Abstract
Background
Heterotopic ossification on the enthesis, which develops after subsequent inflammation, is one of the most distinctive features in ankylosing spondylitis (AS). Prostaglandin E2 (PGE-2) serves as a key mediator of inflammation and bone remodeling in AS. Celastrol, a well-known Chinese medicinal herb isolated from Tripterygium wilfordii, is widely used in treating inflammatory diseases, including AS. It has been proven that it can inhibit lipopolysac-charide-induced expression of various inflammation mediators, such as PGE-2. However, the mechanism by which celastrol inhibits inflammation-induced bone forming in AS is unclear.
Objective
To investigate whether celastrol could inhibit isolated AS fibroblast osteogenesis induced by PGE-2.
Methods
Hip synovial tissues were obtained from six AS patients undergoing total hip replacement in our hospital. Fibroblasts were isolated, primarily cultured, and then treated with PGE-2 for osteogenic induction. Different doses of celastrol and indometacin were added to observe their effects on osteogenic differentiation. Cell proliferation, osteogenic markers, alizarin red staining as well as the activity of alkaline phosphatase were examined in our study.
Results
Celastrol significantly inhibits cell proliferation of isolated AS fibroblasts and in vitro osteogenic differentiation compared with control groups in a time- and dose-dependent manner.
Conclusion
Our results demonstrated that celastrol could inhibit isolated AS fibroblast proliferation and in vitro osteogenic differentiation. The interaction of PI3K/AKT signaling and Wnt protein may be involved in the process. Further studies should be performed in vivo and animal models to identify the potential effect of celastrol on the bone metabolism of AS patients.
Introduction
Ankylosing spondylitis (AS), an inflammatory and immune disease that mainly affects axial joints,Citation1 is characterized by a strong correlation between chronic inflammation and abnormal new bone formation.Citation2 However, it is not entirely understood.
As an important mediator of inflammation, prostaglandin E2 (PGE-2) modulates the anabolic/catabolic process, which occurs in the bone forming and absorption,Citation3 and is the most abundant among prostaglandins in osteoblasts.Citation4 PGE-2 promotes bone remodeling through inducing osteoblast cell differentiationCitation5,Citation6 and is widely involved in the heterotopic ossification.Citation7,Citation8 Moreover, PGE-2 plays a more essential role in the development of heterotopic ossification than other prostaglandins in the rabbit model.Citation9 PGE-2 could exert antiapoptotic effects on bone marrow stem cells, leading to an increase in the number of cells and subsequent osteoblastic cell differentiation.Citation10 Beside this, PGE-2 is commonly used for osteogenic induction via upregulation of bone morphogenetic protein 2 (BMP-2),Citation11 which has the ability to induce osteoblastic precursor cell differentiation and in vitro osteogenesis.Citation12,Citation13
To date, the possibility of PGE-2 involvement in the pathophysiogenesis and AS progression has been investigated.Citation14 Genome-wide association studies on AS recently reported that gene prostaglandin E receptor 4, one of the four genes that encode the PGE-2 receptors (EP1–EP4),Citation15 was associated with AS.Citation16 Indeed, EP4-knockout mice exhibited a marked reduction in bone resorption, causing impaired formation of osteoclasts, matrix metalloproteinase MMP-2 and MMP-13.Citation17,Citation18 Furthermore, PGE-2 downregulated Wnt/β-catenin inhibitors, including dickkopf-1 and sclerostin, which have been proven to be two crucial negative regulated factors in AS bone forming,Citation19,Citation20 through AKT/PI3K and Wnt signaling cross-interactions.Citation21 Nonsteroidal anti-inflammatory drugs (NSAIDs) were frequently used for patients with AS to inhibit heterotopic ossification over the years, which supports the possibility that prostaglandins were local mediators of inflammation and bone remodeling involved in this process.Citation22–Citation24
Although NSAIDs are generally used for AS patients, common side effects associated with the long-term use of NSAIDs include gastrointestinal and cardiovascular toxicities.Citation25,Citation26 Searching for new drugs with low side effects to target AS inflammation and new bone formation are thus urgent tasks.
As complementary and alternative medications, traditional Chinese medicine not only has a long history of therapeutic use but also is acceptable and tolerated by patients.Citation27 In People’s Republic of China, Tripterygium wilfordii, which is a medicinal herb, has been used in the treatment of inflammatory and rheumatic diseases for thousands of years. T. wilfordii is reported to improve physical activity and relieve symptoms in patients with rheumatoid arthritis (RA)Citation28 and AS.Citation29 Celastrol, one of the active compounds present in T. wilfordii, has been identified to have strong anti-inflammatory activityCitation30,Citation31 and reduce the severity of clinical arthritis.Citation32,Citation33 Previous reports demonstrated that celastrol strongly suppressed lipopolysaccharide-induced expression of PGE-2 at low concentrations,Citation34 via the downregulation of COX-1 and -2 activation.Citation35 This provided a theoretical basis for understanding the inhibitory effects of celastrol against PGE-2-induced osteogenesis.
So far, most studies related to celastrol in inflammatory disease were mainly focused on RA.Citation36 However, the effects of celastrol on AS bone forming have not been documented before. Therefore, our study was carried out to investigate the effect of celastrol on the proliferation and osteogenesis of isolated AS fibroblasts induced by PGE-2 for the first time. To elucidate the mechanisms, we examined the inhibitory role of celastrol on isolated AS fibroblast proliferation and in vitro osteogenic differentiation by using different modern techniques.
