Abstract
In recent years, there have been limited reports on the efficacy of later-line anti-programmed cell death −1 (PD-1) therapy in achieving prolonged and complete remission in patients with hepatocellular carcinoma (HCC). Tislelizumab, a humanized anti-PD-1 monoclonal IgG4 antibody, has shown promising results in the treatment of HCC. This report highlights the case of a patient with HCC who experienced the development of lung metastatic lesions following HCC resection and chemotherapy, but achieved a prolonged complete response (CR) after receiving tislelizumab treatment. In April 2017, a 56-year-old male diagnosed with primary HCC underwent hepatectomy and hepatic arterial infusion pump placement. Following the surgery, the patient received adjuvant hepatic arterial infusion chemotherapy (HAIC) with 4 cycles of cisplatin+5-fluorouracil (PF) regimen starting in June 2017. In May 2018, lung metastatic lesions were detected, and the patient underwent 4 cycles of oxaliplatin+leucovorin+5-fluorouracil (FOLFOX) chemotherapy. However, the disease progressed in August 2018, leading to the administration of arsenic trioxide treatment. Despite this, further progression was observed in October 2018, prompting the patient’s enrollment in a clinical trial for tislelizumab therapy. Initially, the patient achieved a partial response (PR) to tislelizumab, which was followed by a CR that lasted for almost 4 years. Unfortunately, tislelizumab treatment had to be discontinued due to immune-related adverse events (AE). Subsequently, the patient received lenvatinib and maintained a CR until July 2023. Tislelizumab monotherapy, when used as a third-line treatment, has demonstrated remarkable efficacy in facilitating patients with advanced HCC to attain a durable CR.
Introduction
Hepatocellular carcinoma (HCC) is a highly aggressive and life-threatening liver cancer.Citation1,Citation2 Globally, the age-standardized annual mortality rate of HCC is 12.9 per 100,000 in men and 4.8 per 100,000 in women.Citation3 In China, the incidence of HCC is particularly high due to the prevalence of hepatitis B and C infections, with age-adjusted incidence rates of 26.7 per 100,000 men and 8.9 per 100,000 women.Citation4 Surgical resection, the primary treatment option for HCC, is only feasible for approximately 50% of patients at the time of initial diagnosis. Even after resection, the rates of recurrence and metastasis remain high.Citation1,Citation2,Citation5 The recurrence rate after curative resection or ablation is reported to exceed 70% within 5 years, even in patients who are considered highly likely to be cured.Citation6 The risk of HCC recurrence exhibits a bimodal distribution, with the highest recurrence rate occurring within 1–2 years after resection or ablation.Citation7–9 Early recurrence is often attributed to occult micro-metastasis of the primary tumor, driven by the invasive characteristics of the primary tumor (including tumor size, multiplicity, vascular invasion, high histological grade, and elevated serum alpha-fetoprotein [AFP] levels, etc.), and early recurrence of HCC is commonly considered to be more invasive and associated with poorer long-term clinical outcomes.Citation9–11
In recent years, significant advancements in systemic therapies for recurrent or metastatic advanced HCC have emerged. According to the latest National Comprehensive Cancer Network (NCCN) guidelines, first-line treatments now include the combination of atezolizumab and bevacizumab, or tyrosine kinase inhibitors (TKIs) such as sorafenib and lenvatinib.Citation12 Furthermore, major research efforts have been done in the postoperative setting for patients with curative intent. The IMbrave050 study showed that, in patients with high-risk surgically resected or ablated HCC, adjuvant atezolizumab plus bevacizumab was associated with significantly improved recurrence-free survival, which was considered as a standard of care.Citation13,Citation14 However, the optimal second-line treatment for advanced liver cancer is unclear, especially for patients who have progressed on first-line treatments targeting anti-angiogenesis or immunotherapy. A retrospective real-world study showed that for HCC patients progressed after first-line treatment with atezolizumab and bevacizumab, the most effective second-line systematic therapy was lenvatinib.Citation15 In addition, for patients who are not candidates to receive TKIs or antiangiogenic treatments due to contraindications or financial constraints, chemotherapy regimens such as oxaliplatin+leucovorin+5-fluorouracil (FOLFOX) are also a first-line treatment option for advanced HCC.Citation16 However, the available treatment choices are further restricted after the failure of first-line chemotherapy, and there is no agreed standard for subsequent treatment.
