Abstract
Adrenal cortical carcinoma (ACC) is a rare cancer that poses a number of management challenges due to the limited number of effective systemic treatments. Complete surgical resection offers the best chance of long-term survival. However, despite complete resection, ACC is associated with high recurrence rates. This review will discuss the management of recurrent ACC in adults following complete surgical resection. Management should take place in a specialist center and treatment decisions must consider the individual tumor biology of each case of recurrence. Given the fact that ACC commonly recurs, management to prevent recurrence should be considered from initial diagnosis with the use of adjuvant mitotane. Close follow up with clinical examination and imaging is important for early detection of recurrent disease. Locoregional recurrence may be isolated, and repeat surgical resection should be considered along with mitotane. The use of radiotherapy in ACC remains controversial. Systemic recurrence most often involves liver, pulmonary, and bone metastasis and is usually managed with mitotane, with or without combination chemotherapy. There is a limited role for surgical resection in systemic recurrence in selected patients. In all patients with recurrent disease, control of excessive hormone production is an important part of management. Despite intensive management of recurrent ACC, treatment failure is common and the use of clinical trials and novel treatment is an important part of management.
Background
Adrenal cortical carcinoma (ACC) has an incidence of approximately 0.5–2.0/million per year.Citation1–Citation3 ACC can develop at any age with a maximal incidence seen in adults aged 40–50 years.Citation4 Clinical presentation is due to functional symptoms related to excess adrenal hormone production, local symptoms related to tumor mass/local invasion, or incidental diagnosis by radiology. ACC is a heterogeneous disease characterized by a generally poor prognosis with an overall 5-year survival of less than 35%.Citation5,Citation6 At presentation, most patients have localized disease amenable to surgical resection, and 30%–40% of patients will have systemic disease.Citation6–Citation8 Due to poor response rates to systemic treatments, few patients with systemic disease achieve complete remission. Complete surgical resection offers the best hope for long-term survival; however ACC remains a challenging malignancy as many patients develop recurrent disease despite complete resection. In isolated cases, patients with systemic disease will have remission following treatment. Although it is not a focus of this review, the management principles for the treatment of recurrence following systemic remission are similar to recurrence following complete surgical resection.
Pathology
A challenge in the management of ACC is to quantify the recurrence risk from diagnosis. In the absence of metastatic disease or local invasion, the pathological diagnosis of ACC alone can be difficult due to the lack of clear-cut morphological criteria.Citation9 Differential diagnostic scores have been developed for pathological diagnosis; currently the Weiss and modified Weiss scores are the most widely accepted scoring systems and are based on histological findings.Citation10,Citation11 These systems are not infallible and tumors initially diagnosed as benign can have unpredictable behavior. Immunohistochemistry provides important information for the diagnosis of ACC.Citation12 Insulin-like growth factor 2 (IGF-2) overexpression has been identified in up to 90% of patients with sporadic ACC compared to adrenal cortical adenomas.Citation13 The proliferation marker Ki-67 has also been demonstrated to be of importance in determining ACC and a patient’s risk of recurrence. A high Ki-67 index (>10%) is associated with a shortened disease-free status and decreased overall survival.Citation9,Citation14
Experimentally, the use of transcriptome, microRNA, and methylation profiling have been useful in diagnosing ACC, and offer the potential to stratify the risk of recurrence; however these techniques are yet to be validated in clinical practice.Citation15–Citation19
One example of this experimentation is the gene expression analysis of 153 adrenal tumors by de Reynies et al, where adrenal tumors were able to be classified into distinct diagnostic and prognostic groups.Citation20 This study found differential expression of the cell cycle regulation genes DLG7 and PINK1 were a reliable indicator of benign and malignant tumors. ACCs were able to be classified into two distinct prognostic groups based on the combined expression of the genes BUB1B and PINK1, with the better prognostic group less likely to have recurrent disease following surgery and also having an improved overall survival rate.
