Abstract
The subject of this narrative review is macrotrabecular-massive hepatocellular carcinoma (MTM‐HCC). Despite their rarity, these tumours are of general interest because of their epidemiological and clinical features and for representing a distinct model of the interaction between the angiogenetic system and neoplastic cells. The MTM‐HCC subtype is associated with various adverse biological and pathological parameters (the Alfa-foetoprotein (AFP) serum level, tumour size, vascular invasion, and satellite nodules) and is a key determinant of patient prognosis, with a strong and independent predictive value for early and overall tumour recurrence. Gene expression profiling has demonstrated that angiogenesis activation is a hallmark feature of MTM-HCC, with overexpression of both angiopoietin 2 (ANGPT2) and vascular endothelial growth factor A (VEGFA).
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer in the world, with 841100 new cases in 2018, and it is the second leading cause of cancer death, with a 5-year survival of 18%. In terms of sex, HCC is the fifth most common cancer in males and the ninth most common cancer in females worldwide.Citation1 It has been reported that approximately 80% of HCC cases occur in developing countries. HCC appears frequently in patients with cirrhosis, and the most common risk factors include alcohol consumption, hepatitis B (HBV) or hepatitis C (HCV) virus infection and nonalcoholic steatohepatitis (NASH).Citation2,Citation3
HCC is a major health problem, and the majority of patients are diagnosed at an advanced stage, resulting in poor treatment outcomes.Citation4
According to EASL and AASLD guidelines, current HCC diagnosis does not require histological confirmation due to excellent reported diagnostic performance of imaging procedures.Citation4,Citation5
In patients with cirrhosis, HCC may be diagnosed noninvasively using multiphasic computed tomography (CT) or dynamic contrast material–enhanced magnetic resonance imaging (MRI) using the Liver Imaging Reporting and Data System (LI-RADS), which standardizes HCC imaging acquisition and terminology and enables accurate stratification of the probability of HCC and overall malignancy.Citation4,Citation6–8
Although numerous histological tumour variants have been reported over the last decades, there has been no robust determination of the clinical impact of pathological classification to date; therefore, a liver biopsy is needed to obtain more information on the clinical implications of the HCC histological subtype.
HCC is a highly heterogeneous cancer at both molecular and histological levels. The HCC phenotype appears to be closely related to particular gene mutations, tumour subgroups and/or oncogenic pathways. Several HCC subtypes characterized by histological features and growth patterns have been identified, including solid (compact), pseudoglandular/acinar, and trabecular patterns, as described in the current WHO classification.Citation9
These subtypes correlate with clinical features and prognosis but have not been thoroughly tested as predictors of a response to local or systemic therapies, which explains their limited clinical usefulness.Citation10
Recent studies have shown that the macrotrabecular-massive subtype of HCC (MTM-HCC) has distinct molecular features and poor prognosis among the aforementioned subtypes.Citation11
The subject of this review is this aggressive subtype of HCC: the diagnostic, associated clinicopathological and imaging features are analysed, and treatment is discussed with particular emphasis on actual knowledge and a brief parenthetical consideration of angiopoietin 2 inhibitors, an ongoing subject of discussion.
Histological Definition: Origins to the Present
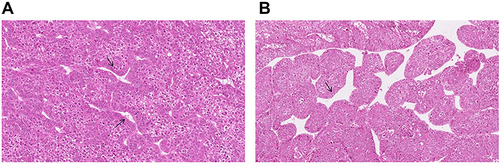
The most common growth pattern of HCC is a trabecular form that mimics normal hepatic cord plates. This growth pattern has been referred to as “macrotrabecular” (MT) when the trabeculae become >6 cells thick,Citation12,Citation13 and HCC in which the MT pattern constitutes >50% of the entire tumour is considered a subtype: macrotrabecular-massive hepatocellular carcinoma (MTM-HCC).Citation11–17
MT-HCC was first recognized as a distinct growth pattern in 1983,Citation12 but no studies supporting this observation have since been performed. There are only a few citations of MT-HCC in the literature.Citation11,Citation18,Citation19
The MTM-HCC subtype was first defined in a French collaborative study conducted by Calderaro.Citation17
In this systematic analysis of more than 340 HCCs, the cut-off for defining HCC as MTM-HCC was the presence of more than 50% of the MT pattern in a tumour, which in turn was defined as a hepatic cord thickness >6 cells.Citation17 Using biopsy samples, cases are classified as MTM-HCC if at least one focus of the macrotrabecular pattern is identified, without taking into account the areal percentage occupied by the pattern.Citation11
Compared to the results reported by the French group, Jean et al reported a lower cut-off of a ≥30% MTM pattern as a diagnostic criterion,Citation15 which needs to be validated by further studies ().
