Abstract
Purpose
To describe the clinical presentation of patients diagnosed with presumed latent ocular syphilis and congenital ocular syphilis at tertiary referral center in Turkey, and to compare the clinical findings with patients described in other studies, specifically focusing on demographics and co-infections.
Methods
This is a retrospective study reviewing the medical records of patients diagnosed with ocular inflammation between January 2012 and June 2014 at a tertiary referral center in Turkey. Ocular syphilis was diagnosed on the basis of non-treponemal and treponemal antibody tests, and cerebrospinal fluid analysis. All the patients diagnosed with ocular syphilis were tested for human immunodeficiency virus (HIV), Toxoplasma gondii, rubella, cytomegalovirus, and herpes.
Results
A total of 1,115 patients were evaluated between January 2012 and June 2014, and 12 patients (1.07%) were diagnosed with ocular syphilis based on the inclusion criteria. None of the patients were seropositive for HIV. Two patients were seropositive for T. gondii-specific IgG. Clinical presentations include non-necrotizing anterior scleritis, non-necrotizing sclerokeratitis, anterior uveitis, intermediate uveitis, posterior uveitis, panuveitis, and optic neuritis. All of the patients showed clinical improvement in the level of ocular inflammation with intravenous penicillin 24 million U/day for 10 days. Three patients received additional oral methotrexate as an adjunctive therapy. Two cases received low-dose trimethoprim–sulfamethoxazole.
Conclusion
Ocular syphilis is an uncommon cause of ocular inflammation in HIV-negative patients. Central retinochoroiditis is the most common ocular manifestation, and it is the most common cause of visual impairment. Ocular syphilis might present associated with co-infections such as T. gondii in developing countries. Oral methotrexate might be beneficial as an adjunctive therapy for ocular syphilis in resolving the residual intraocular inflammation and cystoid macular edema after specific therapy with intravenous penicillin.
Introduction
Syphilis is an infectious disease caused by the spirochete Treponema pallidum which is most often transmitted sexually in acquired disease or vertically during pregnancy in congenital syphilis (CS).Citation1,Citation2 Four stages have been described in acquired disease, and overlap can exist between the stages.Citation3,Citation4 The primary stage is characterized by a painless ulcerated lesion known as a chancre, which is thought to be the site of entrance into the host.Citation3 The secondary stage typically occurs 2 weeks to several months after infection and is associated with a skin rash on the palms of the hands and soles of the feet.Citation4 A period of latency can occur after the secondary stage, and recurrences often present during the 1st year after diagnosis.Citation5 Patients can remain in this stage indefinitely or develop tertiary syphilis.Citation5
During this stage, serious systemic manifestations occur, including cardiovascular and neurologic symptoms as well as gumma formation throughout the body.Citation6–Citation8 Ocular syphilis is considered to occur during any stage of infection, and it is known as “great masquerader”.Citation9 CS has been classified as early CS and late CS.Citation10 Early CS is characterized by organ involvements including liver, kidney, bone, and hematological and mucocutaneous manifestations.Citation10 Ocular manifestations including interstitial keratitis, chorioretinitis, salt–pepper fundus, glaucoma, cataract, and chancres of the eyelid have been mostly described in late CS.Citation11 Every patient with ocular inflammation is recommended to be tested for syphilis.Citation9 Since non-specific treponemal tests, including venereal disease research laboratory test (VDRL) and rapid plasma reagin test (RPR), normalize during the latent and tertiary stages, testing for syphilis should include both non-specific treponemal tests and specific treponemal antibody tests including fluorescent treponemal antibody absorption (FTA-ABS) and the microhemagglutination assay for T. pallidumCitation12 (MHA-TP). Treatment for presumed latent ocular syphilis is the same as for neurosyphilis, specifically 10–14 days of intravenous penicillin (IV PCN) 3–4 million units every 4 hours.Citation13 In this study, we describe the clinical presentation of patients diagnosed with presumed latent ocular syphilis and congenital late syphilis at a tertiary referral center in Turkey. We compare the clinical findings with patients described in other studies, specifically focusing on demographics and co-infections.