Management following initial surgical resection
Due to the high risk of recurrent disease, management of recurrence should be considered from the initial diagnosis. As with other malignancies, the management should take place in a multidisciplinary setting. Following surgery, the surgical resection margins need to be carefully assessed. If a complete resection (R0) has not been achieved, the role and feasibility of further surgical resection needs to be considered, as complete surgical resection is a critical prognostic factor.Citation1,Citation7 Patients with functional tumors should have post-operative hormone levels assessed as these levels can be used to indicate the completeness of surgical resection.Citation21
Adjuvant mitotane
Adjuvant mitotane needs to be considered in all patients following surgical resection. Mitotane, a synthetic derivative of the insecticide dichlorodiphenyltrichloroethane (DDT) is an adrenolytic agent that has been the mainstay of medical management for metastatic ACC since it was discovered in the 1950s. However, its role in the adjuvant setting is less clear.Citation5 Adjuvant mitotane has been shown in a number of retrospective case control series to improve recurrence-free survival following complete surgical resection;Citation22,Citation23 but these results have been criticized due to the possibility of selection bias and confounding.Citation24 Adjuvant mitotane requires long-term treatment and frequent drug monitoring.Citation25 Toxicity such as anorexia, nausea, vomiting, and diarrhea are common and can limit adjuvant mitotane’s use as a long-term treatment.Citation1,Citation24,Citation25 Mitotane use is associated with hypertriglyceridemia, changes in hormone binding globulins, and induction of hepatic microsomal enzymes leading to multiple drug interactions.Citation3,Citation25 These effects, and the need for monitoring, are further discussed in the section of mitotane therapy for systemic recurrence.
It has been suggested that, due to the difficulties associated with long term mitotane therapy, the use of adjuvant mitotane can be determined by the risk of recurrence, which can be stratified into low to intermediate and high risk.Citation26 Patients with a high recurrence risk are defined by an initial tumor size of >8 cm, microscopic invasion of blood vessels/tumor capsule, or a Ki-67 index of >10%. These patients should be offered adjuvant mitotane routinely and considered for radiotherapy to the adrenal bed. Patients without these indications can be classified as low to intermediate risk, and for these patients the Efficacy of Adjuvant Mitotane Treatment (ADIUVO) study is currently recruiting.Citation27 This study is an international randomized trial comparing mitotane to observational follow up. Until these results are available most centers recommend adjuvant mitotane after complete resection.Citation1
Follow up after surgical resection
Due to the risk of recurrence and the possibility of further surgical treatment for recurrent ACC patients, close follow up is required. Early detection of recurrence is important as local recurrence or limited metastatic disease may be amenable to complete surgical resection (R0), which can be followed by long periods of disease-free survival.Citation1
Follow-up should take the form of clinical assessment and progress imaging by computerized tomography (CT) with or without positron emission tomography (PET) scanning. In specialist centers, a range of follow up protocols has been suggested. These protocols include abdominal and chest CT every 3 months for the first 2 years post-surgery, increasing to 6–12 monthly intervals for at least 5 years.Citation21,Citation25 PET scans can be used as an alternative to CT imaging.Citation28 Other imaging such as bone scans should be performed on a symptomatic basis. Patients with functional tumors should have hormone levels measured every 3 months as a means of early detection of tumor recurrence.Citation21 A novel follow-up method currently under investigation is the use of urine steroid metabolomics, which the EURINE-ACT study is currently assessing as a technique to detect recurrence in comparison to imaging.Citation29
Recurrence rates and the role of specialist centers
ACC recurs commonly after complete surgical resection with reported rates of 21%–91%.Citation7,Citation22,Citation23,Citation30,Citation31 The wide ranges of reported recurrences are likely due to variability with patient selection of each series. Most series reporting recurrence are retrospective, including patients who have been referred to specialist centers after the development of recurrence, thereby creating a selection bias. This was highlighted by the series of Fassnacht et al which compared Stage II ACC patients, who were followed up prospectively following surgery by a specialist unit, against a group of patients referred 4 months or more after surgery.Citation23 Patients referred at the time of initial surgery were found to have a recurrence rate of 30%, compared to 74% for patients referred later. This series also found improved 5-year survival rates of 96% in patients referred initially, compared to 55% in patients referred later. In this series, patients who were referred at an earlier point of time were more likely to receive adjuvant mitotane, and it is thought the survival benefit could be due to a combination of patient selection and the increased use of mitotane. There is additional evidence that treatment in a high-volume center (defined by number of ACC cases treated each year, with 0.8 indicating a high volume center) may also improve treatment and survival.Citation32
If available, treatment in a specialist center is important. ACC is rare, and this low incidence makes it difficult for individual medical centers to gain experience in its treatment. The advent of specialist centers has allowed for the development of international ACC study collaborations and led to prospective trials, such as the First International Randomized trial in locally advanced and Metastatic Adrenocortical Carcinoma Treatment (FIRM-ACT) trial.Citation53 These collaborative efforts are leading to a greater knowledge of the natural history and management of ACC and improving treatment.
