Abstract
Purpose
To determine the effects of vaginal birth after cesarean (VBAC) versus repeated cesarean sections (RCS) after a primary cesarean section (CS), on the rate of intraoperative and postpartum maternal morbidity.
Patients and methods
This is a retrospective population-based cohort study. During the study period (1988–2005) there were 200,012 deliveries by 76,985 women at our medical center; 16,365 of them had a primary CS, of which 7429 women delivered a singleton infant after the primary CS, met the inclusion criteria, were included in our study, and were followed for four consecutive deliveries. Patients were divided into three study groups according to the outcome of their consecutive delivery after the primary CS: VBAC (n = 3622), elective CS (n = 1910), or an urgent CS (n = 1897). Survival analysis models were used to investigate the effect of the urgency of CS and the numbers of pregnancy predating the primary CS on peripartum complications.
Results
Women who failed a trial of labor had a higher rate of uterine rupture than those who had a VBAC. Patients who delivered by CS had a higher rate of endometritis than those giving birth vaginally. The rate of cesarean hysterectomy and transfer to other departments increased significantly at the fourth consecutive surgery (P = 0.02 and P = 0.003, respectively). VBAC was associated with a 55% reduction in the risk of intrapartum complications in comparison to a planned CS (hazard ratio [HR] 0.45; 95% confidence interval [CI]: 0.22–0.89. A greater maternal parity at the time of primary CS was associated with lower intrapartum and postpartum morbidities (HR 0.44; 95% CI: 0.24–0.79; HR 0.54; 95% CI: 0.47–0.62, respectively).
Conclusions
(1) A successful VBAC is associated with a reduction in the intrapartum complications; and (2) maternal morbidity increases substantially from the fourth consecutive cesarean delivery.
Introduction
Cesarean section (CS) is the most common surgery performed in the US and its rate is progressively rising throughout the world.Citation1 The major increase in the CS rate in western societies was recorded between the 1970s and early 1980s. A transient decrease in primary CS, along with an increase in vaginal birth after cesarean (VBAC), was observed between 1989 and 1996;Citation2 however, since 1996, the total cesarean rate has been annually increasing reaching 27.6% in 2003Citation3 and 30.1% in 2006.Citation4
Maternal morbidity associated with a CS is substantially higher than that of a vaginal delivery.Citation5–Citation7 Therefore, VBAC had been regarded as an effective method to reduce the rate of recurrent cesarean deliveries. However, recent studies demonstrated higher maternal and fetal complications in patients undergoing a trial of labor after CS than in those electively delivered by an elective repeated CS.Citation8–Citation10 Indeed, a symptomatic uterine rupture occurred in 0.5%–0.7% of women who underwent a trial of laborCitation11 and the rate of hypoxic–ischemic encephalopathy increases among patients who attempt a trial of labor especially in cases of uterine rupture during this process.Citation11–Citation14 Because of that, the American College of Obstetrics and Gynecology (ACOG), has recommended that a trial of labor after cesarean delivery is to be done only in hospitals that have facilities for emergency CS. The new guidelines say that hospitals ill-equipped for immediate surgery should help women find care elsewhere and have a plan to manage uterine ruptures.Citation15
Thus far, the data regarding maternal complications of deliveries following a CS (either by VBAC or elective repetitive CS), has mainly focused on the first birth after the primary CS. In contrast, there is a paucity of information concerning maternal morbidity associated with either repeated VBAC or repeated CS (RCS). The aims of this large population cohort study including women with a prior CS were to: (1) compare the maternal morbidity associated with elective repetitive CSs and repeated VBACs; and (2) compare the maternal morbidity of an elective repetitive CS with that of an emergency CS due to failed trial of labor.
Materials and methods
Study population and selection of patients
This retrospective population-based cohort study included 7429 women with a singleton pregnancy who delivered subsequently to a primary CS at the Soroka University Medical Center, a regional tertiary medical center in Beer Sheva, Israel, where all the births in the region take place. Cases were identified by searching a computerized birth records database. Women included in the study were followed up to a maximum of four consecutive deliveries after their primary CS in the univariate analyses.