Materials and methods
This is a retrospective study reviewing the medical records of patients diagnosed with ocular inflammation between January 2012 and June 2014 at a tertiary referral center in Turkey. This study adheres to the tenets of Declaration of Helsinki. Institutional review board/ethics committee approval was obtained from the Dunya Goz Hospital, Ankara Turkey. Written informed consent was obtained for all individuals who enrolled in this study. The results of non-treponemal antibody tests VDRL and RPR, and specific FTA-ABS and MHA-TP, cerebrospinal fluid (CSF) FTA-ABS and CSF protein levels were analyzed. The diagnosis of presumed latent ocular syphilis and presumed congenital late syphilis was done according to the criteria described in the literature.Citation2,Citation13 All the patients diagnosed with presumed latent ocular syphilis and presumed congenital late syphilis were tested for human immunodeficiency virus (HIV) and TORCH (Toxoplasma gondii, rubella, cytomegalovirus, herpes). Clinical presentation, demographic information, and response to treatment were collected for each patient. Best corrected visual acuity (BCVA) was tested by using a Snellen chart. Snellen fractions of BCVA were converted to LogMAR. Intraocular pressure was measured by a using non-contact tonometer (NT-530, Nidek Co., Ltd., Gamagori, Japan). Slit-lamp biomicroscopy with SL-D7 (Topcon, Tokyo, Japan) and dilated fundus examination using an indirect ophthalmoscope (Keeler, West Berkshire, UK) were performed for all patients. Fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA), and spectral domain optical coherence tomography (SD-OCT) were done by Spectralis Heidelberg Research Architecture plus optical coherence tomography (HRA + OCT; Heidel-berg Engineering, Heidelberg, Germany). Visual field analysis was performed by Humphrey HFA II (Carl Zeiss Meditec AG, Jena, Germany). None of the patients had been treated for syphilis before admission to our clinic. In all, 4 (33.3%) of the 12 patients were receiving oral prednisone less than 3 months duration for their intraocular inflammation at presentation. None of the patients were on topical prednisolone acetate on admission. All of the patients received treatment with IV PCN 24 million U/day for 10 days. IV methylprednisolone for 3 days followed by high-dose oral prednisone was added to IV PCN treatment for the patient with papillitis. Oral methotrexate between 15 and 20 mg/week doses for 6 months was added to three patients 4 weeks after IV PCN therapy. Low-dose trimethoprim–sulfamethoxazole (trimethoprim, 160 mg plus sulfamethoxazole, 800 mg; one tablet twice daily, 2 days per week) as primary prophylaxis against T. gondii was given for 1 year for 2 patients who were seropositive for specific IgG for T. gondii.
Results
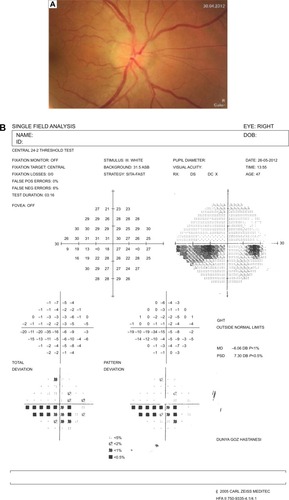
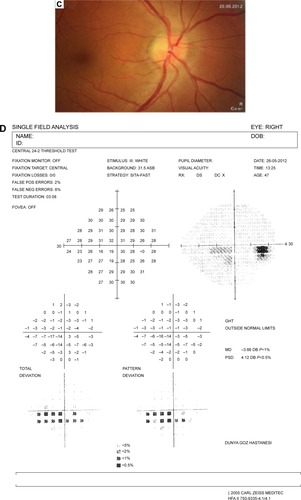
Medical records of 1,115 patients diagnosed with ocular inflammation were evaluated between January 2012 and June 2014. In all, 12 (1.07%) patients, 17 eyes were diagnosed with ocular syphilis. Briefly, 10 patients, 13 eyes had diagnosis of presumed latent ocular syphilis, and 2 patients, 4 eyes had diagnosis of presumed congenital late syphilis. Mean age at presentation was 43.75 years (range 8 and 67 years), and all of the patients were Caucasian. In all, 7 (58.3%) were male and 5 (41.7%) were female. Five (41.6%) patients had bilateral