Abstract
Currently, there is no definitive cure for epilepsy. The available medications relieve symptoms and reduce seizure attacks. The major challenge with the available antiepileptic medication is safety and affordability. The repurposing of montelukast for epilepsy can be an alternative medication with a better safety profile. Montelukast is a leukotriene receptor antagonist that binds to the cysteinyl leukotrienes (CysLT) receptors used in the treatment of bronchial asthma and seasonal allergies. Emerging evidence suggests that montelukast’s anti-inflammatory effect can help to maintain BBB integrity. The drug has also neuroprotective and anti-oxidative activities to reduce seizure incidence and epilepsy. The present review summarizes the neuropharmacological actions of montelukast in epilepsy with an emphasis on the recent findings associated with CysLT and cell-specific effects.
Introduction
Epilepsy is one of the most common chronic brain diseases and it affects over 70 million people worldwide.Citation1 Epilepsy is life-altering, in part, because it is unpredictable, and as such it curtails daily activities like driving, attending school, and working.Citation2 Available anti-epilepsy treatment options include medications, keto diets, vagal nerve stimulation, and surgery.Citation3 However, the currently available anti-epileptic medications do not bring a definitive cure.Citation4 More than one-third of the epileptic patients who take the currently available drugs do not get the required benefit. These drugs also have serious side effects.Citation5 Particularly, pregnant women, children, the elderly, and patients with chronic comorbidities such as chronic kidney or liver disease are at higher risk of toxicity from those drugs.Citation6,Citation7 Developing a new anti-epileptic medication could be expensive and time consuming. Repurposing available medications could reduce the cost and time required for the discovery of new anti-epileptic drug.
Montelukast is a cysteine leukotriene receptors (CysLTR) antagonist which is currently being used for the treatment of bronchial asthma and seasonal allergies.Citation8,Citation9 In recent years, montelukast has been reported to have beneficial pharmacological effects in the nervous,Citation10 cardiovascular,Citation8 and cerebrovascular systems.Citation11 Epidemiologic studies have shown that montelukast reduces the incidence and severity of seizures.Citation12,Citation13 These results indicate that montelukast could be developed into a disease-modifying drug for epilepsy. This review summarizes the current findings on the role of montelukast to control seizures.
Epilepsy Pathophysiology and Cysteine Leukotrienes
Leukotrienes (LTs) are one of the major constituents of biologically active eicosanoids.Citation14 LTs are secreted during inflammation by mast cells, eosinophil, and leukocytes.Citation15 They possess a wide range of biological activities including leukocyte chemotaxis, vascular leakage, endothelial cell migration, smooth muscle cells and astrocyte proliferation.Citation15
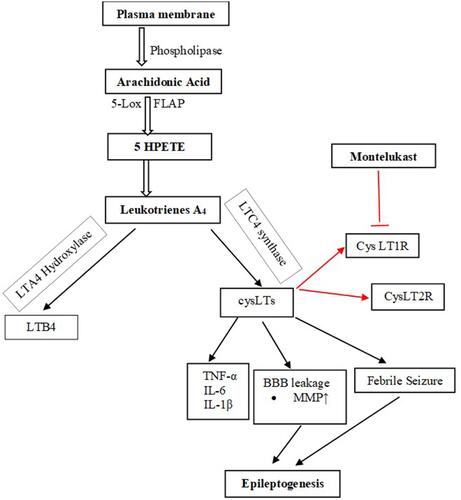
In the human body, LTs are derived de novo from arachidonic acid (AA).Citation16 AA is released from membrane phospholipids through the action of phospholipase A2.Citation17 The biosynthesis of LTs from AA is dependent on the action of the enzyme 5-lipoxygenase and its activating protein, 5-lipoxygenase activating protein (FLAP).Citation8 There are five types of LTs: leukotriene A4 (LTA4), leukotriene B4 (LTB4), leukotriene C4 (LTC4), leukotriene D4 (LTD4), and leukotriene E4 (LTE4).Citation16 LTA4 and LTB4 are non-cysteinyl leukotrienes as they lack the cysteine moietyCitation18 which is present in the Cys-LTs (LTC4, LTD4, and LTE4)Citation15 ().
