Abstract
Purpose
Hispanics, the largest minority in America, have increased risk of several medical issues and face noteworthy health disparities. This study compares care-seeking behaviors and choice experience among Hispanics, Asians, Blacks, and Whites, considering SES (income, education, and insurance status) and across five healthcare provider (HCP) types. Concurrent analysis provides a comprehensive view of how and where inequity manifests in healthcare.
Methods
A cross-sectional online survey assessed 1485 adults (Hispanic=314, Asian=313, Black=316, White=542, recruited through a panel agency) of the frequency of visiting primary care providers, dentists, optometrists, gynecologists, and specialists for chronic conditions. Participants also rated the importance of self-selecting a HCP and difficulty in finding one.
Results
Whites visited each HCP most regularly. Compared to Asians, more Hispanics saw specialists regularly (45.1% vs 56.5%, p=0.042), and Blacks saw dentists less (47.0% vs 38.3%, p=0.028) and gynecologists more often (21.2% vs 33.1%, p=0.024). No other frequency differences were observed among minorities. Low-income participants across four races saw dentists and gynecologists with comparable infrequency. Hispanics and Asians assigned similarly significantly lower self-choice importance and experienced more difficulty relative to Whites or Blacks. Participants with lower income or education visited HCPs less regularly yet perceived the same choice importance as higher-SES peers (p>0.05). Notably, discrepancies in visit frequency between Whites and minorities were more pronounced in higher-SES than lower-SES group. Differences in experiencing care-seeking difficulty were associated with income (p=0.029) and insurance type (p=0.009) but not education (p>0.05).
Conclusion
Higher income and education increase healthcare utilization; however, racial disparities persist, particularly among higher-SES groups. Despite similarities among minorities, the extent of disparities varied by SES and provider type. The findings help explain evident inequity in healthcare access and health outcomes. Tailored patient education, culturally-specific navigation support, and more inclusive services are needed to address barriers faced by minorities and disadvantaged populations.
Introduction
Diversity is a signature of the US; health disparities across race/ethnicity and socioeconomic status (SES) have continued to draw attention, yet improvements are uneven. Hispanics constitute a rapidly growing population in America, comprising over 62.1 million individuals (19.1%) with different backgrounds and lived experiences.Citation1 Compared to other populations, they are at higher risk of several health issues, such as undiagnosed hypertensionCitation2 (33% vs 26.5% of Whites),Citation3 age-related eye diseases (eg, glaucoma, cataract),Citation4 and obesity (44.8% vs 17.4% of Asians).Citation5 Hispanics are also more likely to be uninsured (18.8% vs 10% in Black and 6.6% in White);Citation6 one in five reported experiencing discrimination in the healthcare system, and 17% avoided seeking care due to fear of prejudice.Citation7 These gaps have not been addressed adequately, resulting in inequities in receiving care and health outcomes.Citation8
Research on health disparities often cites healthcare access as the central issue.Citation9,Citation10 In addition to availability and affordability,Citation11 access also includes individuals’ decisions regarding service utilization.Citation12 Comparing healthcare usage preferences and perceptions among groups can illustrate health behavior or experience differences that may contribute to existing inequities. Extensive research has documented the process of selecting a primary care provider (PCP), with patients often prioritizing provider qualification and years of experience,Citation13 logistical factors (eg, location, wait time),Citation14,Citation15 and cost or insurance coverage.Citation16,Citation17 US patients visit specialists less frequently than PCPs,Citation18 citing higher costs,Citation19 appointment delays,Citation20 negative perceptions about specific specialties (eg, mental health),Citation21 or PCPs serving as gatekeepers.Citation22 Race/ethnicity has also been reported as a prominent factor in the frequency of visiting healthcare providers (HCP) with minorities having lower rates in comparison to Whites, even when accounting for barriers in care accessibility.Citation23 Hispanics expressed that care-seeking can be impeded by experienced or anticipated discrimination,Citation24 limited English proficiency or health literacy,Citation25–27 cultural barriers (eg, stigma surrounding certain medical conditions),Citation28,Citation29 SES,Citation30 immigration status,Citation31 or a low rate (9%) of Hispanic HCPs.Citation32 Moreover, PCP shortage is more prevalent in zip codes with higher ratio of African Americans,Citation33 which indicates less procedure referrals,Citation34 continuity of care,Citation35 and quality of care.Citation36 The Social Determinants of Health theory helps explain why societal and economic factors (including where one lives) influence an individual’s health outcomes far more than their genetic makeup.Citation37,Citation38 These barriers impact the health status of minorities and disadvantaged populations. For example, lower health literacy has been associated with decreased symptom reporting,Citation39 living in poverty,Citation40 lack of insurance,Citation40 and lower quality of care.Citation41 In addition, individuals’ perceived dynamics or challenges in interacting with their HCP may determine their health behaviors. According to the Theory of Reasoned Action, an individual’s attitudes and beliefs influence their intentions to engage in a particular behavior.Citation42 Studies have cited how cultural beliefs such as religion, spiritual disposition, and centrality of family impact Hispanics’ health-related behaviors and decision-making such as end-of-life care.Citation43,Citation44 The custom of relying on complementary and alternative medicine may also contribute to misunderstandings that impact care provided by Western HCPs.Citation45–47
When examining health behavior and inequities, most studies investigated one or two ethnic minority groups or compared to Whites.Citation48–50 Considering the complex factors relating to Hispanics’ preferences, barriers, and choices in healthcare that may affect health outcomes, there remains a gap in the literature assessing minorities’ healthcare-seeking behavior comparing multiple racial/ethnic groups and concurrently with SES. Disparity likely starts from the beginning of the patient journey; better understanding of initial choices could inform interventions to improve experience and foster equity.
