Abstract
Background
The usefulness of ribonucleotide reductase catalytic subunit M1 (RRM1) for predicting the therapeutic effects of gemcitabine-containing chemotherapy in patients with non-small cell lung cancer (NSCLC) remains controversial. RRM1-positive patients show unique clinicopathological features.
Methods
Here, we performed a meta-analysis to systematically evaluate the relationship between RRM1 expression and the clinicopathological characteristics of NSCLC patients treated with gemcitabine-containing regimens. A comprehensive electronic and manual search was performed to identify relevant articles. The pooled relative risk (RR) and 95% CI were used to estimate the relation between the clinicopathological characteristics of NSCLC patients and RRM1 expression.
Results
The study included 31 observational studies and 3,667 patients. The analysis showed no significant association between RRM1 expression and pathological type, stage, and smoking status; however, RRM1 positivity was significantly lower in women than in men (43.0% vs 51.7%, RR=0.84, 95% CI: 0.74–0.94, P=0.004).
Conclusion
The present pooled analyses demonstrated that RRM1 positivity in women with advanced NSCLC was associated with a higher rate of response to gemcitabine-containing regimens. Immunohistochemistry may be valuable to prescreen for RRM1 expression in clinical practice, whereas PCR can be routinely used as a verification method. These findings will help design suitable molecular-targeted therapies for NSCLC.
Introduction
Lung cancer is a common malignancy and the main cause of cancer-related mortality in the world. Non-small cell lung cancer (NSCLC) accounts for 80% of all lung cancer patients worldwide.Citation1–Citation3 Lung carcinoma is divided into two subtypes according to the response to conventional treatments and the histological features of tumors: small cell lung carcinoma and NSCLC. Despite advances in the therapeutic approaches to the treatment of lung cancer, including immunotherapy, chemotherapy, radiotherapy, and noninvasive surgery, the 5-year relative survival rate of patients with lung cancer iŝ18% in the USA.Citation1
First-line chemotherapy for NSCLC usually consists of a platinum-containing doublet regimen. Patients with advanced NSCLC are generally treated with chemotherapy drugs, including cisplatin and gemcitabine.Citation4 Gemcitabine, a pyrimidine nucleoside antimetabolite, is active in advanced NSCLC, especially in combination with a platinum derivative or a next-generation anticancer agent.Citation5,Citation6 Pharmacoeconomic evaluation suggests that a gemcitabine-based regimen is the least costly regimen for the treatment of advanced NSCLC.Citation7 However, patients with advanced NSCLC may develop resistance to gemcitabine, which is associated with a poor prognosis. Therefore, identification of the markers for predicting clinical outcomes and treatment sensitivity in patients receiving gemcitabine chemotherapy would be of great value.
Ribonucleotide reductase catalyzes the reduction of ribonucleotide 5-diphosphate to deoxyribonucleotide 5-diphosphate for DNA synthesis and damage repair. The ribonucleotide reductase catalytic subunit M1 (RRM1) gene is located on chromosome segment 11p15.5 and encodes a key enzyme involved in DNA synthesis that catalyzes the biosynthesis of deoxyribonucleotides.Citation8,Citation9 Preclinical studies show that RRM1 is involved in gemcitabine sensitivity in NSCLC.Citation10,Citation11 High levels of RRM1 are associated with a decreased response to gemcitabine-containing regimens, whereas RRM1 downregulation is associated with a high rate of response to gemcitabine-containing regimens.Citation12,Citation13 Therefore, RRM1 may be a predictive biomarker for gemcitabine chemotherapy in NSCLC.
