Abstract
Purpose
To ascertain if optical biometry determination of axial length (AL) and intraocular lens (IOL) power is significantly different compared to ultrasound (US) biometry in cases with borderline signal-to-noise ratio (SNR).
Patients and methods
Sixty patients who had cataract and IOL Master biometry with borderline SNR (1.6–2.0) were included. A retrospective chart review was performed to compare data collected with optical biometry and US biometry in cataract cases with borderline SNR.
Results
Results showed that optical biometry IOL and AL measurements were not significantly different from the US measurements. Analysis also demonstrated good agreement between the two methods.
Conclusion
Our study suggests that, in cases of borderline quality data, IOL power and AL measurements with optical biometry are still useful in surgical planning and that additional US measurements may be used more as a corroborative tool.
Introduction
With an incidence of 53.7%, cataract remains a significant ophthalmic morbidity where surgical treatment continues to be the definitive treatment and active area of research.Citation1,Citation2 An increasing number of technologies have been introduced over time to assist in biometric measurement of the eye, further enhancing refractive accuracy and precision as an achievable quality metric.
Optical biometry has been one of the mainstay elements in biometry over the past two decades, essentially supplanting routine use of applanation and immersion-based ultrasound (US) for most cataract assessments.Citation3–Citation6 However, this technique has inherent limitations based on use of wavelengths in this region of the electromagnetic spectrum. Data quality for optical biometry is frequently diminished in cases of very dense cataracts and posterior subcapsular cataracts, and this can be quantified in the form of signal-to-noise ratio (SNR).Citation7–Citation9 Olsen et al reported a minimum difference in axial length (AL) between optical biometry and US at an SNR value of ≥2.1. They also found that the rate of error started increasing at SNR of 2.0 and reached its peak at approximately 1.3.Citation10 In these clinical scenarios, it is common to then rely on applanation or immersion US, which serves as either an adjunct or primary biometric device for surgical planning.Citation11 When optical biometry results in clear-cut poor quality data, US often is the only tool available, though this typically requires more time, human personnel power, extra training and a higher level of patient contact.Citation12–Citation19
What is less known is how different technologies compare when signal from the optical biometry is of borderline quality, which could result from poor patient fixation, high refractive error, dense media opacities or posterior subcapsular cataract.Citation20,Citation21 The objective of this study was to determine the differences in AL and recommended intraocular lens (IOL) power measured in the same eye with these methods when optical biometry yields borderline quality results.
Patients and methods
This retrospective medical record review research project was approved by the Institutional Review Board of Department of Veteran Affairs (VA) Puget Sound Health Care System, and the study protocol adhered to the tenets of the Declaration of Helsinki. Electronic medical records were searched for patients who underwent cataract surgery at a single hospital-based eye clinic after they received both optical biometry with the IOL Master (IOLMaster 500, Carl Zeiss Meditec, Dublin, CA, USA) and US biometry (Eyecubed, Ellex Inc., Minneapolis, MN, USA) prior to surgery. Since this is a low-risk retrospective study and all patients were de-identified prior to data analysis, the Institutional Review Board at VA Puget Sound has waived the need for informed consent (FWA00004617).
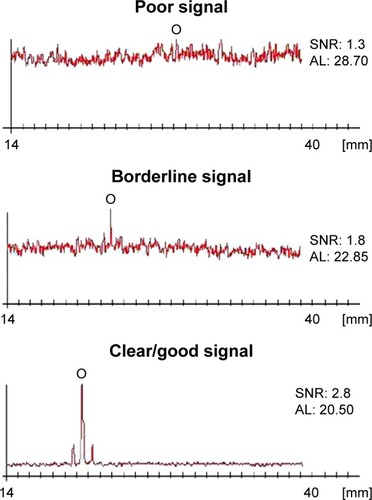
Patients who had IOL Master biometry with borderline SNR (1.6–2.0) were included, while patients with good SNR (>2.0), poor SNR (<1.6), and borderline SNR associated with non-physiologic AL values were excluded (). A total of 60 patients and 95 eyes were reviewed. Of the 22 patients who met the inclusion criteria, 25 eyes were analyzed for IOL power, while 27 eyes were analyzed for AL. All optical biometry and US scans were performed by the same two experienced personnel. Of note, these personnel separately took measurements on different eyes.
Figure 1 Different levels of signal quality resulting from optical biometry. Abbreviations: AL, axial length; SNR, signal-to-noise ratio.
The Holladay 1 IOL formula was used for comparison for each biometric unit with an identical surgeon factor. Additional analysis with the Hoffer Q (fixed identical peripheral anterior chamber depth [pACD]), SRK-T (fixed identical A constant) and average of all three formulae was also performed. The calculated IOL power for one single piece acrylic IOL (ZCB00, Abbott Medical Optics Inc., Santa Ana, CA, USA) in the capsular bag with a refractive target of −0.50 and the mean AL were then compared.
Statistical analysis was performed using SPSS version 24 (IBM Corporation, New York, NY, USA) with P<0.05 considered statistically significant.