Terms such as Hispanic, Latino, and Latinx have been used to describe populations that speak Spanish/Portuguese or have heritage in Latin America. In this study, Hispanic refers inclusively to US residents who have origins in a Spanish-speaking or Latin American country and those who self-identify as Latino/Hispanic, regardless of birthplace or whether they speak Spanish. The objectives of this research were to investigate group discrepancies among Hispanics, Asians, Blacks, and Whites in the frequency of visiting PCPs and specialists (dentist, gynecologist, optometrist) as well as their perceived importance of self-selecting a HCP and difficulty in finding one. This study also examined behaviors and perceptions by income and educational levels and insurance status to discern the independent and joint influences of race/ethnicity and SES. Analyzing variations in obtaining care and decision-making experiences can provide a deeper understanding of the causes and nuances of disparities in service utilization. The findings could inform policy makers in identifying access barriers and designing culturally sensitive interventions to improve health equity.
Methods
Study Sample
Two identical online cross-sectional surveys were conducted in March and October 2023. The first fielding surveyed a nationally representative sample; setting the acceptable margin of error at 3%, a target of at least 1067 participants was determined based on the size of the American population.Citation51,Citation52 To ensure adequate number in each racial/ethnic group for meaningful statistical comparisons, the second fielding collected additional responses from the three largest minority populations: participants self-identified as Hispanic/Latinos, Asian/Asian Americans/Pacific Islander, or Black/African Americans. A US-based panel survey company assisted in survey distribution and participant recruitment; eligibility criteria included age 18 or older, US resident, and visited a HCP in the past two years. Potential respondents opted-in to receive survey announcements; if they chose to participate but did not meet the above-mentioned criteria, they were thanked and excluded from data collection.
Duke University IRB approved the study protocol (#2023-0315). Prior informed consent was obtained from each participant.
Measures
The questionnaire assessed care-seeking behaviors, decision-making preferences and experiences in healthcare, related logistical factors, and demographics. The primary outcome variables were doctor-visit frequencies: participants were asked if they regularly see a PCP, dentist, optometrist, gynecologist (non-male participants only), and medical specialist if they have a chronic condition. Two other questions queried care-seeking preference and experience: “From not at all (1) to extremely important (5), how important is it for you to have a say in choosing your own provider?” and “On a scale from very difficult (1) to very easy (5), how difficult is it for you to find a healthcare provider when you need one?”.
Responses to the five provider visits and two perception questions were compared across four groups (Hispanic, Asian, Black, and White) and three SES factors. Educational levels were categorized as low (high school/GED or less), medium (some college), and high (college degree or more); annual household income levels were grouped as low (≤ US$49,999), medium ($50,000-$99,999), and high (≥ $100,000).
Statistical Analysis
Kruskal–Wallis tests were performed to determine whether participants’ HCP visit frequencies and perception/experience were significantly associated with race or SES. Then, Mann–Whitney U-tests were run to identify which pairs of racial or income/education groups were significantly different. To further investigate whether the observed impact of race/ethnicity was due to SES, each group was divided into lower/higher income and education subgroups for additional tests. All analyses were performed using SPSS (Version 29.0.0.0).
Results
Participant Characteristics
A total of 1522 participants completed the survey. Respondents who self-identified as American Indian/Native American (n=7), mixed race/other (n=23), or “prefer not to say” (n=7) were excluded due to the small numbers; 1485 responses were retained for analysis. Each racial/ethnic group had at least 300 participants, with relatively balanced distributions on other demographics (). Among them, 1360 (91.6%) reported having a PCP, 22.3% of who did not visit regularly; 901 (60.7%) indicated having a chronic medical condition, for which 56.0% saw a specialist regularly.
