Abstract
Erythromelalgia (EM) is a rare disorder characterized by erythematous, warm, painful extremities, which is often precipitated by cold conditions. The pathophysiology of EM is incompletely understood. Recent investigations have identified sodium channelopathy as a genetic cause for this pain condition, classified as primary inherited EM. Other subtypes are idiopathic EM and secondary EM. The management of pain in EM is challenging as no single therapy has been found to be effective. There is varying response to pharmacotherapy and significant variability within this clinical population, resulting in a stepwise trial and error approach. Consequently, EM is often associated with poorer health-related quality of life with higher morbidity. There is currently no consensus or guidelines on management of pain in EM. This is a review of the literature on management of pain using pharmacologic, procedural intervention and nonpharmacologic treatment in children and adults with EM.
Introduction
Erythromelalgia (EM), previously also known as erythermalgia, was initially described in 1878 by Mitchell, with hallmark symptoms of red (erythros) limbs (melos) that are painful (algos).Citation1 This was subsequently subdivided into primary, idiopathic, and secondary forms in 1938 by Smith and Allen, reflecting our understanding of the polymorphic etiologies that may contribute to this disorder.Citation2 EM is a challenging condition to manage. There are several factors that have limited a systematic approach to management of the disease. First, the underlying pathophysiology remains poorly understood, thereby limiting intentional treatment of pain. Second, EM is a rare disorder, estimated to affect 0.36–2 per 100,000 people per year in the USA and Europe,Citation3–Citation5 making it a difficult subject of research. Finally, the trajectory of symptoms and the long-term prognosis for patients are not well understood. Although there are promising studies that may provide clarity for the future interventions, therapies currently available remain unfortunately ineffective for many patients.
The classic presentation of EM is the triad of severe paroxysmal burning pain, erythema, and increased skin temperatures in the extremities.Citation6,Citation7 There are isolated reports of facial, auricular and genital involvement.Citation8–Citation10 EM can present at any age with onset commonly reported in the first decade of life, although it is most often diagnosed in the fifth and sixth decades.Citation11 Pain is exacerbated by increased ambient temperatures, exercise, and limb dependence. Relief is often achieved using cooling strategies such as immersion of limbs in ice-cold water, application of cold socks/gloves, and decreasing ambient heat (eg, ventilation, fans). Profound complications from chronic cold exposure have been reported, including maceration, ulceration, windburn, hypothermia, and frostbite.Citation12 Infections, sepsis, and amputation have been linked to cold exposure.Citation13 The course of EM is variable, with exacerbations and remissions.Citation14,Citation15 Of critical impact is the persistent and severe nature of pain that has been found to impair physical, psychological, and social functioning, resulting in poorer quality of life, with higher rates of morbidity and mortality.Citation16
The etiology of EM is incompletely understood. Genetic research has identified a link between cases of inherited EM and mutations in the Nav1.7 sodium channel encoded by the SCN9A gene.Citation17,Citation18 Nav1.7 subtypes are preferentially expressed in sensory and sympathetic ganglia neurons, and mutations result in neuronal excitability by reducing current threshold and enhancing repetitive firing in dorsal root ganglia.Citation19,Citation20 These mutations have rarely been detected in sporadic or secondary cases. Patients with SCN9A mutations have been classified as primary inherited EM. The other category of primary EM has been denoted as idiopathic, describing sporadic cases where a specific genetic mutation has not or cannot be identified.
Neuropathological and microvascular functional changes are implicated the pathophysiology of the secondary forms of EM. Studies have identified neurogenic dysregulation of cutaneous sympathetic fibers and impaired function as a potentially causative finding in patients with EM.Citation21 Investigations such as thermoregulatory sweat testing and quantitative sudomotor axon reflex test supported the diagnosis of small fiber neuropathy in patients with EM.Citation22–Citation24 Other studies suggest vascular causes, with pain from chronic perfusion deficit and tissue ischemia.Citation25,Citation26
To date, there is no therapy that has demonstrated consistently high efficacy across individuals with EM, highlighted by the lack of consensus or guidelines on the treatment of EM. The aim of this study was to conduct a systematic review of pain treatment for EM and provide an update on treatment options. The published data are gathered from small case series, retrospective cohorts, case studies, and several randomized controlled trials (RCTs).
Methods
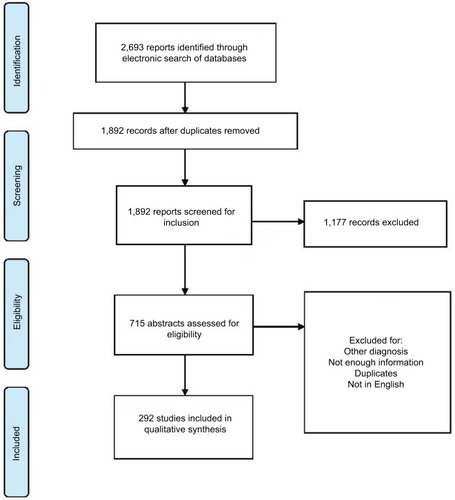
A literature search was performed using PubMed, Ovid, and Web of Science databases, yielding an initial total of 2,693 records. The search term was “erythromelalgia” in the title and as the MeSH term. The inclusion criteria were studies on EM, published after 1985 and in English.
