Abstract
Recently, attention to the lifestyle of patients has been rapidly increasing in the field of pain therapy, particularly with regard to the role of nutrition in pain development and its management. In this review, we summarize the latest findings on the role of nutrition and nutraceuticals, microbiome, obesity, soy, omega-3 fatty acids, and curcumin supplementation as key elements in modulating the efficacy of analgesic treatments, including opioids. These main topics were addressed during the first edition of the Study In Multidisciplinary Pain Research workshop: “FYD (Feed Your Destiny): Fighting Pain”, held on April 7, 2016, in Rome, Italy, which was sponsored by a grant from the Italian Ministry of Instruction on “Nutraceuticals and Innovative Pharmacology”. The take-home message of this workshop was the recognition that patients with chronic pain should undergo nutritional assessment and counseling, which should be initiated at the onset of treatment. Some foods and supplements used in personalized treatment will likely improve clinical outcomes of analgesic therapy and result in considerable improvement of patient compliance and quality of life. From our current perspective, the potential benefit of including nutrition in personalizing pain medicine is formidable and highly promising.
Introduction
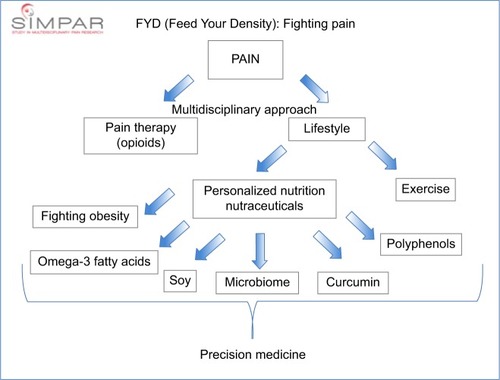
In addition to the severity of the underlying condition, interindividual variability in chronic pain depends on many factors, including its sociocultural context,Citation1 patients’ genetic backgrounds,Citation2,Citation3 psychological factors,Citation4 and pathophysiology,Citation5 that can be modulated and monitored by altering nutritional habits.Citation6 During the eighth annual international meeting of the Study In Multidisciplinary Pain Research (SIMPAR), we attempted to remedy the knowledge gap in this field by conducting a workshop, entitled “FYD (Feed Your Destiny): Fighting Pain”. The main focus of this workshop was on the association of nutrition and nutraceuticals with pain development and perception, appropriate nutrition for patients with cancer, the role of obesity in pain chronification, the microbiome involved in pain, and the specific role of soy, omega-3 fatty acids, curcumin, and polyphenols on inflammatory and degenerative painful diseases as well as on opioid tolerance (). This workshop followed the philosophy of the SIMPAR group, which has strived to direct the international and multidisciplinary dissemination of the most innovative issues regarding pain, ranging from basic science to translational and clinical research. The workshop also integrated a diverse array of theoretical and practical views on the relationship between chronic pain and nutrition. Our ultimate goal was to identify a starting point for a study group aimed to define a new internationally accepted guideline that will seek the integration of nutrition with pharmacological approaches. To this end, we are designing a multicenter randomized placebo-controlled clinical trial evaluating the value of personalized nutrition and nutraceutical supplements as well as assessing the genetic backgrounds and epigenetic dynamicity to identify new objective biomarkers of efficacy for the management of chronic pain. This approach will further the efforts to define a precision medicine model in the treatment of pain. In particular, we will link personalized nutritional programs and nutraceutical supplements with clinical outcomes in terms of efficacy and safety of various therapies and analyze their correlation with the interindividual variability of genetic backgrounds and the modulation of epigenetic patterns (DNA methylation and microRNA expression). Our expectation is that this nutritional approach will further clarify the role of precision medicine in the treatment of pain, acting as an essential, integrated, non-pharmacological strategy and as an aspect of multidisciplinary treatment for chronic pain.
Workshop description
The workshop was divided into two sessions. Doctor Stallone, who is the President of the Italian National Institution for Social Security and Assistance for Biologists (ENPAB) from Rome, described the state of the art of nutrition, stressing the importance of current evidence on obesity comorbidity in the development and progression of a variety of chronic pain conditions. Professor Muscoli from the University of Magna Graecia in Catanzaro presented the current data regarding nutraceuticals, with a focus on their roles in pain conditions. Then, Professor Rondanelli from the University of Pavia addressed topics of nutrition in patients receiving opioid therapy, emphasizing the ideal nutritional pyramid to be followed to optimize these patients’ pain management. Professor Franceschi from the Catholic University of Rome elucidated the importance of the gut microbiome in chronic pain. Professor Arranz from the University of Barcelona provided the final lecture of the first session, demonstrating the role of obesity in the function and quality of life (QoL) in patients with chronic pain conditions.
Professor Belfer from McGill University, who served as one of the Presidents of the SIMPAR meeting, described the role of soy in pain and analgesia. She was followed by Professor Lorente-Cebrián from the University of Navarra and Doctor Salamone from Metagenics, a privately held company in Italy that develops nutritional products to maximize genetic potentials, who provided an overview of the effects of omega-3 fatty acids and curcumin on chronic pain. Finally, Doctor Ilari from the Hospital IRCCS San Raffaele Pisana in Rome (a private rehabilitation hospital and research center in Rome) clarified the crucial role of natural derived antioxidants in inflammation and opioid tolerance.
Review of relevant research
The regulation of food intake involves a close relationship between homeostatic and non-homeostatic factors. In particular, homeostatic factors influence the hypothalamic arcuate nucleus and the solitary tract, acting on hunger satiety centers. Ghrelin, YY peptide, spinal nerves, and the vagus nerve provide short-term signals, while leptin, adiponectin, and insulin provide long-term signals of body weight and fat storage.Citation7 The problem of poor nutrition also has neurochemical implications, as levels of dopamine, the “neurotransmitter of pleasure”, increase with consumption of sugars, fats, and salt.
Alonso-Alonso et alCitation8 recently described “food addiction”, explaining that food, like any other rewarding stimulus, has the potential to cause addictive behavior. Drugs and foods share certain traits, yet differ qualitatively and quantitatively. Indeed, drugs directly influence brain dopamine circuits, while food influences dopamine in more indirect ways: from neuronal input from the taste buds to dopamine-secreting neurons in the brain, as well as from signals generated by digestion. Moreover, some people are less influenced than others by the reward system, due to a D2 receptor that is less responsive to dopamine due to interindividual variability of genetic backgrounds, resulting in variability in the amount of food required to reach the same level of pleasure.Citation9 Behavioral drives for palatable food are also moderated by cognition; lateral and dorsomedial regions of the cortex (dorsomedial region and parietal cortex) can influence the reward system. Therefore, the combination of cognitive behavioral therapy, nutritional counseling, physical exercise, and human relationship counseling should be able to suppress the rewarding effects of food and provide reinforcement through the frontal cortex.