Reverse transcriptase PCR (RT-PCR) and immunohistochemistry (IHC) are currently used to detect RRM1. However, an effective algorithm for RRM1 gene screening in the clinical lung cancer population remains undetermined because these two approaches have both advantages and disadvantages. Thus, to increase the detection efficiency of the two methodologies, we studied whether combining the clinicopathological features of NSCLC with RRM1 detection would yield valuable information for the effective prescreening of patients in clinical practice. Although a large number of patients carrying the RRM1 gene show unique clinicopathological characteristics,Citation13–Citation17 the detailed clinicopathological profiles remain unclear because of the small number of cases identified. Here, we performed a pooled analysis of a series of studies to assess the relationship between RRM1 gene expression in NSCLC and the clinicopathological characteristics of patients treated with gemcitabine-containing regimens. To the best of our knowledge, the present study is the first comprehensive and systematic analysis of the clinicopathological characteristics of NSCLC patients harboring the RRM1 gene.
Materials and methods
Literature search
EMBASE, PubMed, China National Knowledge Internet (CNKI), the WanFang database, and the Cochrane Library were searched for relevant studies up to September 2017. Electronic searches were performed using the terms “non-small cell lung cancer or NSCLC,” “gemcitabine,” and “ribonucleotide reductase M1 or RRM1.” The detailed search strategies are showed in . This meta-analysis followed the PRISMA guidelines.
Eligibility criteria
Articles were included based on the following criteria: 1) included NSCLC patients, regardless of the pathological phenotypes; 2) provided information about the RRM1 gene detection method and the clinicopathological characteristics of lung carcinoma patients harboring the RRM1 gene, including gender, clinical stage, smoking habits, and pathological type; and 3) were published as full-text articles. Review articles, conference abstracts, case reports, and those lacking sufficient data (because of the limited data) to evaluate the relative risk (RR) and 95% CI were excluded.
Data collection
Data extraction was independently performed by two authors (Chao Wu and Qiu-Ping Leng) using a standardized form. Data such as first author, year of publication, gender, number of patients, pathological type of tumors, clinical stage, detection method, and RRM1 expression were collected. Discrepancies were settled by discussion, with disagreements resolved by consensus.
Statistical analysis
The pooled RR and 95% CI were used to estimate the strength of the clinicopathological characteristics of NSCLC patients harboring the RRM1 gene. The Cochran’s Q-test and I2 statistics were used to measure the statistical heterogeneity. The random-effects model was implemented if the heterogeneity was significant (P<0.05 or I2>50%)Citation18; otherwise, the fixed-effects model was used.Citation19 Sensitivity analysis was performed by sequentially excluding studies from the current analysis to evaluate the stability of the pooled results. Begg’s test was performed to evaluate the possible potential publication bias of the studies (P<0.05 was considered significant).Citation20 Meta-analyses were performed using Review Manager 5.3 (RevMan 5.3®; Nordic Cochrane Center, Copenhagen, Denmark). Categorical variables were analyzed by the χ2 test using SPSS 24.0 (SPSS Inc., Chicago, IL, USA), and P<0.05 was considered statistically significant.
Results
Characteristics of included studies
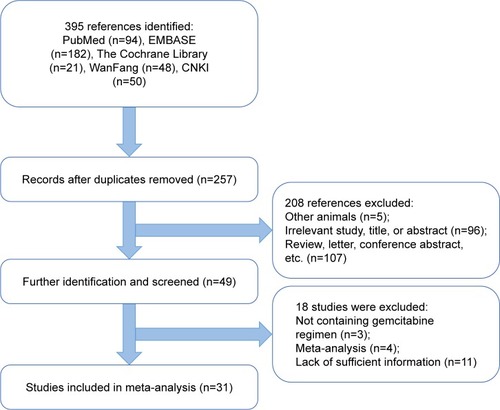
As shown in the flow diagram for the study selection process (), 395 potentially relevant studies were initially obtained from PubMed, EMBASE, CNKI, the WanFang database, and the Cochrane Central Library. After screening the abstracts, titles, and contents, 31 observational studies including 3,667 patients were identified as eligible for the present study. Of the 31 studies, 16 (1,425 patients) reported on the relationship between RRM1 expression and gender in NSCLC patients treated with gemcitabine-containing chemotherapy, whereas the remaining 15 studies (1,242 patients) showed the relationship between RRM1 expression and pathological type. Three studies (288 patients) focused on the relationship between RRM1 expression and clinical stage, whereas eight studies (907 patients) focused on the association of RRM1 expression in NSCLC with smoking status. The baseline features of the selected studies are listed in .