Results
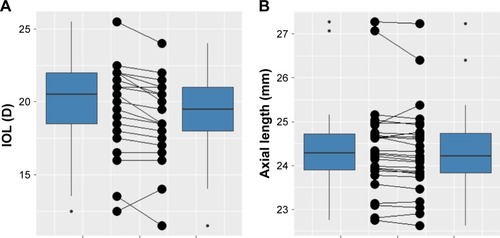
The mean AL for IOL Master was 24.391 mm, and the mean AL for US biometry was 24.336 mm. The mean difference of AL determination was 0.055 mm (95% CI, −0.013–0.1219). The mean difference of IOL power calculation between IOL Master and US biometry was 0.092 D (Holladay I), 0.204 D (Hoffer Q), 0.130 D (SRK-T) and 0.093 D (average of all three formulae) (). shows how the IOL power calculations obtained with IOL Master and US biometry compare side by side. shows how the AL measurements obtained with IOL Master and US biometry compare to each other. IOL Master AL measurements were not significantly different from US biometry measurements by 0.1 mm (P=0.1769) or by 0.03 mm (P=0.463) ().
Table 1 Mean, standard deviation and difference in mean of AL and IOL power from IOL Master and US biometry
Table 2 Paired t-test comparing mean of AL obtained from IOL Master and US biometry
Figure 2 Box plots comparing corresponding data obtained from IOL Master and US biometry.
Abbreviations: IOL, intraocular lens; US, ultrasound.
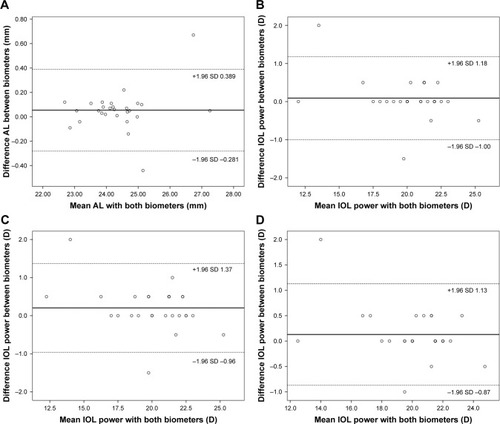
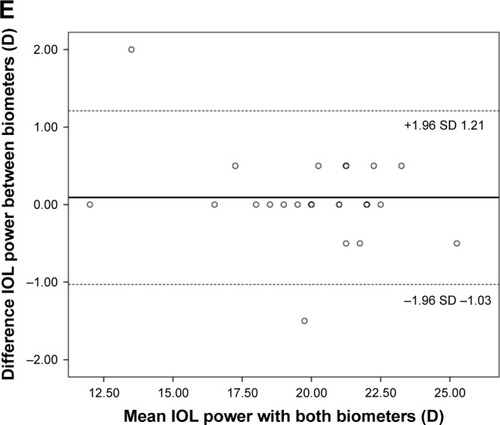
In addition, there was good correlation between biometry for AL (R=0.968) and IOL power calculation (R=0.987). The Bland–Altman plots in show the relationship between IOL Master and US biometry measurements for AL, as well as IOL power using Holladay I, Hoffer Q, SRK-T and the average of 3 formulae, with the variability around the mean appearing to be ±0.34, ±1.09, ±1.17, ±1.0, and ±1.12, respectively.
Figure 3 Bland–Altman Plots demonstrating the agreement between IOL Master and US biometry.
Abbreviations: IOL, intraocular lens; US, ultrasound.
Discussion
Optical biometry offers many distinct advantages compared to US-guided biometry. It is a non-contact approach with likely accuracy and reproducibility in the context of non-severe pathology. When limitations such as dense media opacity, high axial myopia, and/or poor fixation prevent use of optical biometry, US-guided biometry becomes a useful alternative method, as it can be used in cases with significant media opacity.Citation13–Citation16
In this study, we compared optical biometry and US biometry in cataract cases with borderline SNR (1.6–2.0) to better assist cataract surgeons in decision making. Similarly, there were no statistically significant differences in AL measurements between the two groups. We know from previous studies that optical biometry measurements are most reliable when SNR is >2.0, while SNR of ≤1.3 results in the largest variance between optical and US biometry.Citation10 However, little is established in literature for cases with borderline SNR. The results from this study help to determine that in such cases, optical biometry (IOL Master in particular) may still be utilized or, at the very least, clinically relevant when making IOL selections for a specific refractive target.
Even in cases where high-quality data is available, our results and literature also suggest that there is still room for improvement in order to achieve more precise postoperative refractive results. It is therefore still important to any discussion of cataract surgery that there may be a role for spectacles after surgery despite the array of treatments, technologies and formulae. A recent study in 2017 reported 49% of patients were still spectacle-dependent for distance after cataract extraction with IOL implant using the most advanced technologies to target emmetropia. In addition, there was a strong correlation between the use of spectacles post-operatively and surgeons’ advice to obtain them for optimal refractive outcome.Citation22
Precise and accurate biometric data is a fundamental requirement for successful refractive outcomes with cataract surgery. However, pathology often highlights technological related limitations where data of lower quality is the best available. Newer modalities including those utilizing Swept source-based technologies are being integrated to overcome the technological limitations of prior generation biometry.Citation23 Other fronts of improvement include intra-operative aberrometry where in vivo calculations can be used to corroborate pre-operative assessment for confirmation or modification of initial perioperative plans. These additional tools are most likely useful when there is general agreement among technologies.Citation24
For future purposes, additional review in the form of refractive outcomes from the surgery and post-operative axial length measurements would further elucidate the relative consistency between optical biometry and US as well as cataractous and non-cataractous states.