After excluding duplicates (n=801), we identified 1,892 citations using the search criteria. Of the 1,892 citations, we excluded 1,177 that did not fulfill the inclusion criteria. From a review of the abstracts of the remaining 715 studies by SWT and MG, 296 were found eligible for inclusion based on the information provided in the abstract for treatment of pain in EM. Reasons for excluded citations were studies that were not relevant, other diagnosis not related to EM, and basic science reports. Of these 296 studies, full-text reports were assessed for eligibility, giving a final number of 292 relevant studies (). There were 5 RCTs, 1 non-RCT, 6 retrospective studies, 3 studies on nonpharmacologic management, 13 observational studies on EM, 29 case series, 178 case reports, and 57 review articles.
Results
This review will provide details on the pharmacologic, nonpharmacologic, and procedural interventions for pain management. Areas of intervention include trigger management, treatment of underlying pathophysiology, and symptomatic management of pain. The majority of the evidence was gathered from small case series studies, retrospective cohorts, or case reports.
Trigger management
Patients with EM often employ strategies to avoid situations that may precipitate pain (typically induced by heat) and the use of cold exposure reduction. Avoidance of heat includes being in cold ambient environments (air conditioning), limiting physical activities, avoiding footwear, and moving to colder environments. Patients repeatedly immerse their limbs in cold water and apply ice to the extremities. It is important to caution patients that impaired skin integrity and microcirculatory abnormalities from overexposure to water and cold can result in ulceration, maceration, and infections.Citation12,Citation27 Furthermore, there is a concern that patterns of increasing pain in EM may, in fact, be associated with the overuse of cooling strategies.Citation12 Therefore, patients need to be counseled on the appropriate use of cooling strategies, balancing tolerance of pain, and functional activities.
Pharmacotherapy
Many pharmacologic agents have been used to treat EM over the decades. Vascular agents (aspirin, prostaglandins), sodium channel blockers (lidocaine, mexiletine, carbamazepine, oxcarbazepine), antidepressants (tricyclic antidepressants, serotonin reuptake inhibitors), anticonvulsants, antihistamines, topical application of medications, and immunosuppressant drugs have been trialed with no single agent demonstrating complete efficacy, thereby resulting in polypharmacy for the majority of patients. These agents have been administered with the goal of targeting underlying etiology and/or for symptom management.
Aspirin/ticlopidine
Aspirin has been considered as a first-line treatment, likely due to early studies reporting its efficacy and the low side effect profile. There is more evidence that aspirin is effective for patients with associated thrombocythemia and polycythemia vera.Citation28,Citation29 It is hypothesized that this is secondary to its antiplatelet action. Caution should be exercised due to potential gastrointestinal side effects (eg, hemorrhages) of aspirin at high doses. Ticlopidine is an alternative agent that has been trialed and found to be better tolerated.Citation30
Nonsteroidal anti-inflammatory agents
There appears to be a limited role for nonsteroidal anti-inflammatory drugs other than aspirin in the treatment of EM. Piroxicam has been documented as effective in cases of aspirin allergy,Citation31 and indomethacin has been used for cases of facial or auricular EM due to its ability to penetrate the blood brain barrier and its potential role in reducing facial parasympathetic outflow.Citation32
Prostaglandins
Sympathetic dysfunction, arteriovenous shunting of the skin, insufficient perfusion, and tissue hypoxia have been proposed to contribute to pain in EM.Citation33 Prostaglandin and prostacyclin analogs with vasodilatory effects have been the subjects of two small RCTs in EM treatment of pain (n=12–21). Findings were that iloprost and misoprostol were associated with a reduction in symptoms and sympathetic dysfunction.Citation7,Citation34,Citation35
Sodium channel blockers
Drugs that target the underlying genetic cause of cases of hereditary EM (Nav1.7 sodium channel) have proved promising in the preclinical setting. Two proof-of-concept RCTs showed that agents developed specifically to antagonize the abnormal Nav1.7 sodium channel improved symptoms and neurophysiologic markers in patients with an identified SCN9A mutation.Citation36,Citation37 However, these agents are yet to be available in clinical practice.
Lidocaine and mexiletine provide nonselective partial blockade of voltage-gated sodium channels, working on segment 6 of domain IV of the alpha subunit to shorten the action potential duration. Lidocaine is an amide-type local anesthetic agent that stabilizes neuronal membranes by inhibiting the ionic fluxes required for the initiation and conduction of impulses. Lidocaine has been used in the treatment of EM on a trial basis.Citation38–Citation40 However, lidocaine has a narrow therapeutic window with significant cardiac, cognitive, and motor side effects. Further research has also identified that different genetic EM mutations may be responsible for the varying responses of individuals with hereditary EM to lidocaine treatment. Therefore, identifying the specific SCN9A genotype may provide guidance on treatment.Citation41,Citation42 Due to limited availability of genetic testing, current approach to the use of lidocaine may involve a trial and error strategy.Citation43
Positive response to lidocaine infusions has been considered as an indicator of success with mexiletine, an orally available form of lidocaine. Mexiletine has been documented to reduce pain episodes in case reports of children and adults.Citation44–Citation47 However, similar to lidocaine, there is variable clinical response that may be also explained by the genetic polymorphisms in Nav1.7 mutations, some of which may have a stronger response to lidocaine and mexiletine than others.Citation48
Carbamazepine and oxcarbazepine are also often utilized as first-line agents due to their mechanism of action on inactivation of sodium channel subtypes, including Nav1.7. They reduce the excitability of sensory and sympathetic neurons. Carbamazepine has not been found to have significant effects on pain in EM. However, there is some evidence suggesting that individuals who carry a specific mutation on the Nav1.7 sodium channel (V400M) may be more responsive to carbamezepine.Citation49–Citation51 Oxcarbazepine has been used in inherited EM. It has been found to be better tolerated by patients compared to carbamazepine.Citation49
Calcium channel blockers
Calcium channel antagonists have been proposed for use to attenuate the vasoconstriction and reactive hyperemia in EM. Amlodipine, nifedipine, and diltiazem have been utilized with isolated reports of remission.Citation52 Use of high-dose oral magnesium has been reported in 12 patients recruited via an informal survey through The Erythromelalgia Association. Of these patients, 61.5% reported varying degrees of improvement. Two patients’ dose titration was limited by diarrhea as an adverse effect.Citation52 In addition to calcium channel antagonism, magnesium was proposed to have sympatholytic and muscle relaxant qualities to account for potential efficacy.