Materials and methods
Isolation and culture of hip synovial fibroblasts
Six AS patients with hip joint involved received total hip replacement in our hospital. In this study, patients were referred to a rheumatologist if they were: 1) age ≤45 years, 2) symptoms duration ≥3 months, and 3) asymmetrical arthritis pain plus more than one spondyloarthritis (SpA) feature (). All the surgical procedures and experiments were approved by the Ethics Committee, Southern Medical University, People’s Republic of China. All patients signed the informed consent. Briefly, the hip capsule synovium tissues were excised from the hip synovial tissue. Synovium was minced and digested with 3 mg/mL collagenase (type I; Sigma-aldrich, Shanghai, China) in sterile phosphate-buffered saline (PBS) for 2.5 hours at 37°C. The isolated tissues were passed through a 70 mm cell strainer (Becton Dickinson, Franklin Lakes, NJ, USA) to form a single-cell suspension. The released cells were washed with PBS, centrifuged at 300× g for 5 minutes, and subsequently resuspended in Dulbecco’s Modified Eagle’s Medium (Thermo Fisher Scientific, Waltham, MA, USA), a medium containing 10% fetal bovine serum, and supplemented with 100 U/mL penicillin, 100 mg/mL streptomycin, and 2 mM l-glutamine (all of them from Thermo Fisher Scientific). The isolated cells were incubated at 37°C under 5% CO2 to form colonies. The old culture medium was removed and PBS was used to wash the cells one to two times. Then trypsin–EDTA (1 mL/25 cm2) was added to wash the bottom of the culture dish. Then trypsin–EDTA was removed and the culture dish was put into the 37°C cell incubator for 2–3 minutes. Trypsin was inhibited by adding a medium containing 10% FBS. Fresh medium was added and cells were transferred into a new culture dish with normal conditions. The cultured medium with PGE-2 was changed every 2 days throughout the experiments. Flow cytometry was used for fibroblast sorting and identification marked by CD90 and CD106 as previously described.Citation37,Citation38
Table 1 Basic clinical data for AS patients
Cultured fibroblasts were stimulated with PGE-2 (Sigma) at concentrations of 10−7 M as previously describedCitation39 and then incubated in 3 mL of Dulbecco’s Modified Eagle’s Medium supplemented with antibiotics and fungizone. PGE-2 was added for proliferation and osteogenesis in the whole cell culture process. The medium was changed every 2 days throughout the experiments.
Preparation of celastrol and indometacin
A stock solution of celastrol (20 mg in 0.6 mL of dimethyl sulfoxide [DMSO]) was prepared and stored as small aliquots at −20°C until used (Sigma-Aldrich Co., St Louis, MO, USA). Different doses of celastrol (0.5, 1.0, and 2.0 μM) used in vitro in this study were based on that used in a previous study.Citation34 Celastrol stock was diluted in PBS, and PBS–DMSO (1.2%) served as its negative control. Indometacin (1.0 μM) was selected as a positive control. DMSO, 1.0 μM of nonselective NSAIDs–indometacin, and the indicated concentrations of celastrol (0.5, 1.0, and 2.0 μM) were added on day 12.
Proliferation assay
Cells were seeded in 24-well plates at a density of 1×105 cells/well. Cell proliferation was investigated using an MTS assay on days 12, 14, 17, and 20, respectively. In brief, cells were added to 500 μL of MTS solution and incubated for 4 hours. After that, cells were washed with PBS and added to 500 μL of DMSO to remove the MTS solution. The optical density was measured at 570 nm using a Sunrise absorbance reader (Tecan Group Ltd., Shanghai, People’s Republic of China).
Alkaline phosphatase activity
Alkaline phosphatase (ALP) activity was examined according to a published protocol.Citation13 Culture medium was aspirated from AS fibroblasts that were incubated in plates. The plates were rinsed with 150 mM NaCl and 1 mL of reaction buffer containing 0.25 M 2-methyl-2-amino propanol and 1 mM magnesium chloride. An amount of 2.5 mg/mL of p-nitrophenyl phosphate (Sigma) at pH 10.3 was added to each well at 37°C, respectively. The reaction was stopped after 30 minutes by adding 0.5 mL of 0.3 M Na3PO4 at pH 12.3. ALP activity was assessed by measuring the absorbance of light at 410 nm and comparing the experimental samples with standard solutions of p-nitrophenol and a blank group. ALP was normalized for protein concentration using BCA Protein Assay Reagent (Pierce, Rockford, IL, USA), compared with the standard protein, and measured by spectrophotometry at 562 nm.
RNA isolation and quantitative real-time PCR
Total RNA was isolated from the cells by using Trizol (Invitrogen, Carlsbad, CA, USA). cDNA was synthesized from 4 μg of total RNA using 200 U of reverse transcriptase (Invitrogen) according to the manufacturer’s instructions. The gene expression was normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as a housekeeping gene. The sequences of forward and reverse primers used were as follows: BMP-2, 5′-CAGCTTCCACCATGAAGAAT-3′ (F), and 5′-CCAACCTGGTGTCCAAAAGT-3′ (R); runt-related transcription factor 2 (Runx-2), 5′-CTCCCTGAACTCTGCACCAA-3′ (F), and 5′-GTTCTGAAGCACCTGAAATGCG-3′ (R); collagen type I alpha 1, 5′-CCTGGATGCCATCAAAGTCT-3′ (F), and 5′-ACTGCAACTGGAATCCATCG-3′ (R); osteocalcin, 5′-ATGAGAGCCCTCACACTCCT-3′ (F), and 5′-CTTGGACACAAAGGCTGCAC-3′ (R); and GAPDH, 5′-CCATGGAGAAGGCTGGGG-3′ (F), and 5′-CAAAGTTGTCATGGATGACC-3′ (R).