involvement. The initial BCVA of the patients were between 20/400 and 20/20 (0–1.3 LogMAR) with a mean LogMAR visual acuity of 0.3. None of the patients had elevated intraocular pressure (IOP). Demographics and clinical characteristics of the patients are summarized in . One (5.8%) eye had anterior scleritis (), one (5.8%) eye had sclerokeratitis (), and five (20.9%) eyes had non-granulomatous iridocyclitis that were resolved with frequent instillation of topical prednisolone acetate at the 10th day of PCN therapy ( and ). Two (11.7) eyes had intermediate uveitis, five (20.9%) eyes had posterior uveitis, two (11.7%) eyes had panuveitis, and one (5.8%) eye had papillitis SD-OCT of one of the eyes with intermediate uveitis disclosed cystoid macular edema (CME) with a foveal thickness of 693 μm associated with the retina pigment epithelial detachment (PED) and epiretinal membrane formation () that showed regression of CME and PED with a foveal thickness of 362 μm associated with persistence of epiretinal membrane at the 3rd month of the methotrexate (MTX) therapy (). The eyes with posterior uveitis had clinical manifestations of vitritis, branch retinal artery occlusion inferotemporally associated with vessel sheathing and intraretinal hemorrhages (), and focal chorioretinitis characterized by yellowish lesions with faded centers at the level of the pigment epithelium in the macula and paramacular region in both eyes of two patients (). Focal chorioretinitis was the most common posterior segment finding in our study (29.3%). FFA late phase of the left eye with vitritis and branch retinal artery occlusion disclosed venous staining, leakage, and areas of non-perfusion (). FFA early phase of right and left eyes of the patient with focal chorioretinitis disclosed staining at the macula and choroid in the posterior pole, intermediate phase revealed increased staining, and late phase disclosed persistence of staining at the posterior pole (). Indocyanine green angiography early phase of right and left eyes of the patient with focal chorioretinitis disclosed areas of hypofluorescence in the posterior pole, intermediate phase disclosed staining of choroid associated with areas of hypofluorescence, and late phase disclosed areas of hypo and hyperfluorescence associated with increased staining of choroid (). SD-OCT of right and left eyes of patient with focal chorioretinitis revealed CME with a right foveal thickness of 307 μm, and a left foveal thickness of 266 μm (). SD-OCT of right and left eyes of the second patient with focal chorioretinitis disclosed right foveal thickness of 126 μm, and left foveal thickness of 141 μm ().
Figure 1 Represents the color photo of the right eye at pre-treatment and post-treatment phases.
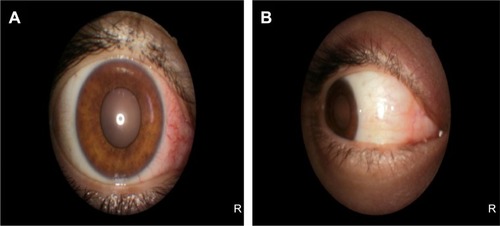
Figure 2 Represents the color photo of the left eye at pre-treatment and post-treatment phases.
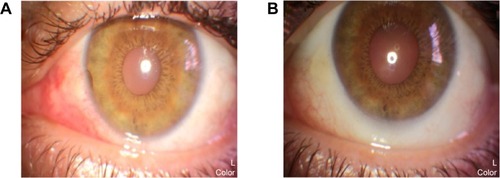
Figure 3 Represents the spectral domain optical coherence tomography of the left eye at pre-treatment and post-treatment phases.
Abbreviations: MTX, methotrexate; OS, left eye.
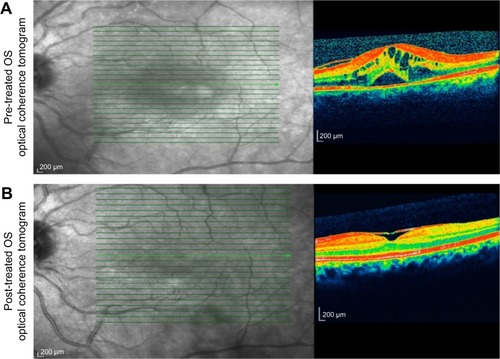
Figure 4 Represents the color fundus photo and fundus fluorescein angiography of the left eye at pre-treatment and post-treatment phases.
Abbreviations: MTX, methotrexate; OS, left eye.
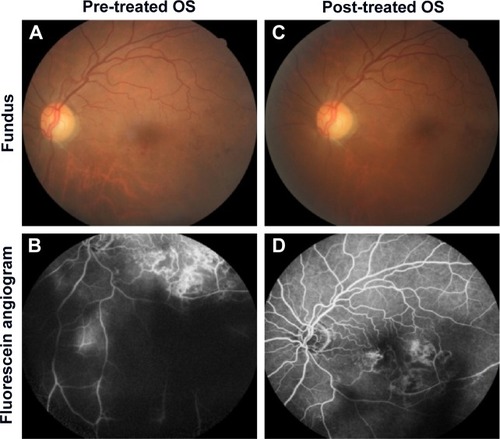
Figure 5 Represents the color fundus photos of the right and left eyes.