Outcome variables
Data concerning demographic characteristics, medical and obstetric history, as well as pregnancy, delivery, and perinatal outcome, were obtained from the computerized database. The primary outcomes were the rate of intrapartum and postpartum maternal complications during consecutive trials of labor and the intraoperative and postoperative complications of patients with repetitive CS. The data were analyzed by two methods: (1) the effect of recurrent CSs versus repeated VBACs on intrapartum, operative, and postpartum complications; and (2) the effect of a failure in trial of labor on maternal morbidity.
For patients who attempted a VBAC, intrapartum complications included failure to progress during the first and second stages of labor, placental abruption, uterine rupture, uterine scar dehiscence, instrumental delivery, blood product transfusion, and the need for urgent CS. Postpartum complications included postpartum fever, endometritis, urinary tract infection, anemia, uterine rupture, blood product transfusion, and transfer to other departments (ie, intensive care unit).
For patients who underwent a CS, either elective or urgent, intraoperative complications included infection, trauma to adjacent organs, hysterectomy, blood products transfusion, and transfer to another department after CS. Post-operative complications included: reopening of cesarean scar, disruption of cesarean scar, and wound infection.
Statistical analysis
Maternal demographic characteristics, peripartum complications, and perinatal outcomes were compared with a two-step analysis. First, we compared the rate of complications between patients who underwent repeated VBAC and those who had RCSs. Subsequently, we compared the rate of complications of elective and urgent CS in patients with RCS and in those who failed a trial of VBAC. Student’s t-test was used to compare means for normally distributed variables. Chi-square and Fisher exact tests were used to compare categorical variables. Cox proportional hazard regression was performed to investigate the association between repeated VBAC, maternal parity at primary CS, and urgent versus planned CS, to peripartum and postpartum complications. A P value of <0.05 was considered significant. Analysis was done using SAS packages (version 9.1; SAS Institute, Cary, NC).
Results
During the study period (1988–2005) there were 200,012 deliveries by 76,985 women at our medical center; 16,365 of them had a primary CS, of which 7429 women delivered a singleton infant after the primary CS, met the inclusion criteria, and were included in our study (the indication and perinatal complication leading to the primary CS are presented in Supplementary Table 1). The study population was further divided according to the outcome of the subsequent delivery after the primary CS: 48.8% (3622/7429) had a successful trial of labor and were included in the VBAC group; 25.5% (1897/7429) had an urgent CS due to maternal or fetal indication and comprised the urgent CS group; and 25.7% (1910/7429) who had an elective CS and were included in that group.
The rate of trial of labor after a primary CS was 74.3% (5519/7429); of these 65.6% (3622/5516) succeeded and had a VBAC. The distribution of repeated VBACs, elective and urgent cesarean deliveries up to four consecutive deliveries after the primary CS, are presented in . The proportion of VBAC out of all the deliveries increases with each additional consecutive birth, and women in the VBAC group had a higher chance of having four consecutive deliveries after the primary CS than women in the urgent CS (odds ratio [OR], 2.13; 95%; confidence interval [CI]: 2.43–3.54) or the elective CS (OR, 13; 95% CI: 9.16–18.55) groups. Of interest is the finding that women included in the urgent CS group had a higher chance of having four consecutive deliveries after the primary CS than those included in the elective CS group (OR, 4.44; 95% CI: 3.03–6.53) (). Demographic characteristics of the study groups are presented in .
Figure 1 Mode of delivery in consecutive deliveries after the primary CS of patients who had a (A) VABC, (B) urgent CS, or (C) elective CS.
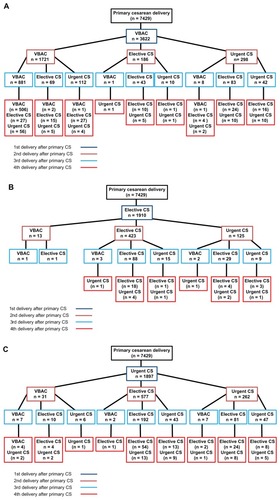
Figure 2 The rate of VBAC, urgent CS and elective CS in the subsequent deliveries after the primary CS.