Alizarin red staining
For Alizarin red staining, the cells were fixed for 1 hour using 70% ethanol at 4°C. After washing with distilled water for three times, Alizarin red solution (40 mM) was added for 10 minutes. Cells were rinsed with distilled water and subsequently washed with PBS. The stained cells were observed under an inverted microscope. Photomicrographs were obtained by using a charge-coupled device camera. Thereafter, Alizarin red was eluted with 10% cetylpyridinium chloride, and the optical density value was read at 510 nm for quantified analysis of ossification activity.
Western blot analysis
Whole cells were lysed using RIPA buffer (10 mM Tris-HCl, pH 7.4, 0.15 M NaCl, 0.5% sodium dodecyl sulfate, 1% NP-40, 1% Na-deoxycholate, 1 mM EDTA, 1 mM phenylmethanesulfonyl fluoride, 1 μg/mL of pepstatin, and 1 μg/mL of leupeptin). Secretory protein was extracted by precipitation with trichloroacetic acid. Western blot analysis was performed with anti-PGE-2, anti-AKT, anti-PI3K, anti-GSK-3β, anti-β-catenin, anti-DKK-1, anti-SOST, or anti-β-actin antibodies (all from Abcam, Cambridge, UK).
Statistical analysis
Data in each group were shown as the mean ± standard deviation calculated from the results of the six samples. Statistical significance was assessed by one-way analysis of variance, and multiple comparison tests were employed by Scheffe’s method. A P-value of <0.05 was considered significant.
Results
Effect of celastrol on proliferation of isolated AS fibroblasts
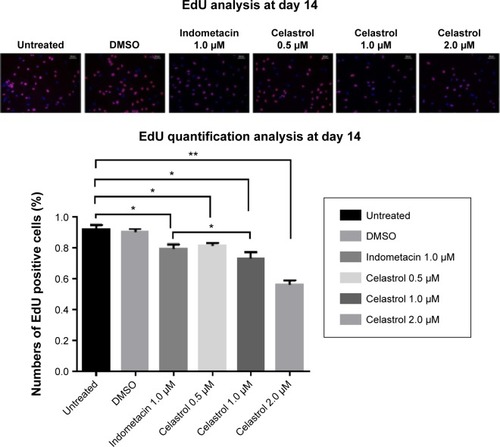
Hip synovial fibroblasts were successfully primary cultured (). In order to investigate the potential effect of celastrol on proliferation of isolated AS fibroblasts, we conducted various concentrations of celastrol, indometacin 1.0 μM, normal and DMSO control, and cell viability was determined using MTS assay. Treatment with 2.0 μM celastrol most greatly decreased cell viability, in comparison with other controls ( and ). To further explore the effect of celastrol on cells, we monitored cell proliferation on day 14 using EdU incorporation assay (). It was also shown that treatment with 2.0 μM celastrol greatly decreased cell viability, and cells treated with 2.0 μM celastrol led to a significant percentage reduction of EdU-positive AS fibroblasts. An amount of 1.0 μM celastrol exhibited stronger ability to suppress AS fibroblast proliferation compared with 1.0 μM indometacin determined by MTS and EdU analysis ( –). The treatment with 1.0 μM indometacin showed slightly more decreased cell viability as well as percentage reduction of EdU-positive AS fibroblasts and was not statistically significant as compared with that in 0.5 μM celastrol ( –).
Figure 1 Fibroblasts were successfully cultured and subcultured regularly by changing the culture medium.
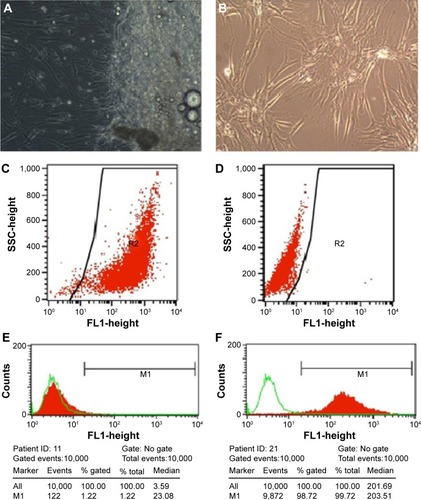
Figure 2 Cell proliferation growth curve treated by various doses of Celastrol, 1.0 μM Indometacin as well as negative controls.
Abbreviation: DMSO, dimethyl sulfoxide.
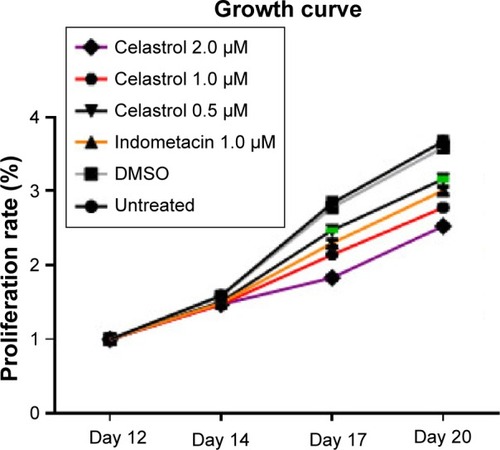
Figure 3 Celastrol inhibits cell proliferation by an MTS assay.
Abbreviations: DMSO, dimethyl sulfoxide; OD, optical density.