Histological Prevalence
An MTM-HCC incidence rate of approximately 10–15% has been reported in different studies.Citation11–16
Ziol et alCitation11 identified the macrotrabecular-massive subtype in 12% of cases in a cohort of 237 HCC surgical samples and 284 HCC liver biopsies. Rastogi performed a retrospective study on 217 HCC patients in which MT-HCC was diagnosed in 20/218 (9.2%) cases, with coexistence of macrotabecular and pseudoglandular patterns in 18% of cases.Citation21 By comparison, Lauwers et alCitation25 noted a macrotrabecular-predominant architecture in a higher number of cases (26.6% of 425 HCC resections).
In the study by Renne et al, MTM-HCC was identified in 7.8% of 541 resected HCCs from Italy, Korea and Japan,Citation20 whereas Feng et al reported MTM-HCC in 38% of 170 resected HCCs in China.Citation22
Coherently with Renne, Cannella et al found MTM-HCC in 7.8% of 295 HCCs cases.Citation23
In a recent American study,Citation24 MTM-HCC was reported in 7.1% of 378 HCC. However, the macrotrabecular pattern was more commonly seen in HCCs arising in non-fibrotic liver tissues compared with HCCs in cirrhosis (13.68% vs 4.95%) ().
Table 1 Macrotrabecular Tumour Incidence
Pathological Features
MTM patterns were found to be significantly correlated with the pathological features of aggressiveness, such as Edmondson grades III–IV (P = 0.001), and less pseudoglandular pattern.Citation20
In the Calderaro study,Citation17 the pathological features associated with the MTM-HCC subtype were satellite nodules and vascular invasion.
Rastogi et alCitation21 performed a study series in which it showed that the macrotrabecular pattern was often associated with poor grades of differentiation, the pT3 stage, tumour sizes of 2–5 cm and >5 cm, and high AFP levels.Citation21
In the Renne study, the MTM-HCC subtype was significantly enriched by vessels that encapsulated tumour clusters (VETC phenotype), which was defined as enrichment of ≥55% of the tumour area by CD34 immunostaining (P = 0.006).Citation20
Molecular Biology
Hepatocellular carcinoma cells accumulate somatic DNA alterations. The most frequent genetic alterations are mutations in the TERT promoter, accounting for approximately 60% of cases, followed by mutations in TP53 in approximately 30% of cases, WNT signalling (CTNNB1 and AXIN1 in approximately 40% and 10% of cases, respectively), or chromatin remodelling (ARID1A and ARID2 in approximately 10% and 5% of cases, respectively).Citation26
Calderaro et alCitation17 was the first to show that a TP53 mutation and FGF19 amplification were associated with the MTM-HCC subtype. A strong association with the G3 transcriptomic subgroup, a subclass linked to cell cycle activation and chromosomal instability, was also observed.Citation17
Interestingly, Li Li Liu et alCitation27 reported a higher expression of tumoral programmed death-ligand 1/chemokine-like factor (CKLF)-like MARVEL transmembrane domain containing 6 (PD-L1/CMTM6) and a higher inflammatory cell density in the MTM-HCC subtype compared to other subtypes. CMTM6 belongs to the chemokine-like factor (CKLF)-like MARVEL transmembrane domain-containing (CMTM) family and is a key regulator of PD-L1; that is, CMTM6 is an important immune checkpoint inhibitor that promotes PD-L1 expression in tumour cells in the defence against T cells.Citation28 In the Renne study, compared to other subtypes, the MTM-HCC subtype was significantly more frequent in p53+ and double-positive phenotypes (P53+ and β-catenin/GS+, with P < 0.001 and P = 0.046, respectively) and less frequent in the β-catenin/GS+ phenotype (P = 0.006).Citation20
The Role of Biopsy
The role of tumour biopsies in the management of patients with HCC is one of the most actively debated subjects in the liver cancer community.Citation29–31
MTM-HCC can be accurately diagnosed in biopsy samples through the identification of MTM patterns.Citation11
Using biopsies to identify morphology and molecular alterations is critically important for elucidating the mechanisms of carcinogenesis, improving diagnosis and prognostication, and finally facilitating the development of personalized medicine by identifying tumour entities with overexpressed PDL-1 that respond to immunotherapy.