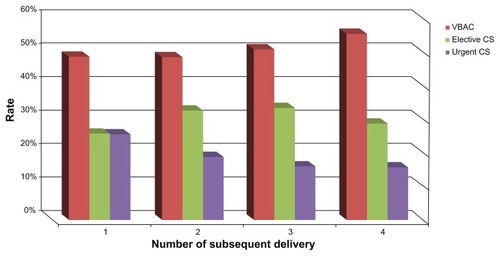
Table 1 Demographic characteristics of patients at subsequent pregnancy after primary cesarean delivery according to the route of delivery
The rate of pregnancy and peripartum complications of the consecutive deliveries after the primary CS is presented in Supplementary Table 2. Patients with RCS, compared to those who had repeated VBACs, had a higher rate of pregnancy complications. A leading indication for repeated urgent CS after the primary CS was labor dystocia; this was the indication for 39.3% of the urgent CSs in the delivery following the primary CS. Of interest, the rate of labor dystocia declined to about 15% of the subsequent deliveries (Supplementary Tables 3–5).
Patients with RCS were more likely to require blood products transfusion than patients in the VBAC group. There was no difference in the rate of uterine rupture between those with RCS and those with consecutive VBACs. The rate of these complications did not differ between urgent and elective CS (). In the first three subsequent deliveries after the primary CS, patients with RCS had higher rates of postpartum fever and endometritis than those with consecutive VBACs ().
Table 2 Delivery related complications of patients with consecutive VBAC without CS or consecutive CS without VBAC
Table 3 Post-partum related complications of patients with consecutive VBAC without CS or consecutive CS without VBAC
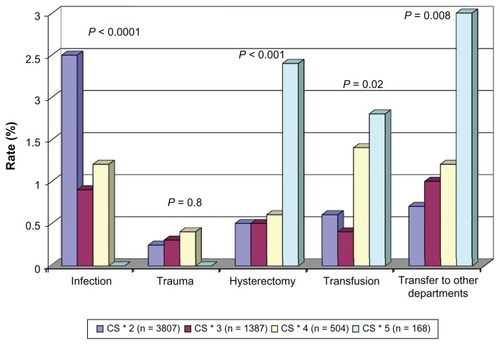
In patients undergoing repeated cesarean deliveries, the rate of blood products transfusion, trauma to adjacent organs, endometritis, postpartum fever, and urinary tract infections did not significantly change with the increase in the number of recurrent cesarean deliveries. However, the rate of cesarean hysterectomy and transfer to other departments increased significantly at the fourth consecutive surgery (P = 0.02 and P = 0.003, respectively) (). The major indications for cesarean hysterectomy were uterine rupture and hemorrhage. The rate of placenta accrete differed among the study group and was highest among the elective CS group 0.73% (14/1910), followed by the urgent CS group 0.16% (3/1897), and lowest among those who had VBAC 0.08% (3/3622; P < 0.001).
Figure 3 Intraoperative complications of patients with recurrent CS.
The neonatal outcome of the study groups is presented in Supplementary Tables 6–8. The rate of 1-minute Apgar score <5 was higher among patients with recurrent CS than in those with consecutive VBACs in all subsequent pregnancies following the primary CS. However, the rate of 5-minute Apgar score <7 did not differ significantly between the study groups in all the subsequent deliveries after the primary CS. The total perinatal mortality rate was higher among women who had a VBAC in the first delivery after the primary CS than in those with recurrent CS, mainly due to a higher rate of antepartum death in the VBAC group. However, in the fourth delivery after the primary CS, women with recurrent CS had a higher rate of total perinatal mortality than those with repeated VBACs, mainly due to a higher rate of postpartum death (Supplementary Tables 7 and 8).
The contribution of a failure in a trial of labor to maternal morbidity is a key question. In order to address it we further analyzed our data including patients who had an urgent cesarean delivery due to labor dystocia. In comparison to women undergoing a nonurgent CS, those who failed a trial of labor had a higher rate of CS complications in general (P < 0.001), infections, and the need to transfer to another department in the second and third delivery after the primary CS ().
Table 4 Intraoperative complications of patients who failed a trial of labor and those who had a nonurgent CS
In comparison to those who had a successful VBAC, those who failed in a trial of labor had a higher rate of uterine rupture (P < 0.001). Of interest, the rate of uterine rupture did not differ between those who had a nonurgent CS and those who failed a trial of labor ().