Table 1 Participant Characteristics by Race/Ethnicity (N=1485)a
Disparities in the Frequency of Seeing a HCP
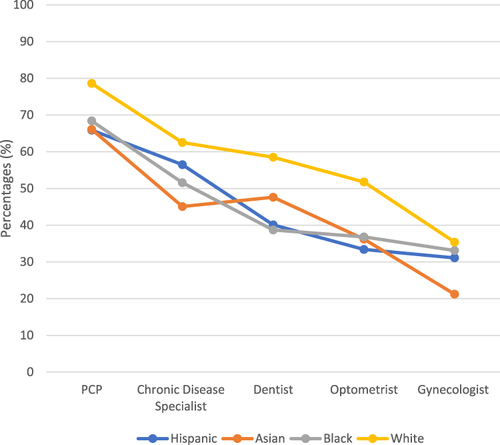
The frequencies of receiving care were significantly associated with race/ethnicity and SES. Overall, Whites had the highest percentages in regularly visiting each of the HCPs (). Analyzing pairwise across the four groups, 15 of the 30 comparisons (six pairs times five providers) were significant; 12 of those occurred between Whites and a minority (). Hispanics and Whites had similar rates of seeing a gynecologist and chronic disease specialist (p>0.05). On the other hand, there were few differences among the three minorities: Hispanics were significantly more likely than Asians to regularly visit a specialist (56.5% vs 45.1%, p=0.042) but no other differences were observed between Hispanics and another minority. Compared to Blacks, Asians had a higher percentage of regularly seeing a dentist (38.3% vs 47.0%, p=0.028) and lower for gynecologist (33.1% vs 21.2%, the lowest of all groups, p=0.024).
Table 2 Care-Seeking Frequency, Decision Preference, and Experience by Race/Ethnicity (N=1485)a
Figure 1 Ratios of Regularly Seeing HCP by Race/Ethnicity (N=1,485)a..
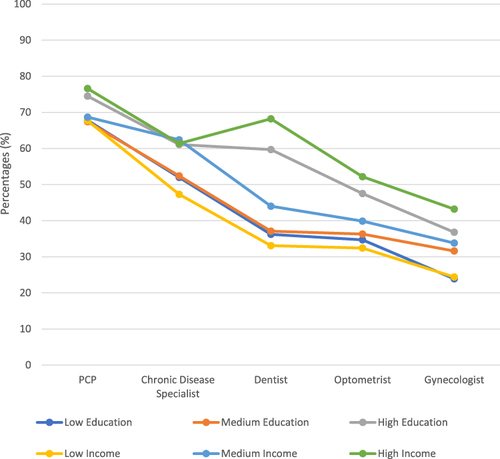
Comparing SES across three income and educational levels in visiting the five HCPs, 21 out of 30 pairwise comparisons were significant (). Groups of high-income or high-education almost consistently showed higher ratios of obtaining care from any provider compared to both low- and medium-SES groups (). The three exceptions were: for gynecologist visit, no significant difference between medium and high groups by either income or education, or between medium- and high-income groups in visiting a specialist (p>0.05). Notably, high-income participants were even more likely than high-education participants to regularly see a dentist, optometrist, and gynecologist. No differences were observed between low- and medium-education groups for all five HCPs (p>0.05). However, the low-income group was significantly less likely than medium-income group to see any HCP regularly, except for PCP.
Table 3 Care-Seeking Frequency, Decision Preference, and Experience by SES (N=1485)a
Figure 2 Ratios of Regularly Seeing HCP by SES (N=1,485)a. a Participants were asked whether they regularly see each of the five HCPs. Of the total 1,485 participants, one responded “prefer not to answer” for the education question and 40 for the income question; they were excluded from this comparison. The resulting subgroup sizes and definitions were Low-Education=361 (≤ high school), Medium-Education=401 (some college), High-Education=722 (≥ college degree), Low-Income=564 (≤ US$49,999), Medium-Income=420 (US$50,000–99,999), and High-Income=461 (≥ US$100,000), of which the reported percentages are calculated from, respectively. For chronic disease specialist: Participants who reported having a chronic disease (ns) were asked whether they regularly see a specialist for it. The subgroup sizes for this category were Low-Education (ns=225), Medium-Education (ns=246), High-Education (ns=450), Low-Income (ns=353), Medium-Income (ns=245), High-Income (ns=306). For Gynecologist: Participants who did not self-identify as male (nf) were asked whether they regularly see a gynecologist. The subgroup sizes for this category were Low-Education (nf=209), Medium-Education (nf=206), High-Education (nf=342), Low-Income (nf=336), Medium-Income (nf=204), High-Income (nf=192).
Relative to participants with public insurance, those with private insurance were more likely to regularly visit a dentist (42.9% vs 55.6%, p<0.001) and gynecologist (23.7% vs 41.3%, p<0.001). The uninsured participants reported much lower visit frequencies (up to 51.8% differences for PCP) across all five HCPs ().
Preference in Decision-Making and Experience of Care-Seeking
Significant associations were also found between race/ethnicity and each of the two care-seeking behavior questions: Q1—importance of self-selecting a HCP and Q2—difficulty in finding a HCP when needed. Across the four groups, eight of the 12 pairwise comparisons were significant; four of which were between Whites and Hispanics or Asians (lower part of ). Hispanics and Asians had no difference regarding perceived importance in choosing their HCP (μ=4.06 and 3.95 out of 5, respectively, p=0.137); both rated significantly lower than Blacks or Whites (μ=4.22 and 4.21, no difference between these two, p=0.843). Likewise, Blacks and Whites reported a significantly easier experience finding a HCP (μ=3.61 and 3.57, p=0.476) than Hispanics or Asians (μ=3.32 and 3.36, lower score denotes more difficulty, p=0.750).