Calderaro et alCitation32 used a molecular-driven selection of biomarkers to implement the diagnosis of HCC morphomolecular subtypes and identified ESM1 (endothelial specific molecule 1) as a reliable microenvironment immunohistochemical marker of MTM-HCC.Citation32
The very aggressive MTM-HCC subtype may lead to a reconsideration of the role of biopsy for HCC diagnosis because the identification of this subtype during pretherapeutic work-up may have strong prognostic implications. Indeed, patients may benefit from adjuvant therapies and/or upfront registration on the liver transplant waiting list after resection or RFA. However, no data are available on the prognostic value of the MTM-HCC subtype regarding recurrence after liver transplantation.
Clinical Features
Calderaro et al showed that the MTM-HCC subtype was characterized by HBV infection, a higher level of alpha-fetoprotein, early relapse and poor survival. Subsequent work by the same group also showed that this subtype was associated with advanced tumour stages, vascular invasion, and poor prognosis.Citation17
MTM-HCC is associated with poor survival in all studies. For example, Calderaro et al reported that the survival rate was 40% at 24 months in INSERM U1162 cohort and 60% at 24 months in validation cohort.Citation17
Although the available data are coherent, additional study series are needed to investigate the clinical impact of MTM-HCC.
Radiological Features of Macrotrabecular-Massive Hepatocellular Carcinoma
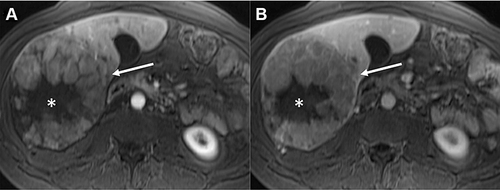
To date, few analyses have been performed on the radiological features of histologically confirmed MTM-HCC (). Most of these have focused on MRI presentations.
Table 2 Imaging Features of Macrotrabecular-Massive HCC Subtype
Macrotrabecular-massive HCC has been reported to be associated with a peculiar microvascular pattern described as a sinusoid-like microvascular pattern or “vessels that encapsulate tumour clusters” (VETC) pattern, appear as a cobweb-like network encapsulating individual HCC clusters.Citation33–35
HCCs with such vascular patterns exhibit a low microvascular density and frequent tumour necrosis, and low microvascular density is highly correlated with low arterial enhancement on MRI.Citation36
In line with these results, Rhee et alCitation14 used MRI data to show that the internal or diffuse hypovascular component (≥50% of the hypovascular component) of the arterial phase combined with two or more ancillary findings (intratumoural artery, arterial phase peritumoural enhancement, and nonsmooth tumour margin) was significantly associated with MTM-HCC and was associated with a poor prognosis.
Mulé et alCitation16 performed a retrospective study on 189 patients, in which MTM-HCCs were classified as LIRADS-5 on multiphase contrast-enhanced MRI and presented substantial necrosis that may help to identify the MTM-HCC subtype with high specificity.
Feng et alCitation22 confirmed previously reported results on MRI and were the first to report that substantial necrosis on CT was related to the presence of VETC.Citation22
Recently, Zhu et alCitation37 reported that for 88 patients with histologically confirmed HCC, intratumour fat was determined to be an independent predictor of MT-HCC, whereas necrosis was not.Citation37
A macrotrabecular area has also been more frequently observed in HCCs with arterial phase rim-like enhancement on gadoxetic acid-enhanced MRI.Citation15
Hence, the presence of substantial necrosis on imaging may lead to consideration for lesion biopsy with therapeutic and prognostic intent, especially as the MTM-HCC subtype can be accurately diagnosed in biopsy samples.Citation11
In a recent Italo-French study,Citation23 the larger size, the presence of tumor in vein (TIV), at least 1 LR-M feature (LI-RADS major features, ie non-rim APHE, non-peripheral “washout”, and enhancing “capsule”), infiltrative appearance and necrosis or severe ischaemia were significantly more frequent in MTM-HCCs than in other subtypes on contrast-enhanced CT).
In addition, TIV and larger size tended to be more frequent in MTM-HCCs on MRI too.Citation23
Imaging findings of MTM-HCC could help select HCC patients who show poor outcomes after curative treatment as potential candidates for clinical trials of neoadjuvant strategies ().