Table 5 Delivery-related complications of patients who failed a trial of labor, those who had a nonurgent CS and those who had a VBAC
To study the additive effect of RCS versus subsequent VBACs we constructed a Cox proportional hazard model separately for intrapartum and postpartum maternal morbidity, in which the outcome of nonurgent repeated morning CS served as the reference point and was compared to the outcome of VBAC and urgent CS at each consecutive delivery. The number of deliveries after the primary CS served as the time parameter. In the model for intrapartum complications, a protective effect was given by any additional VBAC (HR, 0.45; 95% CI: 0.22–0.9) and by maternal parity at primary CS (HR, 0.44; 95% CI: 0.24–0.79) (). Urgent CS was not associated with a significant change in the risk of intrapartum complications versus nonurgent repeated morning CS. In the model for maternal postpartum morbidity, only maternal parity at primary CS had a significant protective effect (HR, 0.54; 95% CI: 0.47–0.62) (). The introduction of maternal age and labor dystocia to the model did not affect its results ().
Table 6a Cox proportional hazard ratio for factors associated with intra-partum and post-partum complications
Table 6b Cox proportional hazard ratio for factors associated with intra-partum and post-partum complications
Discussion
Principal findings of the study
A successful trial of labor after a primary CS is associated with a higher future parity. In comparison to those who delivered by RCS in all subsequent pregnancies, patients who delivered consecutively by repeated VBACs had a lower maternal morbidity, and a 51.9% reduction in the risk of intrapartum complications for each successful trial of labor. A failure in a trial of labor is a major cause of maternal morbidity, mainly in the first delivery after the primary CS.
What is the effect of repeated VBACs versus recurrent CS
The finding that repeated trials of labor ending in successful VBACs are associated with lower maternal morbidity than RCS is novel. This study is the first to compare the outcome of consecutive VBAC to RCSs. Indeed, women who underwent repeated vaginal deliveries after the primary CS had lower rate of blood products transfusion and postpartum infections than women who had repeated cesareans. The finding that each additional VBAC, when compared to elective RCS, was associated with a 55% reduction in the risk for intrapartumand postpartum complication in comparison to elective CS, is novel and further emphasizes the safety and the benefit of a successful trial of labor.
Repeated VBACs were associated with an overall reduction in intrapartum and postpartum maternal morbidity with every additional delivery. This is in accord with the findings of Mercer et al,Citation16 who reported that among 13,532 women from 19 medical centers across the US, VBAC success increased with increasing number of prior VBACs. The rate of uterine rupture decreased after the first successful VBAC and did not increase thereafter. The risk of uterine dehiscence and other peripartum complications also declined substantially after the first successful VBAC. In comparison to the findings of this group, we had a lower rate of uterine rupture in every additional VBAC, and a somewhat lower rate of successful VBAC in each consecutive delivery. The main explanation for this observation is that some of the centers included in the study of Mercer et alCitation16 allowed patients with more than one CS to go into a trial of labor, while in our center more than one CS is a contraindication for a trial of labor. Collectively, our findings and those of others support the protective and positive effect of recurrent VBAC on maternal morbidity.
In contrast to the beneficial effect of recurrent VBAC, repeated cesarean deliveries are associated with increased maternal morbidity. We report herein that the rate of uterine rupture, hysterectomy, blood and blood product transfusion, and the need for transferring the patient to other departments rises with the increasing number of cesarean deliveries, especially after the fourth consecutive CS. This is in accord with previous reports: Makoha et alCitation17 noted similar elevation maternal morbidity, including placenta previa, placenta accreta, hysterectomy, adhesions, bladder injury, postoperative hemoglobin deficit, and need for blood transfusion with an increasing number of cesarean deliveries; and Silver et al,Citation18 for the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network, reported that the risks of placenta accreta, cystotomy, bowel injury, ureteral injury, and ileus, the need for postoperative ventilation, intensive care unit admission, hysterectomy, and blood transfusion requiring four or more units, and the duration of operative time and hospital stay, significantly increased with an increasing number of cesarean deliveries. Similarly to our findings, Silver et alCitation18 reported that there was a substantial increase in the risk for several morbidities, including placenta accreta, cystotomy, and need for hysterectomy or intensive care unit admission with the fourth or greater cesarean delivery. Thus, although there is no strict cut off regarding the number of consecutive CSs, it seems that the maternal risk for serious intraoperative complications increases substantially from the fourth RCS. This information should be included while counseling patients regarding repeated cesarean births.