The ENPAB and Brain Research Foundation network is studying eating behavioral aspects of food addiction; Italian nutrition biologists have recently initiated an “observatory for the study of eating behavior”. The nutraceutical discipline has been coupled with nutritional counseling in the management and prevention of disease.Citation6,Citation10,Citation11 The term “nutraceutical” was coined from the combination of “nutrition” and “pharmaceutical” in 1989 by Doctor Stephen DeFelice. The term refers to a food, or part of a food, providing health benefits, including the prevention and treatment of a disease.Citation12 The global nutraceutical market has been valued at approximately $250 billion in 2014: the market is expected to reach $385 billion by 2020 at a compounded annual growth rate of 7.5% from 2014 to 2020. The nutraceutical market includes functional foods, beverages, and dietary supplements. The annual sales of nutraceutical ingredients market worldwide have been predicted to reach 29.5 billion USD, with nutraceutical product sales predicted to reach 204.8 billion USD in 2017.Citation13,Citation14 Nutraceuticals are products purified from foods generally sold in medicinal forms, such as powders, tablets, or capsules, which have been developed to provide protection against chronic disease. Nutraceuticals can be derived from plants, animals, and microorganisms (eg, essential fatty acids and enzymes) and from marine sources (eg, glucosamine, chitosan, and fish oils). A nutraceutical can also deliver bioactive agents in doses achievable through a healthy diet, although these compounds also provide specific features such as a formulation that enhances their absorption and/or physiological effect. Isolated compounds (although not extracts) from nonfood origin can be used in nutraceuticals only if these compounds are also usually present in foods. Other dietary supplements such as those containing vitamins, minerals, amino acids, and other nutrients or micronutrients with well-known roles in human nutrition and/or known recommended daily allowances are recognized as nutraceuticals if the dosage provided is clearly related to a beneficial effect beyond their recommended daily allowance values.
For the safe use of a new dietary ingredient (NDI), the following information about its chemical nature should be provided: the nature of the extract (raw, enriched, purified), fermentation, chemical synthesis, chemical name of the efficacious molecule, and its impurity profile.Citation15 In the case of non-single compound NDI, it is necessary to standardize the dose/content of efficacious molecules and provide evidence regarding the role of other compounds with high prevalence in the mixture and their relevant effect; it is necessary to understand the stability of a compound in its galenic form and ascertain its bioavailability data in humans. With the assumption that the safe human use of an NDI is documented by food-based exposure data (human plasma levels) and by additional preclinical and clinical safety data, the dietary intake of populations with the highest safe and beneficial dietary intake of the compound is used as a basis to define the intended dose.Citation16 The intended dose can be significantly higher (more than threefold) than the dietary intake, provided that it is supported by additional safety data. The recommended dose must be at least a small multiple below the safe upper limit of the dietary ingredient.Citation17–Citation19
Nutrition, opioids, and cancer
Despite their drawbacks, opioids are still considered by many as the most effective analgesic for chronic pain.Citation20,Citation21 One of the main concerns regarding their use is opioid-induced constipation (OIC), due to their binding to receptors in the gastrointestinal (GI) tract. In mild cases of OIC, symptoms can be mitigated by increasing physical activity together with dietary fiber and fluid intake. More severe cases require specialized medications that target the unique characteristics of OIC. Constipation has been reported to be one of the four factors that significantly and independently predict hospitalization in hospice care.Citation22 Estimates of OIC have been found to vary widely, with investigations identifying rates of OIC among opioid users ranging from 15% to 90%.Citation23–Citation26 In addition, a series of studies conducted in a large hospice in Florida have evaluated the constipation induced by opioids and demonstrated that a considerable proportion of patients hospitalized with cancer (from 40% to 64%) experienced constipation. Interestingly, the number was found to be lower when the data were obtained from a screening of staff (40%) and higher when the researchers interviewed patients regarding their symptoms (63%–64%).Citation27–Citation29 In conclusion, mitigating constipation is an important aspect of the management of patients with opioid-related adverse drug events, as various studies have demonstrated that the presence of constipation is significantly negatively correlated with overall QoL.Citation30,Citation31 The ideal dietary approach for patients on opioids should include increased consumption of fiber and fluids (at least eight glasses daily unless contraindicated), in conjunction with physical activity,Citation32 with abdominal exercises in bed or moving from bed to chair if the patient is not able to walk. Patients are encouraged to eat more high-fiber foods such as fruits (eg, raisins, prunes, peaches, and apples), vegetables (eg, squash, broccoli, carrots, and celery), and 100% wholegrain cereals, breads, and bran. Nevertheless, fiber intake should occur several hours prior to or following the drug administration to mitigate a reduction in the bioavailability of certain drugs.Citation33 Rondanelli et al (unpublished, 2016) have recently designed a food pyramid for patients requiring opioid analgesia, based on anti-inflammatory and antioxidant agents (submitted article). In the presence of a constipation problem, a proper distribution of five meals during the day is suggested, based on breakfast, mid-morning snack, lunch, mid-afternoon snack, and dinner, to activate gastro-ileocecal reflection and allow the progression of food to the rectum. Moreover, it is beneficial to emphasize the intake of both soluble and insoluble fiber, in particular, to reduce constipation.Citation34,Citation35
Microbiome and pain
Mutualistic bacteria (~800–1,000 g) colonize the entire GI tract with different orders of magnitude, increasing from the esophagus to the anus. The so-called gut bacteriome involves >10,000 genes, more than nine phyla (of which ~95% of genes have been identified), >1,000 species (of which 99% of genes have been identified), and >17,000 strains (of which 100% of genes have been identified). The two major phyla are Firmicutes and Bacteroidetes (which constitute 80%–90% of microbiota).Citation36–Citation38 Gut microbiota have specific effects in each section of the GI tract: barrier effect, immunocompetence/tolerance, synthesis, metabolism, drug metabolism, and behavior conditioning. A strong balance between all microbiota species is modulated by several factors, including gastric acidity, biliary salts, mucus thickness, normal peristalsis, and normal anatomy, while a failure of their activity determines an imbalance of gut microbiota composition called dysbiosis, which, in turn, may cause GI and non-GI diseases, including metabolic syndromes. Small intestinal bacterial overgrowth is a specific kind of dysbiosis that is associated with various manifestations, including malabsorption and small bowel carbohydrate fermentation with gas production, abdominal pain, and diarrhea.