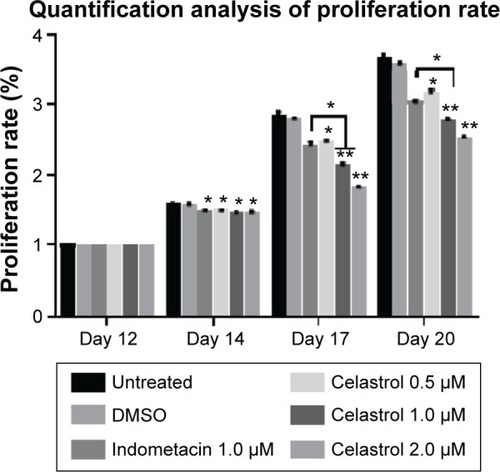
Figure 4 Cell proliferation is measured by performing an EdU incorporation assay on day 14.
Abbreviation: DMSO, dimethyl sulfoxide.
Effect of celastrol on PGE-2-induced osteogenesis in isolated AS fibroblasts
We performed several assays to assess the effect of celastrol on the osteogenesis of AS fibroblasts.
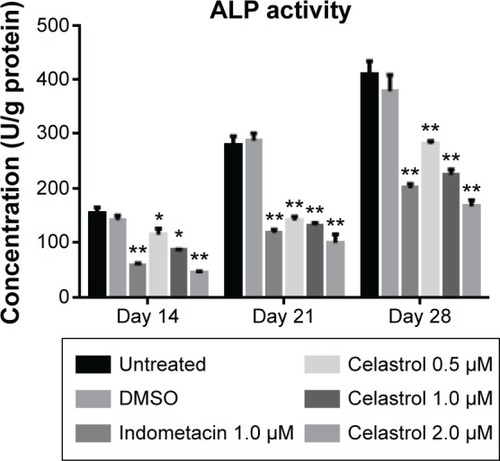
ALP activity
The results demonstrated that large, medium, and small doses of celastrol as well as indometacin had significant inhibitory effects on the ALP activity of PGE-2-induced AS fibroblasts at 2, 3, and 4 weeks (). The ALP activity was inhibited by celastrol in a dose-dependent manner. As shown in , its activity decreased gradually when stimulated with increasing doses of celastrol. Similarly, data obtained from the medium dose of celastrol and indometacin had a similar effect on the ALP activity.
Figure 5 Effect of different doses of celastrol on ALP activity in isolated ankylosing spondylitis fibroblasts compared with indometacin and negative control.
Abbreviations: DMSO, dimethyl sulfoxide; ALP, alkaline phosphatase.
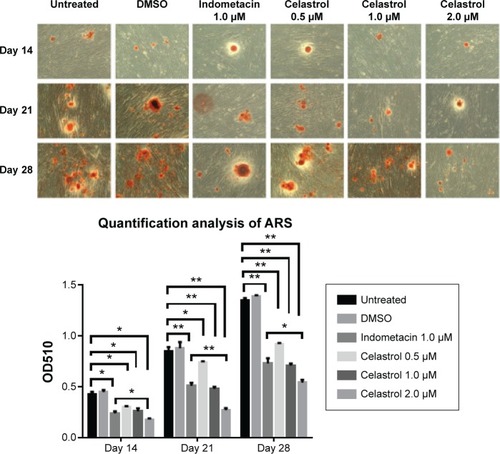
Alizarin red staining
The results demonstrated that large, medium, and small doses of celastrol as well as indometacin had a significant inhibitory effect on the alizarin red staining activity of PGE-2-induced AS fibroblasts on days 14, 21, and 28. Mineralization had the largest decline in 2.0 μM celastrol. The medium dose of celastrol and indometacin had a similar effect on the ARS activity. Celastrol 2.0 μM exhibited stronger inhibition effects of mineralization than indometacin 1.0 μM ().
Figure 6 Effect of different doses of celastrol on Alizarin red staining in isolated ankylosing spondylitis fibroblasts compared with indometacin and negative control.
Abbreviation: OD, optical density.
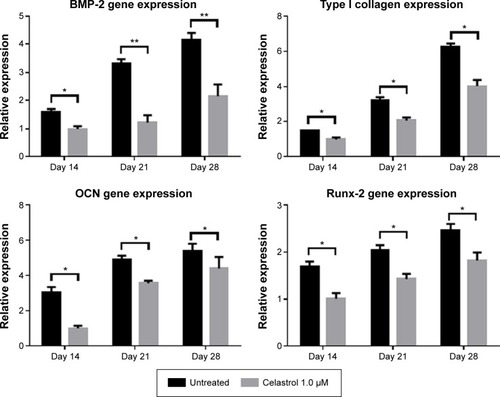
Real-time PCR
The mRNA expressions of BMP-2, type I collagen, Runx-2, and osteocalcin were involved in PGE-2-induced AS fibroblasts. Therefore, to investigate whether celastrol could inhibit PGE-2-induced AS fibroblasts, mRNA levels of BMP-2, type I collagen, Runx-2, and osteocalcin were assessed by real-time PCR on days 14, 21, and 28. Treatment with 1.0 μM celastrol suppressed mRNA and protein expression in a time-dependent manner (). The results indicated that the group with 1.0 μM celastrol had a significantly higher mRNA expression of BMP-2, type I collagen, Runx-2, and osteocalcin than the normal group. Especially, celastrol treatment significantly reduced the expression of BMP-2 on days 21 and 28 (**P<0.01). These findings indicated that the medium dose of celastrol had a significant inhibitory effect on mRNA expressions of BMP-2, type I collagen, Runx-2, and osteocalcin in PGE-2-induced AS fibroblasts compared with the normal group (*P<0.05).
Figure 7 An amount of 1.0 μM celastrol inhibits mRNA expressions of osteogenic genes in prostaglandin E2-induced ankylosing spondylitis fibroblasts compared with untreated control.