Figure 1 Biosynthesis pathway of the Cys-LT and their receptors. Biosynthesis of CysLTs starts with the release of arachidonic acid from plasma membrane by the action of phospholipase. Arachidonic acid is metabolized to leukotriene A4 that in turn is metabolized to both non-cysteine leukotriene, LTB4, and cysteine leukotrienes. The CysLTs act on the receptors, CysLT1R and CysLT2R. Montelukast competitively block the effects of CysLTs on these receptors. The red color of the arrows show the site where montelukast acts.
Cysteinyl leukotrienes exhibit several biological activities in nanomolar concentrations through at least two specific G-protein coupled receptor subtypes named CysLTR-1 and CysLTR-2 which show 38% homolog.Citation19 Different studies have demonstrated that binding of LTD4 to the CysLT1 receptor leads to G-protein activation and the release of secondary intracellular messengers including diacylglycerol, inositol phosphates, and Ca2þ. This is followed by the activation of protein kinase C and accompanied by the mobilization of Ca2þ derived from both intracellular and extracellular stores.Citation20,Citation21 Furthermore, CysLT1 receptor activation by LTD4 has been reported to be associated with a transduction system based on the activation of phosphoinositide-3-kinase, extracellular-receptor kinase, mitogen-activated protein kinase, nuclear factor-kB (NF-kB), tumor necrosis factor, and matrix metalloproteinases-9 pathway.Citation22
Cys-LTs also induce the release of Matrix metallopeptidases (MMPs), including MMP-2 and MMP-9, inflammatory cytokines such as interleukins (ILs), NF-kB, and tumor necrosis factor- α (TNF-α) from macrophages through the cys-LT1 receptor.Citation23,Citation24 The release of these inflammatory mediators was highly associated with Amyloid beta1-42 (Ab1–42) induced cytotoxicity.Citation10
LTs and 5-lipoxygenase metabolite overexpression cause severe tissue damage. Relative to airway inflammation, many mediators, such as orupeptides and substance P, play a role in many of these interactions with LTs.Citation25 During inflammatory activation, LTs are synthesized and become functional. CysLTs induce smooth muscle contraction, vascular leakage,Citation26 eosinophil recruitment, mucus production and chemotaxis. LTB4 induces leukocyte chemoattraction, particularly of granulocytes and T cells, rapid invasion and recruitment of these cells to the plasma membrane of endothelial cells and production of reactive oxygen species.Citation18 CysLTs bind to their two receptors, CysLT1R and CysLT2R. These receptors are therapeutic targets for drug development to cure asthma and other immune diseases.Citation27 CysLT1 receptors also mediate astrocyte proliferation, which is the basis of post-ischaemic astrocytosis and glial scar formation.Citation28 CysLT1 receptor antagonists can inhibit ischaemia-like injury-induced astrocytosis, thereby inhibiting glial scar formation.Citation29
The role of inflammation in central nervous system disease pathogenesis has already been widely investigated, and elevated serum inflammatory mediators have been found in many neurological disorders.Citation30 Experimental and clinical studies have shown that seizures induce brain inflammation and recurrent seizures perpetuate chronic inflammation.Citation31 In a healthy brain, the expression of the CysLTRs is weak, but it was reported to increase during several pathological conditions.Citation19 Earlier studies have associated CysLTs and their receptors with several neurodegenerative disorders like, multiple sclerosis, parkinson’s disease, Huntington’s disease, epilepsy, traumatic brain injuryCitation32,Citation33 and alzheimer’s disease.Citation18
Emerging evidence indicates that inflammatory mediators including LTD4 play a relevant role in the pathophysiology of epilepsy.Citation19 However, only a few studies have investigated the role of LOX- derived arachidonic acid metabolites in epilepsy. Leukotriene levels were found to increase in a time-dependent manner in the brain during kainate-induced seizures in rats. Besides, LTD4 Intracerebroventricular (ICV) injection facilitated pentylenetetrazol (PTZ) induced seizures and increased Blood Brain Barrier (BBB) permeability in mice.Citation34 This effect could be relevant since magnetic resonance imaging studies in patients with post-traumatic epilepsy demonstrated that the site of increased BBB permeability colocalized with the presumed epileptic focus and animal studies found a positive correlation between the extent of BBB opening and the number of seizures.Citation35