The most commonly used agents for preventing or treating nonsteroidal anti-inflammatory drugs (NSAIDs)-induced damage are proton pump inhibitors (PPIs). However, these medications do not offer protection to the lower small intestine and actually exacerbate NSAID-induced small intestinal lesions. A critical role of bacteria composing gut microbiota was recently reinforced by a study demonstrating that NSAID enteropathy in rats is exacerbated by concomitant treatment with a PPI through a dysbiotic mechanism. Specifically, the investigators identified a marked loss of Bifidobacterium and Lactobacilli following PPI treatment.Citation39 NSAID-related gastroenteropathy is due to a decrease of Lactobacilli, with an impairment of the maintenance of luminal pH, mucosal permeability, enterocyte adhesion, mucus production, and immune system modulation. The concomitant decrease of Bifidobacterium exacerbates both intestinal motility and local immunity.Citation40 These data allow us to conclude that NSAIDs induce mucosal injuries confined not only to the stomach but also to the small intestine.Citation41 This provides an explanation for NSAID-related abdominal pain. In this regard, paracetamol administration may be safer than NSAIDs, as its utilization does not require concomitant treatment with PPI, impair gut permeability, and affect platelet function.Citation42 Opioids may also be a valid option in treating abdominal pain. Based upon the Italian Intersociety Recommendations (SIAARTI, SIMEU, SIS 118, AISD, SIARED, SICUT, IRC) on pain management in the emergency setting, statement F, pain relief and the use of opioids in patients with acute abdominal pain do not increase the risk of error in diagnosis and therapeutic pathways in adults.Citation43
Obesity and chronic pain
Obesity is categorized by using body mass index (BMI), which is calculated as the body weight divided by the square of body height (kg/m2). Depending on BMI values, people may be classified as underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9), or obese (≥30). Approximately 39% of adults (18 years and older) worldwide are overweight, with 13% obese (World Health Organization, 2015, http://www.who.int/mediacen-tre/factsheets/fs311/en/). Obesity is related to important metabolic diseases such as diabetes, hypertension, heart disease, and hypercholesterolemia. Nevertheless, ~80% of enrolled patients fail to complete weight loss programs (Federation of European Nutrition Societies data). It is estimated that by 2025, the global obesity prevalence will reach 18% among men and exceed 21% among women, while severe obesity will exceed 6% among men and 9% among women.Citation44 Growing evidence suggests that there is a precise relationship between obesity and chronic pain; they coexist and adversely impact each other (reciprocal negative effects).Citation45–Citation47 Obesity and pain serve to further reduce functional capacity and QoL,Citation48 causing patients to become less physically active and more depressed, with consequences for sleep, stress, lifestyle, and chronic inflammation status. Accordingly, a reduction from high to normal BMI may improve QoL.Citation49 The effect of obesity in chronic pain conditions has been studied in fibromyalgia, osteoarthritis, rheumatoid arthritis, and low back pain. Thus, the management of obesity as well as chronic pain should be considered synergistic. Adipose tissue is not only an energy store but also an active endocrine organ involved, among other functions, in the regulation of inflammation.Citation50 Obese individuals suffer more chronic pain than normal weight subjects;Citation51 therefore, changes in lifestyle can help improve both obesity and chronic pain conditions.Citation52,Citation53 A study demonstrated that increasing BMI, specifically android distribution of fat mass, was strongly associated with foot pain and disability.Citation54 In contrast, a beneficial effect of a gynoid distribution of fat was observed, suggesting that the mechanism of obesity’s effect on disability might be the result of both a mechanical effect (through increasing the load on the skeletal system) and a systemic effect related to metabolic factors and pro-inflammatory cytokine production.Citation54
Soy and pain
Soybeans are a source of phytoestrogens (such as isoflavone genistein) with potent estrogenic activity. Studies suggest that soy consumption may result in several pain-related functions including increasing anti-nociception via GABAA receptor mechanismsCitation55 inhibiting the protein kinase C,Citation56 modulating cytokinesCitation57 and the immune response,Citation58 and acting as an antioxidant.Citation59 Interestingly, the effects of soy on human pain are gender based to a degree, with higher analgesia observed in men.Citation60 In rats, the effects of soy on neuropathic pain have been demonstrated to be model specific. The US Food and Drug Administration in 1999 approved the claim of soy in lowering cholesterol, and soy immediately became part of a “healthy lifestyle”, with reported positive effects on reducing symptoms and signs of many diseases from diabetes and osteoporosis to diarrhea and kidney diseases.Citation61 However, mixed results were found for soy’s analgesic effects, for example, on cyclical breast pain.Citation62 Several animal and human studies have been performed, suggesting that the effects of soy depend on the kind of soy used; soy beverages seem not to have an impact on women with breast cancer,Citation63 revival soy does not affect the symptoms of fibromyalgia (no improvements in pain, function, and depression),Citation64 while whole soybean soymilk powder appears to reduce neuropathic pain when administered preemptively.Citation57,Citation65 The effects of soy on pain also depend upon the specific pain condition. It is protective against postsurgical (postmastectomy) painCitation66 and osteoarthritisCitation67 and is an analgesic for menopausalCitation68 and bone cancer pain,Citation69 but it increases other types of pain such as migraines.Citation70 Finally, soy protein has a gender-specific action, as it improves osteoarthritis pain in men although not in women.Citation67 Currently, it remains to be determined when and how soy intervention is involved in obtaining major analgesic effects in the individual patient.
Omega-3 fatty acids and pain
Several diseases have an inflammatory component, such as obesity or neurodegenerative diseases of aging. Eicosapentaenoic acid (EPA) (20 carbons:5 double bonds) and docosahexaenoic acid (DHA) (22 carbons:6 double bonds) are long-chain polyunsaturated fatty acids (LC-PUFA), omega-3 (n-3) fatty acids, whose source is represented by fish oils and fish oil supplements. Both EPA and DHA derive from the α-linolenic acid (ALA 18:3 omega-3). They block inflammation through a variety of mechanisms of action, proresolving lipid mediators.Citation71,Citation72 In vivo studies demonstrated that omega-3 LC-PUFAs prevent inflammatory symptoms linked to obesity rather than adiposity in obese and metabolic syndrome conditions.Citation73–Citation93 Omega-3 LC-PUFAs also play a role in cardiovascular diseases.Citation88,Citation94–Citation109 Various health associations including the American Heart Association and the American Diabetes Association recommend daily fish and/or n-3 LC-PUFAs (EPA/DHA) intake for the prevention of chronic heart disease and cardiovascular diseases. Regarding degenerative disorders, longitudinal studies have demonstrated negative correlations between fish intake and cognitive impairment in mental/cognitive decline, Alzheimer disease, and dementia, generally.Citation110–Citation119 Moreover, DHA is the precursor of the neuroprotectin D1, which reduces neuro-inflammation and protects neural cells against Alzheimer disease and photoreceptor renewal.Citation5,Citation120,Citation121 Directions for further investigation include the analysis of the relationship between dietary EPA and DHA in regulating pain and the evaluation of the possible role of EPA and DHA as potential therapeutic agents in nociceptive and neuropathic pain.