Figure 2 Radiological imaging of MTM-HCC. MR images in a 39-year-old woman with 13-cm heterogeneous macrotrabecular-massive hepatocellular carcinoma (MTM-HCC) in right liver lobe (arrow). Note the presence of a large central area without enhancement on late arterial (A) and venous (B) phases images, corresponding to substantial necrosis (*). Figure provided courtesy of Sébastien Mulé.
Treatment
According to the Barcelona Clinic Liver Cancer (BCLC), the only curative treatments for HCC to date – whatever the histological subtype (including MTM) – are liver transplantation, resection and in some cases thermal ablation. Compared to the standard surgical approach in HCC, there are no dedicated technical strategies allowing to improve survival outcomes. Systemic treatment is the only option for advanced HCC.Citation4 Sorafenib was the first agent shown to improve the survival of patients with advanced HCC or in cases of intermediate-stage disease despite progression with transarterial therapies.Citation38 Treatment practices have changed in recent years with the advent of LenvatinibCitation39 as another first-line treatment choice and Regorafenib,Citation40 Ramucirumab,Citation41 and CabozantinibCitation42 as second-line treatment options. Checkpoint-blockade immunotherapy targeting programmed cell death protein 1 (PD-1) has recently shown promising efficacy for HCC. In May 2020, the FDA approved a combination treatment of Atezolizumab and Bevacizumab for patients with unresectable or metastatic HCC who have not received prior systemic therapy based on the primary analysis results of the IMbrave150 study.Citation43
Li Li Lu et alCitation27 reported that the MTM-HCC subtype was characterized by a high expression of CMTM6/PD-L1, suggesting that MTM-HCC patients are suitable candidates for tumour immunotherapy.
Targeting particular subsets of tumours remains a promising approach, as shown by the recent success of the REACH-2 trialCitation41 that assessed the efficacy of Ramucirumab, an anti-angiogenic drug, in patients with elevated alpha-fetoprotein serum levels. Interestingly, MTM-HCC is characterized by increased levels of alpha-fetoprotein and activation of angiogenesis; the antitumour effect of Ramucirumab or other anti-angiogenic drugs in patients with this subtype of HCC should be assessed.Citation41
During trans-arterial chemoembolization (TACE), the ischemic damage caused by the arterial occlusion induces the production of the hypoxia-inducible factor (HIF)-1α, a known modulator of PD-L1 expression, decreased the percentage of T-regs and increased the CD4+/CD8+ ratio.Citation44
In particular, Montasser et al in their series with 11 cases of MTM-HCC demonstrated an increase of PD-1 and PD-L1 expression in HCC following TACE that supported the use of TACE in combination with immunotherapy.Citation45
This rationale guided the design of trials testing the combination of TACE and anti-PD-1 mAb (like, in NCT03397654 trial – pembrolizumab after TACE- or NCT03143270 trial – nivolumab with drug-eluting bead-TACE). More data are needed to evaluate the benefits of treatment combining TACE and checkpoint inhibitors in MTT-HCC.
Prognosis
HCC is a highly malignant tumour associated with a poor prognosis, and only a subset of patients are eligible for curative treatment options. Moreover, the recurrence rate is high.Citation5 The tumour size, vascular invasion, grading and staging are important variables for predicting HCC prognosis.Citation46
Although the MTM-HCC subtype is more prevalent in intermediate or advanced HCC, MTM-HCC represented a significant fraction (10%) of tumours classified as very early or early HCC (BCLC 0/A) in a cohort studied by Ziol et al.Citation11
Macrotrabecular-massive HCC (MTM-HCC) appears to be associated with early relapse after resection or percutaneous ablation, independent of classical clinical and radiological prognostic factors.Citation34
The MTM-HCC pattern was found to promote the metastatic potential of a mouse HCC cell line in vivo through the release of tumour clusters into the bloodstream in an epithelial-to-mesenchymal transition-independent manner.Citation34
In the same line, in a recent American study,Citation47 the authors identified the MTM subtype as the most common histo-morphologic features in primary tumors associated with metastasis amongst 39 HCC cases studied.
Calderaro et alCitation17 observed an association between MTM-HCC and poor prognosis (early relapse and poor survival). Major aggressiveness of this HCC subtype (major incidence of vascular invasion and satellite nodules) was also reported.
