Abstract
Purpose
In asymptomatic patients with Stage IV colorectal cancer, the debate continues over the efficacy of primary resection compared to chemotherapy alone. The aim of this study was to define the optimal management for asymptomatic patients with colorectal cancer and unresectable liver metastases.
Patients and methods
Patients receiving elective surgery (n = 17) were compared to patients receiving chemotherapy only (n = 31). Data concerning patients’ demographics, location of primary tumor, comorbidities, performance status, Child–Pugh score, extension of liver metastases, size of primary, and other secondary locations were collected.
Results
Thirty-day mortality after chemotherapy was lower than that after surgical resection (19.3% versus 29.4%; not significant). In patients with >75% hepatic involvement, mortality at 1 month was higher after receiving surgical treatment than after chemotherapy alone (50% versus 25%). In patients with <75% hepatic involvement, 30-day mortality was similar in both groups (not significant). Thirty-day mortality in patients with Stage T3 was lower in those receiving chemotherapy (16.7% versus 30%; not significant). Overall survival was similar in both groups. The risk of all-cause death after elective surgery (2.1) was significantly higher than in patients receiving chemotherapy only (P = 0.035).
Conclusion
This study demonstrated that in palliative treatment of asymptomatic unresectable Stage IV colorectal cancer, the overall risk of death was significantly higher after elective surgery compared to patients receiving chemotherapy alone. However, in the literature, there is no substantial difference between these treatments. New studies are required to better evaluate outcomes.
Introduction
Colorectal cancer (CRC) represents more than 9% of all new cancer cases worldwide,Citation1 and in 2002, more than 1 million new cases were diagnosed. In the US, the incidence of this malignancy has decreased by 3.0% in men and 2.2% in women in 1998–2006, with a reduction in male mortality of 3.9% in 2002–2006.Citation2 However, an increased incidence of CRC has occurred in Europe, particularly in the southeastern countries.Citation3 Among patients with newly diagnosed CRC, 20%–30% have liver metastases,Citation4,Citation5 10%–15% have peritoneal carcinomatosis,Citation6,Citation7 and 10%–25% have lung metastases.Citation8–Citation10
According to the European Society for Medical Oncology guidelines, hepatectomy for patients with metastatic CRC is to be performed only with curative intent following the criteria of oncological radicality and if it is indicated that there is enough remnant liver parenchyma following the resection (>30%) and/or in the absence of unresectable multivisceral spreading of the disease or carcinomatosis.Citation11,Citation12
Treatment of advanced stages of CRC, especially in patients not eligible for curative surgery, consists of medical therapies. The availability of new polychemotherapeutic regimens (5-fluorouracil, folinic acid, and oxaliplatin; FOLFOX) in combination with biologic agents (monoclonal antibodies such as bevacizumab, cetuximab, and panitumumab) has markedly improved the median survival of patients in advanced stages, with no increase in the incidence of complications.Citation13–Citation16
In a retrospective study, 93% of patients with Stage IV CRC on chemotherapy did not develop complications related to the primary tumor.Citation17 In patients with obstructive tumor, the use of stents allowed them to be quickly started on systemic chemotherapy.Citation18,Citation19 Nevertheless, in asymptomatic patients with Stage IV CRC, the debate continues over the efficacy of primary neoplasia resection compared to chemotherapy alone.Citation20
The aim of this study was to determine if there was any improvement in overall survival and a reduction of posttreatment mortality after resection of the primary tumor, with respect to nonoperative treatment in patients with Stage IV CRC and unresectable liver metastases.
Patients and methods
Data on patients with synchronous unresectable liver metastases from CRC who consecutively underwent palliative therapy between January 2010 and December 2011 were retrospectively reviewed. Among patients with rectal cancer, only those with intraperitoneal localization were selected because extraperitoneal rectal cancer with unresectable liver metastases is best treated with chemotherapy and radiation therapy as an effective palliative treatment. None of the 48 patients included in this multicentric study had bowel obstruction, bleeding, or perforation.
Seventeen patients (operative group) underwent elective palliative surgery consisting of colonic resection, 14 of whom had open surgery by median laparotomy, two with primary tumor in rectosigmoid colon underwent laparoscopic colorectal dissection followed by suprapubic laparotomy in which total mesorectal excision and colorectal anastomosis were performed, and one with right CRC had laparoscopic exploration followed by total laparotomic right colectomy due to local extension of the disease. Seven of the patients who underwent elective surgery had neoplastic stenosis; however, despite this, obstinate constipation was reported.