Table 1 Baseline characteristics of the included studies
Meta-analysis results
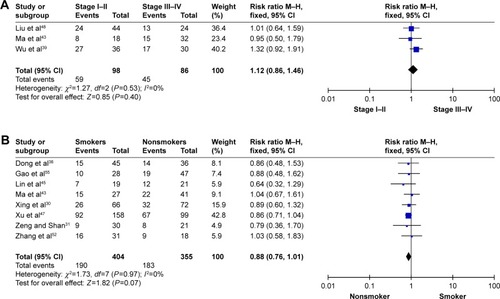
In total, 3,667 participants from 31 observational studies were included in the present meta-analysis; 1,772 patients (49.1%) harbored the RRM1 gene. Of the 31 studies, 16 studies demonstrated an association between RRM1 expression in NSCLC and gender. There was no significant heterogeneity among these studies (Pheterogeneity=0.74, I2=0%); therefore, a fixed-effects model was used to analyze the data. The pooled findings are shown in . Women with positive RRM1 expression had a statistically significantly lower risk of NSCLC than men (43.0% vs 51.7%, RR=0.84, 95% CI: 0.74–0.94, P=0.004). Fifteen studies assessed the role of RRM1 expression in the adenocarcinoma and non-adenocarcinoma groups. There was no significant heterogeneity among the studies (Pheterogeneity=0.68, I2=0%). The results of the study showed no significant differences between the adenocarcinoma and non-adenocarcinoma groups (44.4% vs 44.3%, RR=0.97, 95% CI: 0.84–1.10, P=0.61) (). Three studies investigated the association between RRM1 expression and tumor staging. There was no significant heterogeneity among these studies (Pheterogeneity=0.53, I2=0%); therefore, the data were analyzed using a fixed-effects model. The present meta-analysis demonstrated that there was no significant difference between stage I–II and stage III–IV (RR=0.88, P=0.07) (). In addition, eight studies evaluated the correlation between RRM1 gene expression and smoking history. There was no significant heterogeneity among these studies (Pheterogeneity=0.97, I2=0%), and hence the data were analyzed using a fixed-effects model. The results demonstrated that there was no significant difference between smokers and nonsmokers (RR=0.88, P=0.07) ().
Figure 2 Meta-analysis of data for RRM1.
Abbreviations: RRM1, ribonucleotide reductase catalytic subunit M1c; M–H, Mantel–Haenszel.
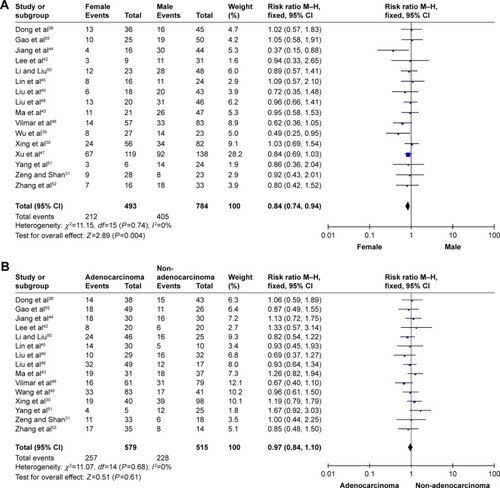
Figure 3 Meta-analysis of data for RRM1.
Abbreviations: M–H, Mantel–Haenszel; RRM1, ribonucleotide reductase catalytic subunit M1.