These features were confirmed in a report by Ziol et alCitation11 of a significantly higher recurrence rate and worse overall survival in patients with this HCC subtype compared to other subtypes. Similar results were found by Jeon et alCitation15 for patients who underwent liver resection/transplantation. Li Li Liu et alCitation27 showed that at the molecular level, CMTM6/PD-L1 expression was an independent prognostic factor for patient survival in the MTM-HCC subtype population, with increased risk of HCC progression and death.
The above-mentioned reported data are in line with those of Zhu et al,Citation48 showing that elevated expression of CMTM6 in a cohort of HCC cases was frequently accompanied by worsening of malignant phenomena, including high AFP levels, large tumour sizes, advanced TNM stages, and vascular invasion.
This association between macrotrabecular-massive growth pattern and higher AFP expression was recently confirmed by the recent studies of Cannella et alCitation23 Ridder et alCitation49 (Supplementary Material Figure S1).
New Perspectives
Angiopoietin 2 Inhibitors, An Ongoing Subject of Discussion
In MTM-HCC, angiopoietin 2 (ANGPT2) mRNA levels are overexpressed, along with a significant almost increasing trend in the vascular endothelial growth factor (VEGF) level.Citation17
To date, ANGPT2, in cooperation with VEGFA, is known to promote neoangiogenesis and endothelial sprouting in the tumoral environment.Citation50
It has also been shown that secretion of ANGPT2 by various primary solid tumours can induce metastasis via the extravasation of circulating tumour cellsCitation51 by loosening endothelial cell junctions and increasing vascular permeability of distant organs.Citation34,Citation52
In HCC, ANGPT2 produced by neoplastic cells may disseminate directly in adjacent liver parenchyma and contribute to the increased frequency of satellite nodules observed in MTM-HCC.
It is reasonable to expect that silencing the expression of ANGPT2 growth factor by neoplastic cells could disrupt the formation of this particular pattern and reduce both intrahepatic neoplasia and extrahepatic metastases.Citation34
Hashizume et alCitation53 have suggested that Ang2 inhibitors and VEGF inhibitors may have complementary antiangiogenic actions and effects on reducing tumour growth.
Ang2 inhibition prevents the growth of new vessels by endothelial sprout formation, whereas VEGF inhibition causes tumour vessel regression, and the formation of empty basement membrane sleeves reduces tumour growth. The combined blockade of Ang2 and VEGF has additive effects on sprouting and vessel regression and decelerates tumour growth.Citation53
Schmittnaegel et alCitation54 also demonstrated that blocking angiogenesis using these types of antibodies enhanced antitumour immunity (by increasing extravasation and perivascular accumulation of antitumour CD8+ cells and interferon-γ-producing cytotoxic T lymphocytes).Citation54
The synergistic use of ANGPT2 inhibitors and Bevacizumab (anti-VEGF) combined with immunotherapy could open novel therapeutic avenues for this highly aggressive HCC subtype and may represent a new tool for HCC treatment, bringing HCC molecular classification into clinical practice.
Artificial Intelligence: Which Role in the Future for MTT-HCC
The artificial intelligence (AI), computer-based algorithms for data analysis and by the construction of predictive models based on the usage of various imaging techniques, especially in combination with HCC molecular biomarkers, recently used for improving image recognition and representation in HCC diagnosis and prognosis.Citation55 For example, in their most recent article that represents a proof-of-principle study, Zeng et alCitation56 propose a novel approach using AI to predict activation of inflammatory gene signatures associated with increased sensitivity to immunotherapy, for improving personalized allocation of therapy. In this trend, the combination of artificial intelligence and automated computerized image analysis is likely to provide a new tool for MTM-HCC diagnosis and for characterisation of biomarkers to help in therapy work-up in the near future.
Conclusion
This article is a narrative review of the most recent data in the field of MTM-HCC, and provides insights on future directions and challenges.
In conclusion, MTM-HCC is an aggressive subtype of HCC characterized by vascular invasion, a higher level of alpha-fetoprotein, early relapse and poor survival.
Although the available data are coherent, additional study series are needed to investigate the clinical impact of MTM-HCC on treatment response. The development of particular therapeutic strategies and/or trials focusing on the particularly aggressive subtype of MTM-HCC should be considered. One limitation is the subjective nature of pathology and nonoptimal interobserver agreement among pathologists; however, artificial intelligence and automated computerized image analysis are likely to provide a unique opportunity to achieve consensus in MTM-HCC diagnosis in the near future.