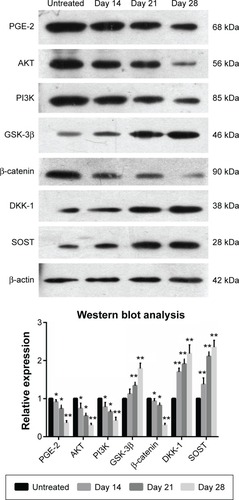
Effect of celastrol on PGE-2, Wnt, and AKT/PI3K signaling cross-interactions by Western blot analysis
In order to explore the potential mechanism of celastrol on osteogenesis in isolated AS fibroblasts, we performed Western blot analysis to examine the expression of related proteins pretreated with a medium dose of celastrol. The untreated bands were used as controls. The intensity of the bands was quantified by densitometric analysis and normalized against the appropriate controls. The average results from six independent experiments are shown in and . Accordingly, we found the expression of PGE-2, AKT, and PI3K reduced substantially. The expression of GSK-3β increased significantly, whereas the level of β-catenin decreased with time. On the other hand, the expression of DKK-1 and sclerostin, Wnt signaling inhibitors, elevated gradually.
Figure 8 Celastrol (1.0 μM) impacts the expression of related proteins in isolated fibroblasts.
Abbreviation: PGE-2, prostaglandin E2.
Discussion
In terms of AS, inflammation is frequently on the sacroiliac joints,Citation40 anterior and posterior vertebral corners of the spine,Citation41 and hip jointsCitation42 where syndesmophytes develop. Previous studies have proposed a positive association between vertebral corner inflammation of baseline magnetic resonance imaging and subsequent development of new syndesmophytes,Citation43–Citation45 which supports a hypothesis that inflammation is implicated in new bone formation of patients with AS. In recent years, the inflammation biomarkers related to AS bone turnover have been mostly focused on tumor necrosis factor-α. Nevertheless, interventions targeting tumor necrosis factor-α were not expected to obtain favorable prognosis on AS radiographic progression.Citation46,Citation47 To date, NSAIDs acted as the most effective drugs to prevent structural damage in AS patientsCitation22–Citation24 by inhibiting COX-1 and -2 to reduce the production of PGE-2. This fact indicated that PGE-2 may play a crucial role in the interplay between inflammation and new bone formation in AS.
This study was aimed to investigate the underlying mechanism by which celastrol exerts its activity on AS fibroblast proliferation and osteogenesis, thus finding new potential ways for the treatment of AS.
Celastrol is one of the remedial ingredients isolated from the root of the Thunder God Vine, also named “Lei Gong Teng” in Chinese. The Thunder God Vine is a perennial vine of Celastraceae family (bittersweet), which has been widely used in People’s Republic of China for the treatment of autoimmune and inflammatory diseases for centuries.Citation48 The plant is poisonous, but its root pulp contains several therapeutically active compounds. Moreover, celastrol is the most widely studied and promising compound isolated from the Thunder God Vine.Citation28 Celastrol contains electrophilic sites within the rings of quinone methide structure and it can react with the nucleophilic thiol groups of cysteine residues and form covalent Michael adducts.Citation49 Its inhibitory effects against COX-1, COX-2, and PGE-2 have been identified,Citation33,Citation34 which are similar with NSAIDs. The difference is that celastrol is also endowed with cytotoxic-like function and could exhibit anticancer effects.Citation49–Citation51
In the present study, results showed that celastrol effectively inhibited proliferation and bone formation of PGE-2-induced AS fibroblasts. Notably, to elucidate the potential mechanism of antibone forming action of celastrol, we found that cross-interactions of Wnt, BMP-2, and AKT/PI3K signaling pathways were involved in this process.
We selected AS fibroblasts as target cells. In addition to mesenchymal stem cells, fibroblast are another category with osteogenic potentials, especially in pathological conditions.Citation52 Fibroblasts are the most common cells in connective tissues around joints. Fibroblasts and osteoblasts all originate from mesenchymal stem cells with overlapping phenotypes and similar differentiation pathways, which enables possible mutual biological transformation.Citation53 Fibroblasts could also provide surroundings for calcium deposition and bone formation by producing extracellular matrix vesicles and type I collagen, which plays a crucial role in trauma repair and ectopic ossification in certain pathophysiologic processes.Citation54,Citation55 In addition, fibroblasts also express osteogenic markers Runx-2 and osteocalcin (OCN). It has been reported that NIH3T3 cells (a fibroblast cell line derived from mouse) could express osteogenic markers and develop mineralization deposits in vitro induced by dexamethasone and 1,25(OH)2D3.Citation56 Human derived ligament fibroblasts could also develop osteogenic differentiation in conditioned medium.Citation57 Previous studies also identified that activities of fibroblast proliferation and collagen synthesis could be enhanced by inflammatory mediators in vitro, which develop bone formation, proliferation of the connective tissues, or fibrosis.Citation58,Citation59 An early immunohistochemistry analysis by Ono et alCitation60 found four cell types are present in the ossified ligament tissues: chondrocytes, chondrocyte-like cells, fibroblast-like cells, and fibroblasts. According to the distribution of cells, the authors believed that chondrocytes are derived from fibroblasts. In addition, chondrocyte-like cells and fibroblast-like cells are the same cell types, both originating from fibroblasts.Citation56 Other experimental and animal studies have also proved that fibroblasts have osteogenic potential in certain conditions.Citation61,Citation62 All these findings suggest fibroblasts in AS may convert to osteoblast-like type cells and express osteogenic makers under certain conditions.