ACC can recur at any time, with most recurrences occurring in the first 2 years following surgery, with 40% of patients relapsing in this time.Citation31 After complete resection, more than 50% of patients will develop recurrence within 5 years.Citation8,Citation33
Locoregional recurrence comprises 19%–60% of total recurrences reported.Citation34–Citation36
Approximately 25% of patients have isolated locoregional recurrence.Citation34 Locoregional recurrence can involve the pancreas, spleen, liver, diaphragm, and retroperitoneum.Citation37
Systemic recurrences are most commonly detected in the lungs and liver with reported rates of 39%–65% total recurrences. Citation7,Citation35,Citation37 Around 25% of systemic recurrences have been reported in lymph nodes, and 15% reported in bone.Citation37
Management of recurrent ACC
When deciding on management, it is essential to consider the underlying tumor biology of ACC for each individual patient. ACC is an aggressive malignancy with a varied and heterogeneous natural history, and its treatment, such as extensive surgery, can carry considerable morbidity. Tumor biology is assessed by clinical judgment; it has been suggested that a minimum recurrence-free period of 6–12 months should be used to select patients who are likely to benefit from further surgery.Citation26,Citation38 Patients who have developed recurrence within 3 months of surgical resection, have rapidly progressive symptoms, or a lactate dehydrogenase level of >1000 units/L indicate rapidly progressive ACC and are unlikely to respond to current treatment.Citation1 The management of recurrent disease will be discussed for locoregional (adrenal bed) and systemic disease recurrence.
Locoregional recurrence
Surgery
With isolated locoregional recurrence, repeat surgery in selected patients can lead to improved survival.Citation31,Citation33 An aggressive surgical approach to achieve complete resection (R0) is advisable in patients who are fit for reoperation.Citation34 In a recent large series review, Datrice et al have shown that resection for recurrent disease is safe and of benefit in patients with a disease-free interval of greater than 12 months.Citation38 The surgical principles during reoperation are the same as those during the index procedure, with the aim to completely resect all disease, as incomplete resection leads to poorer survival outcomes.Citation7
If complete resection is not possible, debulking of tumors offers little benefit, but may be considered in selected patients prior to adjuvant therapy.Citation21 Debulking surgery is of most benefit in patients with functional tumors not controlled by medical treatment.
For patients with isolated locoregional recurrence not amenable to a likely R0 resection, neo-adjuvant combined chemotherapy should be offered with the aim of complete resection if there is a response to treatment.
Surgery should be undertaken in a specialist center by an experienced endocrine surgeon in consultation with a multidisciplinary team.Citation27 An open surgical approach is recommended for reoperation for locoregional recurrence due to the risk of tumor spillage, while minimally invasive surgery is inappropriate in this setting.Citation39
Radiotherapy
Radiotherapy remains a controversial subject in the treatment of ACC and has traditionally been reserved for situations of palliative therapy.Citation40 There has been limited evidence and no clear consensus guidelines in the specific role of neo-adjuvant or adjuvant radiotherapy.Citation21 The proximity of the adrenal bed to sensitive organs such as the kidney, liver, spinal cord, and small bowel has made treatment difficult, especially with older radiotherapy techniques.Citation41
Despite this, radiotherapy should be considered in patients with locoregional recurrence. Most evidence for radiotherapy is in regards to adjuvant radiotherapy. The evidence is conflicting; some series have demonstrated that patients who received adjuvant radiotherapy to the resection bed were less likely to develop locoregional recurrence,Citation35 while other specialist centers have found no difference with the use of adjuvant radiotherapy.Citation42 Guidelines proposed by the German ACC consortium recommend commencement of adjuvant radiotherapy within 3 months of surgery for patients with microscopically involved or inderterminate resection margins and stage III disease regardless of resection status. In addition, radiotherapy should be considered for tumors greater than 8 cm, with a Ki-67 Index > 10% or invasion of adjacent vasculature.Citation43
In a retrospective series over a 20 year period of 58 patients with 64 treatment instances of ACC, it was found that a 4.7 times higher risk of local recurrence was associated with a lack of radiotherapy, compared to treatment regimens that involved radiotherapy after surgical resection; however there was no difference in overall survival.Citation44 This study had a number of limitations including a mix of treatment episodes, with 37 treatments for primary ACC and 27 for recurrent disease. Treatments involved surgery alone in 38 instances; ten instances were for surgery with adjuvant radiotherapy, and 16 for definitive radiotherapy for unresectable disease.
Radiotherapy has been shown to be effective in a palliative setting, especially to symptomatic bone, brain, and inferior vena cava disease.Citation41,Citation43,Citation45
Given the conflicting evidence, the role of radiotherapy is yet to be elucidated by multicenter prospective trials. Until this data is available, radiotherapy should be considered after reoperation for locoregional control and for definitive treatment in recurrence not amenable to surgical resection.
Radiofrequency ablation
Percutaneous image-guided radiofrequency ablation (RFA) has appeal in delivering a minimally invasive, locally effective treatment, especially in patients who are not candidates for reoperation.