Abbreviations
HCC, hepatocellular carcinoma; MTM-HCC, macrotrabecular hepatocarcinoma; LT, liver transplantation; PD-1, checkpoint-blockade immunotherapy targeting programmed cell death protein 1; CMTM6, chemokine-like factor-like (CKLF) MARVEL transmembrane domain-containing 6; ANGPT2, angiopoietin; VEGF, vascular endothelial growth factor; AFP, alpha-fetoprotein.
Disclosure
Hélène Regnault reports personal fees from Boston Scientific, outside the submitted work. Vincent Leroy reports personal fees from AbbVie, Intercept, and Mayoly, and grants and personal fees from Gilead, outside the submitted work. Julien Calderaro reports shares in Crosscope, and personal fees from Keen Eye, outside the submitted work. The authors report no other potential conflicts of interest in relation to this work.
Additional information
Funding
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
- El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142(6):1264–1273.e1. doi:10.1053/j.gastro.2011.12.061
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi:10.1002/hep.28431
- European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi:10.1016/j.jhep.2018.03.019
- Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723–750. doi:10.1002/hep.29913
- Tang A, Bashir MR, Corwin MT, et al.; LI-RADS Evidence Working Group. Evidence supporting LI-RADS major features for CT- and MR imaging-based diagnosis of hepatocellular carcinoma: a systematic review. Radiology. 2018;286(1):29–48. doi:10.1148/radiol.2017170554
- Chernyak V, Tang A, Flusberg M, et al. LI-RADS® ancillary features on CT and MRI. Abdom Radiol. 2018;43(1):82–100. doi:10.1007/s00261-017-1220-6
- Elsayes KM, Kielar AZ, Elmohr MM, et al. White paper of the Society of Abdominal Radiology hepatocellular carcinoma diagnosis disease-focused panel on LI-RADS v2018 for CT and MRI. Abdom Radiol. 2018;43(10):2625–2642. doi:10.1007/s00261-018-1744-4
- Nagtegaal ID, Odze RD, Klimstra D, et al.; WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76(2):182–188. doi:10.1111/his.13975
- Zucman-Rossi J, Villanueva A, Nault JC, Llovet JM. Genetic landscape and biomarkers of hepatocellular carcinoma. Gastroenterology. 2015;149(5):1226–1239.e4. doi:10.1053/j.gastro.2015.05.061
- Ziol M, Poté N, Amaddeo G, et al. Macrotrabecular-massive hepatocellular carcinoma: a distinctive histological subtype with clinical relevance. Hepatology. 2018;68(1):103–112. doi:10.1002/hep.29762
- Kishi K, Shikata T, Hirohashi S, Hasegawa H, Yamazaki S, Makuuchi M. Hepatocellular carcinoma. A clinical and pathologic analysis of 57 hepatectomy cases. Cancer. 1983;51(3):542–548. doi:10.1002/1097-0142(19830201)51:3<542::AID-CNCR2820510330>3.0.CO;2-2
- Kondo F, Wada K, Kondo Y. Morphometric analysis of hepatocellular carcinoma. Virchows Arch A Pathol Anat Histopathol. 1988;413(5):425–430. doi:10.1007/BF00716991
- Rhee H, Cho ES, Nahm JH, et al. Gadoxetic acid-enhanced MRI of macrotrabecular-massive hepatocellular carcinoma and its prognostic implications. J Hepatol. 2021;74(1):109–121. doi:10.1016/j.jhep.2020.08.013
- Jeon Y, Benedict M, Taddei T, Jain D, Zhang X. Macrotrabecular hepatocellular carcinoma: an aggressive subtype of hepatocellular carcinoma. Am J Surg Pathol. 2019;43(7):943–948. doi:10.1097/PAS.0000000000001289
- Mulé S, Galletto Pregliasco A, Tenenhaus A, et al. Multiphase liver MRI for identifying the macrotrabecular-massive subtype of hepatocellular carcinoma. Radiology. 2020;295(3):562–571. doi:10.1148/radiol.2020192230
- Calderaro J, Couchy G, Imbeaud S, et al. Histological subtypes of hepatocellular carcinoma are related to gene mutations and molecular tumour classification. J Hepatol. 2017;67(4):727–738. doi:10.1016/j.jhep.2017.05.014
