III randomized clinical trials in moderate-to-severe plaque psoriasis (UNCOVER-2 and -3)Am J Clin Dermatol2017182 273 28028074446
- FarahnikBBeroukhimKZhuTHIxekizumab for the treatment of psoriasis: a review of phase III trialsDermatol Ther (Heidelb)201661 25 3726910853
- GottliebABLacourJPKormanNTreatment outcomes with ixekizumab in patients with moderate-to-severe psoriasis who have or have not received prior biological therapies: an integrated analysis of two Phase III randomized studiesJ Eur Acad Dermatol Venereol Epub2016101
- EspositoMGisondiPCassanoNSurvival rate of antitumor necrosis factor-a treatments for psoriasis in routine dermatological practice: a multicenter observational studyBr J Dermatol20131693 666 67223647206
- Dyring-AndersenBSkovLZachariaeCIxekizumab for treatment of psoriasisExpert Rev Clin Immunol2015114 435 44225748485
- ElyoussfiSThomasBJCiurtinCTailored treatment options for patients with psoriatic arthritis and psoriasis: review of established and new biologic and small molecule therapiesRheumatol Int2016365 603 61226892034