Available evidence has shown that RFA can produce effective, short-term local control of primary ACC in an adjuvant setting for tumors less than 50 mm in size, that are not near sensitive tissues or large blood vessels.Citation46 RFA has been demonstrated in a small case series of 15 ACC recurrences to be well tolerated, with 53% of patients demonstrating decrease in tumor size or loss of enhancement on imaging.Citation46 Smaller tumors fared better (<50 mm), with up to 67% demonstrating complete ablation.
RFA in combination with surgical resection may allow for better disease control in the setting of local and isolated systemic recurrence.Citation38 However, side effects of bleeding, infection, and injury to adjacent organs can occur. Nevertheless, with advancing technology, RFA has the potential to have a role in treatment options of recurrent ACC in selected patients.Citation38
Systemic recurrence
Patients who develop systemic disease have a poor prognosis, with a 5-year survival rate of less than 15%.Citation6,Citation22,Citation31,Citation47 Conventional medical treatment is mitotane, with or without chemotherapy, and adrenal hormone control. However, response rates to medical treatment remain disappointing.Citation3 There is a limited role for surgical resection in a small number of selected patients. Given the limited treatment options and poor prognosis of ACC, novel treatments and clinical trials are important components in the treatment of systemic disease.
Medical treatment
Conventional or first line treatments can be mitotane alone or mitotane in combination with chemotherapy. European Society for Medical Oncology guidelines recommend combination chemotherapy and mitotane for patients with inoperable ACC with high tumor volume and rapid disease, whilst mitotane alone can be used initially for patients with low tumor volume, slow progression, or those unfit for chemotherapy.Citation3
Mitotane
Patients who have not previously received systemic treatment should receive high dose mitotane as a first line treatment.Citation1 High dose mitotane aims for a blood level of 14–20 mg/L. Mitotane blood levels should be checked following 3 weeks of treatment, and if plasma levels remain low (<7 mg/L), the dose should be adjusted and cytotoxic chemotherapy considered. Supportive treatment with hydrocortisone substitution is required to cover adrenal insufficiency, and fludrocortisone may be required depending on blood pressure, serum potassium levels, and plasma renin activity.Citation3 The effect of mitotane to induct cytochrome P450 3A4 means that up to half of administered hydrocortisone can be rapidly inactivated, requiring high steroid doses to obtain adequate cover.Citation48 Mitotane inhibits 5α-reductase and androgen replacement may also be required.Citation48 Liver function tests, thyroid function, and blood lipid levels need to be monitored while patients are receiving mitotane.Citation3
Approximately one third of patients will receive a response but generally there is little increase in survival rates,Citation25,Citation49,Citation50 although there are reported isolated cases of long-term disease controlCitation51 and rare cases of disease remission.Citation52 For functional tumors, an additional benefit of mitotane is that it will control hormone excess in most patients.Citation50
Chemotherapy plus mitotane
Patients who have rapidly progressing disease should receive combination treatment as a first line treatment; however, the response rates are poor, with few patients receiving long term benefit.Citation1 Chemotherapy used in ACC as conventional treatment includes either streptozocin, or the combination etoposide, doxorubicin, and cisplatin (EDP). These two treatments were compared in the FIRM-ACT study.Citation53 A response rate of 23% was found in the EDP-mitotane group, versus 9% in the streptozocin-mitotane group. The EDP-mitotane group had a 5 month progression-free survival advantage compared to 2 months for the Streptozocin-mitotane group, but no significant overall survival benefit. Despite the poor response, this trial is important as it is the largest prospective trial (304 patients) undertaken on ACC and provides a baseline against which further novel treatments can be compared. Given these results, patients should receive EDP and mitotane as a first line combination treatment.Citation5
Patients receiving mitotane with or without chemotherapy should be assessed at two-monthly intervals for tumor progression. Patients who show tumor regression or stable disease should be considered for surgical resection or continuation of therapy. Patients with progressive disease should consider other chemotherapy regimens or be enrolled in a clinical trial.
Salvage chemotherapy treatments
There are currently no established second or third line chemotherapy regimens for systemic disease.Citation54 However, a phase-II trial of gemcitabine plus capecitabine has shown some encouraging results, with 46% of patients having stable disease for more than 4 months,Citation55 and this has been suggested as a possible second/third line regimen.Citation1 Patients should be considered for clinical trials if they have progressive disease with conventional treatment.