Antidepressants
Various classes of antidepressants have been used. Selective serotonin and norepinephrine reuptake inhibitors such as fluoxetine, sertraline, and venlafaxine have also been used with reported remission.Citation53,Citation54 Serotonin antagonists such as methysergide and pizotifen have been tried with some reported effectiveness.Citation110,Citation111 These agents may affect vascular control by inhibition of serotonin reuptake and act on sympathetic fibers by inhibition of reuptake of noradrenaline. Data on tricyclic antidepressants (eg, amitriptyline, imipramine; SNRI, eg, duloxetine) are limited to case reports or series, often with variable responses and in conjunction with polypharmacy.Citation55
Anticonvulsants
Gabapentinoids such as gabapentin and pregabalin are commonly used to treat neuropathic pain. This has been extended for potential application in the neuropathic nature of pain described in EM. The hypothesized analgesic action involves the voltage-gated L-type calcium channels. Gabapentin has a well-established safety profile with the most common adverse effect being sedation, which may be self-limiting. Gabapentin has been used with variable success in the treatment of EM, often combined with other medications.Citation14,Citation49,Citation56 Pregabalin is a structural analog of gamma-aminobutyric acid, similar to gabapentin. It binds to the alpha 2 delta ligand of the voltage-gated calcium channels in the central nervous system that are proposed to exert its nociceptive and anticonvulsant activity. It appears to act as a presynaptic inhibitor of the release of excitatory neurotransmitters including glutamate, substance P, and calcitonin gene-related peptide. Common side effects are dizziness, somnolence, dry mouth, and weight gain. The case reports show that this has been used in EM with limited success.Citation57,Citation58 Both agents are started at a low dose and titrated to effect.
Antihistamines
Antihistamines may have potent vascular effects and may be considered for treatment. Cyproheptadine and pizotifen are antihistamines with serotonin antagonist effects at 5-HT2 receptors.Citation59 A survey of the members of The Erythromelalgia Association reported marked improvement in 40% of patients with antihistamine, but not in 60%.Citation55 This includes use of desloratadine, chlorpheniramine, and diphenhydramine. In contrast, non-sedating antihistamine cetirizine hydrochloride did not show improvement, except in a pediatric patient as shown by a case report.Citation60 It has been proposed that there may also be longstanding local allergic reaction in EM, for which antihistamines may have some efficacy.
Sodium nitroprusside
Sodium nitroprusside has been used to treat EM associated with hypertension in both adults and children.Citation61,Citation62 Hypertension has been reported in a large number of patients with EM. The proposed mechanism of the analgesic effect for sodium nitroprusside may be related to its mechanism of arteriolar vasodilation.
Topical agents
As the symptoms of EM appear to be localized, the topical route may be preferable to reduce the systemic effects of medications. Different compounds have been used, including topical amitriptyline-ketamine, lidocaine, capsaicin, and midodrine. In a retrospective case series of 32 adults prescribed amitriptyline-ketamine topical compound, over 70% had some or substantial relief of pain, with no adverse effects.Citation63 The penetration of topical lidocaine into intact skin was proposed to be sufficient to produce analgesic effect.Citation64,Citation65 Topical midodrine 0.2%, an alpha 1 agonist, was used for its vasoconstriction properties and was found to be successful in symptom reduction for 12 patients.Citation66 A single case report of capsaicin cream was identified, with reported success.Citation67
Immunosuppressant agents
There are a number of case reports and series on the use of immunosuppressants. One theory is that an autoimmune etiology and small fiber neuropathy may underlie EM. There are ongoing investigations to further determine whether there may be a subgroup classification of corticosteroid-responsive patients with EM, particularly in whom there were documented antecedent infections, trauma, or surgery as potential precipitants.Citation68 Several case reports have documented clinical recovery for patients with comorbid diagnoses of both small and large fiber neuropathy after treatment with intravenous immunoglobulin infusions, methylprednisolone, and oral corticosteroids.Citation43,Citation69–Citation71 The role of immunosuppressants in the treatment of EM remains unclear, with limited data and lack of clarity regarding the role of immune function in the development of EM.
Beta-blockers
Beta blockers have been used for EM, specifically to treat vulvar involvement.Citation8 Specific mechanisms were not proposed, except that nebivolol may have vasodilatory effects.
Nicotinic acid
Nicotinic acid has been used for mushroom poisoning; Paralepistopsis acromelalga, formerly known as Clitocybe acromelalga, is a rare poisonous mushroom. The mycotoxins in this mushroom cause symptoms resembling those of EM; however, its pathogenesis remains unclear.Citation72
Opioids
None of the case reports reviewed had reported opioids to be useful as a sole therapy. On the contrary, many studies report that opioids, even in combination with other medications, are not helpful in controlling the severe pain found in EM patients.Citation73 As there are risks (tolerance, sedation, respiratory depression, constipation) associated with chronic opioid use, caution must be exercised in its administration for neuropathic pain conditions.
Procedural interventions
Procedural interventions have been reported, and range from less-invasive techniques such as injection of botulinum toxin and sympathetic blockade to highly invasive procedures such as implantation of spinal cord stimulators. The reported cases are small in number, and these are primarily attempted in patients who were assessed as refractory to pharmacologic management.