Fibroblasts isolated from AS patients were significantly affected by PGE-2-induced expression of osteogenic phenotype. The results of our study highlighted a marked reduction in cell proliferation and distinctive attenuation of osteogenic activity of celastrol-treated AS fibroblasts compared to negative controls in a time- and dose-dependent manner. In addition, a medium dose of celastrol exhibited similar effects in both ARS staining and ALP activity, as indometacin. As mentioned above, we hypothesized that this protection against abnormal new bone formation may be mediated via the cross-interactions of PGE-2 and different signaling pathways, such as Wnt, BMP-2, and AKT/PI3K. The Wnt pathway and PGE-2 have mutual cross-interactions. Especially, canonical Wnt proteins promoted PI3K/Akt activity, resulting in GSK-3β phosphorylation and the growth of free β-catenin levels.Citation63 On the other hand, PGE-2 activated the trimetric G-protein by binding to its EP2 receptor. The Gβγ subunits activated PI3-kinase which in turn activated Akt. After that, Akt phosphorylated GSK-3β leading to inhibiting its phosphorylation of β-catenin.Citation64 All in all, the PI3K-Akt signaling pathway is involved in PGE-2-induced osteogenic differentiation. Besides, PGE-2 exerted its anabolic effects to induce BMP-2 and COX-2 via activating osteoblastic EP2 and EP4 receptors.Citation65 BMP-2 in turn induced COX-2 expression, resulting in accelerating the production of PGE-2.Citation66
Previous studies widely reported the effect of celastrol on osteoclasts in RA models. Nanjundaiah et alCitation67 found celastrol could inhibit inflammation-induced osteoclasto-genesis in arthritic rats via stimulating RANKL production and increasing RANKL/OPG ratio. Moreover, Gan et alCitation68 observed that celastrol not only directly suppressed the formation and function of osteoclasts, but also reduced the RANKL-induced expression of osteoclastic genes and transcriptional factors. In our study, celastrol inhibited fibroblast proliferation and osteogenesis, which implicated that celastrol performed “complete inhibition” of osteoblasts, fibroblasts, and osteoclasts. This was why celastrol impaired their further activities and functions.
AS damages bone in the same way as RA in the initial stage of the disease. Nevertheless, some cases are followed by abnormal bone formation, which is probably linked with the subtle modulation via inflammation and bone metabolism on the different stages of disease. Although the underlying mechanism has not been clearly delineated, we hypothesize that it is associated with the attenuation of PGE-2. Our results supported this proposition. A low dose of exogenous PGE-2 (<0.5 mg) stimulated bone apposition. Instead, high doses caused bone resorption, which is expected to be identified in a further study.
In our study, several limitations should be taken into account. First, we only took in vitro AS fibroblasts as study samples. Therefore, animal models or other in vivo models should be performed to substantiate these results. Second, we only demonstrated the role of celastrol on PGE-2 and downstream proteins of PGE-2. Despite all this, other inflammation markers related to bone metabolism are worthy of further in-depth study. Last, we only obtained tissues from AS patients due to ethical reasons. Additional tissue samples from healthy controls, RA, OA patients, and so on would be helpful to identify whether the findings are specific to AS.
In conclusion, our study provided a novel insight regarding the inhibitory effect of celastrol on the proliferation of AS fibroblasts and PEG-2-induced osteogenesis. We demonstrated for the first time that celastrol inhibited PGE-2-induced osteogenic differentiation in AS fibroblasts. Meanwhile, celastrol could also reduce the number of fibroblasts in a time- and dose-dependent manner. These results revealed that celastrol inhibits further differentiation of fibroblasts into osteogenic phenotype. In future studies, application of celastrol might be a promising approach in the treatment of new bone formation in AS by performing pharmacokinetic and toxicological analyses in animals and humans as well as randomized control studies.
Supplementary material
Table S1 Raw Data Of Western Blot Analysis Results with 1.0 μM celastrol compared with untreated group
Disclosure
The authors report no conflicts of interest in this work.
References
- BraunJSieperJAnkylosing spondylitisLancet20073691379139017448825
- SieperJAppelHBraunJRudwaleitMCritical appraisal of assessment of structural damage in ankylosing spondylitis: implications for treatment outcomesArthritis Rheum20085864965618311819
- KawaguchiHPilbeamCCHarrisonJRRaiszLGThe role of prostaglandins in the regulation of bone metabolismClin Orthop Rel Res19953133646
- YokotaKKusakaMOshimaTStimulation of prostaglandin E2 synthesis in cloned osteoblastic cells of mouse (MC3T3-E1) by epidermal growth factorJ Biol Chem198626115410154153096986
- Ramirez-YanezGOSeymourGJWalshLJForwoodMRSymonsALProstaglandin E2 enhances alveolar bone formation in the rat mandibleBone2004351361136815589217
- FlanaganAMChambersTJStimulation of bone nodule formation in vitro by prostaglandins E1 and E2Endocrinology19921304434481309342
- NorrdinRWJeeWSSHighWBThe role of prostaglandins in bone in vivoProstaglandins Leukot Essent Fatty Acids1990411391492281118