Curcumin and pain
Curcumin represents a natural substance with anti-inflammatory activity; it is derived from the turmeric (Curcuma longa) plant, which is a rhizomatous, herbaceous, and perennial plant belonging to the Zingiberaceae family. It lives in mild temperatures (20°C–30°C in the tropical rainy regions), reaches 1 m in height and bears hermaphrodite flowers. The active substances of this plant are concentrated in the rhizomes. Turmeric powder from the rhizomes contains 3%–7% of three different curcuminoids (curcumin, demethoxycurcumin, and bisdemethoxycurcumin), essential oils, and fibers. The European Food Safety Authority, in a scientific evaluation of curcumin as food additive, declared that curcumin is not carcinogenic and there are no concerns regarding genotoxicity.Citation122 The acceptable daily intake of curcumin corresponds to 3 mg/kg body weight (bw)/day based on the no observed adverse effect level of 250–320 mg/kg bw/day. Intake of curcumin from the normal diet amounts to <7% of the acceptable daily intake of 3 mg/kg bw/day. It might weakly interfere with anticoagulation, although that normally does not require dosage adjustments.
By using the keyword “curcumin”, we identified 8,394 publications in PubMed between January 1, 2000, and April 30, 2016. Aggarwal et alCitation123 identified the inflammatory targets modulated by curcumin. A randomized, single-blind study on the efficacy and tolerability of curcumin in patients with rheumatoid polyarthritis demonstrated that curcumin extract produces a significant reduction of joint pain, joint swelling, and disease activity score.Citation124 Ramadan and El-MenshawyCitation125 demonstrated that the combination of curcumin and ginger is as effective as NSAIDs in a rat model of rheumatoid arthritis. Several animal model studies of curcumin have been performed in neuropathic pain.Citation126–Citation128 Hu et alCitation129 recently determined that curcumin attenuates opioid-induced hyperalgesia by inhibiting Ca2+/calmodulin-dependent protein kinase II α activity, and recently, Hu et alCitation130 found that a nanoformulation of poly(lactic-co-glycolide)-cucumin–curcumin may reverse opioid-induced hyperalgesia by inhibiting caMKIIa and downstream signaling. Curcumin is an antioxidant, as demonstrated by the 2,367 publications published in PubMed from 1988 to November 18, 2015. The antioxidant power is ten times that of vitamin E;Citation131 it has a direct activity on reactive oxygen species, on induction of NRF2, and induces mitochondrial biogenesis.Citation132–Citation134 Curcumin also plays a role in regulating epigenetic patterns.Citation135 Curcumin demonstrates synergistic activity with numerous drugs used to treat different painful conditions, and ongoing studies are evaluating the effect of 3-month treatment with curcumin on inflammation and QoL of patients with metabolic syndrome and osteoarthritis. Curcumin has low bioavailability, although bio-optimization techniques can improve it, thereby increasing the therapeutic and preventive potentials of the natural substance.Citation136
Polyphenols and pain
The use of natural antioxidants can be considered a useful approach to control the development and progression of several diseases. Epidemiological studies have demonstrated a relationship between the Mediterranean diet and a reduced incidence of pathologies such as coronary disease and cancer. A central hallmark of this diet is the high consumption of virgin olive oil as its main source of fat. This oil contains antioxidant components in the non-saponifiable fraction, including phenolic compounds absent in seed oils. The olive is the fruit of Oleaeuropaea, a tree native to the coastal Mediterranean region, which produces 98% of the world’s total (~11 million tons) and lends important economic and dietetic benefits to the people of that region.Citation137 Oleuropein and its hydrolysis product hydroxytyrosol are the main phenolic constituents of olive leaves and believed to be responsible for their pharmacological effects, as they are the most potent olive oil antioxidants.
In recent years, Citrus bergamia juice also has been raising interest and has been the subject of several studies considering its potential for health promotion. Bergamot is the common name for Citrus bergamia Risso et Poiteau, a plant belonging to the Rutaceae family (subfamily Esperidea). The beneficial effects of bergamot juice mainly derive from the bergamot polyphenol fraction. Currently, bergamot polyphenol fraction offers a viable alternative in the treatment of hypercholesterolemia in patients intolerant to treatment with statins. The mechanisms of action of bergamot-derived polyphenolic fraction include the reduction of cholesterol absorption and the inhibition of cholesterol biosynthesis, potentiating the effect of rosuvastatin.Citation138–Citation141 Muscoli et alCitation142 recently demonstrated in a rodent model of opioid tolerance that the removal of free radicals with phenolic compounds of olive oil, such as hydroxytyrosol and oleuropein or bergamot polyphenolic fraction derivatives, reinstates the analgesic action of morphine.Citation143 In particular, evidence exists that removal of nitric oxide, superoxide (SO), and peroxynitrite can prevent and reverse inflammatory pain, neuropathic pain, and morphine-induced hyperalgesia and tolerance.Citation142–Citation144 The identification of natural radical scavengers as novel non-narcotic agents is a viable therapeutic target for the development of non-narcotic analgesics in pain of various etiologies. Recent studies reinforce the importance of natural antioxidant products as a source of drugs to alleviate chronic pain.Citation142,Citation143,Citation145 Chronic injection of morphine in mice led to the development of tolerance associated with increased nitrotyrosine and the marker of lipid peroxidation malondialdehyde formation together with nitration and deactivation of manganese SO dismutase (MnSOD) in the spinal cord. Removal of free radicals by hydroxytyrosol and oleuropein blocked morphine tolerance by inhibiting nitration and malondialdehyde formation and replacing MnSOD activity. Thus, the analgesic effect in vivo of phenolic fraction of virgin olive oil derives from its antioxidant activities.Citation142 In addition, the development of anti-nociceptive tolerance to repeated doses of morphine in mice is consistently associated with increased tyrosine-nitrated proteins in the dorsal horn of the spinal cord as the enzyme glutamine synthase. Nitration of this protein is intimately linked to inactivation of its biological function and a resulting increase of glutamate levels in the spinal cord. Repeated administration of bergamot polyphenolic fraction as well as other substances with antioxidant properties such as N(G)-nitro-l-arginine methyl ester or manganese (III) tetrakis (4-benzoic acid) porphyrin significantly reduces the development of opioid-induced hyperalgesia. This effect was accompanied by a reduction of SO production, prevention of glutamine synthetase nitration, and reestablishment of its activity and of glutamate levels.Citation145
Conclusion
The FYD workshop focused on the role of personalized nutrition and nutraceuticals, by considering how they might be helpful in the management of chronic pain, as well as their physiological features (such as body mass and microbiome) and pathological ones (such as cancer). We primarily focused on soy, curcumin, and omega-3 fatty acids, oleuropein and bergamot polyphenols. Although we have presented a considerable body of relevant literature in our review, additional investigations are needed to determine exactly which dietary recommendations and supplements are suitable in the clinical pain setting and how they might help patients by improving pain relief, functionality, and QoL according to a broader multidisciplinary therapeutic approach. New prospective, randomized clinical trials will need to be performed. A new edition of the FYD workshop will be organized to create a stable yet dynamic discussion within the scientific community to promote the employment of nutrition and nutraceuticals as viable tools in pain therapy and to produce innovative guidelines to better address the therapeutic needs of patients with chronic pain.