Therapy with botulinum toxin type A with successful reduction in the episode and intensity of pain has been reported in one case report.Citation74 The mechanism of action of botulinum toxin is through inhibition of acetylcholine from the cholinergic nerve terminals, but this does not explain the analgesic activities. Proposed analgesic mechanism is through an inhibition of peripheral and central sensitization by blocking the release of proinflammatory neurotransmitters such as substance P and glutamate. Botulinum toxin has been trialed for diabetic neuropathic pain and trigeminal neuralgia, and its application in EM has been proposed as a potentially less invasive treatment modality.
There are several case reports of EM of lower extremity pain being treated with procedures targeting the thoracic and lumbar sympathetic system in adults and children. One hypothesis of pain in EM is that it is a result of tissue hypoxemia from abnormal microvascular blood flow, and that the pain may be sympathetically mediated; sympathetic blockade may ultimately increase tissue perfusion and relieve ischemic pain. These procedures are usually conducted in the setting of refractory cases, as there are increased risks of complications (unintentional tissue damage, neuritis, motor deficits). The types of interventions include epidural or sympathetic blocks, sympathectomy (chemical, radiofrequency ablation, surgical), and spinal cord stimulators. Epidural infusions of bupivacaine were reported to result in complete remission in two patients.Citation75,Citation76 For sympathetic blockade, different methods and agents (local anesthetics, phenol, corticosteroids, clonidine) have been used. Various methods of enhancing the success of blockade are recommended to increase the precision of the target, including fluoroscopy and computed tomography–guided procedures.Citation77–Citation80
There are three case reports of spinal cord stimulator implantation for refractory pain.Citation81–Citation83 This was conducted in patients with refractory pain and was considered after successful trial by placing percutaneous spinal cord stimulator electrodes in the epidural space. Several theories have been proposed for this: spinal cord stimulation selectively blocks a subgroup of C or Aδ fibers, and neuromodulation via activation of the Aβ fibers by gate control theory. Neurosurgical intervention was conducted in three pediatric patientsCitation112 who underwent stereotactic destruction of ventral posterolateral nucleus and centromedian nucleus. One patient demonstrated resolution from secondary EM with correction of multiple spinal cord malformations.Citation84
Nonpharmacologic intervention
Evidence-based treatment of chronic pain conditions includes a multidisciplinary approach. This is also recommended for pain related to EM. There are limited studies that have evaluated the impact of nonpharmacologic interventions.
The efficacy of an intensive pain rehabilitation program has been evaluated in eight adults with EM. There was a significant improvement in physical and emotional functioning, with a reduction in depressive symptoms and negative pain-related cognitions.Citation85 This suggested a potential role of a multidisciplinary rehabilitation approach focused on increasing functioning in various domains that may be significantly reduced in patients with severe pain experiences.
With regard to other nonpharmacologic interventions, there are limited studies. Single case reports have been published on pain reduction for patients through hypnosis, biofeedback treatment, and massage therapy.Citation86–Citation88
Discussion
There has been substantial advancement in the understanding of the pathophysiology underlying EM. However, research findings have yet to translate to clinical practice. With no consensus or established guidelines for treatment, the approach for this difficult-to-treat condition has been mostly by trial and error. Yet, there are aspects in the evaluation and management of EM that can be incorporated in order to provide a more systematic approach for patients.
First, establishing the diagnosis of EM may require further testing to rule out other differential diagnoses. There are no formal diagnostic criteria, and the diagnosis of EM is usually based on the hallmark symptoms of erythematous, warm, painful limbs precipitated by heat and relieved by cold conditions. Other conditions resembling clinical presentation need to be excluded. Second, screening may need to be undertaken for associated disease processes. Third, investigation of a potential genetic cause for EM may guide the choice of pharmacologic therapy. Fourth, a multidisciplinary approach should be adopted for treatment of pain. This should incorporate a detailed assessment of the impact of pain on self-care, physical activities, job and school attendance, psychosocial functioning, sleep, and participation in normative roles. Finally, it is important to engage the patient and family in physical and psychological therapies with the goal of optimizing function, in addition to pain reduction.
The diagnosis of EM is based on evaluation of the symptom profile and exclusion of other differential diagnosis. This may include myeloproliferative disorders, connective tissue diseases, malignancy, and peripheral neuropathy. Diagnoses that present with similar features include complex regional pain syndrome and Fabry disease.Citation89 There are some differences in patients with complex regional pain syndrome. In the majority of cases, there is unilateral limb involvement and cold stimuli will usually worsen the pain. As for Fabry disease, it is an X-linked lysosomal storage disorder due to α-galactosidase deficiency secondary to GLA gene mutation. Pain is an early symptom localized to the hands and feet with hyperalgesia or allodynia. This may be triggered by extremes of temperature. Laboratory testing for α-galactosidase can be conducted to rule out Fabry disease. There are also reports of EM symptoms secondary to drugs, and cessation of the offending agent has been reported to be associated with resolution of symptoms (). For secondary EM, documented associations include myeloproliferative diseases such as polycythemia vera, idiopathic thrombocytosis, or other conditions such as diabetes mellitus (). This has clinical significance as treatment of the underlying disease process may reduce EM symptomatology. Targeted specific therapy based on the pathophysiology of EM may be more effective, for example, aspirin may be more effective in patients with EM and polycythemia vera.
