Abstract
Background
The purpose of this study was to compare the accuracy of the new Sirius® Scheimpflug anterior segment examination device for measurement of central corneal thickness (CCT) and anterior chamber depth (ACD) with that of CCT measurements obtained by ultrasound pachymetry and ACD measurements obtained by ultrasound biometry, respectively.
Methods
CCT and ACD was measured in 50 right eyes from 50 healthy subjects using a Sirius Scheimpflug camera, SP100 ultrasound pachymetry, and US800 ultrasound biometry.
Results
CCT measured with the Sirius was 546 ± 39 μm and 541 ± 35 μm with SP100 ultrasound pachymetry (P = 0.003). The difference was statistically significant (mean difference 4.68 ± 10.5 μm; limits of agreement −15.8 to 25.20 μm). ACD measured with the Sirius was 2.96 ± 0.3 mm compared with 3.36 ± 0.29 mm using US800 ultrasound biometry (P < 0.001). The difference was statistically significant (mean difference −0.40 ± 0.16 mm; limits of agreement −0.72 to 0.07 mm). When the ACD values obtained using ultrasound biometry were corrected according to the values for CCT measured by ultrasound, the agreement increased significantly between both technologies for ACD measurements (mean difference 0.15 ± 0.16 mm; limits of agreement −0.16 to 0.45 mm).
Conclusion
CCT and ACD measured by Sirius and ultrasound methods showing good agreement between repeated measurements obtained in the same subjects (repeatability) with either instrument. However, CCT and ACD values, even after correcting ultrasound ACD by subtracting the CCT value obtained with either technology should not be used interchangeably.
Introduction
Measurement of central corneal thickness (CCT) is a critical procedure in many clinical situations, including diagnosis and follow-up of corneal disease, evaluation before and after surgery, and assessment of corneal physiology.
Ultrasound pachymetry is widely recognized as the gold standard against which all other techniques should be compared, and attempts have been made to map peripheral corneal thicknessCitation1,Citation2 and corneal volumeCitation3 using this technology or new high-frequency ultrasound biomicroscopy.Citation4,Citation5 However, modern optical methods have the advantage of evaluating this parameter noninvasively, providing more information about corneal structure and morphology. Orbscan® and Pentacam® are two devices that obtain corneal thickness from the central 8–10 mm of the cornea using translational or rotational slit-scanning principles, respectively.Citation6,Citation7 Removal of the acoustic factor in Orbscan II improves the agreement with Pentacam for central measurements.Citation8 However, the accuracy of peripheral corneal thickness measurements obtained with Orbscan has been questioned in the literature.Citation6 Several studies have compared their measurements of CCTCitation9,Citation10 and some have even made a direct comparison in the corneal periphery.Citation11 Further, these systems can also measure other anterior ocular segment parameters, including anterior chamber depth (ACD) a critical parameter for intraocular lens implantation and other clinical assessments.Citation12,Citation13 The Sirius® (Costruzione Strumenti Oftalmici, Florence, Italy) is a new Scheimpflug imaging device that measures full corneal pachymetry and ACD.Citation14–Citation16 The aim of this study was to compare CCT and ACD measurements recorded using this new Scheimpflug corneal topographic system, using ultrasound methods as a reference.
Materials and methods
Subjects
CCT and ACD were measured in the right eyes of 50 volunteers (28 males, 22 females) of mean age 36.7 ± 4.8 (range 21–49) years using the Sirius Scheimpflug system and compared against ultrasound measurements obtained for CCT by the SP100 Handy pachymeter (Tomey, Nagoya, Japan) and for ACD by the US800 biometer (Nidek, Gamagori, Japan). The sample size was calculated based on average CCT values obtained using ultrasound pachymetry to achieve a statistical power of 80% with a significance level of 0.05.
Inclusion criteria were no corneal pathology or corneal scarring, no previous ocular surgery, and no concomitant ocular or systemic medication likely to induce changes in corneal thickness. None of the patients was wearing contact lenses at the time of the study. After the purpose and procedures used in the study were fully explained, each subject gave their informed consent. Data were collected at Opticlinic, a private clinic in Lisbon, Portugal.