- Torbenson MS. Morphologic subtypes of hepatocellular carcinoma. Gastroenterol Clin North Am. 2017;46(2):365–391. doi:10.1016/j.gtc.2017.01.009
- Tan PS, Nakagawa S, Goossens N, et al. Clinicopathological indices to predict hepatocellular carcinoma molecular classification. Liver Int. 2016;36(1):108–118. doi:10.1111/liv.12889
- Renne SL, Woo HY, Allegra S, et al. Vessels Encapsulating Tumor Clusters (VETC) is a powerful predictor of aggressive hepatocellular carcinoma. Hepatology. 2020;71(1):183–195. doi:10.1002/hep.30814
- Rastogi A, Maiwall R, Ramakrishna G, et al. Hepatocellular carcinoma: clinicopathologic associations amidst marked phenotypic heterogeneity. Pathol Res Pract. 2021;217:153290. doi:10.1016/j.prp.2020.153290
- Feng Z, Li H, Zhao H, et al. Preoperative CT for characterization of aggressive macrotrabecular-massive subtype and vessels that encapsulate tumor clusters pattern in hepatocellular carcinoma. Radiology. 2021;300(1):219–229. doi:10.1148/radiol.2021203614
- Cannella R, Dioguardi Burgio M, Beaufrère A, et al. Imaging features of histological subtypes of hepatocellular carcinoma: implication for LI-RADS. JHEP Rep. 2021;3(6):100380. doi:10.1016/j.jhepr.2021.100380
- Jain A, Mazer B, Deng Y, et al. Hepatocellular carcinoma: does the background liver with or without cirrhosis matter? Am J Clin Pathol. 2021;2021:aqab125.
- Lauwers GY, Terris B, Balis UJ, et al.; International Cooperative Study Group on Hepatocellular Carcinoma. Prognostic histologic indicators of curatively resected hepatocellular carcinomas: a multi-institutional analysis of 425 patients with definition of a histologic prognostic index. Am J Surg Pathol. 2002;26(1):25–34. doi:10.1097/00000478-200201000-00003
- Schulze K, Nault JC, Villanueva A. Genetic profiling of hepatocellular carcinoma using next-generation sequencing. J Hepatol. 2016;65(5):1031–1042. doi:10.1016/j.jhep.2016.05.035
- Liu LL, Zhang SW, Chao X, et al. Coexpression of CMTM6 and PD-L1 as a predictor of poor prognosis in macrotrabecular-massive hepatocellular carcinoma. Cancer Immunol Immunother. 2021;70(2):417–429. doi:10.1007/s00262-020-02691-9
- Burr ML, Sparbier CE, Chan YC, et al. CMTM6 maintains the expression of PD-L1 and regulates anti-tumour immunity. Nature. 2017;549(7670):101–105. doi:10.1038/nature23643
- Torbenson M, Schirmacher P. Liver cancer biopsy–back to the future?! Hepatology. 2015;61(2):431–433. doi:10.1002/hep.27545
- Mueller C, Waldburger N, Stampfl U, et al. Non-invasive diagnosis of hepatocellular carcinoma revisited. Gut. 2018;67(5):991–993. doi:10.1136/gutjnl-2017-314981
- Poté N, Cauchy F, Albuquerque M, et al. Contribution of virtual biopsy to the screening of microvascular invasion in hepatocellular carcinoma: a pilot study. Liver Int. 2018;38(4):687–694. doi:10.1111/liv.13585
- Calderaro J, Meunier L, Nguyen CT, et al. ESM1 as a marker of macrotrabecular-massive hepatocellular carcinoma. Clin Cancer Res. 2019;25(19):5859–5865. doi:10.1158/1078-0432.CCR-19-0859
- Tanigawa N, Lu C, Mitsui T, Miura S. Quantitation of sinusoid-like vessels in hepatocellular carcinoma: its clinical and prognostic significance. Hepatology. 1997;26(5):1216–1223. doi:10.1053/jhep.1997.v26.pm0009362365
- Fang JH, Zhou HC, Zhang C, et al. A novel vascular pattern promotes metastasis of hepatocellular carcinoma in an epithelial-mesenchymal transition-independent manner. Hepatology. 2015;62(2):452–465. doi:10.1002/hep.27760
- Yoon JH, Kim H. CT characterization of aggressive macrotrabecular-massive hepatocellular carcinoma: a step forward to personalized medicine. Radiology. 2021;300(1):230–232. doi:10.1148/radiol.2021210379
- Wang B, Gao ZQ, Yan X. Correlative study of angiogenesis and dynamic contrast-enhanced magnetic resonance imaging features of hepatocellular carcinoma. Acta Radiol. 2005;46(4):353–358. doi:10.1080/02841850510021247