Chemically induced seizures in rodents are associated with an early upregulation of hippocampal 5-lipoxygenase enzyme and resultant accumulation of leukotrienes.Citation21 Spontaneously epileptic gerbils have demonstrated higher levels of cysteinyl-leukotriene formation in their brain tissue than their normal counterparts.Citation36 Leukotrienes level increased in the brain during kainate-induced seizures.Citation34
In addition, kainic acid-induced seizures are associated with increased brain levels of leukotrienes and PGF2a in the cortex, hippocampus, and hypothalamus of rats.Citation37 The effects of pharmacological treatment, kindling, and challenge with PTZ on CysLT1 and CysLT2 receptor immunoreactivity in the cerebral cortex of mice were examined. It was found that epilepsy is associated with increased levels of inflammatory mediators in the brain, including leukotrienes, which are produced by neurons, glia, and endothelial cells in the BBB.Citation12 Neutrophils that have breached the BBB can lead to the immediate synthesis of CysLTs.Citation38 Farias et al demonstrated that cysLTs significantly increase after fluid percussion-induced brain injury, being detected as early as 10 min after injury and continuing to rise over an hour.Citation39 A pharmacological data provided by Lenz et al also indicated that CysLT1R antagonism maintains BBB integrity.Citation34 In accordance, Palmer et al demonstrated that LTD4 increases the firing rate of Purkinje cells in vivo, suggesting an excitatory role for this lipid mediator.Citation40 Glutamate released during seizures acts on capillary NMDA receptors to cause blood-brain barrier disruption through cPLA2, COX-2 and 5-LOX leading to increased MMP expression, degradation of Tight Junction Proteins (TJs) and increased barrier leakage which increases the likelihood of further seizures.Citation41,Citation42
Pharmacological modulation of 5-lipooxygenase, an enzyme required for the biosynthesis of leukotrienes, has been shown to potentiate the protective effect of a COX-2 inhibitor on kainic acid induced seizures in rodents.Citation21 Inhibition of LOX using dual inhibitors of LOX/COX pathway like phenidone and BW755C has led to decreased production of CysLTs and attenuated seizure activity, respectively.Citation43 Similarly, zileuton, a LOX inhibitor, was shown to decrease spike-wave discharges in pilocarpine-induced epileptic rats, strongly suggesting that leukotrienes play a role in epilepsy.Citation19 Montelukast, a CysLT1 receptor inverse agonist and 1,2,3,4-tetrahydroisoquinoline, regarded as a LTD4 synthetic pathway inhibitor, dose-dependently suppress the development of kindled seizures, as well as pilocarpine-induced spontaneous recurrent seizures.Citation21 Interestingly, it has been shown that while LTD4 facilitates, montelukast, pranlukast and Bay-u9773 (a dual CysLT1/CysLT2 antagonist) decrease PTZ-induced seizures and BBB permeability disruption. Pranlukast, zafirlukast and montelukast are cysLT-1 antagonists that are available in the market.Citation44
Repurposing of Montelukast as an Antiepileptic Drug
Montelukast, 1-((1(R)-(3-(2-(7-chloro-2-quinolinyl)-(E)-ethenyl)phenyl)-3-[(2-(1-hydroxy-1-methylethyl)phenyl)propyl)thiol]-methyl)] cyclopropane acetate, is a selective CysLT1 receptor antagonistCitation45 possessing anti-inflammatory effects and has been widely used for the treatment of inflammatory diseases such as asthma and allergic rhinitis.Citation46 Montelukast was approved for use in the United States in 1998 and is widely used with more than 20 million prescriptions being filled yearly.Citation47 Montelukast is the most prescribed CysLT1 receptor antagonist in Europe and the USA.Citation48
Montelukast showed a neuroprotective effect through antioxidant, anti-inflammatory, and antiapoptotic mechanisms.Citation49 It is reported to have a neuroprotective activity in several neuronal disorders such as alzheimer’s disease, cerebral ischemia, multiple sclerosis and seizures.Citation13,Citation50 Other studies also displayed that it possesses a wide spectrum of anti-inflammatory properties in several chronic diseases.Citation8 The evidences of the antiepileptic activities of montelukast from animal studies are summarized below ().