Acknowledgments
This work was supported by Grants from Italian Ministry of Instruction (PON03PE_00078_1, PON03PE_00078_2), European Commission (FP7 Collaborative Project Pain-OMICS; grant agreement number: 602736), and Italian Ministry of Health (project code: GR-2010-2318370).
Disclosure
The authors report no conflicts of interest in this work.
References
- Di TellaMCastelliLColonnaFTheory of mind and emotional functioning in fibromyalgia syndrome: an investigation of the relationship between social cognition and executive functionPLoS One2015101e011654225594169
- BurriAOgataSLivshitsGWilliamsFThe association between chronic widespread musculoskeletal pain, depression and fatigue is genetically mediatedPLoS One20151011e014028926599910
- SmithSBReeniläIMännistöPTEpistasis between polymorphisms in COMT, ESR1, and GCH1 influences COMT enzyme activity and painPain2014155112390239925218601
- LeonardBEPain, depression and inflammation: are interconnected causative factors involved?Mod Trends Pharmacopsychiatri201530223526437055
- Lorente-CebriánSCostaAGNavas-CarreteroSAn update on the role of omega-3 fatty acids on inflammatory and degenerative diseasesJ Physiol Biochem201571234134925752887
- TickHNutrition and painPhys Med Rehabil Clin N Am201526230932025952067
- MarxJCellular warriors at the Battle of the BulgeScience200329984684912574615
- Alonso-AlonsoMWoodsSCPelchatMFood reward system: current perspectives and future research needsNutr Rev201573529630726011903
- DavisCLevitanRDYilmazZKaplanASCarterJCKennedyJLBinge eating disorder and the dopamine D2 receptor: genotypes and sub-phenotypesProg Neuropsychopharmacol Biol Psychiatry201238232833522579533
- HoustonMThe role of nutrition and nutraceutical supplements in the treatment of hypertensionWorld J Cardiol201462386624575172
- HoustonMCThe role of nutrition, nutraceuticals, vitamins, antioxidants, and minerals in the prevention and treatment of hypertensionAltern Ther Health Med201319Suppl 13249
- RajatSManishaSRobinSKumarSNutraceuticals: a reviewInt J Pharm2012349599
- KapoorASharfsteinJMBreaking the gridlock: regulation of dietary supplements in the United StatesDrug Test Anal201683–442443027072846
- ShanahanCJde LorimierRFrom science to finance – a tool for deriving economic implications from the results of dietary supplement clinical studiesJ Diet Suppl2016131163425166888
- MisterSHathcockJUnder the law, FDA must grant different standards for new dietary ingredients and food additivesRegul Toxicol Pharmacol201262345645822310217
- UmhauJCGargKWoodwardAMDietary supplements and their future in health care: commentary on draft guidelines proposed by the Food and Drug AdministrationAntioxid Redox Signal201216546146222181059
- FDA (Food and Drug Administration) [webpage on the Internet]Draft guidance for industry: dietary supplements: new dietary ingredient notifications and related issues2011 Available from: http://www.fda.gov/regulatoryinformation/guidances/ucm257563.htmAccessed August 22, 2016
- Institute of Medicine (US) Food ForumThe Human Microbiome, Diet, and Health: Workshop SummaryWashington, DCNational Academies Press (US)2013
- TalatiARNew dietary ingredient notifications: a comprehensive review and strategies for avoiding FDA objectionsFood Drug Law J200762238739817632968
- BealBRWallaceMSAn overview of pharmacologic management of chronic painMed Clin North Am20161001657926614720
- JamisonRNMaoJOpioid analgesicsMayo Clin Proc201590795796826141334
- CandrilliSDDavisKLIyerSImpact of constipation on opioid use patterns, health care resource utilization, and costs in cancer patients on opioid therapyJ Pain Palliat Care Pharmacother200923323124119670020
- NelsonADCamilleriMChronic opioid induced constipation in patients with nonmalignant pain: challenges and opportunitiesTherap Adv Gastroenterol201584206220
- WanYCormanSGaoXLiuSPatelHModyREconomic burden of opioid-induced constipation among long-term opioid users with noncancer painAm Health Drug Benefits2015829310226005516
- GaertnerJSiemensWCamilleriMDefinitions and outcome measures of clinical trials regarding opioid-induced constipation: a systematic reviewJ Clin Gastroenterol201549191625356996
- JonesRPrommerEBackstedtDNaloxegol: a novel therapy in the management of opioid-induced constipationAm J Hosp Palliat Care Epub201576
- DonnellySWalshDRybickiLThe symptoms of advanced cancer: identification of clinical and research priorities by assessment of prevalence and severityJ Palliat Care19951112732
- WeitznerMAMoodyLNMcMillanSCSymptom management issues in hospice careAm J Hosp Palliat Care1997141901959295429
- VainioAAuvinenAPrevalence of symptoms among patients with advanced cancer: an international collaborative studyJ Pain Symptom Manage1996123108718910
- HatswellAJVegterSMeasuring quality of life in opioid-induced constipation: mapping EQ-5D-3 L and PAC-QOLHealth Econ Rev20156114
- BellTAnnunziataKLeslieJBOpioid-induced constipation negatively impacts pain management, productivity, and health-related quality of life: findings from the National Health and Wellness SurveyJ Opioid Manag20095313714419662923
- DornSLemboACremoniniFOpioid-induced bowel dysfunction: epidemiology, pathophysiology, diagnosis, and initial therapeutic approachAm J Gastroenterol2014213137
- González CangaAFernández MartínezNSahagún PrietoAMDietary fiber and its interaction with drugsNutr Hosp201025453553920694287
- StanghelliniVBellacosaLCogliandroRFiber and macrogol in the therapy of chronic constipationMinerva Gastroenetrol Dietol2013592217230
- SlavinJLPosition of the American Dietetic Association: health implications of dietary fiberJ Am Diet Assoc2008108101716173118953766
- DethlefsenLMcFall-NgaiMRelmanDAAn ecological and evolutionary perspective on human-microbe mutualism and diseaseNature2007449716481181817943117
- LeyREHamadyMLozuponeCEvolution of mammals and their gut microbesScience200832058831647165118497261
- TapJMondotSLevenezFTowards the human intestinal microbiota phylogenetic coreEnviron Microbiol200911102574258419601958
- BlacklerRWGemiciBMankoAWallaceJLNSAID-gastroenteropathy: new aspects of pathogenesis and preventionCurr Opin Pharmacol201419111624929967
- MontenegroLLosurdoGLicinioRNon steroidal anti-inflammatory drug induced damage on lower gastro-intestinal tract: is there an involvement of microbiota?Curr Drug Saf20149319620424809527