Tislelizumab, a humanized anti-PD-1 monoclonal IgG4 antibody, has shown effectiveness in treating patients with HCC. The RATIONALE-208 trial investigated the efficacy and safety of single-agent tislelizumab as a treatment for advanced HCC following ≥1 prior systemic treatment.Citation17 In the most recent RATIONALE-301 study, patients with unresectable HCC were randomly assigned to receive tislelizumab or sorafenib tosylate as the first-line treatment, and the results showed that the median duration of response was 36.1 months for tislelizumab, similar to durvalumab in the study of HIMALAYA.Citation18,Citation19 To date, similar to other immunotherapies,Citation20–22 only a subset of patients benefits from tislelizumab monotherapy. In this case, we present the successful treatment of a patient with HCC who developed lung metastatic lesions following surgical resection. After experiencing chemotherapy failure, the patient was administered tislelizumab, which resulted in a prolonged complete response (CR).
Case Presentation
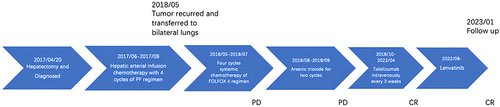
A 56-year-old Han Chinese male presented with a 37-year history of chronic hepatitis B. The patient had no family history of cancer. The patient’s body mass index was 26 kg/m², and the baseline AFP level was 33.34 IU/mL. The initial Computed Tomography (CT) scan on April 2017, revealed hepatic masses, liver cirrhosis, and splenomegaly (). Based on the diagnosis of primary HCC with Barcelona Clinic Liver Cancer stage A, Child-Pugh class A, with a serum albumin level of 42.0 g/L, total bilirubin of 26.77 μmol/L, prothrombin time of 14.4 seconds, and an international normalized ratio of 1.14, the patient underwent hepatectomy and hepatic arterial infusion pump placement in April 2017, under general anesthesia. The resected tumor measured 11×8 cm and was located in the S6 segment and partial S5 segment of the right lobe of the liver. Pathological analysis revealed the presence of microvascular invasion and micronodular cirrhosis surrounding the liver, without any satellite lesions. Immunohistochemistry staining showed that tumor cells, surrounded by CD34-positive capillaries, were positive for glypican-3 and Ki67 (LI: 75%). No reactivity was observed for hepatocytes, cytokeratin 7, or 19. Due to the high cost, the patient did not receive oral TKI therapies. Instead, he underwent hepatic arterial infusion chemotherapy (HAIC) triweekly with the cisplatin+5-fluorouracil (PF) regimen, which consisted of cisplatin 10 mg, D1-7, 5-fluorouracil (5-FU) 0.5 g, D1-7, and calcium folinate 100 mg, D1-7, for a total of four cycles from June 2017 to September 2017. Regular examinations were conducted until May 2018, when an increased level of AFP (76.60 IU/mL) and chest CT results indicated tumor recurrence and the presence of five bilateral lung metastatic lesions, with the largest lesion measuring approximately 2.5 cm (), and other metastatic lesions were shown in Figure S1A Subsequently, the patient received four cycles of systemic chemotherapy using FOLFOX regimen (oxaliplatin 150 mg, D1; 5-FU 0.7g, D1-5; calcium folinate 300 mg, D1-5) triweekly from May to July 2018. Unfortunately, the AFP level continued to increase (210.30 IU/mL), and the imaging findings indicated rapid progression of pulmonary metastasis, indicating disease progression. From August to September 2018, the patient underwent two cycles of arsenic trioxide (arsenic trioxide 15 mg D1-7; 5-FU 0.75g, D1-7) treatment triweekly. However, re-examination in October 2018 revealed further growth of lung lesions and the appearance of new lesions, with the largest measuring 5.4×3.2 cm (), and other lung lesions were shown in Figure S1B. The AFP level continued to rise to 667.4 IU/mL (), accompanied by an increased level of total bilirubin (TBIL) of 14.2 µmol/L. Despite receiving three different chemotherapy regimens, the disease rapidly progressed.
Figure 1 (A) The huge lump on the right lobe of the liver was surgically removed in April 2017. (B) The postoperative follow-up (May 2018) showed tumor recurrence in the lungs. (C) At the end of the last arsenic trioxide chemotherapy and before the use of tislelizumab (October 2018). (D) The efficacy was first evaluated as a partial response after 2 cycles of treatment with tislelizumab (January 2019). (E) The efficacy was first evaluated as a complete response after 12 cycles of treatment with tislelizumab (July 2019). (F) The patient still had a complete response at the latest follow-up (July 2023). The red arrow in indicates the location of the primary tumor. Arrows in indicate the location of recurrent tumors in the lungs.