Table 1 Preclinical Studies Done on the Antiepileptic Effect of Montelukast
Montelukast protected hippocampal tissue by reducing oxidative stress, inflammatory and apoptotic markers.Citation11 Furthermore, it reduced glutamate and lactate dehydrogenase activity as well as infarct size elevated by ischemia/reperfusion.Citation49 Montelukast markedly reduced ox-LDL-induced adhesion of monocytes to endothelial cells.Citation8 An in vitro study has recently shown that montelukast suppressed phagocytosis induced by rotenone and decreased the subsequent proinflammatory cytokine release.Citation36
Montelukast Suppresses inflammatory mediators induced by TNF-a.Citation23 It induces M2 macrophagesCitation51 polarization which is important in the removal of cellular debris, embryonic development, and tissue repair.Citation52 It also suppresses the activity of MMP-2 and MMP-9.Citation53 Montelukast, MK571, and zafirlukast (inverse agonists of CysLT1R) increased cell surface receptor expression in COS-7 cells while LTD4 (a CysLT1 receptor agonist) did the opposite.Citation12 Several forms of brain injuries trigger leukotriene production, including ischemia, trauma, stroke, and seizures, which are associated with increased BBB permeability.Citation54 Epilepsy-related BBB disruption is mediated by Cys-LT and modulation of Cys-LT by montelukast suppresses the development and frequency of seizures in vivo.Citation34 Montelukast and LTD4, respectively, reduced and increased the BBB disruption induced by PTZ.Citation12 Montelukast prevented PTZ-induced BBB disruption by inhibiting paracellular diffusion and leukocyte infiltration and slowing the onset of PTZ-induced seizures.Citation34 Obermeier et al’s finding indicated that the maintenance of BBB integrity may underlie the currently reported anticonvulsant effect of CysLT1R antagonists.Citation55 Intracerebroventricular injection of montelukast prevented seizures and maintained the BBB integrity at the same range of doses and increased latency to seizures correlated with low BBB permeability scores.Citation34
Moreover, the ICV injection of LTD4 facilitates the convulsant effect of PTZ and reverts the anticonvulsant action of montelukast which constitutes converging pharmacological evidence for the involvement of CysLT receptors in seizures.Citation12,Citation19 The two other CysLT receptor antagonists (pranlukast and Bay-u9973) also decreased PTZ-induced seizures which indicated that CysLT receptors' role in seizures.Citation45,Citation56 Montelukast suppressed the development of kindled seizures, as well as pilocarpine-induced spontaneous recurrent seizures in mice. Clinical evidence highlights the efficacy of cysLT receptor antagonists such as pranlukast in patients with intractable partial epilepsy.Citation57 Pranlukast reduced seizure frequencies probably normalizing MMP-9 in serum, reducing leakage of proinflammatory cytokines into CNS, and inhibiting extravasation of leucocytes from brain capillaries.Citation19,Citation57 Inflammatory cytokines and matrix metalloproteinases that cause degradation of the extracellular matrix IL-1 and TNF-α receptors are rapidly upregulated in neurons during seizures, suggesting that they mediate the effects of cytokines on neuronal excitability.Citation58 Cytokine receptors in the CNS are expressed by neurons, microglia,Citation59 and astrocytes.Citation60 Evidence exists for cell type–specific IL-1β signaling in the CNS through the IL-1 type 1 receptor: IL-1β activates the p38 mitogen-activated protein kinase pathway in neurons, leading to induction of cyclic adenosine monophosphate response element–binding protein, whereas NF-κB is activated predominantly in astrocytes, suggesting that this cytokine may have distinct functional effects on neurons and glia.Citation61