An additional effect of repeated VBACs is the higher number of subsequent deliveries after the primary CS in comparison to those of women who had an elective or urgent RCS. Of interest is the fact that a higher proportion of those who underwent an urgent CS, immediately after the primary CS, had four subsequent pregnancies in comparison to those who had an elective CS. This finding is novel, and it may reflect the differences in the study population; meaning that a higher proportion of patients who choose to have an elective cesarean after the primary CS have a tendency to smaller families than those who attempt a trial of labor after the primary CS. Indeed, the sharp decline in the number of deliveries in this group is after the third cesarean. Guise et alCitation19 proposed that a woman’s decision to undergo a trial of labor after a primary CS is a complex process that is affected by medical, cultural, behavioral, and legal factors. The retrospective nature of our study does not allow us a deeper and more thorough investigation into these factors in relation to our population. A specially designed prospective study will need to be conducted in order to address the effect of these factors on the patient’s decision to undergo a trial of labor versus elective CS; nevertheless, educating women about their options early enough in pregnancy for them to make an informed choice is a key factor in this process.
What is the effect of labor dystocia on the success of a trial of labor?
The success of a trial of labor is an end point of many variables. Some of these parameters have been included in different prediction modelsCitation20–Citation23 aiming to assess the probability of a given patient to deliver vaginally after a primary CS. According to our findings, labor dystocia is a significant contributor to a failure of a trial of labor mainly in the first delivery after a primary CS. Dystocia was the indication for almost 40% of the urgent CS in the delivery following the primary CS, yet in the subsequent deliveries, its rate declined to about 15% of the urgent CS. This finding further emphasizes previously published data that women with a history of a labor dystocia which led to their primary CS have a lower chance to succeed in a trial of labor in the subsequent birth.Citation24–Citation27 In addition, our finding that the rate of dystocia as an indication for urgent CS declines in the following deliveries suggests that women who twice failed a trial of labor probably deliver by elective CS in their subsequent pregnancies or stop delivering. Indeed, in our cohort, only 45.9% of women who had an urgent CS during the subsequent birth after the primary cesarean had additional deliveries, mostly by elective CS. In contrast to this group, 60.9% of women who had a successful VBAC after the primary CS continued to deliver and only 8.4% of them had an elective CS. Collectively the data presented herein suggest that the success in vaginal delivery at the subsequent birth after the primary CS has important implication for maternals health and reproductive future. Those who prevail in the trial of labor and have a VBAC will have overall higher pregnancy rate and lower maternal morbidity than those who failed a trial of labor and women who chooses elective RCS.
Strength and limitation of the study
The limitation of this study is its retrospective nature and the fact that the data are derived from a database which has inherited limitations. Moreover, in the analysis of the data it seems that the inclination of the medical team is to go for a RCS whenever the patient has an additional pregnancy complication aside from the previous CS, which may lead to a bias towards allowing a trial of labor only for the healthier women. We could not ascertain this bias; nevertheless, the large number of deliveries included in our study over such a long period, as well as the fact that all the deliveries of our region take place at our medical center, assure us that the data presented herein is a representative sample of our obstetric population.
Conclusion
In summary, repeated VBACS are associated with a lower intrapartum maternal morbidity than planned recurrent cesarean deliveries. The recently published National Institute of Child Health and Human Development (Bethesda, MD) consensus regarding VBAC, states that about 30% of maternal fetal medicine fellows do not consult patients with a previous CS regarding the possibility of a trial of labor.Citation2 The findings of the current study and others may be used to reduce this trend among obstetricians and increase the rate of trial of labor. Moreover, the findings of this study further emphasize the point that a woman who desires large families should be offered a trial of labor after her primary cesarean delivery, especially if she had vaginal deliveries prior to her CS.