- YangRSLiuTKLin-ShiauSYIncreased bone growth by local prostaglandin E2 in ratsCalcif Tissue Int19935257618453506
- BartlettCSRapuanoBELorichDGEarly changes in prostaglandins precede bone formation in a rabbit model of heterotopic ossificationBone20063832233216226065
- WeinrebMShamirDMachwateMRodanGAHaradaSKeilaSProstaglandin E2 (PGE2) increases the number of rat bone marrow osteogenic stromal cells (BMSC) via binding the EP4 receptor, activating sphingosine kinase and inhibiting caspase activityProstaglandins Leukot Essent Fatty Acids200675819016890416
- ZhangJWangJHBMP-2 mediates PGE2-induced reduction of proliferation and osteogenic differentiation of human tendon stem cellsJ Orthop Res201230475221688312
- HuangWCarlsenBWulurIBMP-2 exerts differential effects on differentiation of rabbit bone marrow stromal cells grown in two-dimensional and three-dimensional systems and is required for in vitro bone formation in a PLGA scaffoldExp Cell Res200429932533415350532
- RyooHMLeeMHKimYJCritical molecular switches involved in BMP-2-induced osteogenic differentiation of mesenchymal cellsGene2006366515716314053
- HaroonNKimTHInmanRDNSAIDs and radiographic progression in ankylosing spondylitis Bagging big game with small arms?Ann Rheum Dis2012711593159522863576
- EvansDMSpencerCCPointonJJAustralo-Anglo-American Spondyloarthritis Consortium (TASC), the Wellcome Trust Case Control Consortium 2 (WTCCC2). Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibilityNat Genet20114376176721743469
- MiyauraCInadaMSuzawaTImpaired bone resorption to prostaglandin E2 in prostaglandin E receptor EP4-knockout miceJ Biol Chem2000275198191982310749873
- SakumaYTanakaKSudaMImpaired bone resorption by lipopolysaccharide in vivo in mice deficient in the prostaglandin E receptor EP4 subtypeInfect Immun2000686819682511083800
- ChiowchanwisawakitPLambertRGConner-SpadyBFocal fat lesions at vertebral corners on magnetic resonance imaging predict the development of new syndesmophytes in ankylosing spondylitisArthritis Rheum2011632215222521484769
- AppelHRuiz-HeilandGListingJAltered skeletal expression of sclerostin and its link to radiographic progression in ankylosing spondylitisArthritis Rheum2009603257326219877044
- HeilandGRAppelHPoddubnyyDHigh level of functional dickkopf-1 predicts protection from syndesmophyte formation in patients with ankylosing spondylitisAnn Rheum Dis20127157257422186710
- BonewaldLFJohnsonMLOsteocytes, mechanosensing and Wnt signalingBone20084260661518280232
- BoersmaJWRetardation of ossification of the lumbar vertebral column in ankylosing spondylitis by means of phenylbutazoneScand J Rheumatol197656064816001
- WandersAHeijdeDvLandeweRNonsteroidal antiinflam-matory drugs reduce radiographic progression in patients with ankylosing spondylitis: a randomized clinical trialArthritis Rheum2005521756176515934081
- KroonFLandewéRDougadosMVan der HeijdeDContinuous NSAID use reverts the effects of inflammation on radiographic progression in patients with ankylosing spondylitisAnn Rheum Dis2012711623162922532639
- RollasonVSamerCFDaaliYDesmeulesJAPrediction by pharmacogenetics of safety and efficacy of non-steroidal anti-inflammatory drugs: a reviewCurr Drug Metab20141532634324524667
- FineMQuantifying the impact of NSAID-associated adverse eventsAm J Manag Care20131914 Suppls267s27224494609
- NormileDAsian medicine. The new face of traditional Chinese medicineScience200329918819012522228
- BaoJDaiSMA Chinese herb Tripterygium wilfordii Hook F in the treatment of rheumatoid arthritis: mechanism, efficacy, and safetyRheumatol Int2011311123112921365177
- JiWeiLiJuanLinYueReport of 12 cases of ankylosing spondylitis patients treated with Tripterygium wilfordiiClin Rheumatol2010291067107220563618
- JungHWChungYSKimYSParkYKCelastrol inhibits production of nitric oxide and proinflammatory cytokines through MAPK signal transduction and NF-kappaB in LPS-stimulated BV-2 microglial cellsExp Mol Med20073971572118160842
- KannaiyanRShanmugamMKSethiGMolecular targets of celastrol derived from Thunder of God Vine: potential role in the treatment of inflammatory disorders and cancerCancer Lett201130392021168266
- CascaoRVidalBFonsecaJEMoitaLFGambogic acid and celastrol are two powerful anti-inflammatory drugs in arthritisAnn Rheum Dis201170A72
- LiGQLiuDZhangYAnti-invasive effects of celastrol in hypoxia-induced fibroblast-like synoviocyte through suppressing of HIF-1α/CXCR4 signaling pathwayInt Immunopharmacol20131741028103624144813
- KimDHShinEKKimYHSuppression of inflammatory responses by celastrol, a quinone methide triterpenoid isolated from Celastrus regeliiEur J Clin Invest200939981982719549173
- TaoXSchulze-KoopsHMaLCaiJMaoYLipskyPEEffects of Tripterygium wilfordii Hook. f. extracts on induction of cyclooxygenase 2 activity and prostaglandin E2 productionArthritis Rheum1998411301389433878
- YuHVenkateshaSHMoudgilKDMicroarray-based gene expression profiling reveals the mediators and pathways involved in the anti-arthritic activity of Celastrus-derived CelastrolInt Immunopharmacol201213449950622664142
- SorrellJMCaplanAIFibroblasts – a diverse population at the center of it allInt Rev Cell Mol Biol200927616121419584013
- YangZXHanZBJiYRCD106 identifies a subpopulation of mesenchymal stem cells with unique immunomodulatory propertiesPLoS One20138e5935423555021