Ab1–42-induced CysLT1R expression results in neurotoxicity, inflammatory and apoptotic responses in cultured primary neurons.Citation62,Citation63 Ab1-42 is involved in the pathologic mechanisms of axon damage, axon growth, and network reorganization observed in refractory epilepsyCitation64 and late onset epilepsy of unknown origin mediated by D1 receptor.Citation65 This is because of Ab1–42 activated nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signaling by selectively inducing the nuclear translocation of p65 and p50 subunits, and promoting expression of genes such as proinflammatory or apoptotic profile.Citation66 Treatment with montelukast was able to decrease this increment of nuclear p65 subunit which indicates that montelukast may block Ab1–42-activated NF-κB signaling in primary neurons.Citation10,Citation67 Moreover, blockade of CysLT1R with montelukast reversed Ab1–42-mediated increase of CysLT1R expression, and concomitant changes of the pro-inflammatory factors and the apoptosis-related proteins which result in Ab1–42-associated late onset of epilepsy.Citation68
Conclusion
Overexpression of cysLT in the brain causes the tissue damage, which is responsible for the pathogenesis of many neurological disorders including epilepsy. Various experimental studies indicated that montelukast which is a potent cysLT receptor antagonist blocked CNS inflammation resulting in neuro-protection, treating febrile seizures, potentiate the action of the old antiepileptic drugs, and maintained BBB integrity from dysfunction. It is also relatively safe drug as it has been used for the treatment of asthma for more than two decades. Therefore, montelukast has the potential to be an alternative treatment for epilepsy. However, further studies of both preclinical and clinical studies are required before considering montelukast for a prescription to treat epilepsy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
- Thijs RD, Surges R, O’Brien TJ, Sander JW. Epilepsy in adults. Lancet. 2019;393(10172):689–701. doi:10.1016/S0140-6736(18)32596-0
- Brueggeman L, Sturgeon ML, Martin RM, et al. Drug repositioning in epilepsy reveals novel antiseizure candidates. Ann Clin Transl Neurol. 2019;6(2):295–309. doi:10.1002/acn3.703
- Guberman A. Vagus nerve stimulation in the treatment of epilepsy. Cmaj. 2004;171(10):1165–1166. doi:10.1503/cmaj.1041039
- D’Ambrosio R, Eastman CL, Fattore C, Perucca E. Novel frontiers in epilepsy treatments: preventing epileptogenesis by targeting inflammation. Expert Rev Neurother. 2013;13(6):615–625. doi:10.1586/ern.13.54
- Ventola CL. Epilepsy management: newer agents, unmet needs, and future treatment strategies. Pharm Ther. 2014;39(11):776.
- Asconapé JJ. Use of antiepileptic drugs in hepatic and renal disease. In: Handbook of Clinical Neurology. Vol. 119. Elsevier; 2014:417–432.
- Wahab A. Difficulties in treatment and management of epilepsy and challenges in new drug development. Pharmaceuticals. 2010;3(7):2090–2110. doi:10.3390/ph3072090
- Zhou L, Sun X, Shi Y, Liu J, Luan G, Yang Y. Cysteinyl leukotriene receptor type 1 antagonist montelukast protects against injury of blood–brain barrier. Inflammopharmacology. 2019;27(5):933–940. doi:10.1007/s10787-019-00611-7
- Scholz BH. Neuropsychiatric disorder and montelukast: a case report and vigibase® analysis. Arch Dis Child. 2019;104(1):54–55.
- Lai J, Mei ZL, Wang H, et al. Montelukast rescues primary neurons against Aβ1-42-induced toxicity through inhibiting CysLT1R-mediated NF-κB signaling. Neurochem Int. 2014;75(May):26–31. doi:10.1016/j.neuint.2014.05.006
- Hoxha M, Lewis-Mikhael A-M, Bueno-Cavanillas A. Potential role of leukotriene receptor antagonists in reducing cardiovascular and cerbrovascular risk: a systematic review of human clinical trials and in vivo animal studies. Biomed Pharmacother. 2018;106:956–965. doi:10.1016/j.biopha.2018.07.033