Supplementary clinical definitions
Parity groups were defined as follows: multipara (two to five deliveries) and grand-multipara (six or more deliveries). Hypertension was defined in the presence of blood pressure ≥140/90 mmHg recorded in two separate measurements at least 4 hours apart. Mild hypertension was defined as a diastolic blood pressure ≥90 mmHg and <110 mmHg and/or systolic blood pressure ≥140 mmHg and <160 mmHg. Severe hypertension was def ined in the presence of diastolic blood pressure ≥110 mmHg and systolic blood pressure ≥160 mmHg. Gestational hypertension was defined in the presence of hypertension developed after 20 weeks of gestation without proteinuria. Preeclampsia was diagnosed in the presence of elevated blood pressure and proteinuria of at least + 1 in dipstick; its severity was defined according to the severity of hypertension and/or one of the following + 3 proteinuria by dipstick, thrombocytopenia ≤100,000, elevated liver enzymes, persistent headache and/or blurred vision.Citation28 Gestational diabetes was diagnosed according to oral glucose tolerance test and was classified according to White’s classification. Citation29 Hydramnios (amniotic fluid index [AFI]) > 25 cm or when a vertical pocket of at least 8 cm was measured or as a subjective estimation of increased amniotic fluid volume. Oligohydramnios (AFI) <5 cm, a real-time scanner equipped with a 3.5/5 MHz transducer of appropriate focal length estimated amniotic fluid volume. Preterm delivery was defined as delivery before completion of 37 weeks of gestation.
Newborns were classified according to their weight as: small for gestational age (SGA), birthweight less than the 10th percentile; adequate for gestational age (AGA), birthweight from 10th–90th percentile; and large for gestational age (LGA), birthweight >90th percentile according to regional growth curves.Citation30 Prelabor rupture of membranes (PROM) was defined as rupture of the chorioamniotic membranes before the onset of labor. Uterine rupture was defined as a complete tear of the uterine wall, including the visceral peritoneum with establishment of a direct communication between the uterine and abdominal cavities. Dehiscence was defined as an opening of the previous cesarean scar with intact visceral peritoneum and no direct communication between the uterine and abdominal cavities. Postpartum fever was defined as maternal temperature ≥38°C, which developed at least 24 hours after delivery recorded in two different measurements at least 4 hours apart or one measurement of maternal temperature of ≥38.5°C regardless of the time after delivery. Endometritis was defined as postpartum maternal fever with clinical signs of tenderness above the uterine fundus or during cervical manipulation, foul vaginal discharge and positive endometrial culture. Wound infection was defined according to either clinical signs of infection or positive wound culture. Wound dehiscence was defined as spontaneous opening of CS wound including the abdominal fascia.
Supplementary Table
Table S1. Indications and perinatal complications for primary CS
Table S2. Peri-partum complications in the first delivery after primary CS
Table S3. Peri-partum complications in the second delivery after primary CS
Table S4. Peri-partum complications in the third delivery after primary CS
Table S5. Peri-partum complications in the fourth delivery after primary CS
Table S6. Perinatal outcome of first delivery after primary cesarean delivery according to the route of delivery
Table S7. Neonatal complications in patients with consecutive CS
Table S8. Neonatal complications in patients with consecutive VBAC
Disclosure
The authors report no conflicts of interest in this work and the study was self-funded.
References
- MartinJAHamiltonBESuttonPDVenturaSJMenackerFKirmeyerSBirths: final data for 2004Natl Vital Stat Rep20065511101
- BangdiwalaSIBrownSSCunninghamFGNIH Consensus Development Conference Draft Statement on Vaginal Birth After Cesarean: New InsightsNIH Consens State Sci Statements2010310273 [Epub ahead of print.]