Medical treatment of steroid excess
Patients with systemic disease must undergo monitoring and control of steroid hormone excess, as they can die from infections and hypercortisolism, rather than from tumor burden. This is especially important in the setting of chemotherapy-induced immunosuppression.Citation28 Adrenal enzyme inhibition can be achieved with the use of mitotane, ketoconazole, metyrapone, etomidate, or mifepristone. These medications require close monitoring and frequent dose adjustments.Citation56
Surgery and other local treatments
Surgical resection has a role in selected patients with systemic recurrence of ACC. Patients with metastatic disease amenable to complete surgical resection, for example liver or lung metastasis, should be considered for resection even if it is required to be completed over two stages.Citation21,Citation57,Citation58 Complete surgical resection of recurrent disease in a medically fit and symptomatic patient can be of benefit and is associated with long-term survival in some patients.Citation7,Citation59 Any decision in offering radical surgical treatment is dependent on the tumor biology and will not offer any benefit for patients with rapidly progressive tumors.Citation38
The role for debulking surgery in systemic ACC is more limited and should only be considered for patients with uncontrollable hormone production. In this situation, debulking surgery can provide effective symptom palliation.Citation1,Citation7
Radiotherapy and other ablation techniques (RFA/laser) also have a limited role in systemic recurrence but can be useful for palliation for local symptomatic and hormone production control in selected cases.Citation43,Citation60
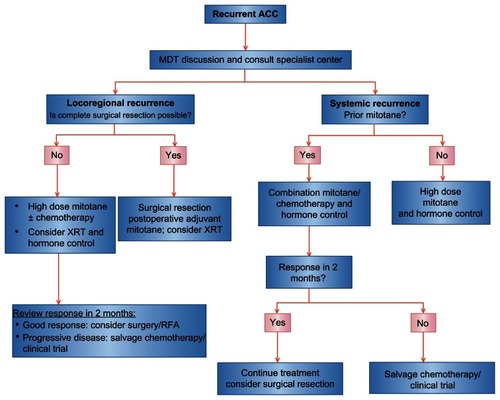
A suggested plan of management for recurrent ACC is shown in .
Novel and future treatments
The poor survival results with systemic ACC demonstrates the need for improved treatment options, and a number of novel and targeted therapies have been studied with mixed results as discussed below.
Tyrosine kinase inhibitors
Treatments trialled have included targeted treatments against epidermal growth factor receptor (EGFR). EGFR is overexpressed in most ACCs, making it a useful target for treatment;Citation61 however, targeted treatment with the tyrosine kinase inhibitor erlotinib plus gemcitabine showed a limited response as a salvage treatment, with a response only seen in one out of ten patients.Citation62 Poor response was also seen with the use of imatinib.Citation63 Sunitinib, which targets several tyrosine kinase inhibitors, has been shown to have a modest response, with some patients achieving stable disease in a phase-II trial.Citation64 This trial showed worse results with concomitant mitotane, possibly due to reduced serum sunitinib levels caused by mitotane induced cytochrome P450-3A4 activity.
More promising results have been seen with the targeting of insulin-like growth factor 1 receptor (IGF-1R). IGF- 2, which is over-expressed in ACCs, is known to signal predominantly through IGF-1R.Citation65 Study of the oral tyrosine kinase inhibitor (OSI-906) which targets IGF-1R has shown promising results, with stabilization of disease seen in five out of 16 patients.Citation66 This agent is currently being evaluated by the GALACCTIC clinical trial.Citation67
Angiogenesis inhibitors
Due to the highly vascular nature of ACC, vascular endothelial growth factor (VEGF) has also been assessed as a treatment target; however, a study of bevacizumab used in combination with capecitabine showed no response in ten patients as a salvage treatment, with severe toxicity seen in two patients.Citation68
Mammalian target of rapamycin signaling
Another target of interest in ACC is mammalian target of rapamycin (mTOR) due to its relationship with IGF-1R. mTOR is a downstream signaling node for a number of receptor tyrosine kinases including IGF-1R; however, inhibition of mTOR alone leads to activation of other tumorigenic pathways, thereby limiting its use as a single agent for the treatment of malignancy.Citation69 An exploratory study of the use of everolimus, a rapamycin analog, has shown no clinical response.Citation70 Combination treatment targeting mTOR showed more promise in a recent phase-I trial using the IGF-1R antibody cixutumumab combined with temsirolimus, where 42% of patients achieved stable disease for a minimum of 6 months.Citation71
Future treatments
Other targets of interest include the Wnt/β-catenin pathway, interleukin-13 receptor alpha2, microRNA therapies, and demethylating agents.Citation19,Citation72–Citation74
Conclusion
Recurrence of ACC remains a difficult disease to treat, but with a multidisciplinary approach it is possible for some patients to achieve long-term disease control and survival. As ACC is a rare disease, many patients are only referred to specialist centers following the development of recurrence. To achieve better outcomes, patients should be referred to, or advice sought from, a specialist center at the initial suspicion of ACC. The poor response rates to current systemic treatment offer ACC as a model to researchers to identify new treatment targets and assess novel treatments to improve outcomes in this difficult disease.
Disclosure
The authors report no conflicts of interest in this work.