- Fleck J, Temp FR, Marafiga JR, et al. Montelukast reduces seizures in pentylenetetrazol-kindled mice. Brazilian J Med Biol Res. 2016;49(4):1–7. doi:10.1590/1414-431X20155031
- Cevik B, Solmaz V, Aksoy D, Erbas O. Montelukast inhibits pentylenetetrazol-induced seizures in rats. Med Sci Monit. 2015;21:869–874. doi:10.12659/MSM.892932
- Wang D, DuBois RN. Eicosanoids and cancer. Nat Rev Cancer. 2010;10(3):181. doi:10.1038/nrc2809
- Ghosh A, Chen F, Thakur A, Hong H. Cysteinyl leukotrienes and their receptors: emerging therapeutic targets in central nervous system disorders. CNS Neurosci Ther. 2016;22(12):943–951. doi:10.1111/cns.12596
- Izumi T, Yokomizo T, Obinata H, Ogasawara H, Shimizu T. Leukotriene receptors: classification, gene expression, and signal transduction. J Biochem. 2002;132(1):1–6. doi:10.1093/oxfordjournals.jbchem.a003185
- Sun GY, Shelat PB, Jensen MB, He Y, Sun AY, Simonyi A. Phospholipases A2 and inflammatory responses in the central nervous system. Neuromolecular Med. 2010;12(2):133–148. doi:10.1007/s12017-009-8092-z
- Rahman SO, Singh RK, Hussain S, Akhtar M, Najmi AK. A novel therapeutic potential of cysteinyl leukotrienes and their receptors modulation in the neurological complications associated with Alzheimer’s disease. Eur J Pharmacol. 2019;842:208–220. doi:10.1016/j.ejphar.2018.10.040
- Gelosa P, Colazzo F, Tremoli E, Sironi L, Castiglioni L. Cysteinyl leukotrienes as potential pharmacological targets for cerebral diseases. Mediators Inflamm. 2017;2017:1–15. doi:10.1155/2017/3454212
- Williamson JR, Cooper RH, Joseph SK, Thomas AP. Inositol trisphosphate and diacylglycerol as intracellular second messengers in liver. Am J Physiol Physiol. 1985;248(3):C203–C216. doi:10.1152/ajpcell.1985.248.3.C203
- Rehni AK, Singh TG. Modulation of leukotriene D4 attenuates the development of seizures in mice. Prostaglandins Leukot Essent Fat Acids. 2011;85(2):97–106. doi:10.1016/j.plefa.2011.04.003
- Savari S, Vinnakota K, Zhang Y, Sjölander A. Cysteinyl leukotrienes and their receptors: bridging inflammation and colorectal cancer. World J Gastroenterol. 2014;20(4):968. doi:10.3748/wjg.v20.i4.968
- Kawai Y, Narita Y, Yamawaki-Ogata A, Usui A, Komori K. Montelukast, a cysteinyl leukotriene receptor 1 antagonist, induces m2 macrophage polarization and inhibits murine aortic aneurysm formation. Biomed Res Int. 2019;2019:1–11. doi:10.1155/2019/9104680
- Yokomizo T, Nakamura M, Shimizu T. Leukotriene receptors as potential therapeutic targets. J Clin Invest. 2018;128(7):2691–2701. doi:10.1172/JCI97946
- Kaya Z, Yayla M, Cinar I, et al. Effect of montelukast, a cysteinyl leukotriene receptor-1 antagonist, on a rat model of acute bacterial sinonasal inflammation. Am J Rhinol Allergy. 2019;33(5):559–566. doi:10.1177/1945892419852576
- Dupré DJ, Le Gouill C, Gingras D, Rola-Pleszczynski M, Staňková J. Inverse agonist activity of selected ligands of the cysteinyl-leukotriene receptor 1. J Pharmacol Exp Ther. 2004;309(1):102–108. doi:10.1124/jpet.103.059824
- Laidlaw TM, Boyce JA. Cysteinyl leukotriene receptors, old and new; implications for asthma. Clin Exp Allergy. 2012;42(9):1313–1320. doi:10.1111/j.1365-2222.2012.03982.x
- Ciccarelli R, D’Alimonte I, Santavenere C, et al. Cysteinyl‐leukotrienes are released from astrocytes and increase astrocyte proliferation and glial fibrillary acidic protein via cys‐LT1 receptors and mitogen‐activated protein kinase pathway. Eur J Neurosci. 2004;20(6):1514–1524. doi:10.1111/j.1460-9568.2004.03613.x
- Robel S. Astroglial scarring and seizures: a cell biological perspective on epilepsy. Neurosci. 2017;23(2):152–168.
- Skaper SD, Facci L, Zusso M, Giusti P. An inflammation-centric view of neurological disease: beyond the neuron. Front Cell Neurosci. 2018;12:72.