- Zhu Y, Weng S, Li Y, et al. A radiomics nomogram based on contrast-enhanced MRI for preoperative prediction of macrotrabecular-massive hepatocellular carcinoma. Abdom Radiol. 2021;46(7):3139–3148. doi:10.1007/s00261-021-02989-x
- Llovet JM, Ricci S, Mazzaferro V, et al.; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi:10.1056/NEJMoa0708857
- Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised Phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–1173. doi:10.1016/S0140-6736(18)30207-1
- Bruix J, Qin S, Merle P, et al.; RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56–66. doi:10.1016/S0140-6736(16)32453-9
- Zhu AX, Kang YK, Yen CJ, et al.; REACH-2 study investigators. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(2):282–296. doi:10.1016/S1470-2045(18)30937-9
- Abou-Alfa GK, Meyer T, Cheng AL, et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N Engl J Med. 2018;379(1):54–63. doi:10.1056/NEJMoa1717002
- Finn RS, Qin S, Ikeda M, et al.; IMbrave150 Investigators. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi:10.1056/NEJMoa1915745
- Liao J, Xiao J, Zhou Y, et al. Effect of transcatheter arterial chemoembolization on cellular immune function and regulatory T cells in patients with hepatocellular carcinoma. Mol Med Rep. 2015;12(4):6065–6071. doi:10.3892/mmr.2015.4171
- Montasser A, Beaufrère A, Cauchy F, et al. Transarterial chemoembolisation enhances programmed death‐1 and programmed death‐ligand 1 expression in hepatocellular carcinoma. Histopathology. 2021;79(1):36–46. doi:10.1111/his.14317
- Zhang Y, Chen SW, Liu LL, Yang X, Cai SH, Yun JP. A model combining TNM stage and tumor size shows utility in predicting recurrence among patients with hepatocellular carcinoma after resection. Cancer Manag Res. 2018;10:3707–3715. doi:10.2147/CMAR.S175303
- Kumar D, Hafez O, Jain D, Zhang X. Can primary hepatocellular carcinoma histomorphology predict extrahepatic metastasis? Hum Pathol. 2021;113:39e46. doi:10.1016/j.humpath.2021.04.008
- Zhu X, Qi G, Li C, et al. Expression and clinical significance of CMTM6 in hepatocellular carcinoma. DNA Cell Biol. 2019;38(2):193–197. doi:10.1089/dna.2018.4513
- Ridder DA, Weinmann A, Schindeldecker M, et al. Comprehensive clinicopathologic study of alpha fetoprotein-expression in a large cohort of patients with hepatocellular carcinoma. Int J Cancer. 2022;150(6):1053–1066. doi:10.1002/ijc.33898
- Gerald D, Chintharlapalli S, Augustin HG, Benjamin LE. Angiopoietin-2: an attractive target for improved antiangiogenic tumor therapy. Cancer Res. 2013;73(6):1649–1657. doi:10.1158/0008-5472.CAN-12-4697
- Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell. 2011;147(2):275–292. doi:10.1016/j.cell.2011.09.024
- Huang Y, Song N, Ding Y, et al. Pulmonary vascular destabilization in the premetastatic phase facilitates lung metastasis. Cancer Res. 2009;69(19):7529–7537. doi:10.1158/0008-5472.CAN-08-4382
- Hashizume H, Falcón BL, Kuroda T, et al. Complementary actions of inhibitors of angiopoietin-2 and VEGF on tumor angiogenesis and growth. Cancer Res. 2010;70(6):2213–2223. doi:10.1158/0008-5472.CAN-09-1977
- Schmittnaegel M, Rigamonti N, Kadioglu E, et al. Dual angiopoietin-2 and VEGFA inhibition elicits antitumor immunity that is enhanced by PD-1 checkpoint blockade. Sci Transl Med. 2017;9(385):eaak9670. doi:10.1126/scitranslmed.aak9670
- Moldogazieva NT, Mokhosoev IM, Zavadskiy SP, et al. Proteomic profiling and artificial intelligence for hepatocellular carcinoma translational medicine. Biomedicines. 2021;9:159. doi:10.3390/biomedicines9020159
- Zeng Q, Klein C, Caruso S, et al. Artificial intelligence predicts immune and inflammatory gene signatures directly from hepatocellular carcinoma histology. J Hepatol. 2022;77:116–127. doi:10.1016/j.jhep.2022.01.018