Instruments and measurements
Three independent experienced examiners performed each of the techniques and all were masked as to the results of the previous tests. Sirius measurements were always performed first. After 5 minutes, an experienced examiner measured CCT with an ultrasound SP100 Handy pachymeter. After 5 minutes, another experienced examiner measured ACD with a US800 ultrasound biometer. One drop of 1% tetracaine hydrochloride was instilled before the pachymetric and biometric readings were taken. Following the manufacturer’s recommendations, three repeated measurements were taken consecutively and averaged. All instruments were calibrated before each measurement session using the test recommended by the manufacturer. To minimize the effect of diurnal corneal hydration changes on ultrasound speed, all measurements were performed in the afternoon between 2 pm and 6 pm.Citation17 All ultrasound measurements were obtained by the same trained examiners (JJ for ultrasound biometry and JMGM for corneal pachymetry).
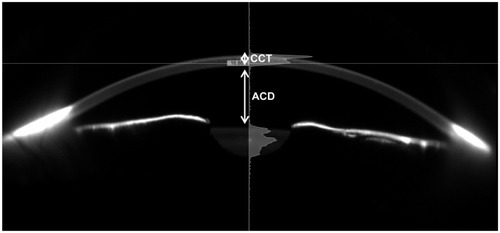
The Sirius is a new topographic device based on the principles of Scheimpflug photography. It consists of a combination of two rotating Scheimpflug cameras and a Placido disk, and allows full analysis of the topography and elevation of the anterior and posterior corneal surface and full corneal thickness (). ACD measurements with Sirius were obtained from the endothelium. All Sirius measurements were obtained by the same trained examiner (JLR).
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences version 19.0 (SPSS Inc, Armond, NY). Normality of the data distribution was evaluated using the Kolmogorov-Smirnov test. The parametric paired-samples t-test was used to explore statistical differences between mean ACD and CCT measurements obtained with both instruments. Repeated-measures analysis of variance was used to evaluate within-session repeatability. The 95% limits of agreement (95% LoA, mean of difference ± 1.96 × SD of the differences) were also calculated and plotted, as recommended by Bland and Altman.Citation18 Considering the different methods of measurement, it was expected that a better agreement between optical and ultrasound methods would be achieved by adding or subtracting CCT data from ACD values. Thus, agreement was re-evaluated after correcting ACD values measured with ultrasound by subtracting from them the CCT measured with ultrasound pachymetry and also by adding Sirius CCT to ACD to compare them with ACD values measured using ultrasound biometry. The level of statistical significance was set at α = 0.05.
Results
shows the mean values of CCT and ACD obtained by Sirius and the ultrasound instruments (SP100 and US800) for each of three consecutive readings. The mean of three repeated measurements obtained with each instrument was not significantly different from each individual value (analysis of variance, P > 0.800). shows the mean, standard deviation, maximum, and minimum values for the CCT and ACD measurements obtained with the Sirius and ultrasound devices. The values suggest an overestimation of ACD by the US800 relative to the Sirius. illustrates the difference between CCT measured using the Sirius and that measured by the SP100 ultrasound pachymeter. CCT measured with the Sirius was 546 ± 39 μm versus 541 ± 35 μm with SP100 ultrasound pachymetry (paired samples t-test, P = 0.003). The amplitude of the LoA interval for the difference (mean difference 4.68 ± 10.5 μm; LoA −15.8 to 25.20 μm) represents about 7.5% of the value obtained with Sirius and 7.6% of the average value obtained with ultrasound pachymetry. shows the differences between ACD measured with the Sirius compared with that using US800 biometry. ACD measured with the Sirius was 2.96 ± 0.3 mm versus 3.36 ± 0.29 mm with the US800 ultrasound pachymeter (paired samples t-test, P < 0.001). In this case, the difference was statistically significant (mean difference −0.40 ± 0.16 mm; LoA −0.72 to 0.07 mm), with the amplitude of the LoA interval representing 26.78% of the average ACD value obtained with the Sirius and 23.5% of the value obtained by ultrasound biometry.
Figure 2 Bland-Altman analysis of CCT values measured by ultrasound and Sirius®. Abbreviation: CCT, central corneal thickness.