- WeinrebMShamirDMachwateMRodanGAHaradaSKeilaSProstaglandin E2 (PGE2) increases the number of rat bone marrow osteogenic stromal cells (BMSC) via binding the EP4 receptor, activating sphingosine kinase and inhibiting caspase activityProstaglandins Leukot Essent Fatty Acids200675819016890416
- WendlingDToussirotEStreitGPratiCImaging study scores for ankylosing spondylitisJoint Bone Spine20067365566017064946
- Chary-ValckenaereId’AgostinoMALoeuilleDRole for imaging studies in ankylosing spondylitisJoint Bone Spine20117813814320851029
- Vander CruyssenBVastesaegerNCollantes-EstevezEHip disease in ankylosing spondylitisCurr Opin Rheumatol20132544845423689637
- BaraliakosXListingJRudwaleitMSieperJBraunJThe relationship between inflammation and new bone formation in patients with ankylosing spondylitisArthritis Res Ther200810R10418761747
- MaksymowychWPChiowchanwisawakitPClareTPedersenSJØstergaardMLambertRGInflammatory lesions of the spine on magnetic resonance imaging predict the development of new syndesmophytes in ankylosing spondylitis: evidence of a relationship between inflammation and new bone formationArthritis Rheum2009609310219116919
- van der HeijdeDLandeweRBaraliakosXMRI-inflammation of the vertebral unit (VU) only marginally contributes to new syndesmophytes formation in that unit: A multi-level analysesAnn Rheum Dis200867130
- van der HeijdeDLandewREinsteinSRadiographic progression of ankylosing spondylitis after up to two years of treatment with etanerceptArthritis Rheum2008581324133118438853
- van der HeijdeDLandewéRBaraliakosXRadiographic findings following two years of infliximab therapy in patients with ankylosing spondylitisArthritis Rheum2008583063307018821688
- KannaiyanRShanmugamMKSethiGMolecular targets of celastrol derived from Thunder of God Vine: potential role in the treatment of inflammatory disorders and cancerCancer Lett201130392021168266
- SalminenALehtonenMPaimelaTKaarnirantaKCelastrol: molecular targets of Thunder God VineBiochem Biophys Res Commun201039443944220226165
- CaoLZhangXCaoFInhibiting inducible miR-223 further reduces viable cells in human cancer cell lines MCF-7 and PC3 treated by celastrolBMC Cancer20151587326552919
- ShaMYeJLuanZYGuoTWangBHungJXCelastrol induces cell cycle arrest by MicroRNA-21-mTOR-mediated inhibition p27 protein degradation in gastric cancerCancer Cell Int20151510126500453
- LoriesRJLuytenFPActivated fibrocytes: circulating cells that populate the arthritic synovium?Rheumatology (Oxford)20104961761819965972
- DucyPSchinkeTKarsentyGThe osteoblast: a sophisticated fibroblast under central surveillanceScience20002891501150410968779
- HoshiKAmizukaNSakouTFibroblasts of spinal ligaments pathologically differentiate into chondrocytes induced by recombinant human bone morphogenetic protein-2: morphological examinations for ossification of spinal ligamentsBone1997211551629267691
- LiGPengHCorsiKUsasAOlshanskiAHuardJDifferential effect of BMP4 on NIH/3T3 and C2C12 cells: implications for endochondral bone formationJ Bone Mineral Res20052016111623
- ShuiCScuttAMMouse embryo-derived NIH3T3 fibroblasts adopt an osteoblast-like phenotype when treated with 1alpha, 25-dihydroxyvitamin D(3) and dexamethasone in vitroJ Cell Physiol200219316417212384993
- YuFCuiYZhouXHanJOsteogenic differentiation of human ligament fibroblasts induced by conditioned medium of osteoclast-like cellsBioScience Trends20115465121572246
- EidKLablerLErtelWTrentzOKeelMSystemic effects of severe trauma on the function and apoptosis of human skeletal cellsJ Bone Joint Surg20068813941400
- RutherfordRBMoalliMFranceschiRTWangDGuKKrebsbachPHBone morphogenetic protein-transduced human fibroblasts convert to osteoblasts and form bone in vivoTissue Eng2002844145212167230
- OnoKYonenobuKMiyamotoSOkadaKPathology of ossification of the posterior longitudinal ligament and ligamentum flavumClin Orthop Relat Res1999359182610078125
- HoshiKAmizukaNSakouTKurokawaTOzawaHFibroblasts of spinal ligaments pathologically differentiate into chondrocytes induced by recombinant human bone morphogenetic protein-2: morphological examinations for ossification of spinal ligamentsBone1997211551629267691
- ReddiAHHugginsCBiochemical sequences in the transformation of normal fibroblasts in adolescent ratsProc Natl Acad Sci U S A197269160116054504376
- FukumotoSHsiehCMMaemuraKAkt participation in the Wnt signaling pathway through DishevelledJ Biol Chem2001276174791748311278246
- CastelloneMDTeramotoHWilliamsBODrueyKMGutkindJSProstaglandin E2 promotes colon cancer cell growth through a Gs-axin-β-catenin signaling axisScience20053101504151016293724
- GrahamSGamieZPolyzoisIProstaglandin EP2 and EP4 receptor agonists in bone formation and bone healing: in vivo and in vitro evidenceExpert Opin Investig Drugs200918746766
- ChikazuDLiXKawaguchiHBone morphogenetic protein 2 induces cyclooxygenase 2 in osteoblasts via a Cbfal binding site: role in effects of bone morphogenetic protein 2 in vitro and in vivoJ Bone Miner Res2002171430144012162497
- NanjundaiahSMVenkateshaSHYuHTongLStainsJPMoudqilKDCelastrus and its bioactive celastrol protect against bone damage in autoimmune arthritis by modulating osteoimmune cross-talkJ Biol Chem201222222162222622549786
- GanKXuLFengXCelastrol attenuates bone erosion in collagen-induced arthritis mice and inhibits osteoclast differentiation and function in RANKL-induced RAW264.7Int Immunopharmacol20152423924625529994