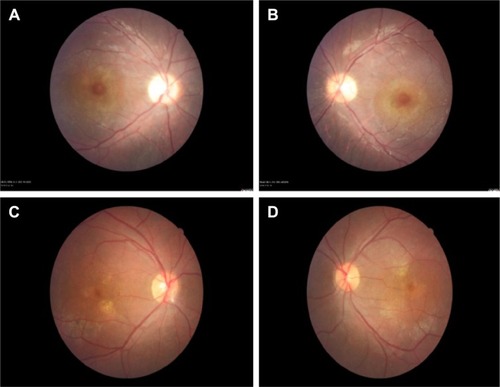
Figure 6 Represents the fundus fluorescein angiography of the right and left eye.
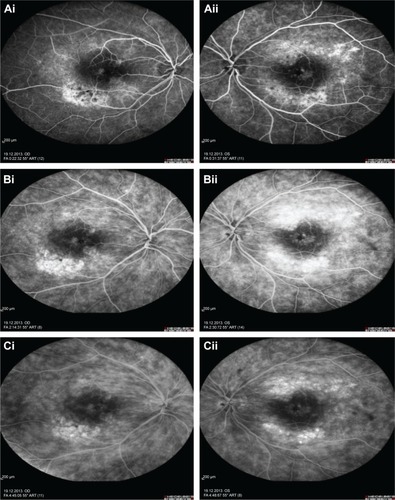
Figure 7 Represents the indocyanine green angiography of the right and left eye.
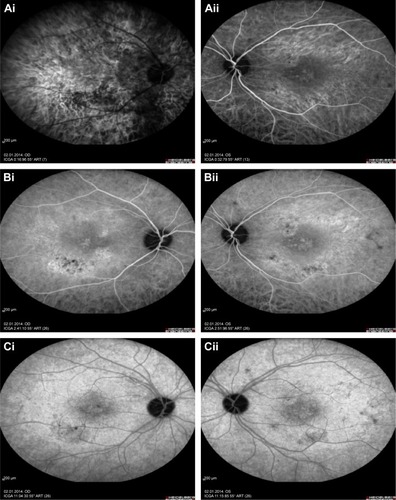
Figure 8 Represents the spectral domain optical coherence tomography of the right and left eyes at pre-treatment phase.
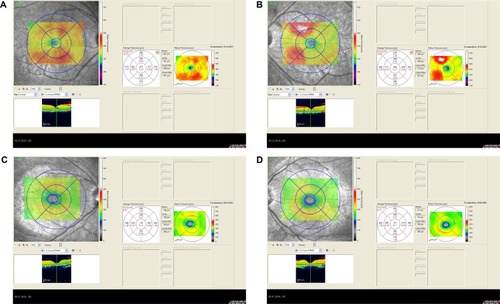
Table 1 Demographics and clinical characteristics of the cases
The resolution of vitritis and intraretinal hemorrhages associated with persistence of arterial sheathing inferotemporally was noted for the patient with vitritis and branch retinal artery occlusion OS at the 3rd month of the MTX therapy (). FFA late venous phase disclosed decreased areas of non-perfusion, vascular leakage, and staining associated with the areas of capillary occlusions inferotemporally (). SD-OCT foveal thickness measurements of two patients with focal chorioretinitis in right and left eyes remained stable with treatment disclosing right foveal thickness of 131 μm, and left foveal thickness of 147 μm for the first patient, and right foveal thickness of 368 μm, and left foveal thickness of 266 μm at the 6th month of the follow-up exam (). The eyes with panuveitis disclosed creamy-yellow superficial retinal accumulations and optic disc congestion (). FFA early phase showed increased choroidal fluorescence OU () and venous phase showed increased staining at the optic disc and bifurcation of the vessels OU (). The resolution of vitritis, the creamy-yellow superficial retinal accumulations and optic disc congestion were noted in right and left eyes of the patient with panuveitis at the 3rd month of the MTX therapy (). FFA arterial phase disclosed decreased choroidal fluorescence in right eye, and venous phase indicated the resolution of staining at the optic disc and bifurcations of the vessels in left eye (). Fundus examination of the patient with right papillitis disclosed 2+ hyperemia and 2+ swelling of the right optic disc (). Humphrey visual field analyzer 24-2 disclosed central scotoma and increased blind spot OD (). The resolution of optic disc congestion and edema OD with improvement of HVF 24-2 central scotoma in right eye at the 1st month of follow-up visit was noted for the patient with papillitis (). None of the patients were seropositive for HIV, and 2 (16.6%) of the 12 patients were seropositive for T. gondii-specific IgG antibody. The CSF FTA-ABS analysis of all cases was negative. Elevated CSF protein was found in 2 cases who were seropositive for T. gondii-specific IgG antibody.