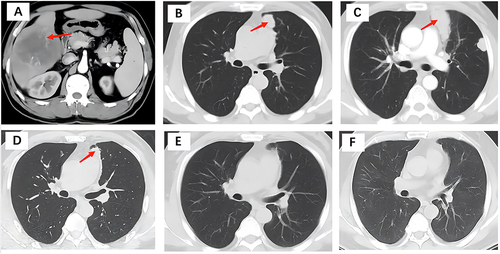
Figure 2 Evolution in time of the albumin-bilirubin (ALBI) score and neutrophil-to-lymphocyte ratio (NLR) (A), α-fetoprotein (AFP) levels (B), aspartate aminotransferase (AST), creatinine (CR), and alanine aminotransferase (ALT) (C), direct bilirubin (DBIL), indirect bilirubin (IDBIL), and total bilirubin (TBIL) (D).
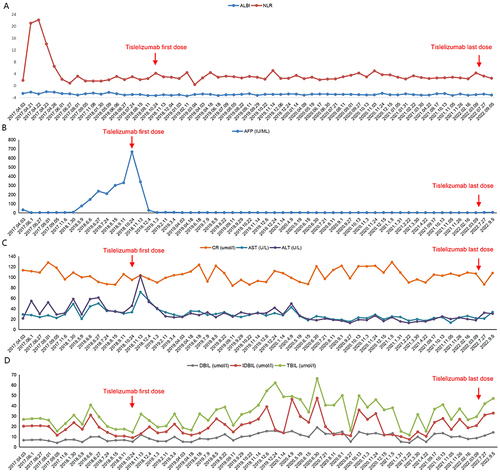
In the absence of significant contraindications, the patient was enrolled in a multicenter, open-label, Phase 2 clinical trial of BGB-A317-208 for the treatment of advanced unresectable HCC. Starting from October 2018, the patient received intravenous administration of tislelizumab 200 mg every 3 weeks. Evaluations were conducted every two cycles using a modified response evaluation criteria for solid tumors. Following the first cycle of treatment, the AFP level decreased to 340.20 IU/mL (), and the level of TBIL was 19.2 µmol/L. After two cycles of therapy, the CT images showed a partial response (PR) in the pulmonary lesions ( and S1C). Three cycles later, the AFP level normalized, and the level of TBIL was 19.3 µmol/L. In July 2019, after 12 cycles of treatment, the patient achieved a CR ( and S1D), with a neutrophil to lymphocyte ratio (NLR) of 2.83 () and TBIL of 25.9 µmol/L. Tislelizumab monotherapy was continued as maintenance treatment until April 2022 for a total of 54 cycles. It should be noted that tislelizumab was suspended from January 2020 to April 2020 due to the COVID-19 pandemic in Hubei. In addition, in September 2021, a retrospective analysis of PD-L1 immunostaining scoring was performed using the tumor tissue specimen collected from hepatectomy in April 2017. The results showed that the tumor proportion score (TPS), which considers the percentage of tumor cells expressing PD-L1, was 0%, and the combined positive score (CPS), which considers the expression of PD-L1 in both tumor and inflammatory cells, was 5.Citation23 During the discontinuation of tislelizumab, the AFP level remained normal, as did the CT examinations.
The patient was readmitted in April 2022 for complaints of shortness of breath and chest pain after exercise, which occurred half a month after the last dose of tislelizumab. The chest CT revealed multiple patchy shadows bilaterally in the lungs, and the TBIL level was elevated to 27.28 µmol/L. Bacterial infection was ruled out through bronchoalveolar lavage, and immediate treatment with methylprednisolone 160 mg (4.27 mg/kg) twice daily in combination with cefoperazone/sulbactam 2 g twice daily was initiated. After ten days of therapy, by May 2022, the respiratory symptoms were significantly relieved, and the patchy shadows on the chest CT were greatly reduced. The increased TBIL level and pneumonia were considered treatment-related adverse events (TRAEs), graded as 1 and 3, respectively. Due to concerns about serious immune-related adverse events (AEs), the tislelizumab immunotherapy was discontinued. From May to August 2022, the patient did not receive any anti-tumor treatment. As a precaution against disease recurrence, the patient was subsequently prescribed oral lenvatinib in September 2022. In the latest re-examination conducted in July 2023, the patient remained in a continuous CR state () and achieved an overall survival (OS) exceeding 6 years. In addition, the patient’s albumin-bilirubin (ALBI) score was 1–2 throughout the anti-tumor treatment (), and his hepatitis B status was under control with regular antiviral therapy. The timeline is shown in .