References
- FassnachtMLibéRKroissMAllolioBMedscapeAdrenocortical carcinoma: a clinician’s updateNat Rev Endocrinol20117632333521386792
- WajchenbergBLAlbergaria PereiraMAMedoncaBBAdrenocortical Carcinoma: clinical and laboratory observationsCancer200088471173610679640
- BerrutiABaudinEGelderblomHAdrenal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-upAnn of Oncol201223Suppl 7vii131vii13822997446
- KebebewEReiffEDuhQYClarkOHMcMillanAExtent of disease at presentation and outcome for adrenocortical carcinoma: have we made progress?World J Surg200630587287816680602
- KirschnerLSThe next generation of therapies for adrenocortical cancersTrends in Endocrinol Metab201223734335022626690
- AbivenGCosteJGroussinLClinical and biological features in the prognosis of adrenocortical cancer: poor outcome of cortisol-secreting tumors in a series of 202 consecutive patientsJ Clin Endocrinol Metab20069172650265516670169
- SchulickRDBrennanMFLong-term survival after complete resection and repeat resection in patients with adrenocortical carcinomaAnn Surg Oncol19996871972610622498
- StojadinovicAGhosseinRAHoosAAdrenocortical carcinoma: clinical, morphologic, and molecular characterizationJ Clin Oncol200220494195011844815
- FassnachtMAllolioBClinical management of adrenocortical carcinomaBest Pract Res Clin Endocrinol Metab200923227328919500769
- LauSKWeissLMThe Weiss system for evaluating adrenocortical neoplasms: 25 years laterHum Pathol200940675776819442788
- AubertSWacrenierALeroyXWeiss system revisited: a clinicopathologic and immunohistochemical study of 49 adrenocortical tumorsAm J Surg Pathol200226121612161912459628
- SoonPSHGillAJBennDEMicroarray gene expression and immunohistochemistry analyses of adrenocortical tumors identify IGF2 and Ki-67 as useful in differentiating carcinomas from adenomasEndocr Relat Cancer200916257358319218281
- SchmittAASaremaslaniPPSchmidSSRearrangements at the 11p15 locus and overexpression of insulin-like growth factor-II gene in sporadic adrenocortical tumorsJ Clin Endocrinol Metab1994786144414537911125
- MorimotoRSatohFMurakamiOImmunohistochemistry of a proliferation marker Ki67/MIB1 in adrenocortical carcinomas: Ki67/ MIB1 labeling index is a predictor for recurrence of adrenocortical carcinomasEndocr J20085514955 Available at: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=18187873&retmode=ref&cmd=prlinksAccessed January 14, 201318187873
- GicquelCCBertagnaXXGastonVVMolecular markers and long-term recurrences in a large cohort of patients with sporadic adrenocortical tumorsCancer Res200161186762676711559548
- AssieGGiordanoTJBertheratJGene expresion profiling in adrenocortical neoplasiaMol Cell Endocrinol20123511111117 Available at: http://www.sciencedirect.com/science/article/pii/S0303720711006162Accessed February 14, 201322056416
- SoonPSLibéRBennDELoss of heterozygosity of 17p13, with possible involvement of ACADVL and ALOX15B, in the pathogenesis of adrenocortical tumorsAnn Surg2008247115716418156936
- PattersonEEHollowayAKWengJFojoTKebebewEMicroRNA profiling of adrenocortical tumors reveals miR-483 as a marker of malignancyCancer201011781630163921472710
- RechacheNSWangYStevensonHSDNA methylation profiling identifies global methylation differences and markers of adrenocortical tumorsJ Clin Endocrinol Metab2012976E1004E101322472567
- de ReyniesAAssieGRickmanDSGene expression profiling reveals a new classification of adrenocortical tumors and identifies molecular predictors of malignancy and survivalJ Clin Oncol20092771108111519139432
- SchteingartDEDohertyGMGaugerPGManagement of patients with adrenal cancer: recommendations of an international consensus conferenceEndocr Relat Cancer200512366768016172199
- TerzoloMAngeliAFassnachtMAdjuvant mitotane treatment for adrenocortical carcinomaN Engl J Med2007356232372238017554118
- FassnachtMJohanssenSFenskeWImproved survival in patients with stage II adrenocortical carcinoma followed up prospectively by specialized centersJ Clin Endocrinol Metab201095114925493220668036
- HuangHFojoTAdjuvant mitotane for adrenocortical cancer – a recurring controversyJ Clin Endocrinol Metab200893103730373218842984