Figure 9 Represents the spectral domain optical coherence tomography of the right and left eyes at post-treatment phase.
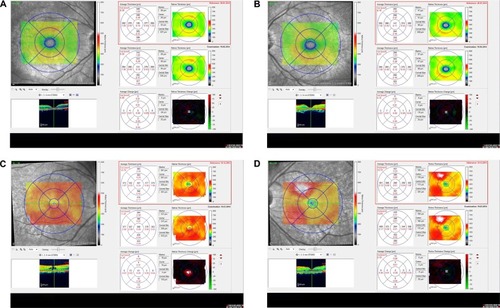
Figure 10 Represents the color fundus photo and fundus fluorescein angiography of the right and left eye at pre-treatment and post-treatment phases.
Abbreviations: MTX, methotrexate; OS, left eye; OD, right eye.
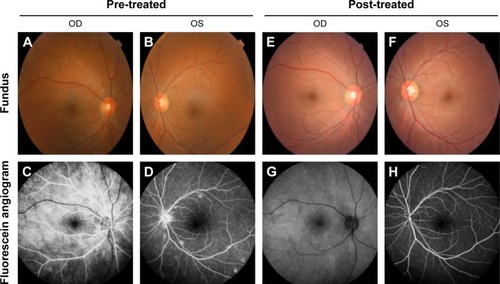
Figure 11 Represents the color fundus photo and Humphrey visual field 24-2 of the right eye at pre-treatment and post-treatment phases.
The patients who have received IV PNC only were followed-up 6 months to 2 years without recurrences. The patients who have received both IV PNC and oral MTX were followed-up 15–24 months period without recurrences. The final BCVA of the patients were between 20/50 and 20/20 (0.4–0.0 logMAR) with a mean LogMAR visual acuity of 0.06. Focal chorioretinitis was found as the most common cause of visual impairment.
Discussion
Syphilis is a sexually transmitted infection (STI) with a steady increase in the number of infected cases in the USA since the middle of 1980s.Citation14 A dramatic rise in incidence of primary and secondary syphilis in the USA has been reported from 2.1 per 100,000 people in 2000 to 4.5 per 100,000 in 2011.Citation15 The Centers for Disease Control and Prevention (CDC) has revealed that 72% of all primary and secondary syphilis cases occurred in men who have sex with men (MSM) in 2011 which has increased from 7% in 2000.Citation16 In a study of MSM presented to sexually transmitted disease (STD) clinics, a higher proportion of primary and secondary syphilis has been noted in cases co-infected with HIV (10.1%) than HIV-negative cases (2.6%).Citation17 Since 2001, threefold rise in incidence of syphilis and HIV infection in MSM have been reported in the age group of up to 25 years at the University Hospital of Dresen.Citation18 The strong association between ocular syphilis co-infection with HIV has been considered to be related to genital ulcerative diseases that facilitate HIV infection.Citation17 Our study disclosed the incidence of ocular syphilis among patients with ocular inflammation between January 2012 and June 2014 as 1.07%. There was no comparable study related to the incidence of ocular syphilis in Turkey. However, RPR seropositivity among the blood donors at the central blood bank of Turkey has been reported to increase from 0.04% in 1987 to 0.2% in 2002.Citation19 None of our cases were found seropositive for HIV. A low rate of HIV co-infection has also been reported in the first national seroprevalence survey in Saudi Arabia.Citation20 This might be related to the sexual behaviors of individuals living in mostly Muslim populations. A steady increase, approximately 15-fold in the incidence of ocular syphilis between 1999 and 2004, has also been reported in UK.Citation21 The British Ocular Syphilis Study (BOSS) has revealed a total of 41 new cases (63 eyes) of intraocular syphilis between 2009 and 2011 with an annual incidence of 0.3 per million UK adult population.Citation22 The mean age, sex distribution, and laterality of ocular involvement in BOSS were as 48.7 years, 90.2% male, and 56% bilateral involvement, respectively.Citation22 Our study disclosed the mean age as 43.8 years, 58.3% male, and 41.6% bilateral involvement that were compatible with the BOSS study. Syphilis is considered to display diverse ophthalmologic manifestations.Citation12,Citation23 A case series study of ocular syphilis in 18 eyes of 12 patients in a Singaporean population between 2004 and 2009 disclosed that anterior uveitis and panuveitis were reported two most common findings.Citation24 The other case series study including 22 patients with syphilitic uveitis followed at Singapore National Eye Center between 1995 and 2006 has revealed that non-granulomatous iridocyclitis was the most common finding (62.1%) at presentation followed by panuveitis (27.5%), posterior uveitis (13.7%), and intermediate uveitis (10.3%).Citation25 This study also disclosed that vitritis (65.4%) was the most common posterior segment finding.Citation25 The most common posterior segment finding in our study was found as posterior uveitis presenting as chorioretinitis rather than vitritis. In a study involving 35 eyes of 19 Chinese patients with syphilitic uveitis, posterior uveitis has been disclosed as the most common finding.Citation26 In a recent study from the USA involving 61 eyes of 35 patients, independent of HIV status panuveitis was reported as the most common presentation in ocular syphilis.Citation27 Our study disclosed that both non-granulomatous iridocyclitis (20.9%) and posterior uveitis (20.9%) were two most common presentations followed by panuveitis (11.7%) and intermediate uveitis (11.7%). Ocular syphilis was also reported to manifest as scleritis, episcleritis, or optic neuritis.Citation28