Figure 3 The timeline of patients treated.
During the patient’s treatment with tislelizumab, the average level of TBIL increased to 30.50 µmol/L from the average level of 22.99 µmol/L observed at relapse prior to tislelizumab therapy (). When the immunotherapy was temporarily halted, the level of TBIL decreased below 30 µmol/L after intravenous administration of prednisone at a dosage of 30 mg (0.4 mg/kg). The levels of alanine aminotransferase (ALT), aspartic transaminase (AST), and bilirubin showed a mild to moderate increase after the first cycle of immunotherapy (), but quickly recovered with the administration of glutathione. The highest peak of TBIL level was observed approximately two years later in June 2020, reaching 62.17 µmol/L. Meanwhile, the urinary creatinine level was increased to 112 µmol/L, and the uric acid level was elevated to 459 μmol/L. The levels of creatine kinase (CK) and creatine kinase isoenzymes (CK-MB) were 285 IU/L and 25.80 IU/L, respectively.
The electrocardiogram showed a slight downward shift in the ST-T segment (II, III, and aVF), and vertically lowered T waves (II, aVF, V5, and V6). However, the patient did not experience any significant discomfort such as palpitation or chest tightness. The bilirubin level, kidney function, and myocardial enzyme levels returned to normal after three days of intravenous prednisone administration at a dosage of 30 mg.
Discussion
The key finding in this case is that tislelizumab demonstrated the ability to induce durable CR in the patient with advanced HCC as a later-line treatment after failure of multiple lines of chemotherapy. The patient in this case experienced lung metastasis after initial surgery and HAIC. The short-time presence of a significantly increased AFP level of 667.4 IU/mL confirmed the lung lesions as extrahepatic metastasis of HCC. Despite receiving two lines of chemotherapy, the lung metastasis continued to progress. However, once the patient initiated third-line treatment with tislelizumab monotherapy, the lung metastasis started to regress and eventually resulted in a CR after nine months of treatment. The patient remained in CR for 4 years, even after a temporary suspension of tislelizumab due to the COVID-19 pandemic. This case highlights the potential of immunotherapy as a viable option for advanced HCC patients who have not responded to multiple lines of chemotherapy.
The NCCN guidelines recommend the use of antiangiogenic therapy in combination with immunotherapy or TKI monotherapy, such as sorafenib or lenvatinib, as first-line systemic treatments for unresectable HCC.Citation12 However, the efficacy of anti-PD1 monotherapy as a first-line treatment for HCC is still a topic of debate. Several studies suggested limited benefit of PD-1 inhibitor monotherapy as first-line therapy, nevertheless, pembrolizumab was listed as an option with a category of 2B recommendation.Citation24,Citation25 The efficacy of PD-1 inhibitor monotherapy as front or later-line treatment has been explored. In the phase 2 KEYNOTE-224 trial, 18 patients who were naïve to systemic therapy achieved an objective response rate (ORR) of 17% with pembrolizumab, but only one patient achieved a CR after previous treatment with first-line sorafenib.Citation26 In the updated 2.5-year follow-up data of KEYNOTE-224, the ORR evaluated by an independent central review was 18.3% with four CRs, but all patients who achieved CR subsequently experienced disease progression during the follow-up period.Citation27 The Phase 3 KEYNOTE-240 trial demonstrated a median OS of 13.9 months (95% CI, 11.6 to 16.0 months) and a median progression-free survival (PFS) of 3 months (95% CI, 2.8 to 4.1 months) with pembrolizumab plus best supportive care (BSC).Citation28 The best overall response included six CRs (2.2%).Citation28 However, the difference in OS and PFS did not reach the expected statistical significance, and the later follow-up data for patients who achieved CR have not been updated. Analysis of Asian patients in the KEYNOTE-240 trial showed a trend of greater benefit in the Asian subgroup, with a median OS of approximately 13.8 months in the pembrolizumab group compared to 8.3 months in the placebo group, when compared to the overall cohort.Citation29 The phase 3 KEYNOTE-394 trial further demonstrated that pembrolizumab as a second-line therapy significantly prolonged the OS and PFS in Asian patients, including those who had received prior first-line treatment of oxaliplatin-based chemotherapy, which is not an approved standard first-line treatment. The interim analysis showed six CRs, and the final analysis showed nine CRs, but it was not reported whether these patients with CRs experienced disease progression or not.Citation30
Based on the therapies mentioned earlier, it is evident that achieving a CR with currently available monotherapy is challenging, regardless of whether it is used as a first-line or second-line treatment. However, the RATIONALE-208 trial investigated the efficacy and safety of tislelizumab as a third-line PD-1 inhibitor monotherapy in patients who had received multiple lines of previous treatments.Citation17 In the trial, a total of 111 patients were included, with 102 patients having received more than two lines of previous treatments and 9 patients having received more than three lines of previous treatments.Citation17 Among these patients, one patient achieved a CR and did not experience disease progression during the follow-up period.Citation17 This finding suggests that tislelizumab, as a later-line therapy, has the potential to induce a durable CR in patients with advanced HCC who have not responded to multiple lines of previous treatments. The patient in this case achieved CR with third-line tislelizumab therapy after both oxaliplatin-based chemotherapy and arsenic trioxide combined with 5-FU failed. The duration of response was extended, lasting for more than 48 months, with the OS exceeding six years. However, it is important to note that this response was observed in only one patient and the patient presented a TPS of 0%, and a CPS of 5, while microsatellite instability (MSI) status and tumor mutational burden (TMB) were not performed due to limitations in available resources and the retrospective nature of data collection. Further research and larger studies are needed to validate these findings and assess the overall efficacy and safety of tislelizumab in patients with HCC.