The research was extended to the analysis of two detection methods (RT-PCR and IHC) for direct comparison of sensitivity and specificity. Of 1,231 patients analyzed by IHC in 15 studies, 539 (43.8%) had high-level expression of RRM1; 2,265 patients had successful RT-PCR detection of RRM1 expression in 16 studies, of which 1,256 (55.5%) expressed the RRM1 gene ().
Table 2 Methods for the detection of RRM1 expression
Sensitivity analysis and publication bias
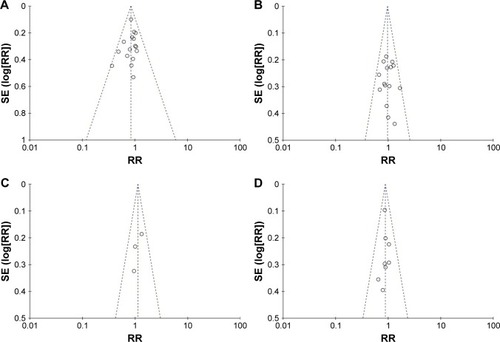
Sensitivity analysis was performed by sequentially excluding individual studies to examine the impact of each study on the summarized findings. This revealed that the findings were statistically robust and credible (data not shown). Begg’s test was performed to evaluate the potential publication bias of the studies.Citation20 The shape of the funnel plot was symmetrical, suggesting there was no obvious publication bias ().
Discussion
Gemcitabine (2′,2′-difluorodeoxycytidine), which is active against NSCLC, is a deoxycytidine analog that is incorporated into DNA and competitively inhibits DNA synthesis.Citation21 Resistance to gemcitabine is associated with RRM1 overexpression.Citation22–Citation24 RRM1 catalyzes the biosynthesis of deoxyribonucleotide and participates in DNA synthesis and damage repair. Preclinical studies show that RRM1 expression is associated with chemosensitivity to gemcitabine-containing therapies and that a low level of RRM1 expression is associated with a better response to gemcitabine-containing chemotherapy.Citation10,Citation11
RRM1, which is located on chromosome segment 11p15.5, is involved in the regulation of tumor proliferation, invasiveness, and metastasis. This region, also known as LOH11A, shows frequent loss of heterozygosity in NSCLC.Citation8,Citation9 Previous clinical studies demonstrated a close relationship between RRM1 expression and the response to gemcitabine-containing regimens in different types of cancer, including pancreatic cancer, nasopharyngeal carcinoma, and NSCLC.Citation8,Citation12,Citation15,Citation17,Citation25–Citation56
Here, we reviewed almost all available published articles and conducted the present meta-analysis to examine the correlation between RRM1 expression and the clinicopathological features of NSCLC. Analysis of 3,667 participants from 31 studies indicated a low rate (49.1%) of RRM1 expression in NSCLC patients. Therefore, we examined the clinicopathological characteristics of RRM1-positive lung cancer patients to improve the screening efficacy. The present analysis demonstrated that RRM1 positivity in lung cancer patients was more prevalent in men than in women (43.0% vs 51.7%, RR=0.84, 95% CI: 0.74–0.94, P=0.004). The proportion of RRM1-positive patients in adenocarcinoma was slightly lower than that in non-adenocarcinoma, although the relation was not statistically significant (RR=0.97, 95% CI: 0.84–1.10, P=0.61). The proportion of RRM1-positive patients was slightly lower in nonsmokers than in smokers with NSCLC (47.0% vs 51.5%, RR=0.88, 95% CI: 0.76–1.01, P=0.07). Similarly, RRM1 gene positivity was not strongly correlated with clinical stage in NSCLC patients (RR=1.12, 95% CI: 0.86–1.46, P=0.40).