The analysis by SES on perceived importance and experience revealed more commonalities across subgroups than by race/ethnicity. Examining the influences of education and income, only two of the 12 pairwise comparisons were significant: the low-income group experienced more difficulty (μ=3.37) in finding a HCP than medium- and high-income groups, respectively (μ=3.60 and 3.52, p=0.279, insignificant between the latter two groups). Further, participants at different educational levels showed no variation in either the importance or difficulty of care-seeking. Similarly, participants with public and private insurance rated the same levels of choice importance (μ=4.12 and 4.14, p=0.921 (lower part of ).
The Impacts of Race/Ethnicity by SES on Patient Behavior and Perception
To further investigate the influence of race/ethnicity considering individuals’ SES, each group was split by income (< or ≥ $50,000) and educational level (without or with a college degree) to determine whether higher attainment of earning or education could overcome the evident healthcare inequalities. For both care-seeking frequencies and preference/experience, all four SES subgroups (especially the lower-SES subgroups) showed fewer significant differences across race/ethnicity than the full sample, indicating the observed disparity was partially but not wholly attributed to SES. Moreover, as higher-SES subgroups had more regular visits to each HCP than their lower-SES peers, the behavior divergence still primarily occurred between Whites and a minority group; in particular, the higher-education subgroup showed the largest number of pairwise differences across race/ethnicity—12 out of 30 ().
Table 4 Care-Seeking Frequency, Decision Preference, and Experience Across Race/Ethnicity by SES – Pairwise Significance (N=1485)a
Among minorities, there was no significant difference in seeing a PCP, specialist, dentist, and optometrist in the lower-income, lower-education, and higher-income subgroups (with one exception where more Hispanics saw a specialist regularly than Asian (58.5% vs 42.3%, p=0.016) in lower-income participants). For gynecologist, participants within lower-income (20.2%~31.5%, p=0.212) or lower-education (24.0%~28.7%, p=0.897) subgroups had similar visit infrequencies regardless of race/ethnicity; in higher-income subgroup, only Asians had lower percentage of regular visit than Whites (21.9% vs 50.9%, p=0.004) and also was the lowest of all races/ethnicities in the higher-education subgroup (; full comparison statistics are presented in Appendix Tables 1 and Appendix Tables 2).
Regarding perceived importance of self-selecting a HCP, lower-education participants showed uniformity across race/ethnicity (3.98~4.17, p=0.09); Hispanics rated lower than Blacks in the lower-income subgroup (4.02 vs 4.22, p=0.025) and higher than Asian in the higher-education subgroup (4.16 vs 3.94, p=0.047). On care-seeking experience, lower-income/education Hispanics and Asians reported significantly greater difficulty in finding a HCP than Whites or Blacks; this disparity persisted for Asians compared to Whites in higher-income/education subgroups but no other differences were observed across other race/ethnicity ().
Discussion
This study reveals several novel insights into healthcare disparities among four racial/ethnic groups and income and educational levels across five provider types. Unlike previous research that often examined these factors in isolation, our concurrent analysis provides a comprehensive view of how race and SES independently and jointly influence healthcare-seeking behaviors and decision preferences. The detailed examination by provider type further points to specific areas—such as dental and optometric care—where interventions are needed for the respective populations. The approach allows a nuanced understanding of how and where inequity manifests across various aspects of healthcare.
While minorities account for 40% of the US population,Citation53 Whites consistently had the highest ratios of regularly seeing the five HCPs investigated (although 20% of the pairwise analyses showed a similar ratio with one other group). Few statistical variations in behavior were observed among minorities, indicating their common reservation in seeking care. Literature has documented barriers such as fear of discrimination,Citation54,Citation55 lack of or inadequate health insurance, limited access to specialty care,Citation11 language challenges,Citation56,Citation57 and lower health literacy.Citation27
At the same time, despite similarities among minorities, the extent of the disparities varies by race and provider type. Relative to Hispanics and Asians, Whites and Blacks reported similarly higher perceived importance in choosing their own doctor and easier times in finding one. Such division has not been reported in earlier research, likely because most studies compared Whites to a single or multiple grouped minorities, and Asians were more often left out in these analyses.Citation58,Citation59 The shared obstacles faced by Hispanics and Asians, as opposed to Blacks, could be attributed to the greater proportion of immigrants in these populations who are less familiar with the US healthcare system, proficient in navigating health insurance, or comfortable in choosing or interacting with American HCPs. Categorizing all racial minorities as a homogeneous and disadvantaged group overlooks distinctions in customs, lived experiences, and actions and expectations surrounding healthcare utilization. Our findings suggest the importance of culturally tailored interventions and support systems in healthcare settings.