- AllolioBFassnachtMAdrenocortical carcinoma: clinical updateJ Clin Endocrinol Metab20069162027203716551738
- FassnachtMAllolioBWhat is the best approach to an apparently nonmetastatic adrenocortical carcinoma?Clin Endocrinol2010735561565
- University of Turin, ItalyEfficacy of Adjuvant Mitotane Treatment (ADIUVO)ClinicalTrials.gov [website on the Internet]Bethesda, MDUS National Library of Medicine2008 [updated 2011]. Available from: http://clinicaltrials.gov/show/NCT00777244. NLM identifier: NCT00777244Accessed January 10, 2013
- LacroixAApproach to the patient with adrenocortical carcinomaJ Clin Endocrinol Metab201095114812482221051577
- ArltWBiehlMTaylorAEUrine steroid metabolomics as a biomarker tool for detecting malignancy in adrenal tumorsJ Clin Endocrinol Metab201196123775378421917861
- KendrickMLLloydREricksonLAdrenocortical carcinoma: surgical progress or status quo?Arch Surg200113654354911343545
- CrucittiFBellantoneRFerranteABoscheriniMCrucittiPGroup TAIRSThe Italian registry for Adrenal Cortical Carcinoma: analysis of a multiinstitutional series of 129 patients. The ACC Italian Registry Study GroupSurgery19961191611708571201
- LombardiCPRaffaelliMBoniardiMAdrenocortical carcinoma: effect of hospital volume on patient outcomeLangenbecks Arch Surg2011397220120722069043
- PommierRFBrennanMFAn eleven-year experience with adrenocortical carcinomaSurgery19921129639711455321
- BellantoneRFerranteABoscheriuiMRole of reoperation in recurrence of adrenal cortical carcinoma: Results from 188 cases collected in the Italian National Registry for Adrenal Cortical CarcinomaSurgery19971226121212189426440
- FassnachtMHahnerSPolatBEfficacy of adjuvant radiotherapy of the tumor bed on local recurrence of adrenocortical carcinomaJ Clin Endocrinol Metab200691114501450416895957
- LombardiCPRaffaelliMDe CreaCOpen versus endoscopic adrenalectomy in the treatment of localized (stage I/II) adrenocortical carcinoma: results of a multiinstitutional Italian surveySurgery201215261158116423068084
- BrennanMFAdrenocortical CarcinomaCA Cancer J Clin1987376349365
- DatriceNMLanganRCRipleyRTOperative management for recurrent and metastatic adrenocortical carcinomaJ Surg Oncol2011105770971322189845
- MillerBSGaugerPGHammerGDDohertyGMResection of adrenocortical carcinoma is less complete and local recurrence occurs sooner and more often after laparoscopic adrenalectomy than after open adrenalectomySurgery201215261150115723158185
- PercarpioBKnowltonAHRadiation therapy of adrenal cortical carcinomaActa Radiol Ther Phys Biol197615428829262490
- LebastchiAHKunstmanJWCarlingTAdrenocortical Carcinoma: Current Therapeutic State-Of-The-ArtJ Oncol20122012111
- HabraMAEjazSFengLA Retrospective cohort analysis of the efficacy of adjuvant radiotherapy after primary surgical resection in patients with adrenocortical carcinomaJ Clin Endocrinol Metab201398119219723150683
- PolatBFassnachtMPfreundnerLRadiotherapy in adrenocortical carcinomaCancer2009115132816282319402169
- SabolchAFengMGriffithKHammerGDohertyGBen-JosefEAdjuvant and Definitive Radiotherapy for Adrenocortical CarcinomaInt J Radiat Oncol Biol Phys20118051477148420675074
- MilgromSAGoodmanKAThe role of radiation therapy in the management of adrenal carcinoma and adrenal metastasesJ Surg Oncol2012106564765022488095
- WoodBJAbrahamJHvizdaJLAlexanderHRFojoTRadiofrequency ablation of adrenal tumors and adrenocortical carcinoma metastasesCancer200397355456012548596
- IcardPGoudetPCharpenayCAdrenocortical carcinomas: surgical trends and results of a 253-patient series from the French Association of Endocrine Surgeons study groupWorld J Surg200125789189711572030
- ChortisVTaylorAESchneiderPMitotane therapy in adrenocortical cancer induces CYP3A4 and inhibits 5α-reductase, explaining the need for personalized glucocorticoid and androgen replacementJ Clin Endocrinol Metab201398116117123162091
- HaakHRHermansJvan deVeldeCJHOptimal treatment of adrenocortical carcinoma with mitotane: results in a consecutive series of 96 patientsBr J Cancer19946959479518180029
- HahnerSFassnachtMMitotane for adrenocortical carcinoma treatmentCurr Opin Investig Drugs200564386394