The present study provided evidence to guide the pre-screening of NSCLC patients for selecting a population likely to harbor this specific gene. Dong et alCitation36 reported that RRM1 expression in tumor tissues could be a predictive biomarker in patients with advanced NSCLC receiving gemcitabine-containing chemotherapy. These authors showed that 83 of 229 (36.20%) NSCLC tumors were RRM1-positive, and 13 RRM1-positive tumors were detected in women (36.11% [13/36]). Vilmar et alCitation46 reported that 47 of 140 (33.57%) NSCLC patients were RRM1-positive, and 14 RRM1-positive tumors were found in women (24.56% [14/57]). These results are consistent with those of the present meta-analysis showing a prevalence of 43.00% in women. As the incidence of RRM1 is low in NSCLC patients, investigating the clinicopathological characteristics of RRM1-positive lung cancer patients is necessary to improve the screening efficacy and reduce medical costs. Evaluation of the clinicopathological characteristics of NSCLC patients was the first prescreening step.
RT-PCR and IHC are the most reliable methodologies to detect the RRM1 gene. Reynolds et al used a fluorescence-based IHC method combined with automated quantitative analysis, but failed to observe important differences in survival in NSCLC patients with different levels of RRM1 gene expression who received gemcitabine-containing chemotherapy.Citation57,Citation58 Zheng et alCitation59 used these two methods simultaneously and found that the mRNA expression levels were closely related to protein expression levels. In the present study, the positive rates of IHC and RT-PCR were 43.8% and 55.5%, respectively, indicating that these methods are reliable for detecting RRM1 expression. IHC, which is a well-established method for detecting RRM1 expression, is a convenient and cost-effective technique for detecting RRM1 expression in patients with NSCLC.Citation60 Currently, RT-PCR is the most sensitive method for detecting and quantifying mRNA. Large-sample prospective studies are necessary to further evaluate the efficacy of RT-PCR detection for the prediction of chemosensitivity to gemcitabine associated with RRM1 expression.
This study had several limitations. First, the conclusions are mainly based on observational studies. A meta-analysis of well-designed nonrandomized studies can be as accurate as that of randomized-controlled trials.Citation61 Second, only studies written in English or Chinese were included in the meta-analysis. This means that eligible studies published in other languages may have been overlooked, which may have introduced selection bias. Third, most of the participants of the current pooled analysis were Asian. Therefore, future studies should include subjects from diverse ethnicities. The present survey also lacked sufficient individual patient data. Therefore, additional details and subgroup data such as sex, smoking status, pathologic classification, and clinical stages are needed for further analysis.
Conclusion
Our meta-analysis suggests that RRM1 positivity is related to a higher response rate to gemcitabine-based regimens in women with advanced NSCLC. RRM1 may be used as a biomarker to predict the response rate to gemcitabine-based chemotherapy in NSCLC. IHC could be used to prescreen for RRM1 expression in the clinic, and RT-PCR could be used for confirmation. Further large-scale, well-designed prospective studies are necessary to determine the potential correlation between RRM1 expression in NSCLC and the clinicopathological characteristics of patients treated with gemcitabine-containing chemotherapy.