Conclusions
In conclusion, optical and US biometry compare favorably with no clinically significant difference in IOL power and axial length measurements when SNR is of borderline quality. Optical biometry still proves clinically useful in planning for such cases. Interestingly, and still an area of active interest, optical biometry can yield clinically significant refractive error even in some cases with good SNR. This suggests that appropriate discussion with patients on refractive target and post-operative spectacle use is necessary in every cataract case even as methods continue to improve.
Acknowledgments
This study was supported by an unrestricted grant from Research to Prevent Blindness Inc NYC to the University of Washington Department of Ophthalmology.
Disclosure
The authors report no conflicts of interest in this work.
References
- KleinBEKleinRLeeKEIncidence of age-related cataract over a 10-year interval: the Beaver Dam Eye StudyOphthalmology2002109112052205712414414
- CongdonNVingerlingJRKleinBEPrevalence of cataract and pseudophakia/aphakia among adults in the United StatesArch Ophthalmol2004122448749415078665
- Montés-MicóRCaronesFButtacchioAFerrer-BlascoTMadrid-CostaDComparison of immersion ultrasound, partial coherence interferometry, and low coherence reflectometry for ocular biometry in cataract patientsJ Refract Surg201127966567121323302
- FindlODrexlerWMenapaceRHeinzlHHitzenbergerCKFercherAFImproved prediction of intraocular lens power using partial coherence interferometryJ Cataract Refract Surg200127686186711408132
- DrexlerWFindlOMenapaceRPartial coherence interferometry: a novel approach to biometry in cataract surgeryAm J Ophthalmol199812645245349780097
- KolegaMŠKovačevićSČanovićSPavičićADBašićJKComparison of IOL – master and ultrasound biometry in preoperative intra ocular lens (IOL) power calculationColl Antropol201539123323526040097
- HirnschallNMurphySPimenidesDMaurinoVFindlOAssessment of a new averaging algorithm to increase the sensitivity of axial eye length measurement with optical biometry in eyes with dense cataractJ Cataract Refract Surg2011371454921071170
- FreemanGPesudovsKThe impact of cataract severity on measurement acquisition with the IOLMasterActa Ophthalmol Scand200583443944216029267
- PrinzANeumayerTBuehlWInfluence of severity of nuclear cataract on optical biometryJ Cataract Refract Surg20063271161116516857503
- OlsenTThorwestMCalibration of axial length measurements with the Zeiss IOLMasterJ Cataract Refract Surg20053171345135016105605
- RajanMSKeilhornIBellJAPartial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculationsEye200216555255612194067
- Velázquez-EstadesLJWangerAKellawayJHardtenDRPragerTCMicrobial contamination of immersion biometry ultrasound equipmentOphthalmology20051125e13e1815878049
- VerhulstEVrijghemJCAccuracy of intraocular lens power calculations using the Zeiss IOL master. A prospective studyBull Soc Belge Ophtalmol20012812816165
- RoseLTMoshegovCNComparison of the Zeiss IOLMaster and applanation A-scan ultrasound: biometry for intraocular lens calculationClin Exp Ophthalmol200331212112412648044
- BhattABScheflerACFeuerWJYooSHMurrayTGComparison of predictions made by the intraocular lens master and ultrasound biometryArch Ophthalmol2008126792993318625938
- GoebelsSCSeitzBLangenbucherAComparison of the new biometer OA-1000 with IOLMaster and Tomey AL-3000Curr Eye Res201338991091623841799
- GoebelsSCSeitzBLangenbucherAReproducibility of the optical Biometer OA-1000 (Tomey)Biomed Res Int2014201481476124818155
- GoebelsSPattmöllerMEppigTCaylessASeitzBLangenbucherAComparison of 3 biometry devices in cataract patientsJ Cataract Refract Surg201541112387239326703487
- LiampaZKynigopoulosMPallasGGerdingHComparison of two partial coherence interferometry devices for ocular biometryKlin Monbl Augenheilkd2010227428528820408075
- LegeBAHaigisWLaser interference biometry versus ultrasound biometry in certain clinical conditionsGraefes Arch Clin Exp Ophthalmol2004242181214648138
- OlsenTSources of error in intraocular lens power calculationJ Cataract Refract Surg19921821251291564648
- FarhoudiDBBehndigAMontanPLundströmMZetterströmCKugelbergMSpectacle use after routine cataract surgery: a study from the Swedish National Cataract RegisterActa Ophthalmol201896328328728857438
- SrivannaboonSChirapapaisanCChonpimaiPLoketSClinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometerJ Cataract Refract Surg201541102224223226703299
- WileyWFBafnaSIntra-operative aberrometry guided cataract surgeryInt Ophthalmol Clin2011512119129