- Vezzani A, French J, Bartfai T, Baram TZ. The role of inflammation in epilepsy. Nat Rev Neurol. 2011;7(1):31. doi:10.1038/nrneurol.2010.178
- Sharma R, Leung WL, Zamani A, O’brien TJ, Espinosa PMC, Semple BD. Neuroinflammation in post-traumatic epilepsy: pathophysiology and tractable therapeutic targets. Brain Sci. 2019;9(11):318. doi:10.3390/brainsci9110318
- Lucas S, Rothwell NJ, Gibson RM. The role of inflammation in CNS injury and disease. Br J Pharmacol. 2006;147(S1):S232–S240. doi:10.1038/sj.bjp.0706400
- Lenz QF, Arroyo DS, Temp FR, et al. Cysteinyl leukotriene receptor (CysLT) antagonists decrease pentylenetetrazol-induced seizures and blood–brain barrier dysfunction. Neuroscience. 2014;277:859–871. doi:10.1016/j.neuroscience.2014.07.058
- Vezzani A, Friedman A, Dingledine RJ. The role of inflammation in epileptogenesis. Neuropharmacology. 2013;69:16–24. doi:10.1016/j.neuropharm.2012.04.004
- Mansour RM, Ahmed MAE, El-Sahar AE, El Sayed NS. Montelukast attenuates rotenone-induced microglial activation/p38 MAPK expression in rats: possible role of its antioxidant, anti-inflammatory and antiapoptotic effects. Toxicol Appl Pharmacol. 2018;358(September):76–85. doi:10.1016/j.taap.2018.09.012
- Sperk G, Lassmann H, Baran H, Kish SJ, Seitelberger F, Hornykiewicz O. Kainic acid induced seizures: neurochemical and histopathological changes. Neuroscience. 1983;10(4):1301–1315. doi:10.1016/0306-4522(83)90113-6
- Michael J, Marschallinger J, Aigner L. The leukotriene signaling pathway: a druggable target in Alzheimer’s disease. Drug Discov Today. 2019;24(2):505–516. doi:10.1016/j.drudis.2018.09.008
- Farias S, Frey LC, Murphy RC, Heidenreich KA. Injury-related production of cysteinyl leukotrienes contributes to brain damage following experimental traumatic brain injury. J Neurotrauma. 2009;26(11):1977–1986. doi:10.1089/neu.2009.0877
- Palmer MR, Mathews WR, Hoffer BJ, Murphy RC. Electrophysiological response of cerebellar Purkinje neurons to leukotriene D4 and B4. J Pharmacol Exp Ther. 1981;219(1):91–96.
- Van Vliet EA, Otte WM, Wadman WJ, et al. Blood-brain barrier leakage after status epilepticus in rapamycin-treated rats I: magnetic resonance imaging. Epilepsia. 2016;57(1):59–69. doi:10.1111/epi.13246
- Rempe RG, Hartz AMS, Soldner ELB, et al. Matrix metalloproteinase-mediated blood-brain barrier dysfunction in epilepsy. J Neurosci. 2018;38(18):4301–4315. doi:10.1523/JNEUROSCI.2751-17.2018
- Simmet T, Tippler B. Cysteinyl-leukotriene production during limbic seizures triggered by kainic acid. Brain Res. 1990;515(1–2):79–86. doi:10.1016/0006-8993(90)90579-Z
- Theron AJ, Steel HC, Tintinger GR, Gravett CM, Anderson R, Feldman C. Cysteinyl leukotriene receptor-1 antagonists as modulators of innate immune cell function. J Immunol Res. 2014;2014:1–16. doi:10.1155/2014/608930
- Zhao R, Shi WZ, Zhang YM, Fang SH, Wei EQ. Montelukast, a cysteinyl leukotriene receptor-1 antagonist, attenuates chronic brain injury after focal cerebral ischaemia in mice and rats. J Pharm Pharmacol. 2011;63(4):550–557. doi:10.1111/j.2042-7158.2010.01238.x
- Kawai Y, Narita Y, Ogata A, Usui A, Komori K. Therapeutic potential of montelukast, cysteinyl leukotriene receptor 1 antagonist, for aortic aneurysm. Eur J Vasc Endovasc Surg. 2019;58(6):e419. doi:10.1016/j.ejvs.2019.06.1064
- Health NI. Livertox: clinical and research information on drug-induced liver injury. US Natl Libr Med. 2017.