Participants with lower income or education saw all HCPs less regularly than their more privileged counterparts. However, perceived choice importance did not vary by either SES factors; compared across race, all groups (except Asians) rated the same importance regardless of SES. Further examination showed the greater influence of income over education: the high-income subgroup had more frequent visits to dentist, optometrist, and gynecologist than high-education subgroups; and the difficulty in finding a provider was statistically associated with income and insurance type but not education. The divergence reflects the expensive, fragmented US healthcare system with individual responsibility for insurance and separate dental and eye care coverage. SES is often reported an indicator of health outcomesCitation60 and life expectancy,Citation61 associated with accessibility and quality of care.Citation10 The high rates of uninsuranceCitation62,Citation63 and lack of dental and eye care coverage among low-income individualsCitation64 hinder their care-seeking choices and perpetuate inequities. Oral, eye, and gynecological care are integral to overall health and social wellbing.Citation65 Incorporating related health education and basic checkups in PCP visits, inclusive insurance, and interprofessional collaborationCitation66 would help address these inadequacies.Citation67
Notably, though the likelihood of obtaining and receiving care increases with upward socioeconomic mobility, higher SES does not uniformly mitigate healthcare disparities between Whites and minorities; in many cases, racial disparities are more pronounced among higher-SES groups. The result challenges the conventional assumption about the protective effects of socioeconomic advancements.Citation68–70 Again, the narrowing of the gaps vary by race and provider type. PCP visit difference between Hispanics and Whites in lower-income and lower education groups were not observed in the higher-income and higher-education groups; likewise, their optometrist visit difference in the lower-income group was not found in the higher-income group. Nevertheless, for Asians, such disparity did not diminish with higher income or education for any provider type, possibly because Whites’ visit frequencies increased at a faster rate. The contrast underscores the complexity of healthcare access and utilization in the US, exposing that greater income or education attainment alone is insufficient to overcome existing racial inequities; there are hidden needs among higher-SES minorities who still face considerable barriers. Earlier studies have discussed the racialized structure of the US healthcare system disadvantaging minorities, including overt or subtle discrimination and unequal treatments.Citation7,Citation24,Citation32,Citation71 Moreover, it is concerning to observe greater racial differences in experienced difficulty in lower-SES populations and fewer differences in both behavior and perceptions among minorities regardless of SES.
These findings help explain the enduring inequities in receiving care and subsequent health outcomes with important implications for policymakers and healthcare professionals. Cultural and structural factors concerning specific groups need to be considered to design effective interventions that reduce access barriers. Tailored patient education, improved navigation support, and inclusive services that address the unique needs of disadvantaged populations and minorities (including higher-SES minority groups) could help mitigate these disparities.
Limitations and Future Research
Two of the study’s limitations were attributed to the nature of the online survey. It limited the participation to individuals with internet access and certain levels of English and digital proficiency. The results may also be influenced by self-selection and non-response biases, as the survey was anonymous, and participants could decline participation at any stage. To ensure a 95% confidence level with a low margin of error in the results, the study collected over 300 more responses than the pre-determined target while attending to have sufficient and comparable sample sizes across the four racial/ethnic groups. As the research objective was to highlight group disparities rather than causality, the analysis primarily reported on statistical differences. The cross-sectional design captured behavior and perceptions at one point in time but cannot account for possible changes over time. Finally, the measures were self-recalled and perceived rather than actual visit records. Additional indicators of decision-making and care experience across racial/ethnic and SES groups could be included in future studies to unveil other variations. For instance, considering the diversity and level of assimilation to the US, country of origin, language proficiency, and immigration status can shed light on ways to improve perceived healthcare accessibility and utilization. It would be valuable to employ qualitative methods to explore the underlying causes of the persistent barriers and evaluate the effectiveness of targeted interventions along with longitudinal studies to track changes. Moreover, with the rise in eHealth services, it would be informative to investigate how health behaviors and preferences differ between online platforms and in-person interactions, as well as the provision of educational programs to support populations needing additional assistance.
Conclusion
By analyzing how people of different race/ethnicity and SES level experience healthcare differently, the study adds depth to the understanding of systemic inequities in healthcare provision and utilization. Access is built up on availability, affordability, approachability, and individual decisions. SES and race are intertwined determinants of patients receiving care. Easier access, more welcoming environments, and greater HCP diversityCitation66 can lower barriers and encourage care-seeking when needed to minimize preventable ailments and improve health outcomes among minorities and disadvantaged populations. Increasing awareness regarding seeing different provider types and expanding primary care to include basic gynecologist, dentist, and optometrist visits are efforts that can contribute to a more equal and appropriate regularity in obtaining care. Policymakers, HCPs, and public health professionals should continue to address not just economic or insurance factors but also structural, perceptual, and cultural-specific issues for system changes when creating laws, designing and delivering care, and implementing interventions to ensure a more inclusive health system.
Ethics Approval and Informed Consent
The research study complied with the Declaration of Helsinki and was approved by Duke University IRB. Informed consent was obtained from each participant.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors would like to thank Duke University Interdisciplinary and International Studies, Undergraduate Research Support, Program II, and Bass Connections for their support in data collection and open-access publication.
Data Sharing Statement
Data presented in this manuscript are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Hispanic/Latino - The Office of Minority Health. Available from: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64. Accessed August 6, 2023.
- Campos CL, Rodriguez CJ. High blood pressure in Hispanics in the United States: a review. Curr Opin Cardiol. 2019;34(4):350. doi:10.1097/HCO.0000000000000636
- Fei K, Rodriguez-Lopez JS, Ramos M. Racial and Ethnic Subgroup Disparities in Hypertension Prevalence, New York City Health and Nutrition Examination Survey, 2013–2014. Prev Chronic Dis. 2017;14. 10.5888/pcd14.160478.