Table 1 Differential diagnoses of erythromelalgia
Table 2 Disorders reported to be associated with erythromelalgia
With the diagnosis of inherited EM, the exact genetic mutation may provide some guidance regarding medication management. Inherited EM is usually resistant to most pharmacologic therapies, and the genetic differences in the affected sodium channel may account for therapeutic inefficiency in certain individuals.Citation50 For this group of patients, detailed family history should be undertaken with the guidance of a genetic counselor to assess for potential inheritance. Family members should receive genetic counseling and evaluation for treatment.
Most patients with EM require multimodal pharmacotherapy, specifically targeting both pathophysiology and neuropathic pain. As there are variable responses to a wide range of therapeutic options and limited high-quality data, no universally effective treatment regimen has been established. This can result in a frustrating process of trial and error for the patient and treating team, while the patient suffers from severe pain episodes. Quite often, a combination of modalities may be required to provide effective management. A common starting point would be to trial agents with least risk and most likely efficacy. For the patient diagnosed with inherited EM, knowledge of underlying genetic mutation may allow specific sodium channel blockers as the first medication trial. If unknown, oxcarbazepine or carbamezepine may be initiated and titrated to maximum dose. If ineffective, lidocaine infusion may be considered, followed by mexiletine if it shows efficacy in pain reduction. Adjunct treatment with antidepressants and gabapentinoids may be added with the goal of treating central causes of pain. Other agents such as antihistamines that may have vascular mechanisms may be added to the regimen. A strategic approach would be to discontinue agents that do not have any efficacy, in order to avoid polypharmacy and the potential adverse effects of medication interactions. Finally, physical and occupational therapy, rehabilitation, and pain psychology treatment would also be recommended. Other functional domains such as sleep disturbances should also be addressed, including the use of pharmacotherapy and cognitive behavioral therapy, due to the bidirectional relationship between sleep and pain.
Limitations
There are several limitations of this review. First, there are no RCTs that evaluate for the efficacy of a single commercially available pharmacologic agent, or compared nonpharmacologic approaches. Second, the available studies have small sample sizes and are primarily composed of retrospective reviews and case reports. Third, there are limited reports on long-term outcomes. Finally, it is also unclear whether there are differences between pediatric and adult populations with regard to the etiology of EM and treatment outcomes. All these factors highlight the challenges of testing the impact of pharmacologic and/or nonpharmacologic treatment. There are opportunities for research in this area, including through collaborative consortiums to collectively gather data on this rare condition.
Conclusion
EM is a challenging condition to treat due to our lack of understanding of the pathomechanisms of the disease process. To date, treatment is a stepwise trial and error approach, and no single therapy has been found to be effective for any patient. In addition to partial responses, there is varying response to pharmacotherapy and significant variability within this clinical population to treatment. This may be due to the etiology of EM or the natural course of disease process. Therefore, incorporating a multidisciplinary approach to address pain and its significant negative impact across many domains of functioning may target the goals of improving function, in addition to pain reduction in this difficult-to-treat population. Numerous investigations have extended our understanding of the underlying mechanisms of EM. Most recently, Farrar et al identified acute axonal depolarization and ischemia that occurs with heat, providing an insight into underlying pathophysiology of EM.Citation90 Genetic evidence also supports investigative efforts to develop Nav1.7 blockers as a novel therapeutic strategy. These are undergoing clinical trials.Citation2,Citation91 Finally, advancement in electrophysiology, molecular modeling, thermodynamic analysis, and functional analyses profiling is improving our understanding of the molecular mechanisms underlying pain in EM.Citation51 These studies are much needed to address the pain and significant comorbidity in patients with EM.
Disclosure
The authors report no conflicts of interest in this work.
References
- MørkCKverneboKErythromelalgia—A Mysterious Condition?Arch Dermatol2000136340640910724206
- TangZChenZTangBJiangHPrimary erythromelalgia: a reviewOrphanet J Rare Dis201510112726419464
- AlhadadAWollmerPSvenssonAErikssonKFErythromelalgia: Incidence and clinical experience in a single centre in SwedenVasa2012411434822247059
- ReedKBDavisMDPIncidence of erythromelalgia: a population-based study in Olmsted County, MinnesotaJournal of the European Academy of Dermatology and Venereology2009231131518713229