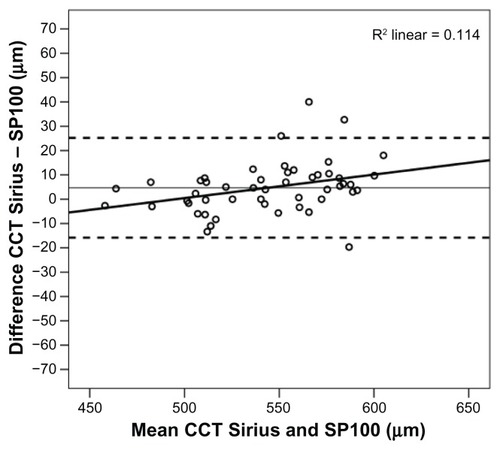
Figure 3 Bland-Altman analysis of ACD values measured with ultrasound biometry and Sirius® device.
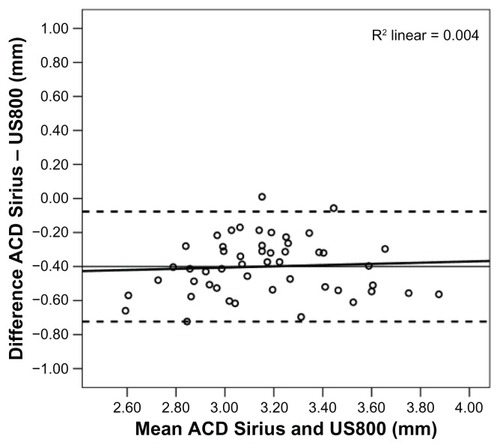
Table 1 Average values and standard deviation for central corneal thickness and anterior chamber depth measurements obtained with the ultrasound devices and Sirius® for three runs of measurements
Table 2 Average values, standard deviation, and range for central corneal thickness and anterior chamber depth measurements obtained with ultrasound and the Sirius®
When the ACD values obtained with ultrasound biometry were corrected according to the values for ultrasound CCT, the agreement increased significantly between both technologies (mean difference 0.15 ± 0.16 mm; LoA −0.16 to 0.45 mm), with amplitude of the LoA representing 18% and 20.6% of the ACD measured with ultrasound biometry and Sirius, respectively, as shown in and .
Figure 4 Bland-Altman analysis of ACD values measured with ultrasound biometry and Sirius® device by adding the value of CCT to the Sirius ACD value.
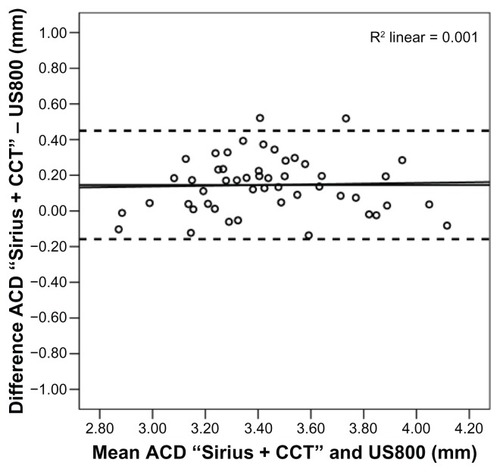
Figure 5 Bland-Altman analysis of ACD values measured with ultrasound biometry subtracting the value of CCT from the ultrasound biometric measure and Sirius® device.
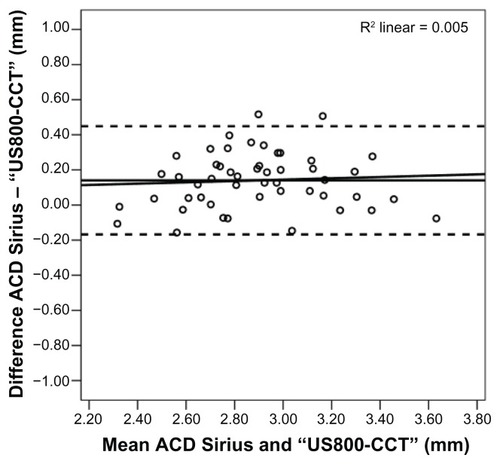
Average ACD measurements obtained by Sirius were 0.40 ± 0.16 mm lower (paired-samples t-test, P < 0.001) than measurements obtained by the US800 biometer (); after removing (or adding) the CCT value to that for the ACD, the Sirius® measurement was 0.15 ± 0.16 mm higher (paired-samples t-test, P < 0.001) than that obtained by the US800 pachymeter, as shown in and , respectively. These differences were not statistically significant.