- Montuschi P, Sala A, Dahlen S-E, Folco G. Pharmacological modulation of the leukotriene pathway in allergic airway disease. Drug Discov Today. 2007;12(9–10):404–412. doi:10.1016/j.drudis.2007.03.004
- Saad MA, Abdelsalam RM, Kenawy SA, Attia AS. Montelukast, a cysteinyl leukotriene receptor-1 antagonist protects against hippocampal injury induced by transient global cerebral ischemia and reperfusion in rats. Neurochem Res. 2014;40(1):139–150. doi:10.1007/s11064-014-1478-9
- Jadidi-Niaragh F, Mirshafiey A. Histamine and histamine receptors in pathogenesis and treatment of multiple sclerosis. Neuropharmacology. 2010;59(3):180–189. doi:10.1016/j.neuropharm.2010.05.005
- Lin Y-C, Huang M-Y, Lee M-S, et al. Effects of montelukast on M2-related cytokine and chemokine in M2 macrophages. J Microbiol Immunol Infect. 2018;51(1):18–26. doi:10.1016/j.jmii.2016.04.005
- Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013;496(7446):445. doi:10.1038/nature12034
- Liu D, Ge S, Zhou G, et al. Montelukast inhibits matrix metalloproteinases expression in atherosclerotic rabbits. Cardiovasc Drugs Ther. 2009;23(6):431. doi:10.1007/s10557-009-6211-6
- Bıber N, Toklu HZ, Solakoglu S, et al. Cysteinyl-leukotriene receptor antagonist montelukast decreases blood–brain barrier permeability but does not prevent oedema formation in traumatic brain injury. Brain Inj. 2009;23(6):577–584. doi:10.1080/02699050902926317
- Obermeier B, Daneman R, Ransohoff RM. Development, maintenance and disruption of the blood-brain barrier. Nat Med. 2013;19(12):1584. doi:10.1038/nm.3407
- Wang M-L, Huang X-J, Fang S-H, et al. Leukotriene D4 induces brain edema and enhances CysLT2 receptor-mediated aquaporin 4 expression. Biochem Biophys Res Commun. 2006;350(2):399–404. doi:10.1016/j.bbrc.2006.09.057
- Takahashi Y, Imai K, Ikeda H, Kubota Y, Yamazaki E, Susa F. Open study of pranlukast add-on therapy in intractable partial epilepsy. Brain Dev. 2013;35(3):236–244. doi:10.1016/j.braindev.2012.04.001
- Kobylarek D, Iwanowski P, Lewandowska Z, et al. Advances in the potential biomarkers of epilepsy. Front Neurol. 2019;10.
- Hanisch U-K. Microglia as a source and target of cytokine activities in the brain. In: Microglia in the Regenerating and Degenerating Central Nervous System. Springer; 2002:79–124.
- Rothhammer V, Quintana FJ. Control of autoimmune CNS inflammation by astrocytes. In: Seminars in Immunopathology. Vol. 37. Springer; 2015:625–638.
- Vezzani A, Granata T. Brain inflammation in epilepsy: experimental and clinical evidence. Epilepsia. 2005;46(11):1724–1743. doi:10.1111/j.1528-1167.2005.00298.x
- Awasthi A, Matsunaga Y, Yamada T. Amyloid-beta causes apoptosis of neuronal cells via caspase cascade, which can be prevented by amyloid-beta-derived short peptides. Exp Neurol. 2005;196(2):282–289. doi:10.1016/j.expneurol.2005.08.001
- Tang -S-S, Hong H, Chen L, et al. Involvement of cysteinyl leukotriene receptor 1 in Aβ1–42-induced neurotoxicity in vitro and in vivo. Neurobiol Aging. 2014;35(3):590–599. doi:10.1016/j.neurobiolaging.2013.09.036
- Sima X, Xu J, Li J, Zhong W, You C. Expression of β‑amyloid precursor protein in refractory epilepsy. Mol Med Rep. 2014;9(4):1242–1248. doi:10.3892/mmr.2014.1977
- Costa C, Parnetti L, D’Amelio M, et al. Epilepsy, amyloid-β, and D1 dopamine receptors: a possible pathogenetic link? Neurobiol Aging. 2016;48:161–171. doi:10.1016/j.neurobiolaging.2016.08.025
- Bales KR, Du Y, Dodel RC, Yan G-M, Hamilton-Byrd E, Paul SM. The NF-κB/Rel family of proteins mediates Aβ-induced neurotoxicity and glial activation. Mol Brain Res. 1998;57(1):63–72. doi:10.1016/S0169-328X(98)00066-7
- Weiskirchen R. Commentary: montelukast prevents mice against acetaminophen-induced liver injury. Front Pharmacol. 2019;10:1289. doi:10.3389/fphar.2019.01289
- Larner AJ. Epileptic seizures in AD patients. Neuromolecular Med. 2010;12(1):71–77. doi:10.1007/s12017-009-8076-z
- Elwany NE. Protective effect of montelukast against pentylenetetrazole- induced acute seizures and kindling in mice. ZUMJ. 2015;21(6).
- Fleck J, Marafiga JR, Jesse AC, Ribeiro LR, Rambo LM, Mello CF. Montelukast potentiates the anticonvulsant effect of phenobarbital in mice: an isobolographic analysis. Pharmacol Res. 2015;94:34–41. doi:10.1016/j.phrs.2015.02.001