Non-necrotizing anterior scleritis (5.8%), non-necrotizing sclerokeratitis (5.8%), and optic neuritis (5.8%) were the least common findings in our study population. Since T. pallidum is a non-culturable bacteria, the diagnosis is considered to depend on mainly serological tests.Citation29 Three syphilis testing algorithms – traditional algorithm, reverse algorithm, and the European Centre for Disease Prevention and Control (ECDC) algorithm have been reported among the serological diagnostic tests.Citation29,Citation30 The traditional algorithm uses a non-treponemal test, VDRL or RPR for screening, and screen-reactive samples are tested by a treponemal assay such as MHA-TP of FTA-ABS for confirmation.Citation30 The reverse screening algorithm uses an automated, treponemal test such as enzyme immunoassay (EIA).Citation30 Samples that are reactive by EIA are then tested by RPR to assess disease and treatment status.Citation30 This technique allows clinical laboratories a rapid syphilis testing.Citation30 However, the results of EIA screening and RPR are often reported discordant such as reactive by EIA and non-reactive by RPR.Citation31 Centers for Disease Control and Prevention (CDC) recommends to perform MHA-TP to further analyze the discordant sera.Citation31 A non-reactive MHA-TP result suggests that the results of EIA screening are falsely reactive, while a reactive MHA-TP result supports either a past, successfully treated syphilis or late/latent syphilis.Citation32 The European Centre for Disease Prevention and Control algorithm uses a treponemal immunoassay that is followed by a second, different treponemal assay as a confirmatory test in high-prevalence populations.Citation32 We used the traditional algorithm for the serological diagnosis of syphilis in our study.
T. pallidum disseminates to the central nervous system within days after exposure.Citation33 Neurological involvement is reported to occur during any stage of the infection, and it is manifested as asymptomatic neurosyphilis, acute meningeal syphilis, meningovascular syphilis, paretic neurosyphilis, and tabetic neurosyphilis.Citation33,Citation34 Syphilis-specific CSF diagnostic tests including CSF VDRL, FTA-ABS, or PCR for T. pallidum DNA are recommended whenever any additional signs of neurosyphilis such as headache, hypoacusis, tinnitus, cranial nerve abnormalities, and motor and sensory symptoms occur.Citation35 The majority of cases of neurosyphilis are reported in HIV-infected patients.Citation36,Citation37 This is considered to be associated impaired control of syphilis infection due to compromised host immune activity as a result of HIV co-infection.Citation36 Especially, HIV-patients with a CD4 count of <350 cells/μL seem to be under a higher risk of developing CSF and neurological abnormalities most likely meningitis.Citation37
Co-infections with other causes of STI such as Neisseria gonorrhea, Herpes simplex virus 2, Chlamydia trachomatis, Hepatitis B and Hepatitis C virus and Trichomonas vaginalis are reported to be prevalent in developing countries.Citation38–Citation41 The incidence of syphilis between 1990 and 1996 in Slovak Republic has been reported to increase nearly five times, and the patients have been most commonly co-infected with Neisseria gonorrhea.Citation38 Increased number of cases of syphilis in the Black Sea region of Turkey has been reported between the years 1992 and 1994 related to unprotected sex, promiscuity, and prostitution.Citation39 The incidence of syphilis in pregnant women has also noted to increase in Slovak Republic between 1990 and 1996 with the stable number of cases with CS.Citation38 TORCHES (toxoplasmosis, rubella, cytomegalic inclusion disease, herpes virus including Epstein-Barr, syphilis) was defined as congenital co-infection with more than one pathogens, and it was considered as an infectious etiology of congenital cataract.Citation41–Citation45 CS and congenital toxoplasmosis are more frequent infectious causes of congenital blindness or visual impairment.Citation42,Citation43 Rare cases of CS co-infected with congenital rubella and congenital toxoplasmosis co-infected with congenital rubella have been described.Citation44 However, co-infected with T. gondii in congenital ocular syphilis has been scarcely described in the literature.Citation45 Our study disclosed that two of the cases who were siblings with congenital late syphilis were seropositive for T. gondii-specific IgG antibody. The cause of their visual impairments was related to posterior uveitis presented as central retinochoroiditis.