- MenackerFTrends in cesarean rates for first births and repeat cesarean rates for low-risk women: United States, 1990–2003Natl Vital Stat Rep200554418
- MartinJAHamiltonBESuttonPDCenters for Disease Control and Prevention National Center for Health Statistics National Vital Statistics SystemBirths: final data for 2005Natl Vital Stat Rep2007566110318277471
- Lydon-RochelleMTGardellaCCárdenasVEasterlingTRRepeat cesarean delivery: what indications are recorded in the medical chart?Birth200633141116499526
- AllenVMOConnellCMBaskettTFMaternal morbidity associated with cesarean delivery without labor compared with induction of labor at termObstet Gynecol2006108228629416880297
- MillerDACholletJAGoodwinTMClinical risk factors for placenta previa-placenta accretaAm J Obstet Gynecol199717712102149240608
- FlammBLGoingsJRLiuYWolde-TsadikGElective repeat cesarean delivery versus trial of labor: a prospective multicenter studyObstet Gynecol19948369279328190433
- GrobmanWAGilbertSLandonMBOutcomes of induction of labor after one prior cesareanObstet Gynecol20071092 Pt 126226917267822
- McMahonMJLutherERBowesWAJrOlshanAFComparison of a trial of labor with an elective second cesarean sectionN Engl J Med1996335106896958703167
- LandonMBHauthJCLevenoKJNational Institute of Child Health and Human Development Maternal-Fetal Medicine Units NetworkMaternal and perinatal outcomes associated with a trial of labor after prior cesarean deliveryN Engl J Med2004351252581258915598960
- EndresLKBarnhartKSpontaneous second trimester uterine rupture after classical cesareanObstet Gynecol2000965 Pt 280680811094213
- GuiseJMMcDonaghMSOsterweilPNygrenPChanBKHelfandMSystematic review of the incidence and consequences of uterine rupture in women with previous caesarean sectionBMJ20043297456192515231616
- WenSWRusenIDWalkerMMaternal Health Study Group, Canadian Perinatal Surveillance SystemComparison of maternal mortality and morbidity between trial of labor and elective cesarean section among women with previous cesarean deliveryAm J Obstet Gynecol200419141263126915507951
- ACOG Practice bulletin no. 115: vaginal birth after previous cesarean deliveryObstet Gynecol20101162 Pt 145046320664418
- MercerBMGilbertSLandonMBNational Institute of Child Health and Human Development Maternal-Fetal Medicine Units NetworkLabor outcomes with increasing number of prior vaginal births after cesarean deliveryObstet Gynecol20081112 Pt 128529118238964
- MakohaFWFelimbanHMFathuddienMARoomiFGhabraTMultiple cesarean section morbidityInt J Gynaecol Obstet200487322723215548394
- SilverRMLandonMBRouseDJNational Institute of Child Health and Human Development Maternal-Fetal Medicine Units NetworkMaternal morbidity associated with multiple repeat cesarean deliveriesObstet Gynecol200610761226123216738145
- GuiseJMEdenKEmeisCVaginal birth after cesarean: new insightsEvid Rep Technol Assess (Full Rep)2010139720629481
- CostantineMMFoxKByersBDValidation of the prediction model for success of vaginal birth after cesarean deliveryObstet Gynecol200911451029103320168103
- GrobmanWALaiYLandonMBNational Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units Network (MFMU)Development of a nomogram for prediction of vaginal birth after cesarean deliveryObstet Gynecol2007109480681217400840
- GrobmanWALaiYLandonMBDoes information available at admission for delivery improve prediction of vaginal birth after cesarean?Am J Perinatol2009261069370119813165
- GrobmanWALaiYLandonMBEunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units NetworkCan a prediction model for vaginal birth after cesarean also predict the probability of morbidity related to a trial of labor?Am J Obstet Gynecol2009200156. e1e618822401
- PeacemanAMGersnoviezRLandonMBNational Institute of Child Health and Human Development Maternal-Fetal Medicine Units NetworkThe MFMU Cesarean Registry: impact of fetal size on trial of labor success for patients with previous cesarean for dystociaAm J Obstet Gynecol200619541127113117000245
- LandonMBLeindeckerSSpongCYNational Institute of Child Health and Human Development Maternal-Fetal Medicine Units NetworkThe MFMU Cesarean Registry: factors affecting the success of trial of labor after previous cesarean deliveryAm J Obstet Gynecol20051933 Pt 21016102316157104
- BujoldEGauthierRJShould we allow a trial of labor after a previous cesarean for dystocia in the second stage of labor?Obstet Gynecol200198465265511576583
- BaisJMvan der BordenDMPelMVaginal birth after caesarean section in a population with a low overall caesarean section rateEur J Obstet Gynecol Reprod Biol200196215816211384799
- ACOG Committee on Practice Bulletins–ObstetricsACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, Jan 2002Obstet Gynecol200299115916716175681
- WhitePPregnancy complicating diabetesAm J Med19497560961615396063
- LeibermanJRFraserDWeitzmanSGlezermanMBirthweight curves in southern Israel populationsIsr J Med Sci19932941982038155098