- Klein R, Klein BEK. The Prevalence of Age-Related Eye Diseases and Visual Impairment in Aging: current Estimates. Invest Ophthalmol Vis Sci. 2013;54(14):ORSF5–ORSF13. doi:10.1167/iovs.13-12789
- Overweight. Obesity Statistics - NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed March. 2024;10:1.
- Branch B, Conway D Health Insurance Coverage by Race and Hispanic Origin: 2021; 2021.
- Findling MG, Bleich SN, Casey LS, et al. Discrimination in the United States: experiences of Latinos. Health Serv Res. 2019:54(S2):1409–1418. 10.1111/1475-6773.13216.
- National Academies of Sciences E, Division H and M, Practice B on PH and PH. The State of Health Disparities in the United States. Communities in Action: Pathways to Health Equity. National Academies Press (US). 2017. https://www.ncbi.nlm.nih.gov/books/NBK425844/.
- Yearby R. Racial Disparities in Health Status and Access to Healthcare: the Continuation of Inequality in the United States Due to Structural Racism. Am J Econ Sociol. 2018;77(3–4):1113–1152. doi:10.1111/ajes.12230
- McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and Access to Healthcare: interrelated Drivers for Healthy Aging. Front Public Health. 2020;8:231. doi:10.3389/fpubh.2020.00231
- Ezeonwu MC. Specialty-care access for community health clinic patients: processes and barriers. J Multidiscip Healthc. 2018;11:109–119. doi:10.2147/JMDH.S152594
- Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does “access to health care” mean? J Health Serv Res Policy. 2002;7(3):186–188. doi:10.1258/135581902760082517
- Ellis RJ, Yuce TK, Hewitt DB, et al. National Evaluation of Patient Preferences in Selecting Hospitals and Healthcare Providers. Med Care. 2020;58(10):867–873. doi:10.1097/MLR.0000000000001374
- Bornstein BH, Marcus D, Cassidy W. Choosing a doctor: an exploratory study of factors influencing patients’ choice of a primary care doctor. J Eval Clin Pract. 2000;6(3):255–262. doi:10.1046/j.1365-2753.2000.00256.x
- Liu N, Finkelstein S, Kruk M, Rosenthal D. When Waiting to See a Doctor Is Less Irritating: understanding Patient Preferences and Choice Behavior in Appointment Scheduling. Manage Sci. 2017;64. doi:10.1287/mnsc.2016.2704
- Kozikowski A, Morton-Rias D, Mauldin S, Jeffery C, Kavanaugh K, Barnhill G. Choosing a Provider: what Factors Matter Most to Consumers and Patients? J Patient Exp. 2022;9:237437352210741. doi:10.1177/23743735221074175
- Lin C, Tu P, Parker T, Mella-Velazquez A, Bier B, Braund WE. The Influences of SES on Patient Choice of Doctor: a Systematic Review. Am J Prev Med. 2024. doi:10.1016/j.amepre.2024.06.012
- Romaire MA. Use of Primary Care and Specialty Providers: findings from the Medical Expenditure Panel Survey. J Gen Intern Med. 2020;35(7):2003–2009. doi:10.1007/s11606-020-05773-7
- Franks P, Fiscella K. Primary care physicians and specialists as personal physicians: health care expenditures and mortality experience. J Fam Pract. 1998;47(2):105–110.
- Fradgley EA, Paul CL, Bryant J. A systematic review of barriers to optimal outpatient specialist services for individuals with prevalent chronic diseases: what are the unique and common barriers experienced by patients in high income countries? Int J Equity Health. 2015;14(1):52. doi:10.1186/s12939-015-0179-6
- Kouyoumdjian H, Zamboanga BL, Hansen DJ. Barriers to community mental health services for Latinos: treatment considerations. Clin Psychol Sci Pract. 2003;10(4):394–422. doi:10.1093/clipsy.bpg041
- Sripa P, Hayhoe B, Garg P, Majeed A, Greenfield G. Impact of GP gatekeeping on quality of care, and health outcomes, use, and expenditure: a systematic review. Br J Gen Pract. 2019;69(682):e294–e303. doi:10.3399/bjgp19X702209
- Cai C, Gaffney A, McGregor A, et al. Racial and Ethnic Disparities in Outpatient Visit Rates Across 29 Specialties. JAMA Intern Med. 2021;181(11):1525–1527. doi:10.1001/jamainternmed.2021.3771
- Sorkin DH, Ngo-Metzger Q, De Alba I. Racial/Ethnic Discrimination in Health Care: impact on Perceived Quality of Care. J Gen Intern Med. 2010;25(5):390–396. doi:10.1007/s11606-010-1257-5
- DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and Health Outcomes. J Gen Intern Med. 2004;19(12):1228–1239. doi:10.1111/j.1525-1497.2004.40153.x
- Sentell T, Braun KL. Low Health Literacy, Limited English Proficiency, and Health Status in Asians, Latinos, and Other Racial/Ethnic Groups in California. J Health Commun. 2012;17(sup3):82–99. doi:10.1080/10810730.2012.712621
- Jacobs RJ, Ownby RL, Acevedo A, Waldrop-Valverde D. A qualitative study examining health literacy and chronic illness self-management in Hispanic and non-Hispanic older adults. J Multidiscip Healthc. 2017;10:167–177. doi:10.2147/JMDH.S135370
- Misra S, Jackson VW, Chong J, et al. Systematic Review of Cultural Aspects of Stigma and Mental Illness among Racial and Ethnic Minority Groups in the United States: implications for Interventions. Am J Community Psychol. 2021;68(3–4):486–512. doi:10.1002/ajcp.12516
- Mascayano F, Tapia T, Schilling S, et al. Stigma toward mental illness in Latin America and the Caribbean: a systematic review. Braz J Psychiatry. 2016;38(1):73–85. doi:10.1590/1516-4446-2015-1652
- Anderson K, Fullerton A. Residential Segregation, Health, and Health Care: answering the Latino Question. Race Soc Probl. 2014;6(3):262–279. doi:10.1007/s12552-014-9125-2
- Cabral J, Cuevas AG. Health Inequities Among Latinos/Hispanics: documentation Status as a Determinant of Health. J Racial Ethn Health Disp. 2020;7(5):874–879. doi:10.1007/s40615-020-00710-0
- Tyson A, Lopez MH 5 facts about Hispanic Americans and health care. Pew Research Center. Available from: https://www.pewresearch.org/short-reads/2023/10/30/5-facts-about-hispanic-americans-and-health-care/. Accessed January 16, 2024.