- KornelyESchlagheckeRComplete remission of metastasized adrenocortical carcinoma under o,p’-DDDExp Clin Endocrinol1994102150538005209
- IliasIAlevizakiMPhilippouGAnastasiouESouvatzoglouASustained remission of metastatic adrenal carcinoma during long follow upJ Endocrinol Invest200124753253511508789
- FassnachtMTerzoloMAllolioBCombination chemotherapy in advanced adrenocortical carcinomaN Engl J Med2012366232189219722551107
- FassnachtMKreisslMCWeismannDAllolioBNew targets and therapeutic approaches for endocrine malignanciesPharmacol Ther2009123111714119374919
- SperonePFerreroADaffaraFGemcitabine plus metronomic 5-fluorouracil or capecitabine as a second-/third-line chemotherapy in advanced adrenocortical carcinoma: a multicenter phase II studyEndocr Relat Cancer201017244545320410174
- VeytsmanINiemanLFojoTManagement of Endocrine Manifestations and the Use of Mitotane As a Chemotherapeutic Agent for Adrenocortical CarcinomaJ Clin Oncol200927274619462919667279
- GaujouxSAl-AhmadieHAllenPJResection of Adrenocortical Carcinoma Liver Metastasis: Is it Justified?Ann Surg Oncol20121982643265122526905
- Winkel denJOPfannschmidtJMuleyTMetastatic adrenocortical carcinoma: results of 56 pulmonary metastasectomies in 24 patientsAnn Thorarc Surg201192619651970
- MihaiRIacoboneMMakayOOutcome of operation in patients with adrenocortical cancer invading the inferior vena cava – a European Society of Endocrine Surgeons (ESES) surveyLangenbecks Arch Surg2011397222523122134748
- PacellaCMStasiRBizzarriGPercutaneous laser ablation of unresectable primary and metastatic adrenocortical carcinomaEur J Radiol2008661889417498906
- AdamPHahnerSHartmannMEpidermal growth factor receptor in adrenocortical tumors: analysis of gene sequence, protein expression and correlation with clinical outcomeMod Pathol201023121596160420693985
- QuinklerMHahnerSWortmannSTreatment of advanced adrenocortical carcinoma with erlotinib plus gemcitabineJ Clin Endocrinol Metab20089362057206218334586
- GrossDJMunterGBitanMThe role of imatinib mesylate (Glivec) for treatment of patients with malignant endocrine tumors positive for c-kit or PDGF-REndocr Relat Cancer200613253554016728580
- KroissMQuinklerMJohanssenSSunitinib in refractory adrenocortical carcinoma: a phase II, single-arm, open-label trialJ Clin Endocrinol Metabolism2012971034953503
- TaconLJPrichardRSSoonPSRobinsonBGClifton-BlighRJSidhuSBCurrent and Emerging Therapies for AdvancedAdrenocortical CarcinomaOncologist2011161364821212436
- MacaulayVMMiddletonMREckhardtSGPhase I study of OSI-906, dual tyrosine kinase inhibitor of insulin-like growth factor- 1 receptor (IGF-1R) and insulin receptor (IR) in combination with erlotinib (E) in patients with advanced solid tumorsJ Clin Oncol201028153016
- Astellas Pharma IncA Study of OSI-906 in Patients With Locally Advanced or Metastatic Adrenocortical Carcinoma (GALACCTIC)ClinicalTrials.gov [website on the Internet]Bethesda, MDUS National Library of Medicine2009 [updated 2012]. Available from http://clinicaltrials.gov/show/NCT00924989. NLM identifier NCT00924989Accessed January 10, 2013
- WortmannSQuinklerMRitterCBevacizumab plus capecitabine as a salvage therapy in advanced adrenocortical carcinomaEur J Endocrinol2010162234935619903796
- MemmottRMDennisPAAkt-dependent and -independent mechanisms of mTOR regulation in cancerCell Signal200921565666419166931
- FraenkelMGueorguievMBarakDSalmonAGrossmanABGrossDJEverolimus therapy for progressive adrenocortical cancerEndocrine Epub February 16, 2013
- NaingALoRussoPFuSInsulin growth factor receptor (IGF-1R) antibody cixutumumab combined with the mTOR inhibitor temsirolimus in patients with metastatic adrenocortical carcinomaBr J Cancer2013108482683023412108
- TissierFCavardCGroussinLMutations of beta-catenin in adrenocortical tumors: activation of the wnt signaling pathway is a frequent event in both benign and malignant adrenocortical tumorsCancer Res200565177622762716140927
- IorioMVCroceCMMicroRNA dysregulation in cancer: diagnostics, monitoring and therapeutics. A comprehensive reviewEMBO Mol Med20124314315922351564
- JainMZhangLHeMInterleukin-13 receptor alpha2 is a novel therapeutic target for human adrenocortical carcinomaCancer2012118225698570822570059