- MatsuiHShimokawaOKanekoTNaganoYRaiKHyodoIThe pathophysiology of non-steroidal anti-inflammatory drug (NSAID)-induced mucosal injuries in stomach and small intestineJ Clin Biochem Nutr201148210711121373261
- Remington-HobbsJPettsGHarrisTEmergency department management of undifferentiated abdominal pain with hyoscine butyl-bromide and paracetamol: a randomised control trialEmerg Med J2012291298999422307926
- SavoiaGColuzziFDi MariaCItalian intersociety recommendations on pain management in the emergency setting (SIAARTI, SIMEU, SIS 118, AISD, SIARED, SICUT, IRC)Minerva Anestesiol201581220522524847740
- NCD Risk Factor Collaboration (NCD-RisC)Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participantsLancet2016387100261377139627115820
- NarouzeSSouzdalnitskiDObesity and chronic pain: opportunities for better patient carePain Manag20155421721926072666
- OkifujiAHareBDThe association between chronic pain and obesityJ Pain Res2015839940826203274
- McVinnieDSObesity and painBr J Pain20137416317026516520
- HassanMKJoshiAVMadhavanSSAmonkarMMObesity and health-related quality of life: a cross-sectional analysis of the US populationInt J Obes2003271012271232
- ArranzLIRafecasMAlegreCEffects of obesity on function and quality of life in chronic pain conditionsCurr Rheumatol Rep201416139024264719
- RodriguezAEzquerroSMéndez-GiménezLBecerrilSFrühbeckGRevisiting the adipocyte: a model for integration of cytokine signaling in the regulation of energy metabolismAm J Physiol Endocrinol Metab20153098E691E71426330344
- WrightLJSchurENoonanCAhumadaSBuchwaldDAfariNChronic pain, overweight, and obesity: findings from a community-based twin registryJ Pain201011762863520338816
- ZdziarskiLAWasserJGVincentHKChronic pain management in the obese patient: a focused review of key challenges and potential exercise solutionsJ Pain Res20158637725709495
- MessierSPMihalkoSLLegaultCEffects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the idea randomized clinical trialJAMA2013310121263127324065013
- TanamasSKWlukaAEBerryPRelationship between obesity and foot pain and its association with fat mass, fat distribution, and muscle massArthritis Care Res (Hoboken)201264226226821972207
- AlbertazziPNon-estrogenic approaches for the treatment of climacteric symptomsClimacteric200710Suppl 211512017882686
- LuoSLanTLiaoWZhaoMYangHGenistein inhibits Aβ25–35-induced neurotoxicity in PC12 cells via PKC signaling pathwayNeurochem Res201237122787279422949092
- ValsecchiAEFranchiSPaneraiAERossiASacerdotePColleoniMThe soy isoflavone genistein reverses oxidative and inflammatory state, neuropathic pain, neurotrophic and vasculature deficits in diabetes mouse modelEur J Pharmacol20116502–369470221050844
- ValsecchiAEFranchiSPaneraiAESacerdotePTrovatoAECol-leoniMGenistein, a natural phytoestrogen from soy, relieves neuropathic pain following chronic constriction sciatic nerve injury in mice: anti-inflammatory and antioxidant activityJ Neurochem2008107123024018691380
- ShenCLSmithBJLoDFDietary polyphenols and mechanisms of osteoarthritisJ Nutr Biochem201223111367137722832078
- TallJMRajaSNDietary constituents as novel therapies for painClin J Pain2004201192614668652
- ZaheerKAkhtarMHAn updated review of dietary isoflavones: nutrition, processing, bioavailability and impacts on human healthCrit Rev Food Sci Nutr Epub20151113
- McFadyenIJChettyUSetchellKDZimmer-NechemiasLStanleyEMillerWRA randomized double blind-cross over trial of soya protein for the treatment of cyclical breast painBreast20009527127614732177
- Van PattenCLOlivottoIAChambersGKEffect of soy phytoestrogens on hot flashes in postmenopausal women with breast cancer: a randomized, controlled clinical trialJ Clin Oncol20022061449145511896091
- Wahner-RoedlerDLThompsonJMLuedtkeCADietary soy supplement on fibromyalgia symptoms: a randomized, double-blind, placebo-controlled, early phase trialEvid Based Complement Alternat Med2011201135069718990724
- ShirYRajaSNWeissmanCSCampbellJNSeltzerZConsumption of soy diet before nerve injury preempts the development of neuropathic pain in ratsAnesthesiology20019551238124411684996
- SatijaAAhmedSMGuptaRBreast cancer pain management – a review of current & novel therapiesIndian J Med Res2014139221622524718395
- ArjmandiBHKhalilDALucasEASoy protein may alleviate osteoarthritis symptomsPhytomedicine2004117–856757515636169
- ThomasAJIsmailRTaylor-SwansonLEffects of isoflavones and amino acid therapies for hot flashes and co-occurring symptoms during the menopausal transition and early postmenopause: a systematic reviewMaturitas201478426327624951101
- ZhaoCWacnikPWTallJMAnalgesic effects of a soy-containing diet in three murine bone cancer pain modelsJ Pain20045210411015042518
- EngelPANew onset migraine associated with use of soy isoflavone supplementsNeurology20025981289129012391374
- CalderPCMarine omega-3 fatty acids and inflammatory processes: effects, mechanisms and clinical relevanceBiochim Biophys Acta20151851446948425149823
- Lorente-CebriánSCostaAGNavas-CarreteroSZabalaMMartínezJAMoreno-AliagaMJRole of omega-3 fatty acids in obesity, metabolic syndrome, and cardiovascular diseases: a review of the evidenceJ Physiol Biochem201369363365123794360
- ParraDRamelABandarraNKielyMMartinezJAThorsdottirIA diet rich in long chain omega-3 fatty acids modulates satiety in overweight and obese volunteers during weight lossAppetite200851367668018602429
- ThomasTRLiuYLindenMARectorRSInteraction of exercise training and n-3 fatty acid supplementation on postprandial lipemiaAppl Physiol Nutr Metab200732347348017510682
- HillAMBuckleyJDMurphyKJHowePRCombining fish-oil supplements with regular aerobic exercise improves body composition and cardiovascular disease risk factorsAm J Clin Nutr20078551267127417490962
- HuertaAEPrieto-HontoriaPLSáinzNMartínezJAMoreno-AliagaMJSupplementation with α-lipoic acid alone or in combination with eicosapentaenoic acid modulates the inflammatory status of healthy overweight or obese women consuming an energy-restricted dietJ Nutr Epub201639
- KunesovaMBraunerovaRHlavatyPThe influence of n−3 polyunsaturated fatty acids and very low calorie diet during a short-term weight reducing regimen on weight loss and serum fatty acid composition in severely obese womenPhysiol Res200655637215857162