As an immunotherapy, tislelizumab inhibits tumor cells by restarting the body’s immune system and enhancing the anti-tumor effects of T cells. Currently, there are no definitive biomarkers that can predict the therapeutic efficacy of immune checkpoint inhibitors (ICIs) in patients with HCC.Citation31 KEYNOTE-224 study, a phase 2 trial evaluating the efficacy and safety of pembrolizumab in patients with advanced HCC, suggested that, compared with TPS, CPS was associated with response to ICIs in a subset of patients.Citation26 Therefore, despite a TPS of 0%, the patient may present good response to tislelizumab for the relatively high CPS. In our case, the patient’s NLR continued to decrease and fluctuated between 2 and 4 after starting tislelizumab treatment. The NLR is an inflammatory marker that has been investigated as a significant independent prognostic indicator in post-therapeutic recurrence and survival of patients with HCC.Citation32–34 Among HCC patients, NLR levels closest to the last visit/death were significantly higher compared to baseline.Citation32 In addition, the ALBI grade has emerged as an alternative, reproducible and objective measure of liver functional reserve in patients with HCC, defining worsening liver impairment across 3 grades (I to III). Previous studies have shown that ALBI grade also predicts survival in patients treated with transarterial chemoembolization and immune checkpoint inhibitor therapy.Citation35 In our case, the patient’s ALBI score remained at 1–2 throughout the tislelizumab monotherapy. The present patient benefiting from long-term therapy may be associated with a relatively high CPS, a lower proportion of NLR and a better ALBI score.
In addition, the notable and sustained effectiveness of tislelizumab monotherapy in this case may be linked to several mechanisms. Firstly, a majority of HCC patients do not benefit from ICIs due to the “cold” tumor characteristic, which is the lack of T-lymphocyte infiltration.Citation36,Citation37 Low dose of 5-FU may deplete myeloid derived suppressor cells (MDSCs) to enhance T-cell infiltration and turn the tumor “hot”, improving the efficacy of checkpoint blockage therapy in a murine Lewis Lung Carcinoma model.Citation38 Secondly, the exploration of mechanism in preclinical and clinical studies showed that platinum-based chemotherapy may harness the positive immunomodulatory effects to enhance the sensitivity of tumor cells to checkpoint blockage therapy.Citation39 Collectively, these factors underscore the need for further research to fully understand and exploit the mechanisms that enhance the effectiveness of immunotherapy in HCC treatment. Furthermore, it should be noted that although the patient did not directly receive the combination therapy of immunotherapy with chemotherapy, prior chemotherapy may have altered the tumor microenvironment, allowing the ICIs to exert a sustained effect.
The potential relationship between treatment effectiveness and AE is an important consideration. Previous studies have demonstrated that immune-related AE can be indicative of drug efficacy.Citation40–42 In this case, the patient experienced persistent elevation of bilirubin levels and AST/ALT during and after treatment. These AE were of grades 1–2 and were effectively managed with corticosteroids. Immune-related hepatitis associated with ICIs often presents with elevated levels of ALT, AST, and bilirubin.Citation41,Citation42 Interestingly, ALT and AST elevations are more commonly observed than bilirubin elevation.Citation43 Histopathological evaluation revealed hepatic lobular injury and bile duct injury, with the latter being less common.Citation44 In this study, the patient consistently showed elevated bilirubin levels but normal ALT and AST. It is possible that the immune-related hepatitis in this case was primarily characterized by bile duct injuries, leading to a distinct manifestation of immune-related hepatitis. This suggests that the occurrence of immune-related AE during immunotherapy may serve as a predictor of its promising effectiveness.