Supplementary material
Table S1 Search strategy
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRLMillerKDJemalAStatisticsCCA Cancer J Clin2017201767730
- WoodSLPernemalmMCrosbiePAWhettonADThe role of the tumor-microenvironment in lung cancer-metastasis and its relationship to potential therapeutic targetsCancer Treat Rev201440455856624176790
- BrayFRenJSMasuyerEFerlayJGlobal estimates of cancer prevalence for 27 sites in the adult population in 2008Int J Cancer201313251133114522752881
- Paz-AresLde MarinisFDediuMMaintenance therapy with pemetrexed plus best supportive care versus placebo plus best supportive care after induction therapy with pemetrexed plus cisplatin for advanced non-squamous non-small-cell lung cancer (PARAMOUNT): a double-blind, phase 3, randomised controlled trialLancet Oncol201213324725522341744
- GeorgouliasVAndroulakisNKotsakisADocetaxel versus docetaxel plus gemcitabine as front-line treatment of patients with advanced non-small cell lung cancer: a randomized, multicenter phase III trialLung Cancer2008591576317765354
- ToschiLCappuzzoFGemcitabine for the treatment of advanced nonsmall cell lung cancerOnco Targets Ther2009220921720616908
- ReaumeMNLeighlNBMittmannNEconomic analysis of a randomized phase III trial of gemcitabine plus vinorelbine compared with cisplatin plus vinorelbine or cisplatin plus gemcitabine for advanced non-small-cell lung cancer (Italian GEMVIN3/NCIC CTG BR14 trial)Lung Cancer201382111512023962449
- PitterleDMKimYCJolicoeurEMCaoYO’BriantKCBeplerGLung cancer and the human gene for ribonucleotide reductase subunit M1 (RRM1)Mamm Genome199910991692210441745
- BeplerGGautamAMcintyreLMPrognostic significance of molecular genetic aberrations on chromosome segment 11p15.5 in non-small-cell lung cancerJ Clin Oncol20022051353136011870179
- BergmanAMEijkPPRuiz van HaperenVWIn vivo induction of resistance to gemcitabine results in increased expression of ribonucleotide reductase subunit M1 as the major determinantCancer Res200565209510951616230416
- OguriTAchiwaHSatoSThe determinants of sensitivity and acquired resistance to gemcitabine differ in non-small cell lung cancer: a role of ABCC5 in gemcitabine sensitivityMol Cancer Ther2006571800180616891466
- BeplerGKusmartsevaISharmaSRRM1 modulated in vitro and in vivo efficacy of gemcitabine and platinum in non-small-cell lung cancerJ Clin Oncol200624294731473716966686
- RosellRDanenbergKDAlberolaVRibonucleotide Reductase Messenger RNA Expression and Survival in Gemcitabine/Cisplatin-Treated Advanced Non-Small Cell Lung Cancer PatientsClinical Cancer Research20041041318132514977831
- RosellRFelipETaronMGene expression as a predictive marker of outcome in stage IIB-IIIA-IIIB non-small cell lung cancer after induction gemcitabine-based chemotherapy followed by resectional surgeryClin Cancer Res20041012 Pt 24215S4219S15217961
- SouglakosJBoukovinasITaronMRibonucleotide reductase subunits M1 and M2 mRNA expression levels and clinical outcome of lung adenocarcinoma patients treated with docetaxel/gemcitabineBr J Cancer200898101710171518414411
- JordheimLPSèvePTrédanODumontetCThe ribonucleotide reductase large subunit (RRM1) as a predictive factor in patients with cancerLancet Oncol201112769370221163702
- CeppiPVolanteMNovelloSERCC1 and RRM1 gene expressions but not EGFR are predictive of shorter survival in advanced non-small-cell lung cancer treated with cisplatin and gemcitabineAnn Oncol200617121818182516980606
- DersimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials1986731771883802833
- MantelNHaenszelWStatistical aspects of the analysis of data from retrospective studies of diseaseJ Natl Cancer Inst195922471974813655060
- BeggCBMazumdarMOperating characteristics of a rank correlation test for publication biasBiometrics1994504108811017786990