Chorioretinitis in the macula and delay in diagnosis were related to visual loss in patients with ocular syphilis.Citation27 The BCVAs of our patients with CS showed slight improvement from 20/80 to 20/50 with IV PCN and low-dose TMP–SMX which was considered as prophylaxis related to the presence of risk factor that was seropositivity for syphilis.
MTX has been considered to have an adjunctive role to suppress intraocular inflammation, reduce uveitic macular edema, and prevent the recurrences of the disease.Citation46 Cases 1–3 received adjunctive therapy with MTX after specific therapy with IV PCN to resolve the residual intraocular inflammation and CME.
Conclusion
Ocular syphilis is uncommon cause of ocular inflammation in HIV-negative patients. Central retinochoroiditis is the most common ocular manifestation, and it is the most common cause of visual impairment. Ocular syphilis might present associated with co-infections such as T. gondii in developing countries. Oral MTX might be beneficial as an adjunctive therapy for ocular syphilis in resolving the residual intraocular inflammation and CME after specific therapy with IV PCN.
Disclosure
The authors report no conflicts of interest in this work.
References
- HookEWMarraCMAcquired syphilis in adultsN Engl J Med199232616106010691549153
- PhiskeMMCurrent trends in congenital syphilisIndian J Sex Transm Dis2014351122024958980
- MindelAToveySJTimminsDJWilliamsPPrimary and secondary syphilis, 20 years’ experience. 2. Clinical featuresGenitourin Med1989651132921046
- ChapelTAThe signs and symptoms of secondary syphilisSex Transm Dis1980741611647455863
- CohenSEKlausnerJDEngelmanJPhilipSSyphilis in modern era: an update for physiciansInfect Dis Clin North Am201327470572224275265
- HandsfieldHHLukehartSASellSNorrisSJHolmesKKDemonstration of Treponema pallidum in a cutaneous gumma by indirect immunofluorescenceArch Dermatol198311986776806191721
- JantzenSUFerreaSLangebnerTLate-stage neurosyphilis presenting with severe neuropsychiatric deficits: diagnosis, therapy, and course of three patientsJ Neurol2012259472072821964751
- KampmeierRHNeurosyphilisAm Pract Dig Treat19482852352518914370
- AldaveAJKingJACunninghamETJrOcular syphilisCurr Opin Ophthalmol200112643344111734683
- De SantisMDe LucaCMappaISyphilis infection during pregnancy: fetal risks and clinical managementInfect Dis Obstet Gynecol2012201243058522829747
- ShaparenkoMVAnton’evAAMilichMVThe clinical and serological characteristics of early congenital syphilis todayVestn Dermatol Venerol1990716202256359
- MargoCEHamedLMOcular syphilisSurv Ophthalmol19923732032201475754
- MorshedMGCurrent trend on syphilis diagnosis: issues and challengesAdv Exp Med Biol2014808516424595610
- KentMERomanelliFReexamining syphilis: an update on epidemiology, clinical manifestations, and managementAnn Pharmacother200842222623618212261
- MatteiPLBeachkofskyTMGilsonRTWiscoOJSyphilis: a reemerging infectionAm Fam Physician201286543344022963062
- Centers for Disease Control and Prevention (CDC)Primary and secondary syphilis – United States, 2003–2004MMWR Morb Mortal Wkly Rep2006551026927316543880
- BernsteinKTStephensSCStronaFVKohnRPPhilipSSEpidemiologic characteristics of ongoing syphilis epidemic among men who have sex with men, San FranciscoSex Transm Dis2013401111723254114
- Spornraft-RagallerPSchmittJStephanVBoashieUBeissertSCharacteristics and coinfection with syphilis in newly HIV-infected patients at the University Hospital Dresden 1987–2012J Dtsch Dermatol Ges201412870771624941863
- KocakNHepgulSOzbayburtluSTrends in major transfusion-transmissible infections among blood donors over 17 years in Istanbul, TurkeyJ Int Med Res200432667167515587762