- KalgaardOMSeemEKverneboKErythromelalgia: a clinical study of 87 casesJ Intern Med199724231911979350163
- HeidrichHFunctional vascular diseases: Raynaud’s syndrome, acrocyanosis and erythromelalgiaVasa2010391334120186674
- ParkerLKPonteCHowellKJOngVHDentonCPSchreiberBEClinical features and management of erythromelalgia: long-term follow-up of 46 casesClinical and Experimental Rheumatology201735808427494156
- JohnsonEIyerPEanesAZolnounDErythema and Burning Pain in the Vulva: A Possible Phenotype of ErythromelalgiaCase Rep Med201120113 Article ID 374167
- MesseguerFAgusti-MejiasAVilata CorellJJRequenaCAuricular erythromelalgia: report of a rare caseDermatol Online J20131916
- KhanSAffleckAPeriodic facial erythema in a patient with postural orthostatic tachycardia syndromeClin Exp Dermatol201843110010228976015
- Dib-HajjSDRushAMCumminsTRGain-of-function mutation in Nav1.7 in familial erythromelalgia induces bursting of sensory neuronsBrain200512881847185415958509
- DavisMDPImmersion foot associated with the overuse of ice, cold water, and fans: a distinctive clinical presentation complicating the syndrome of erythromelalgiaJ Am Acad Dermatol201369116917123768296
- KirbyRLErythromelalgia-not so benignArch Phys Med Rehabil198768389
- Cook-NorrisRHTollefsonMMCruz-InigoAESandroniPDavisMDDavisDMPediatric erythromelalgia: a retrospective review of 32 cases evaluated at Mayo Clinic over a 37-year periodJ Am Acad Dermatol201266341642321798623
- DavisMDPO’FallonWMRogersRSRookeTWNatural history of erythromelalgia - Presentation and outcome in 168 patientsArchives of Dermatology200013633033610724194
- FribergDChenTTarrGvan RijAErythromelalgia? A clinical study of people who experience red, hot, painful feet in the communityInt J Vasc Med201320132 Article ID 864961
- Dib-HajjSDYangYWaxmanSGGenetics and molecular pathophysiology of Na(v)1.7-related pain syndromesAdv Genet2008638511019185186
- McdonnellASchulmanBAliZInherited erythromelalgia due to mutations in SCN9A: natural history, clinical phenotype and somatosensory profileBrain201613941052106526920677
- DabbyRPain disorders and erythromelalgia caused by voltage-gated sodium channel mutationsCurr Neurol Neurosci Rep2012121768321984269
- TanakaBSNguyenPTZhouEYGain-of-function mutation of a voltage-gated sodium channel Na V 1.7 associated with peripheral pain and impaired limb developmentJournal of Biological Chemistry2017292229262927228381558
- ØrstavikKMørkCKverneboKJørumEPain in primary erythromelalgia—a neuropathic component?Pain2004110353153815288393
- GenebrieraJMichaelsJDSandroniPDavisMDPResults of computer-assisted sensory evaluation in 41 patients with erythromelalgiaClin Exp Dermatol201237435035422369570
- DavisMDPWeenigRHGenebrieraJWendelschafer-CrabbGKennedyWRSandroniPHistopathologic findings in primary erythromelalgia are nonspecific: Special studies show a decrease in small nerve fiber densityJ Am Acad Dermatol200655351952216908366
- OaklanderAErythromelalgia: Small-Fiber Neuropathy by Any Other Name?Pediatrics20051161293294
- DavisMDSandroniPRookeTWLowPAErythromelalgia: vasculopathy, neuropathy, or both? A prospective study of vascular and neurophysiologic studies in erythromelalgiaArch Dermatol20031391337134314568838
- DavisMDPSandroniPHarperCMNeurophysiologic and vascular studies in erythromelalgia: A retrospective analysisJournal of Investigative Dermatology1998110590
- ThamSWLiLEffraimPWaxmanSBetween fire and ice: refractory hypothermia and warmth-induced pain in inherited erythromelalgiaBMJ Case Rep20172017 bcr-2017-219486
- MichielsJJAspirin responsive erythromelalgia in JAK2-thrombocythemia and incurable inherited erythrothermalgia in neuropathic Nav1.7 sodium channelopathy: from Mitchell 1878 to Michiels 2017Expert Opin Orphan Drugs201752111129
- WilloughbySPearsonTCThe use of aspirin in polycythaemia vera and primary thrombocythaemiaBlood Rev199812112229597194
- RuggeriMCastamanGRodeghieroFIs ticlopidine a safe alternative to aspirin for management of myeloproliferative disorders?Haematologica1993781821
- CalderoneDCFinziETreatment of primary erythromelalgia with piroxicamJ Am Acad Dermatol19912411451461999514
- ChanTLHBeckerWJJogMIndomethacin-Responsive Idiopathic Red Ear Syndrome: Case Report and PathophysiologyHeadache201858230630829193054
- KalgaardOMClausenOPMellbyeOJHovigTKverneboKNonspecific Capillary Proliferation and Vasculopathy Indicate Skin Hypoxia in ErythromelalgiaArch Dermatol2011147330931421079053
- KalgaardOMørkCKverneboKProstacyclin Reduces Symptoms and Sympathetic Dysfunction in Erythromelalgia in a Double-blind Randomized Pilot StudyActa Derm Venereol200383644244414690340
- MørkCGöran SalerudEAskerCLKverneboKThe Prostaglandin E1 Analog Misoprostol Reduces Symptoms and Microvascular Arteriovenous Shunting in Erythromelalgia—A Double-Blind, Crossover, Placebo-Compared StudyJ Invest Dermatol2004122358759315086539
- GoldbergYPPriceNNamdariRTreatment of Nav1.7-mediated pain in inherited erythromelalgia using a novel sodium channel blockerPain20121531808522035805
- CaoLMcdonnellANitzscheAPharmacological reversal of a pain phenotype in iPSC-derived sensory neurons and patients with inherited erythromelalgiaSci Transl Med20168335ra356