In February 2022, the patient developed a lung lesion, which was suspected to be either lung metastasis or an immune-related AE. Continuing with another cycle of immunotherapy one month later, the condition worsened, leading to the decision to terminate immunotherapy due to consideration of immune-related lung AE. This raises the question of when to discontinue treatment in patients experiencing sustained remission after long-term immunotherapy. In cases of suspected ICI-related lung AE, it is important to consider that the symptoms can be atypical and may present relatively late.Citation45 Therefore, once lung AE are suspected as a result of immunotherapy, it is recommended to promptly discontinue the ICI treatment.Citation46 The termination of 3.5 years of immunotherapy in this patient highlights the need for vigilance and timely intervention when managing potential immune-related AE. Prompt recognition and appropriate management of such AE are crucial to minimize their impact and ensure patient safety during immunotherapy.
In this case, even after discontinuing immunotherapy for six months, the patient maintained CR with subsequent lenvatinib therapy. This could potentially be attributed to the long tail effect of immunotherapy, indicating that a sequential treatment regimen of PD-1 inhibitors followed by TKIs may be an alternative approach for advanced HCC.
However, there were certain limitations in the management of this case that need to be addressed in the future. Histopathological biomarker changes like MSI-H status and TMB were not obtained at crucial time points, such as at the time of disease progression or response, due to the practical challenges of repeated biopsies in clinical practice. Obtaining such information could provide valuable insights into the underlying mechanisms at the tumor level and guide future management strategies for patients with HCC.
Conclusion
This case report delineates an instance of prolonged CR with tislelizumab monotherapy as a third-line treatment in advanced HCC with relatively high CPS, despite prior failures of multiple therapeutic lines. The sustained response observed in our case underscores the potential benefit of utilizing tislelizumab after chemotherapy in specific patients with relatively high CPS and favorable liver function reserve. While our findings support the inclusion of PD-1 inhibitors in sequential treatment regimens, they also highlight the imperative for more comprehensive biomarker profiling in future studies. This will enhance our understanding of patient subsets most likely to benefit from such strategies, ultimately guiding the adoption of more personalized therapeutic approaches in HCC management. However, considering the challenges of repeated biopsies in clinical practice, how to select optimal treatment based on biomarkers still needs to be explored.
Ethics Approval and Consent to Participate
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). This study was a case report, ethical approval was approved by Hubei Cancer Hospital ethics committee (NO. 2018[5]). Written informed consent was obtained from the patient. A copy of the written consent is available for review by the editorial office of this journal.
Consent for Publication
The patient provided consent for the publication of the case.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
Acknowledgments
The authors acknowledge the contribution of patient.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon a reasonable request.
Additional information
Funding
References
- Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular Carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology. 2018;68:723–750. doi:10.1002/hep.29913
- Vogel A, Cervantes A, Chau I, et al. Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29:iv238–iv255.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi:10.3322/caac.21660
- Zheng R, Qu C, Zhang S, et al. Liver cancer incidence and mortality in China: temporal trends and projections to 2030. Chin J Cancer Res. 2018;30:571–579. doi:10.21147/j.issn.1000-9604.2018.06.01
- Villanueva A, Longo DL. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450–1462. doi:10.1056/NEJMra1713263
- Li L, Zhang J, Liu X, et al. Clinical outcomes of radiofrequency ablation and surgical resection for small hepatocellular carcinoma: a meta-analysis. J Gastroenterol Hepatol. 2012;27:51–58. doi:10.1111/j.1440-1746.2011.06947.x
- Tsilimigras DI, Bagante F, Moris D, et al. recurrence patterns and outcomes after resection of hepatocellular Carcinoma within and beyond the Barcelona clinic liver cancer criteria. Ann Surg Oncol. 2020;27:2321–2331. doi:10.1245/s10434-020-08452-3
- Zhou Y, Ding J, Qin Z, et al. Predicting the survival rate of patients with hepatocellular carcinoma after thermal ablation by nomograms. Ann Transl Med. 2020;8:1159. doi:10.21037/atm-20-6116
- Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38(2):200–207. doi:10.1016/S0168-8278(02)00360-4
- Chan AWH, Zhong J, Berhane S, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol. 2018;69:1284–1293. doi:10.1016/j.jhep.2018.08.027
- Yao LQ, Chen ZL, Feng ZH, et al. Clinical features of recurrence after hepatic resection for early-stage hepatocellular carcinoma and long-term survival outcomes of patients with recurrence: A multi-institutional Analysis. Ann Surg Oncol. 2022.