- BuckleyJDHowePRLong-chain omega-3 polyunsaturated fatty acids may be beneficial for reducing obesity-a reviewNutrients20102121212123022254005
- MoriTABurkeVPuddeyIBPurified eicosapentaenoic and docosahexaenoic acids have differential effects on serum lipids and lipoproteins, LDL particle size, glucose, and insulin in mildly hyperlipidemic menAm J Clin Nutr20007151085109410799369
- MoriTAWattsGFBurkeVHilmeEPuddeyIBBeilinLJDifferential effects of eicosapentaenoic acid and docosahexaenoic acid on vascular reactivity of the forearm microcirculation in hyperlipidemic, overweight menCirculation2000102111264126910982541
- MoriTAWoodmanRJThe independent effects of eicosapentaenoic acid and docosahexaenoic acid on cardiovascular risk factors in humansCurr Opin Clin Nutr Metab Care2006929510416477172
- TsitourasPDGucciardoFSalbeADHewardCHarmanSMHigh omega-3 fat intake improves insulin sensitivity and reduces CRP and IL6, but does not affect other endocrine axes in healthy older adultsHorm Metab Res200840319920518348080
- DerosaGCiceroAD’AngeloABorghiCMaffioliPEffects of n-3 pufas on fasting plasma glucose and insulin resistance in patients with impaired fasting glucose or impaired glucose toleranceBiofactors201642331632227040503
- EspositoKMarfellaRCiotolaMEffect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trialJAMA2004292121440144615383514
- RamelAMartinezAKielyMMoraisGBandarraNMThorsdottirIBeneficial effects of long-chain n−3 fatty acids included in an energy-restricted diet on insulin resistance in overweight and obese European young adultsDiabetologia2008511261126818491071
- AbeteIGoyenecheaEZuletMAMartínezJAObesity and metabolic syndrome: potential benefit from specific nutritional componentsNutr Metab Cardiovasc Dis201121Suppl 2B1B1521764273
- Lopez-AlvarengaJCEbbessonSOEbbessonLOTejeroMEVorugantiVSComuzzieAGPolyunsaturated fatty acids effect on serum triglycerides concentration in the presence of metabolic syndrome components. The Alaska-Siberia ProjectMetabolism2010591869219766268
- NestelPShigeHPomeroySCehunMAbbeyMRaederstorffDThe n−3 fatty acids eicosapentaenoic acid and docosahexaenoic acid increase systemic arterial compliance in humansAm J Clin Nutr20027632633012145002
- KabirMSkurnikGNaourNTreatment for 2 mo with n 3 polyunsaturated fatty acids reduces adiposity and some atherogenic factors but does not improve insulin sensitivity in women with type 2 diabetes: a randomized controlled studyAm J Clin Nutr20078661670167918065585
- MicallefMAGargMLThe lipid-lowering effects of phytosterols and (n−3) polyunsaturated fatty acids are synergistic and complementary in hyperlipidemic men and womenJ Nutr20081381086109018492838
- MicallefMMunroIPhangMGargMPlasma n-3 polyunsaturated fatty acids are negatively associated with obesityBr J Nutr20091021370137419454127
- JainAPAggarwalKKZhangPYOmega-3 fatty acids and cardiovascular diseaseEur Rev Med Pharmacol Sci201519344144525720716
- MunroIAGargMLDietary supplementation with n–3 PUFA does not promote weight loss when combined with a very-low-energy dietBr J Nutr201210881466147422214842
- BurrMLAshfield-WattPADunstanFDLack of benefit of dietary advice to men with angina: results of a controlled trialEur J Clin Nutr200357219320012571649
- ThompkinsonDKBhavanaVKanikaPDietary approaches for management of cardio-vascular health-a reviewJ Food Sci Technol201451102318233025328172
- Del GobboLCImamuraFAslibekyanSCohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Fatty Acids and Outcomes Research Consortium (FORCe)ω-3 polyunsaturated fatty acid biomarkers and coronary heart disease: pooling project of 19 cohort studiesJAMA Intern Med201617681155116627357102
- TavazziLMaggioniAPMarchioliRGissi-HF InvestigatorsEffect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trialLancet200837296451223123018757090
- YokoyamaMOrigasaHMatsuzakiMJapan EPA lipid intervention study (JELIS) InvestigatorsEffects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysisLancet200736995671090109817398308
- EstruchRRosESalas-SalvadóJPREDIMED Study InvestigatorsPrimary prevention of cardiovascular disease with a Mediterranean dietN Engl J Med2013368141279129023432189
- Sala-VilaAGuasch-FerréMHuFBDietary α-linolenic acid, marine ω-3 fatty acids, and mortality in a population with high fish consumption: findings from the PRevención con Dieta MEDiterránea (PREDIMED) StudyJ Am Heart Assoc201651e00254326813890
- LeafAAlbertCMJosephsonMPrevention of fatal arrhythmias in high-risk subjects by fish oil n−3 fatty acid intakeCirculation20051122762276816267249
- MozaffarianDFish, mercury, selenium and cardiovascular risk: current evidence and unanswered questionsInt J Environ Res Public Health2009661894191619578467
- CaloLBianconiLColivicchiFn−3 Fatty acids for the prevention of atrial fibrillation after coronary artery bypass surgery: a randomized, controlled trialJ Am Coll Cardiol2005451723172815893193
- DallongevilleJYarnellJDucimetierePFish consumption is associated with lower heart ratesCirculation2003108782082512912821
- Kris-EthertonPMHarrisWSAppelLJFish consumption, fish oil, omega-3 fatty acids, and cardiovascular diseaseCirculation20021062747275712438303
- Kris-EthertonPMInnisSAmerican Dietetic Association, Dietitians of CanadaPosition of the American Dietetic Association and Dietitians of Canada: dietary fatty acidsJ Am Diet Assoc200710791599161117936958
- GeleijnseJMGiltayEJGrobbeeDEDondersARKokFJBlood pressure response to fish oil supplementation: metaregression analysis of randomized trialsJ Hypertens20022081493149912172309
- HartwegJFarmerAJPereraRHolmanRRNeilHAMeta-analysis of the effects of n−3 polyunsaturated fatty acids on lipoproteins and other emerging lipid cardiovascular risk markers in patients with type 2 diabetesDiabetologia2007501593160217541540
- UeshimaHStamlerJElliottPINTERMAP Research GroupFood omega-3 fatty acid intake of individuals (total, linolenic acid, long-chain) and their blood pressure: INTERMAP studyHypertension200750231331917548718
- DullemeijerCDurgaJBrouwerIAn 3 fatty acid proportions in plasma and cognitive performance in older adultsAm J Clin Nutr20078651479148517991662
- van GelderBMTijhuisMKalmijnSKromhoutDFish consumption, n-3 fatty acids, and subsequent 5-y cognitive decline in elderly men: the Zutphen Elderly StudyAm J Clin Nutr20078541142114717413117