- Gaskin DJ, Dinwiddie GY, Chan KS, McCleary RR. Residential Segregation and the Availability of Primary Care Physicians. Health Serv Res. 2012;47(6):2353–2376. doi:10.1111/j.1475-6773.2012.01417.x
- Basu J, Clancy C.Racial disparity, primary care, and specialty referral. Health Serv Res. 2001;36(6):64–77.
- Kristjansson E, Hogg W, Dahrouge S, Tuna M, Mayo-Bruinsma L, Gebremichael G. Predictors of relational continuity in primary care: patient, provider and practice factors. BMC Fam Pract. 2013;14(1):72. doi:10.1186/1471-2296-14-72
- Beal A, Hernandez S. Patient Reports of the Quality of Care in Community Health Centers: the Importance of Having a Regular Provider. J Health Care Poor Underserved. 2010;21(2):591–605. doi:10.1353/hpu.0.0305
- Hahn RA. What is a social determinant of health? Back to basics. J Public Health Res. 2021;10(4):2324. doi:10.4081/jphr.2021.2324
- Social Determinants of Health - Healthy People 2030 | health.gov. Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health. Accessed August 7, 2023.
- Coffman MJ, Norton CK, Beene L. Diabetes symptoms, health literacy, and health care use in adult Latinos with diabetes risk factors. J Cult Divers. 2012;19(1):4–9.
- Becerra BJ, Arias D, Becerra MB. Low Health Literacy among Immigrant Hispanics. J Racial Ethn Health Disp. 2017;4(3):480–483. doi:10.1007/s40615-016-0249-5
- Calvo R. Health Literacy and Quality of Care among Latino Immigrants in the United States. Health Soc Work. 2016;41(1):e44–e51. doi:10.1093/hsw/hlv076
- Theory of Reasoned Action - an overview | scienceDirect Topics. Available from: https://www-sciencedirect-com.proxy.lib.duke.edu/topics/medicine-and-dentistry/theory-of-reasoned-action. Accessed September 22, 2023.
- Smith AK, Sudore RL, Pérez-Stable EJ. Palliative Care for Latino Patients and Their Families: “Whenever We Prayed, She Wept. JAMA J Am Med Assoc. 2009;301(10):1047–E1. doi:10.1001/jama.2009.308
- Gallo Marin B, Oliva R, Anandarajah G. Exploring the Beliefs, Values, and Understanding of Quality End-of-Life Care in the Latino Community: a Spanish-Language Qualitative Study. Am J Hosp Palliat Med. 2023;10499091231188693. doi:10.1177/10499091231188693
- Ortiz BI, Shields KM, Clauson KA, Clay PG. Complementary and Alternative Medicine Use Among Hispanics in the United States. Ann Pharmacother. 2007;41(6):994–1004. doi:10.1345/aph.1H600
- Fowler AL, Mann ME, Martinez FJ, Yeh HW, Cowden JD. Cultural Health Beliefs and Practices Among Hispanic Parents. Clin Pediatr. 2022;61(1):56–65. doi:10.1177/00099228211059666
- Mikhail N, Wali S, Ziment I. Use of Alternative Medicine Among Hispanics. J Altern Complement Med. 2004;10(5):851–859. doi:10.1089/acm.2004.10.851
- Hewins-Maroney B, Schumaker A, Williams E. Health Seeking Behaviors of African Americans: implications for Health Administration. J Health Hum Serv Adm. 2005;28(1):68–95.