Table 3 Mean difference, standard deviation, level of statistical significance, and limits of agreement between each set of measurement techniques to be compared at the 95% confidence interval
Discussion
Although Sirius and ultrasound CCT measurements showed good agreement between repeated measurements obtained in the same subjects with either instrument (ie, good repeatability), their measurements cannot be used interchangeably, given the amplitude of the LoA. Although no previous studies were found comparing the Sirius Scheimpflug device with ultrasound pachymetry, data similar to ours were found by several authors when comparing other Scheimpflug devices, such as the Pentacam® devices, with ultrasound pachymetry.Citation8,Citation19,Citation20 However, other authors have found significant differences in CCT measured using the Pentacam HR imaging system and ultrasound, which might be explained by the incorporation of corneas which were thicker than those used in our sample.Citation21 Furthermore, both the ultrasound pachymeters and Scheimpflug devices were different from those used in our study, which makes comparison with our study very difficult and should only be considered as a guide to the interpretation of other findings in the literature for similar but not identical devices. In this study, the agreement between measurements obtained using the Scheimpflug device and those obtained using ultrasonic pachymetry was good, and the repeatability was also good for both instruments independently, suggesting that Sirius is a clinical tool with less variability when performing serial measurements and follow-up examinations. However, a direct comparison between instruments will be needed before this conclusion could be confirmed.
Although there are no previous studies comparing the ACD with the Sirius directly, several authors report finding no difference in mean ACD measured with the Pentacam Scheimpflug and ultrasound devices.Citation20,Citation22 Nemeth et al reported a mean ACD of 2.87 ± 0.40 mm and 2.89 ± 0.49 mm for the Pentacam and ultrasound devices, respectively, analyzing healthy emmetropic phakic eyes.Citation22 In the present study, despite an apparent overestimation of ACD when measured with ultrasound or an underestimation when measured with Sirius, this is not a real effect. With the ultrasound technique, measurement of the ACD is obtained from the anterior surface of the cornea to the anterior surface of the lens, which includes the corneal thickness. The incorporation of corneal thickness into the ACD value produces an increase of about 0.5 mm in the real value of the ACD. ACD measured by the Scheimpflug technology in Sirius excludes corneal thickness from the measurement, making this measurement more reliable than that obtained by ultrasound biometry. Potential overestimation of ACD by the ultrasound device must be considered. Thus, even after correction, measurements from both instruments should not be used interchangeably, considering that the LoA for the difference is considerably wide, varying between −0.16 to +0.25, which might be relevant for decision-making in phakic intraocular lens implantation.
We also confirmed a moderate trend of an increase in the difference in measurements obtained by Sirius and the SP100 pachymeter as CCT increases (r2 = 0.114, P = 0.007). The plot of the difference versus the mean shows that for CCT values below 480 μm, the Sirius underestimates the corneal thickness compared with the SP100 pachymeter, and for CCT values greater than 480 μm, overestimates the corneal thickness. Sirius renders lower CCT values compared with ultrasound pachymetry for thinner corneas and higher CCT values for thicker corneas. Ultrasound biometry overestimates ACD measurements, because it includes CCT in the measurement. Subtraction of CCT from ultrasound biometry data is recommended in order to obtain more realistic values of ACD.
In summary, the present results provide relevant clinically significant information to consider, particularly with regard to comparison of ACD between the Sirius Scheimpflug anterior segment camera and ultrasound biometry. ACD values provided by Sirius exclude the CCT value, while ultrasound biometry requires removal of the CCT value to obtain a realistic ACD value. The noninvasive nature of Sirius is also an additional advantage.
Acknowledgment
The authors thank Paulo Martins from Opticlinic, Lisboa, Portugal, for allowing us to use the Sirius instrument.
Disclosure
The authors declare that they do not have any proprietary or financial interest in any of the materials mentioned in this paper. Part of the present work was presented at the XXII European Society of Cataract and Refractive Surgeons meeting held on September 17–21, 2011, in Vienna, Austria.