- NCCN clinical practice guidelines in oncology (NCCN guidelines). Hepatob Canc Vers. 2023.
- Qin S, Chen M, Cheng AL, et al. Atezolizumab plus bevacizumab versus active surveillance in patients with resected or ablated high-risk hepatocellular carcinoma (IMbrave050): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2023;402:1835–1847. doi:10.1016/S0140-6736(23)01796-8
- Ntellas P, Chau I. Updates on systemic therapy for hepatocellular carcinoma. Am Soc Clin Oncol Educ Book. 2024;44:e430028.
- Persano M, Rimini M, Tada T, et al. Sequential therapies after atezolizumab plus bevacizumab or lenvatinib first-line treatments in hepatocellular carcinoma patients. Eur J Cancer. 2023;192:113264. doi:10.1016/j.ejca.2023.113264
- General Office of National Health Commission. Guidelines for diagnosis and treatment of primary liver cancer (2022 edition). J Clin Hepatol. 2022;38:288–303.
- Ren Z, Ducreux M, Abou-Alfa GK, et al. Tislelizumab in patients with previously treated advanced hepatocellular Carcinoma (RATIONALE-208): a Multicenter, Non-Randomized, Open-Label, Phase 2 Trial. Liver Cancer. 2023;12:72–84. doi:10.1159/000527175
- Qin S, Kudo M, Meyer T, et al. Tislelizumab vs Sorafenib as First-Line Treatment for Unresectable Hepatocellular Carcinoma: a Phase 3 Randomized Clinical Trial. JAMA Oncol. 2023;9:1651–1659. doi:10.1001/jamaoncol.2023.4003
- Patel TH, Brewer JR, Fan J, et al. FDA approval summary: Tremelimumab in combination with durvalumab for the treatment of patients with unresectable hepatocellular carcinoma. Clin Cancer Res. 2024;30:269–273. doi:10.1158/1078-0432.CCR-23-2124
- Santoni M, Rizzo A, Mollica V, et al. The impact of gender on The efficacy of immune checkpoint inhibitors in cancer patients: The MOUSEION-01 study. Crit Rev Oncol Hematol. 2022;170:103596. doi:10.1016/j.critrevonc.2022.103596
- Rizzo A, Brandi G. Biochemical predictors of response to immune checkpoint inhibitors in unresectable hepatocellular carcinoma. Cancer Treat Res Commun. 2021;27:100328. doi:10.1016/j.ctarc.2021.100328
- Mollica V, Rizzo A, Marchetti A, et al. The impact of ECOG performance status on efficacy of immunotherapy and immune-based combinations in cancer patients: the MOUSEION-06 study. Clin Exp Med. 2023;23:5039–5049. doi:10.1007/s10238-023-01159-1
- De Marchi P, Leal LF, da Silva V D, et al. PD-L1 expression by tumor proportion score (TPS) and combined positive score (CPS) are similar in non-small cell lung cancer (NSCLC). J Clin Pathol. 2021;74:735–740. doi:10.1136/jclinpath-2020-206832
- Qin S, Kudo M, Meyer T, et al. LBA36 Final analysis of RATIONALE-301: Randomized, Phase III study of tislelizumab versus sorafenib as first-line treatment for unresectable hepatocellular carcinoma. Ann Oncol. 2022;33:S1402–S1403.