- NurkEDrevonCARefsumHCognitive performance among the elderly and dietary fish intake: the Hordaland Health StudyAm J Clin Nutr20078651470147817991661
- BeydounMAKaufmanJSSatiaJARosamondWFolsomARPlasma n-3 fatty acids and the risk of cognitive decline in older adults: the Atherosclerosis Risk in Communities StudyAm J Clin Nutr20078541103111117413112
- Freund LeviYVedinICederholmTTransfer of omega-3 fatty acids across the blood-brain barrier after dietary supplementation with a docosahexaenoic acid-rich omega-3 fatty acid preparation in patients with Alzheimer’s disease: the OmegAD studyJ Intern Med201427542843624410954
- Freund-LeviYEriksdotter-JonhagenMCederholmTOmega-3 fatty acid treatment in 174 patients with mild to moderate Alzheimer disease: OmegAD study: a randomized double-blind trialArch Neurol200663101402140817030655
- Freund-LeviYVedinIHjorthEEffects of supplementation with omega-3 fatty acids on oxidative stress and inflammation in patients with Alzheimer’s disease: the OmegAD studyJ Alzheimers Dis20144282383124934544
- QuinnJFRamanRThomasRGDocosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trialJAMA2010304171903191121045096
- ShintoLQuinnJMontineTA randomized placebo controlled pilot trial of omega-3 fatty acids and alpha lipoic acid in Alzheimer’s diseaseJ Alzheimers Dis20143811112024077434
- SamieriCFeartCLetenneurLLow plasma eicosapentaenoic acid and depressive symptomatology are independent predictors of dementia riskAm J Clin Nutr200888371472118779288
- MarcheselliVLMukherjeePKAritaMNeuroprotectin D1/protectin D1 stereoselective and specific binding with human retinal pigment epithelial cells and neutrophilsProstaglandins Leukot Essent Fatty Acids2010821273419931440
- LukiwWJCuiJGMarcheselliVLA role for docosahexaenoic acid-derived neuroprotectin D1 in neural cell survival and Alzheimer diseaseJ Clin Invest2005115102774278316151530
- EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS)Scientific opinion on the re-evaluation of curcumin (E 100) as a food additiveEFSA Journal2010891679
- AggarwalBBGuptaSCSungBCurcumin: an orally bioavailable blocker of TNF and other pro-inflammatory biomarkersBr J Pharmacol201316981672169223425071
- ChandranBGoelAA randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritisPhytother Res201226111719172522407780
- RamadanGEl-MenshawyOProtective effects of ginger-turmeric rhizomes mixture on joint inflammation, atherogenesis, kidney dysfunction and other complications in a rat model of human rheumatoid arthritisInt J Rheum Dis201316221922923773648
- ZhuXLiQChangRCurcumin alleviates neuropathic pain by inhibiting p300/CBP histone acetyltransferase activity-regulated expression of BDNF and cox-2 in a rat modelPLoS One201493e9130324603592
- ZhaoXXuYZhaoQChenCRLiuAMHuangZLCurcumin exerts antinociceptive effects in a mouse model of neuropathic pain: descending monoamine system and opioid receptors are differentially involvedNeuropharmacology201262284385421945716
- JiFTLiangJJLiuLCaoMHLiFCurcumin exerts antinociceptive effects by inhibiting the activation of astrocytes in spinal dorsal horn and the intracellular extracellular signal-regulated kinase signaling pathway in rat model of chronic constriction injuryChin Med J (Engl)201312661125113123506591
- HuXHuangFSzymusiakMLiuYWangZJCurcumin attenuates opioid tolerance and dependence by inhibiting Ca2+/calmodulin-dependent protein kinase II α activityJ Pharmacol Exp Ther2015352342042825515789
- HuXHuangFSzymusiakMTianXLiuYWangZJPLGA-curcumin attenuates opioid-induced hyperalgesia and inhibits spinal CaMKIIαPLoS One2016111e014639326744842
- KhopdeSMPriyadarsiniKIVenkatesanNRaoMNAFree radical scavenging ability and anti-oxidant efficiency of curcumin and its substituted analogueBiophys Chem19998028389
- HosseinzadehdehkordiMAdelinikATashakorADual effect of curcumin targets reactive oxygen species, adenosine triphosphate contents and intermediate steps of mitochondria-mediated apoptosis in lung cancer cell linesEur J Pharmacol201576920321026593433
- González-ReyesSGuzmán-BeltránSMedina-CamposONPedraza-ChaverriJCurcumin pretreatment induces Nrf2 and an antioxidant response and prevents hemin-induced toxicity in primary cultures of cerebellar granule neurons of ratsOxid Med Cell Longev2013201380148018
- LoneJChoiJHKimSWYunJWCurcumin induces brown fat-like phenotype in 3T3-L1 and primary white adipocytesJ Nutr Biochem20162719320226456563
- TeitenMHDicatoMDiederichMCurcumin as a regulator of epigenetic eventsMol Nutr Food Res20135791619162923754571
- AnandPKunnumakkaraABNewmanRAAggarwalBBBioavailability of curcumin: problems and promisesMol Pharm20074680781817999464
- ElSNKarakayaSOlive tree (Olea europaea) leaves: potential beneficial effects on human healthNutr Rev2009671163263819906250
- MollaceVRagusaSSaccoIThe protective effect of bergamot oil extract on lecitine-like oxyLDL receptor-1 expression in balloon injury-related neointima formationJ Cardiovasc Pharmacol Ther200813212012918413898
- Di DonnaLDe LucaGMazzottiFStatin-like principles of bergamot fruit (Citrus bergamia): isolation of 3-hydroxymethylglutaryl flavonoid glycosidesJ Nat Prod20097271352135419572741
- MollaceVSaccoIJandaEHypolipemic and hypoglycaemic activity of bergamot polyphenols: from animal models to human studiesFitoterapia201182330931621056640
- GliozziMWalkerRMuscoliSBergamot polyphenolic fraction enhances rosuvastatin-induced effect on LDL-cholesterol, LOX-1 expression and protein kinase B phosphorylation in patients with hyperlipidemiaInt J Cardiol2013170214014524239156
- MuscoliCLauroFDagostinoCOlea europaea-derived phenolic products attenuate antinociceptive morphine tolerance: an innovative strategic approach to treat cancer painJ Biol Regul Homeost Agents201428110511624750796
- LauroFIlariSGiancottiLAThe protective role of bergamot polyphenolic fraction on several animal models of painPharmaNutritionIn press2016
- SalveminiDLittleJWDoyleTNeumannWLRoles of reactive oxygen and nitrogen species in painFree Radic Biol Med201151595196621277369
- LauroFGiancottiLAIlariSInhibition of spinal oxidative stress by bergamot polyphenolic fraction attenuates the development of morphine induced tolerance and hyperalgesia in micePLoS One2016115e015603927227548