- MemishZAAlmasriMChentoufiAASeroprevalence of Herpes Simplex Virus Type 1 and Type 2 and coinfection with HIV and syphilis: the first national seroprevalence survey in Saudi ArabiaSex Transm Dis201542952653226267880
- DorrisJPSahaKJonesNPSukthankarAOcular syphilis: the new epidemicEye200620670370515933744
- MathewRGGohBTWestcottMCBritish Ocular Syphilis Study (BOSS): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilisInvest Ophthalmol Vis Sci20145585394540024925878
- HughesEHGuzowskiMSimunovicMPHunyorAPMcCluskeyPSyphilitic retinitis and uveitis in HIV-positive adultsClin Exp Ophthalmol2010389851856
- YapSCTanYLChioMTTeohSCSyphilitic uveitis in a Singaporean populationOcul Immunol Inflamm201422191424063580
- AnshuAChenqCLCheeSPSyphilitic uveitis: an Asian perspectiveBr J Ophthalmol200892559459718441168
- YangPZhangNLiFChenYKijlstraAOcular manifestations of syphilitic uveitis in Chinese patientsRetina20123291906191422495332
- MoradiASalekSDanielEClinical features and incidence rates of ocular complications in patients with ocular syphilisAm J Ophthalmol2015159233434325447116
- PuechCGennaiSPavesePOcular manifestations of syphilis: Recent cases over a 2.5-year periodGraefes Arch Clin Exp Ophthalmol2010248111623162920703496
- MorshedMGCurrent trend on syphilis diagnosis: issues and challengesAdv Exp Med Biol2014808516424595610
- TongMLLinLRLiuLLAnalysis of 3 algorithms for syphilis serodiagnosis and implications for clinical managementClin Infect Dis20145881116112424550376
- BinnickerMJJespersenDJRollinsLODirect comparison of the traditional and reverse screening algorithms in a population with a low prevalence of syphilisJ Clin Microbiol201250114815022090407
- SenaACWhiteBLSparlingPFNovel Treponema pallidum serologic tests: a paradigm shift in syphilis screening for the 21st centuryClin Infect Dis201051670077020687840
- SimonRThe great poxClin Infect Dis20043871007100815034834
- GhanemKGNeurosyphilis: a historical perspective and reviewCNS Neurosci Ther2010165157168
- TimmermansMCarrJNeurosyphilis in the modern eraJ Neurol Neurosurg Psychiatry200475121727173015548491
- ChanDJSyphilis and HIV co-infection: when is lumbar puncture indicated?Curr HIV Res200531959815638727
- LynnWALightmanSSyphilis and HIV: a dangerous combinationLancet Infect Dis20044745646615219556
- HegyiVDanillaTHegyiEActual trends of the incidence of syphilis and gonorrhea in the Slovak Republic in the year 1990–1996Sex Transm Inf1998745376
- ApaydınRBilenNGülUBahadırSIncreased number of cases of syphilis in Trabzon, a trade city in the Black Sea region of TurkeySex Transm Inf1998745377
- MakasaMBuveASandoyIFEtiologic pattern of genital ulcers in Lusaka, Zambia: has chancroid been eliminated?Sex Transm Dis2012391078779123001266
- TirunehMSeroprevalence of multiple sexually transmitted infections among antenatal clinic attendees in Gonar Health Center, northwest EthiopiaEthiop Med J200846435936619271400
- MahalakshmiBThereseKLDevipriyaUPushpalathaVMargaritaSMadhavanHNInfectious etiology of congenital cataract based on TORCHES screening in a tertiary eye hospital in Chennai, Tamil Nadu, IndiaIndian J Med Res201013155956420424308
- ThapliyalNShuklaPKKumarBUpadhyaySJainGTORCH infection in women with bad obsteric history – a pilot study in Kumaon regionIndian J Pathol Microbiol200548455155316366124
- Souza RdaSAraújoBFPrevalence of toxoplasmosis, HIV, syphilis and rubella in a population of puerperal women using Whatman 903 filter paperBraz J Infect Dis2010141242920428650
- TurbadkarDMathurMReleMSeroprevalence of TORCH infection in bad obstetric historyIndian J Med Microbiol200321210811017642992
- SahinOZiaeiAThe role of methotrexate in resolving ocular inflammation after specific therapy for presumed latent syphilitic uveitis and presumed tuberculosis-related uveitisRetina20143471451145924531737