- Yau T, Park JW, Finn RS, et al. LBA38_PR - CheckMate 459: a randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann Oncol. 2019;30:v874–v875. doi:10.1093/annonc/mdz394.029
- Zhu AX, Finn RS, Edeline J, et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952. doi:10.1016/S1470-2045(18)30351-6
- Kudo M, Finn RS, Edeline J, et al. Updated efficacy and safety of KEYNOTE-224: a Phase II study of pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. Eur J Cancer. 2022;167:1–12. doi:10.1016/j.ejca.2022.02.009
- Finn RS, Ryoo BY, Merle P, et al. pembrolizumab as second-line therapy in patients with advanced hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J Clin Oncol. 2020;38:193–202. doi:10.1200/JCO.19.01307
- Kudo M, Lim HY, Cheng AL, et al. Pembrolizumab as second-line therapy for advanced hepatocellular carcinoma: a subgroup analysis of Asian patients in the phase 3 KEYNOTE-240 Trial. Liver Cancer. 2021;10:275–284. doi:10.1159/000515553
- Qin S, Chen Z, Fang W, et al. Pembrolizumab versus placebo as second-line therapy in patients from Asia with advanced hepatocellular Carcinoma: A randomized, Double-Blind, Phase III Trial. J Clin Oncol. 2023;41(7):1434–1443. doi:10.1200/JCO.22.00620
- Ponvilawan B, Roth MT. Sequencing Systemic Therapy in Hepatocellular Carcinoma. Curr Treat Options Oncol. 2023;24:1580–1597. doi:10.1007/s11864-023-01135-7
- Johnson PJ, Dhanaraj S, Berhane S, Bonnett L, Ma YT. The prognostic and diagnostic significance of the neutrophil-to-lymphocyte ratio in hepatocellular carcinoma: a prospective controlled study. Br J Cancer. 2021;125:714–716. doi:10.1038/s41416-021-01445-3
- Gibellini L, Borella R, Santacroce E, et al. Circulating and tumor-associated neutrophils in the era of immune checkpoint inhibitors: Dynamics, phenotypes, metabolism, and functions. Cancers (Basel). 2023;15:3327. doi:10.3390/cancers15133327
- Mouchli M, Reddy S, Gerrard M, Boardman L, Rubio M. Usefulness of neutrophil-to-lymphocyte ratio (NLR) as a prognostic predictor after treatment of hepatocellular carcinoma”. Rev Arti Ann Hepa. 2021;22:100249. doi:10.1016/j.aohep.2020.08.067
- Demirtas CO, D’Alessio A, Rimassa L, Sharma R, Pinato DJ. ALBI grade: Evidence for an improved model for liver functional estimation in patients with hepatocellular carcinoma. JHEP Rep. 2021;3:100347. doi:10.1016/j.jhepr.2021.100347
- Yu J, Li M, Ren B, et al. Unleashing the efficacy of immune checkpoint inhibitors for advanced hepatocellular carcinoma: factors, strategies, and ongoing trials. Front Pharmacol. 2023;14:1261575. doi:10.3389/fphar.2023.1261575
- Donne R, Lujambio A. The liver cancer immune microenvironment: therapeutic implications for hepatocellular carcinoma. Hepatology. 2023;77:1773–1796. doi:10.1002/hep.32740
- Mathew AA, Zakkariya ZT, Ashokan A, et al. 5-FU mediated depletion of myeloid suppressor cells enhances T-cell infiltration and anti-tumor response in immunotherapy-resistant lung tumor. Int Immunopharmacol. 2023;120:110129. doi:10.1016/j.intimp.2023.110129
- Xue Y, Gao S, Gou J, et al. Platinum-based chemotherapy in combination with PD-1/PD-L1 inhibitors: preclinical and clinical studies and mechanism of action. Expert Opin Drug Deliv. 2021;18:187–203. doi:10.1080/17425247.2021.1825376
- Espana S, Perez Montes de Oca A, Marques-Pamies M, et al. Endocrine adverse events related to immune-oncology agents: retrospective experience of a single institution. Transl Lung Cancer Res. 2020;9:103–110. doi:10.21037/tlcr.2019.12.17
- Wang D, Chen C, Gu Y, et al. Immune-Related Adverse Events Predict the Efficacy of Immune Checkpoint Inhibitors in Lung Cancer Patients: a Meta-Analysis. Front Oncol. 2021;11:631949. doi:10.3389/fonc.2021.631949
- Das S, Johnson DB. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. J Immunother Cancer. 2019;7:306. doi:10.1186/s40425-019-0805-8
- Chan SL, Yip TC, Wong VW, et al. Pattern and impact of hepatic adverse events encountered during immune checkpoint inhibitors - A territory-wide cohort study. Cancer Med. 2020;9:7052–7061. doi:10.1002/cam4.3378
- Zen Y, Yeh MM. Checkpoint inhibitor-induced liver injury: a novel form of liver disease emerging in the era of cancer immunotherapy. Semin Diagn Pathol. 2019;36:434–440. doi:10.1053/j.semdp.2019.07.009
- Fessas P, Possamai LA, Clark J, et al. Immunotoxicity from checkpoint inhibitor therapy: clinical features and underlying mechanisms. Immunology. 2020;159:167–177. doi:10.1111/imm.13141
- Gutierrez C, McEvoy C, Munshi L, et al. Critical care management of toxicities associated with targeted agents and immunotherapies for cancer. Crit Care Med. 2020;48:10–21. doi:10.1097/CCM.0000000000004087