- ChabnerBALongoDLCancer Chemotherapy and Biotherapy: Principles and PracticePhiladelphia, PALippincott Williams & Wilkins2011
- GautamALiZRBeplerGRRM1-induced metastasis suppression through PTEN-regulated pathwaysOncogene200322142135214212687015
- GoanYGZhouBHuEMiSYenYOverexpression of ribonucleotide reductase as a mechanism of resistance to 2,2-difluorodeoxycytidine in the human KB cancer cell lineCancer Res199959174204420710485455
- DavidsonJDMaLFlagellaMGeeganageSGelbertLMSlapakCAAn increase in the expression of ribonucleotide reductase large subunit 1 is associated with gemcitabine resistance in non-small cell lung cancer cell linesCancer Res200464113761376615172981
- AoyamaTMiyagiYMurakawaMClinical implications of ribonucleotide reductase subunit M1 in patients with pancreatic cancer who undergo curative resection followed by adjuvant chemotherapy with gemcitabineOncol Lett20171353423343028521448
- MlakRKrawczykPCiesielkaMThe relationship between RRM1 gene polymorphisms and effectiveness of gemcitabine-based first-line chemotherapy in advanced NSCLC patientClin Transl Oncol201618991592426650486
- MausMKMackPCAstrowSHHistology-related associations of ERCC1, RRM1, and TS biomarkers in patients with non-small-cell lung cancer: implications for therapyJ Thorac Oncol20138558258623470290
- ZhaoLPXueCZhangJWExpression of RRM1 and its association with resistancy to gemcitabine-based chemotherapy in advanced nasopharyngeal carcinomaChin J Cancer2012311047648322692073
- GuoNZhangWZhangBEGFR and K-RAS mutations and ERCC1, TUBB3, TYMS, RRM1 and EGFR mRNA expression in non-small cell lung cancer: Correlation with clinical response to gefitinib or chemotherapyMol Clin Oncol2015351123112826623063
- XingXWangLXiaoXAnalysis of RRM1 expression in advanced NSCLC and its relationship with chemotherapyChin J Cancer Prev Treat20142118931896
- ZengFShanLInvestigation about expression of RRM1 (ribonucleotide reductase M1) and the correlation with Gemcitabine-based chemotherapy sensitivity in the advanced non-small cell lung cancerJournal of Taishan Medical College200930570573
- ZhaoHZhangHduYGuXPrognostic significance of BRCA1, ERCC1, RRM1, and RRM2 in patients with advanced non-small cell lung cancer receiving chemotherapyTumour Biol20143512126791268825227663
- Xian-JunFXiu-GuangQLiZERCC1 and BRCA1 mRNA expression predicts the clinical outcome of non-small cell lung cancer receiving platinum-based chemotherapyPak J Med Sci201430348849224948964
- WangLMengLWangXWMaGYChenJHExpression of RRM1 and RRM2 as a novel prognostic marker in advanced non-small cell lung cancer receiving chemotherapyTumour Biol20143531899190624155212
- LiangJGJinZYGaoXDPredictive role of RRM1 and BRCA1 mRNA expression on the clinical outcome of advanced non-small cell lung cancerGenet Mol Res20141335292529825078585
- DongXHaoYWeiYYinQduJZhaoXResponse to first-line chemotherapy in patients with non-small cell lung cancer according to RRM1 expressionPLoS One201493e9232024647522
- Jian-WeiBYi-MinMYu-XiaSShi-QingLExpression levels of ERCC1 and RRM1 mRNA and clinical outcome of advanced non-small cell lung cancerPak J Med Sci20132951158116124353711
- SuCZhouSZhangLERCC1, RRM1 and BRCA1 mRNA expression levels and clinical outcome of advanced non-small cell lung cancerMed Oncol20112841411141720467918
- WuGQLiuNNXueXLMultiplex real-time PCR for RRM1, XRCC1, TUBB3 and TS mRNA for prediction of response of non-small cell lung cancer to chemoradiotherapyAsian Pac J Cancer Prev201415104153415824935362
- WangXZhaoJYangLPositive expression of ERCC1 predicts a poorer platinum-based treatment outcome in Chinese patients with advanced non-small-cell lung cancerMed Oncol201027248449019488864
- GuoQZWangJBaiHHigh expression of ERCC1 is a poor prognostic factor in Chinese patients with non-small cell lung cancer receiving cisplatin-based therapyChin J Cancer Res2010224296302