References
- ParafitaMAGonzalez-MeijomeJMDiaz-ReyJACorneal thickness mapping by topographical ultrasonic pachymetryInt Contact Lens Clin2000271221
- ParafitaMYebra-PimentelEGiraldezMJFurther information on the knowledge of topographical corneal thicknessInt Contact Lens Clin19992612813711166139
- CervinoAGonzalez-MeijomeJMFerrer-BlascoTDetermination of corneal volume from anterior topography and topographic pachymetry: application to healthy and keratoconic eyesOphthalmic Physiol Opt20092965266019821928
- ReinsteinDZArcherTJGobbeMStromal thickness in the normal cornea: three-dimensional display with Artemis very high-frequency digital ultrasoundJ Refract Surg20092577678619772263
- WadaIUltrasound biomicroscopic corneal thickness measurement for corneal thickness mappingJpn J Ophthalmol19974112189147182
- Gonzalez-MeijomeJMCervinoAYebra-PimentelEParafitaMACentral and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetryJ Cataract Refract Surg20032912513212551679
- YaziciATBozkurtEAlagozCCentral corneal thickness, anterior chamber depth, and pupil diameter measurements using Visante OCT, Orbscan, and PentacamJ Refract Surg20102612713320163077
- Gonzalez-PerezJGonzalez-MeijomeJMRodriguez AresMTParafitaMACentral corneal thickness measured with three optical devices and ultrasound pachometryEye Contact Lens201137667021301351
- LacknerBSchmidingerGPiehSRepeatability and reproducibility of central corneal thickness measurement with Pentacam, Orbscan, and ultrasoundOptom Vis Sci20058289289916276321
- HoTChengACRaoSKCentral corneal thickness measurements using Orbscan II, Visante, ultrasound, and Pentacam pachymetry after laser in situ keratomileusis for myopiaJ Cataract Refract Surg2007331177118217586372
- Gonzalez-PerezJGonzalez-MeijomeJMRodriguez AresMTParafitaMATopographic paracentral corneal thickness with pentacam and orbscan: effect of acoustic factorEye Contact Lens20113734835321983548
- AlfonsoJFFerrer-BlascoTGonzalez-MeijomeJMPupil size, white-to-white corneal diameter, and anterior chamber depth in patients with myopiaJ Refract Surg20102689189820027985
- HashemiHYazdaniKMehravaranSFotouhiAAnterior chamber depth measurement with a-scan ultrasonography, Orbscan II, and IOLMasterOptom Vis Sci20058290090416276322
- SaviniGBarboniPCarbonelliMHofferKJRepeatability of automatic measurements by a new Scheimpflug camera combined with Placido topographyJ Cataract Refract Surg2011371809181621852068
- SaviniGCarbonelliMSbregliaAComparison of anterior segment measurements by 3 Scheimpflug tomographers and 1 Placido corneal topographerJ Cataract Refract Surg2011371679168521855765
- MillaMPineroDPAmparoFAlioJLPachymetric measurements with a new Scheimpflug photography-based system: intraobserver repeatability and agreement with optical coherence tomography pachymetryJ Cataract Refract Surg20113731031621241914
- DuTRVegaJAFonnDSimpsonTDiurnal variation of corneal sensitivity and thicknessCornea20032220520912658083
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet198613073102868172
- NamSMImCYLeeHKKimEKKimTISeoKYAccuracy of RTVue optical coherence tomography, Pentacam, and ultrasonic pachymetry for the measurement of central corneal thicknessOphthalmology20101172096210320557940
- HashemiHMehravaranSRezvanFChanges in corneal thickness, curvature, and anterior chamber depth during the menstrual cycleCan J Ophthalmol201045677020130714
- ModisLSzalaiENémethGBertaAReliability of the corneal thickness measurements with the Pentacam HR imaging system and ultrasound pachymetryCornea20113056156621139499
- NemethGVajasAKolozsvariBBertaAModisLAnterior chamber depth measurements in phakic and pseudophakic eyes: Pentacam versus ultrasound deviceJ Cataract Refract Surg2006321331133516863970