- ElguetaFde La Cuadra-FontaineJCCledeLFierroCValderramaAErythromelagia: A Rare and Hard-to-Treat Condition: A 9-Year-Old Boy Responsive to Intravenous Lidocaine and Oral MexilitenePain Medicine201314231131223368881
- KuhnertSMPhillipsWJDavisMDLidocaine and mexiletine therapy for erythromelalgiaArch Dermatol1999135121447144910606048
- JakobACreutzfeldtRStaszewskiOWinterpachtABernerRHufnagelMPrimary Erythromelalgia in a 12-Year-Old Boy: Positive Response to Sodium Channel Blockers Despite Negative SCN9A MutationsKlinische Pädiatrie20122240530931222170168
- SheetsPLJacksonJOWaxmanSGDib-HajjSDCumminsTRA Na v 1.7 channel mutation associated with hereditary erythromelalgia contributes to neuronal hyperexcitability and displays reduced lidocaine sensitivityJ Physiol2007581Pt 31019103117430993
- HelåsTSagafosDKleggetveitIPPain thresholds, supra -threshold pain and lidocaine sensitivity in patients with erythromelalgia, including the I848Tmutation in Na V 1.7European Journal of Pain20172181316132528418213
- PaticoffJValovskaANedeljkovicSSOaklanderALDefining a Treatable Cause of Erythromelalgia: Acute Adolescent Autoimmune Small-Fiber AxonopathyAnesthesia & Analgesia2007104243844117242106
- IqbalJBhatMCharooBSyedWSheikhMBhatIExperience with oral mexiletine in primary erythromelalgia in childrenAnn Saudi Med200929431631819584578
- KuhnertSMPhillipsWJDavisMDPLidocaine and mexiletine therapy for erythromelalgiaArch Dermatol1999135121447144910606048
- NathanARoseJBGuiteJWHehirDMilovcichKPrimary Erythromelalgia in a Child Responding to Intravenous Lidocaine and Oral Mexiletine TreatmentPediatrics20051154e504e50715741349
- JangH-SJungDKimSA case of primary erythromelalgia improved by mexiletineBr J Dermatol2004151370871015377366
- VivasACEscandonJKirsnerRSRefractory erythromelalgia of the ears: response to mexiletineAm J Otolaryngol201132216817020392536
- NatkunarajahJAthertonDElmslieFMansourSMortimerPTreatment with carbamazepine and gabapentin of a patient with primary erythermalgia (erythromelalgia) identified to have a mutation in the SCN9A gene, encoding a voltage-gated sodium channelClin Exp Dermatol2009348e640e64219549232
- FischerTZGilmoreESEstacionMA novel Na v 1.7 mutation producing carbamazepine-responsive erythromelalgiaAnn Neurol200965673374119557861
- GehaPYangYEstacionMPharmacotherapy for pain in a family with inherited erythromelalgia guided by genomic analysis and functional profilingJAMA Neurol201673665966727088781
- CohenJSHigh-dose oral magnesium treatment of chronic, intractable erythromelalgiaAnn Pharmacother200236225526011847944
- RudikoffDJaffeIAErythromelalgia: Response to serotonin reuptake inhibitorsJ Am Acad Dermatol19973722812839270523
- FirminDRoguedasAMGrecoMTreatment of familial erythromelalgia with venlafaxineJournal of the European Academy of Dermatology and Venereology200721683683717567325
- CohenJSErythromelalgia: New theories and new therapiesJ Am Acad Dermatol200043584184711050591
- McgrawTKosekPErythromelalgia pain managed with gabapentinAnesthesiology19978649889909105243
- KakizakiAFujimuraTKambayashiYWatabeAAibaSSuccessful treatment of adult-onset erythromelalgia with steroid pulse and pregabalinCase Rep Dermatol20124324224623275767
- KalavaKRobertsCAdairJDRamanVResponse of primary erythromelalgia to pregabalin therapyJournal of Clinical Rheumatology201319528428523872544
- SakakibaraRFukutakeTKitaKHattoriTTreatment of primary erythromelalgia with cyproheptadineJ Auton Nerv Syst1996581-21211228740669
- Al-MinshawySMEl-MazaryA-AMAn Egyptian child with erythromelalgia responding to a new line of treatment: a case report and review of the literatureJ Med Case Rep2014816924568362
- ChanMKHTuckerATMaddenSGoldingCEAthertonDJDillonMJErythromelalgia: an endothelial disorder responsive to sodium nitroprussideArch Dis Child200287322923012193436
- ZsoyluSCoskunTSodium nitroprusside treatment in erythromelalgiaEur J Pediatr198414131851876698066
- PoteruchaTJMurphySLDavisMDPTopical amitriptyline combined with ketamine for the treatment of erythromelalgia: a retrospective study of 36 patients at mayo clinicJournal of Drugs in Dermatology20131230831023545913
- DavisMDPSandroniPLidocaine Patch for Pain of ErythromelalgiaArch Dermatol20021381171911790162
- DavisMDSandroniPLidocaine patch for pain of erythromelalgia: follow-up of 34 patientsArch Dermatol20051411320132116230578
- DavisMDPMorrCSWarndahlRASandroniPTopically Applied Midodrine, 0.2%, an α1 -Agonist, for the Treatment of ErythromelalgiaJAMA Dermatol201515191025102625946117
- MuhiddinKAGallenIWHarriesSPearceVRThe use of capsaicin cream in a case of erythromelalgiaPostgrad Med J1994708298418437824425
- Pagani-EstévezGLSandroniPDavisMDWatsonJCErythromelalgia: identification of a corticosteroid-responsive subsetJ Am Acad Dermatol201776350651128413058
- PfundZStankovicsJDecsiTIllesZChildhood steroid-responsive acute erythromelalgia with axonal neuropathy of large myelinated fibers: A dysimmune neuropathy?Neuromuscular Disorders2009191495219056270
- JacksonALOatesJAA Patient With Adult Erythermalgia: Evidence Suggesting an Autoimmune EtiologyAm J Med Sci2008335432032218414074
- MoodySPachecoSButlerIJKoenigMKSecondary Erythromelalgia Successfully Treated With Intravenous ImmunoglobulinJ Child Neurol201227792292322156790