- LeeJJMaengCHBaekSKThe immunohistochemical overex-pression of ribonucleotide reductase regulatory subunit M1 (RRM1) protein is a predictor of shorter survival to gemcitabine-based chemotherapy in advanced non-small cell lung cancer (NSCLC)Lung Cancer201070220521020223551
- MaKLiEGuoYWangXSunHShaoGRelationship between the efficacy of gemcitabine/cisplatin adjuvant chemotherapy and RRM1 protein expression in postoperative NSCLC patientsZhonghua Zhong Liu Za Zhi201436750551025327655
- JiangBTuCHeWYangCZhaoJAnalysis of RRM1 expression and efficacy of gemcitabine in advanced non-small cell lung cancerCancer Research on Prevention and Treatment2013406871
- LinLZhangXHuJHuangFLiWAnalysis of the relationship between RM1 mRNA expression level and efficacy of gemcitabine maintenance therapy for advanced non-small cell lung cancerThe Practical Journal of Cancer2016312225
- VilmarACSantoni-RugiuESorensenJBPredictive impact of RRM1 protein expression on vinorelbine efficacy in NSCLC patients randomly assigned in a chemotherapy phase III trialAnn Oncol201324230931423038758
- XuCWWangGWangWLAssociation between epidermal growth factor receptor mutations and the expression of excision repair cross-complementing protein 1 and ribonucleotide reductase subunit M1 mRNA in patients with non-small cell lung cancerExp Ther Med20159388088425667646
- LiuDNakashimaNNakanoJCustomized Adjuvant Chemotherapy Based on Biomarker Examination May Improve Survival of Patients Completely Resected for Non-small-cell Lung CancerAnticancer Res20173752501250728476819
- LiuHWangHYangJRRM1 Expression and Efficacy Analysis of Gemcitabine in Advanced Non-small Cell Lung CancerPract Prevent Med2009161114
- LiLLiuXCorrelation of expression of ERCC1/RRM1 with cisplatin combined with gemcitabine chemotherapy sensitivity and prognosis in non-small cell lung cancerBull Acad Mil Med Sci201034265268
- YangZLiuDChenFChenJTanSLinSThe effect of RRM1 expression in lung cancer tissues for predict chemotherapeutic effect of GPChin J Oncol Prev Treat20091124126
- ZhangGBChenJWangLRRRM1 and ERCC1 expression in peripheral blood versus tumor tissue in gemcitabine/carboplatin-treated advanced non-small cell lung cancerCancer Chemother Pharmacol20126951277128722302408
- BeplerGSommersKECantorAClinical efficacy and predictive molecular markers of neoadjuvant gemcitabine and pemetrexed in resectable non-small cell lung cancerJ Thorac Oncol20083101112111818827606
- BoukovinasIPapadakiCMendezPTumor BRCA1, RRM1 and RRM2 mRNA expression levels and clinical response to first-line gemcitabine plus docetaxel in non-small-cell lung cancer patientsPLoS One2008311e369519002265
- GaoZHanBShenJGuAZhongHRelations between RRM1 protein expression levels and effects of gemcitabine and cisplatin chemotherapy in advanced non-small cell lung cancer patientsZhongguo Fei Ai Za Zhi201114434034421496433
- RosellRScagliottiGDanenbergKDTranscripts in pretreatment biopsies from a three-arm randomized trial in metastatic non-small-cell lung cancerOncogene200322233548355312789263
- ReynoldsCObasajuCSchellMJRandomized phase III trial of gemcitabine-based chemotherapy with in situ RRM1 and ERCC1 protein levels for response prediction in non-small-cell lung cancerJ Clin Oncol200927345808581519884554
- CampRLChungGGRimmDLAutomated subcellular localization and quantification of protein expression in tissue microarraysNat Med20028111323132812389040
- ZhengZChenTLiXHauraESharmaABeplerGDNA synthesis and repair genes RRM1 and ERCC1 in lung cancerN Engl J Med2007356880080817314339
- NalbandianAYanBSPichuginABronsonRTKramnikILung carcinogenesis induced by chronic tuberculosis infection: the experimental model and genetic controlOncogene200928171928193819330024
- AbrahamNSByrneCJYoungJMSolomonMJMeta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trialsJ Clin Epidemiol201063323824519716267