- Zhang AY, Snowden LR, Sue S. Differences between Asian and White Americans’ help seeking and utilization patterns in the Los Angeles area. J Community Psychol. 1998;26(4):317–326. doi:10.1002/(SICI)1520-6629(199807)26:4<317::AID-JCOP2>3.0.CO;2-Q
- Khanijahani A, Iezadi S, Gholipour K, Azami-Aghdash S, Naghibi D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health. 2021;20(1):248. doi:10.1186/s12939-021-01582-4
- Murayama K, Usami S, Sakaki M. Summary-statistics-based power analysis: a new and practical method to determine sample size for mixed-effects modeling. Psychol Methods. 2022;27(6):1014–1038. doi:10.1037/met0000330
- Lenth RV. Some Practical Guidelines for Effective Sample Size Determination. Am Stat. 2001;55(3):187–193. doi:10.1198/000313001317098149
- U.S. Census Bureau QuickFacts: United States. Available from: https://www.census.gov/quickfacts/fact/table/US/RHI225222. Accessed December 6, 2023.
- Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the Health Care System and the Use of Preventive Health Services by Older Black and White Adults. Am J Public Health. 2009;99(7):1293–1299. doi:10.2105/AJPH.2007.123927
- Armstrong K, Putt M, Halbert CH, et al. Prior Experiences of Racial Discrimination and Racial Differences in Health Care System Distrust. Med Care. 2013;51(2):144. doi:10.1097/MLR.0b013e31827310a1
- Becerra D, Androff D, Messing JT, Castillo J, Cimino A. Linguistic Acculturation and Perceptions of Quality, Access, and Discrimination in Health Care Among Latinos in the United States. Soc Work Health Care. 2015;54(2):134–157. doi:10.1080/00981389.2014.982267
- Steinberg EM, Valenzuela-Araujo D, Zickafoose JS, Kieffer E, DeCamp LR. The “Battle” of Managing Language Barriers in Health Care. Clin Pediatr. 2016;55(14):1318–1327. doi:10.1177/0009922816629760
- Mercado F, Mercado M, Myers N, Hewit M, Haller NA. Patient preferences in choosing a primary care physician. J Prim Care Community Health. 2012;3(2):125–131. doi:10.1177/2150131911421802
- Freedman RA, Kouri EM, West DW, Keating NL. Racial/Ethnic Differences in Patients’ Selection of Surgeons and Hospitals for Breast Cancer Surgery. JAMA Oncol. 2015;1(2):222. doi:10.1001/jamaoncol.2015.20
- Braveman P, Gottlieb L. The Social Determinants of Health: it’s Time to Consider the Causes of the Causes. Public Health Rep. 2014;129(Suppl 2):19–31. doi:10.1177/00333549141291S206
- Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39(1):273–289. doi:10.1146/annurev-publhealth-031816-044628
- Lipton BJ, Decker SL. The effect of health insurance coverage on medical care utilization and health outcomes: evidence from Medicaid adult vision benefits. J Health Econ. 2015;44:320–332. doi:10.1016/j.jhealeco.2015.10.006
- Elam AR, Tseng VL, Rodriguez TM, Mike EV, Warren AK, Coleman AL. DISPARITIES IN VISION HEALTH AND EYE CARE. Ophthalmology. 2022;129(10):e89–e113. doi:10.1016/j.ophtha.2022.07.010
- Wallace NT, Carlson MJ, Mosen DM, Snyder JJ, Wright BJ. The Individual and Program Impacts of Eliminating Medicaid Dental Benefits in the Oregon Health Plan. Am J Public Health. 2011;101(11):2144–2150. doi:10.2105/AJPH.2010.300031
- Riley WJ. Health Disparities: gaps in Access, Quality and Affordability of Medical Care. Trans Am Clin Climatol Assoc. 2012;123:167–174.
- Vanderbilt AA, Dail MD, Jaberi P. Reducing health disparities in underserved communities via interprofessional collaboration across health care professions. J Multidiscip Healthc. 2015;8:205–208. doi:10.2147/JMDH.S74129
- Kaguru G, Ayah R, Mutave R, Mugambi C. Integrating Oral Health into Primary Health Care: a Systematic Review of Oral Health Training in Sub-Saharan Africa. J Multidiscip Healthc. 2022;15:1361–1367. doi:10.2147/JMDH.S357863
- Boen C. The Role of Socioeconomic Factors in Black-White Health Inequities Across the Life Course: point-in-time Measures, Long-term Exposures, and Differential Health Returns. Soc Sci Med 1982. 2016;170:63–76. doi:10.1016/j.socscimed.2016.10.008
- Assari S, Nikahd A, Malekahmadi MR, Lankarani MM, Zamanian H. Race by Gender Group Differences in the Protective Effects of Socioeconomic Factors Against Sustained Health Problems Across Five Domains. J Racial Ethn Health Disp. 10.1007/s40615-016-0291-3
- Assari S. The Benefits of Higher Income in Protecting against Chronic Medical Conditions Are Smaller for African Americans than Whites. Healthcare. 2018;6(1):2. doi:10.3390/healthcare6010002
- Yearby R, Clark B, Figueroa JF. Structural Racism In Historical And Modern US Health Care Policy. Health Aff. 2022;41(2):187–194. doi:10.1377/hlthaff.2021.01466