- NakajimaNUedaMNicotinic acid treatment for Paralepistopsis acromelalga intoxication: assessment using magnetic resonance imagingClin Toxicol2016547597600
- ParkerLKPonteCHowellKJOngVHDentonCPSchreiberBEClinical features and management of erythromelalgia: long term follow-up of 46 casesClin Exp Rheumatol201735808427494156
- CostaAMeirelesJFestasMJGomesAAbreuPTherapeutic success with local botulinum toxin in erythromelalgiaPain Physician201417E658E66025247918
- D’AngeloRCohenITBrandomBWContinuous epidural infusion of bupivacaine and fentanyl for erythromelalgia in an adolescentAnesth Analg1992741421441734777
- StrickerLJGreenCRResolution of Refractory Symptoms of Secondary Erythermalgia With Intermittent Epidural BupivacaineReg Anesth Pain Med200126548849011561273
- KunduARafiqMWarrenPTobiasJErythromelalgia in the pediatric patient: role of computed-tomography-guided lumbar sympathetic blockadeJournal of Pain Research2016983784527799815
- CerciFBKapuralLYosipovitchGIntractable erythromelalgia of the lower extremities successfully treated with lumbar sympathetic blockJ Am Acad Dermatol2013695e270e27224124862
- BangYJYeoJSKimSOParkYHSympathetic Block for Treating Primary ErythromelalgiaKorean J Pain2010231555920552075
- ShigaTSakamotoAKoizumiKOgawaREndoscopic Thoracic Sympathectomy for Primary Erythromelalgia in the Upper ExtremitiesAnesthesia & Analgesia199988486586610195539
- MatzkeLLLamerTJGazelkaHMSpinal cord stimulation for treatment of neuropathic pain associated with erythromelalgiaReg Anesth Pain Med201641561962027512936
- GraziottiPJGouckeCRControl of intractable pain in erythromelalgia by using spinal cord stimulationJ Pain Symptom Manage1993875025047963776
- PatelNChenECucchiaroGThe complexity of pain management in patients with erythromelalgiaA A Case Rep20155915115326528699
- MoselDDRoslerDErythromelalgia presenting after neurosurgical intervention in a patient with multiple malformations of the spinal cordJ Am Acad Dermatol2011654e120e12221920230
- DurosaroODavisMDHootenWMKerkvlietJLIntervention for erythromelalgia, a chronic pain syndrome: comprehensive pain rehabilitation center, Mayo ClinicArch Dermatol20081441578158319075140
- PuttAMErythromelalgia-a case for biofeedbackNurs Clin North Am197813625630252715
- DicksKRizekPMassage therapy techniques as pain management for erythromelalgia: a case reportInt J Ther Massage Bodywork2010359
- ChakravartyKPharoahPDScottDGBarkerSErythromelalgia–the role of hypnotherapyPostgrad Med J19926879544461561190
- ChenZYeWJiaoSJDiagnosis of a pedigree with Fabry disease mimicking erythromelalgia: the utility of next-generation sequencing in a precision medicine perspectiveInternational Journal of Clinical and Experimental Medicine201691692316926
- FarrarMALeeMJHowellsJAndrewsPILinCSBurning pain: axonal dysfunction in erythromelalgiaPain201715890091128134657
- Dib-HajjSDGehaPWaxmanSGSodium channels in pain disorders: pathophysiology and prospects for treatmentPain2017158S97S10728240647
- EatonMMurphySErythromelalgia misdiagnosed as cellulitisCutis200575374015732433
- ClaytonCFadenHErythromelalgia in a twenty-year-old with infectious mononucleosisPediatr Infect Dis J1993121011028417413
- GuYChenFLiuTEarly detection of an epidemic erythromelalgia outbreak using Baidu search dataSci Rep2015511264926218589
- ZhengZMZhangJHHuJMLiuSFZhuWPPoxviruses isolated from epidemic erythromelalgia In chinaThe Lancet19883318580296
- RajaballyYAMortimerNJAcute neuropathy and erythromelalgia following topical exposure to isopropanolVet Hum Toxicol200446242514748412
- CimolaiNCimolaiTLErythromelalgia accompanying rosuvastatin-associated myopathyJ Dermatol Case Rep2009311321886718
- DrenthJPErythromelalgia induced by nicardipineBMJ1989298668715821582
- ThamiGPBhallaMDrug points: erythromelalgia induced by possible calcium channel blockade by ciclosporinBMJ2003326739591012714471
- AliARothnerAErythromelalgia secondary to verapamilHeadache201757168169
- DulonMRomiplostim-induced erythromelalgia in a patient with idiopathic thrombocytopenic purpuraBritish Journal of Dermatology200916148248219486002
- NanayakkaraPWvan der VeldtAASimsekSSmuldersYMRauwerdaJAVerapamil-induced erythermalgiaNeth J Med200765934935117954955
- DrenthJPMichielsJJvan JoostTVuzevskiVDVerapamil-induced secondary erythermalgiaBr J Dermatol199212732922941390176
- ConfinoIPasswellJHPadehSErythromelalgia following influenza vaccine in a child
- RabaudCBarbaudATrechotPFirst case of erythermalgia related to hepatitis B vaccinationJ Rheumatol19992612332349918272
- SaviucPDanelVNew syndromes in mushroom poisoningToxicol Rev200625319920917192123
- KurzrockRCohenPRParaneoplastic erythromelalgiaClin Dermatol199311173828339204
- HanJHLeeJBKimSJLeeSCWonYHYunSJParaneoplastic erythromelalgia associated with breast carcinomaInt J Dermatol201251787888022715841
- ProtopsaltisIDrossouAKatsantonisIBreast cancer presenting as paraneoplastic erythroderma: an extremely rare caseCase Rep Med20142014 Article ID 351065
- PepperHPrimary erythermalgia: report of a patient treated with methysergide maleateJAMA196820312106610675694372
- CohenJSErythromelalgia: new theories and new therapiesJ Am Acad Dermatol2000435 Pt 184184711050591
- KandelEIStereotactic surgery of erythromelalgiaStereotact Funct Neurosurg199054–5596100