Thirty-one patients (nonoperative group) received chemotherapy alone, leaving the primary tumor in place, ie, nonoperative management (NOM). In this group, 24 patients received FOLFOX plus bevacizumab as first-line therapy. FOLFOX only was administered to the remaining seven patients who were not able to tolerate the combination. Switching to second-line therapy was not needed. Administration of bevacizumab was suspended at 3 months in six patients because of drug-related toxicity or worsening of their condition and in two patients because disease control was reached.
Age, comorbidities, and performance status, and the risk of complications (obstruction and perforation) were the criteria used to choose between the resection of the primary tumor and NOM (). Thirty-day overall mortality and overall survival were the primary and secondary endpoints assessed.
Table 1 Clinical characteristics of the patients according to treatment
Statistics on the clinical characteristics of patients were calculated by Fisher’s exact test for 2 × 2 comparisons and by Pearson’s Chi-squared test for comparisons greater than 2×2 (95% confidence interval, á = 0.05). A multivariate analysis for 30-day mortality and overall survival was performed by Cox logistic regression.
The mean age of the patients was lower in the operative group (). Local extension of the disease was determined by computed tomography scan and pathological examination in the operative group, and by computed tomography scan only in the NOM group ().
Results
Overall mortality within 30 days of commencing palliative chemotherapy was lower than that of surgical resection (five versus six), even though this outcome was not statistically significant. In the operative group, three patients died of liver failure presenting hepatorenal syndrome, two patients died of heart failure, and six patients had postoperative complications (three wound infections, one urinary tract infection, and two with bronchopneumonia). Of the six patients who received chemotherapy only, four died of hepatorenal syndrome and two died of heart failure.
In patients with >75% of the parenchyma replaced by metastases, mortality after treatment was found to be 50% if on elective surgery and 25% if on chemotherapy alone. The reported difference between the two groups of patients for <75% hepatic involvement of the volume was minimal (50%–75%: 2/6 versus 2/10 and <50%: 2/9 versus 2/13 for elective surgery and NOM, respectively) ( and ).
Table 2 Factors affecting 30-day overall mortality and overall survival after elective surgery
Table 3 Factors affecting 30-day overall mortality and overall survival after nonoperative management
Thirty-day mortality in patients with Stage T3 was lower in the group receiving chemotherapy, although this outcome was not statistically significant (3/10 versus 2/12 for elective surgery and NOM, respectively). In patients with Stage T4, local extension of the tumor did not appear to affect 30-day mortality since the difference between the two groups was minimal (2/7 versus 4/19 for elective surgery and NOM, respectively) ( and ).
Secondary localizations in addition to hepatic replacement did not affect 30-day mortality. The two groups were not comparable because not all patients presented extrahepatic metastases ( and ).
Of the patients who underwent elective surgery, eleven started palliative chemotherapy (six received FOLFOX plus bevacizumab and five received FOLFOX only) and six died of disease or complications before starting it. The mean interval between surgery and starting postoperative chemotherapy was 5 weeks.
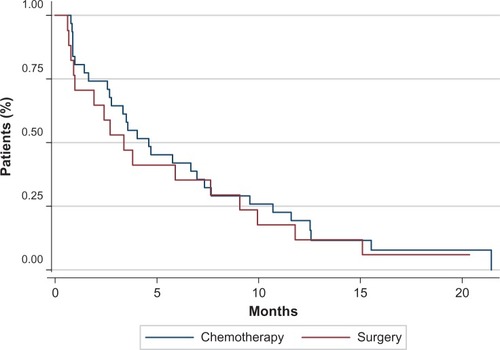
The mean and median follow-up was 8 months and 7 months, respectively. The mean and median overall survival of the patients receiving elective surgery was 6 months and 4 months, respectively. For the patients who underwent palliative chemotherapy only, the mean and median overall survival was 7 months and 5 months, respectively. The 1-year overall survival rate was 17.6% versus 19.4% for elective surgery and chemotherapy alone, respectively ().
Multivariate analysis of the data demonstrated that there were no statistically significant differences in 30-day mortality. On the other hand, data analysis using the Cox regression model demonstrated that the risk of all-cause death was significantly higher after elective surgery (2.1; 95% confidence interval 1.06–4.5; P = 0.035; adjusted to liver replacement nd other metastases) compared to patients receiving chemotherapy only ( and ).
Overall the two groups showed similar performance status. The difference between the two groups was greatest for American Society of Anesthesiologists I/ Eastern Cooperative Oncology Group 0 (). Furthermore, patients undergoing surgery had a better hepatic function since they had a smaller metastatic liver replacement than those receiving chemotherapy alone ().
Discussion
Resection of the primary tumor is necessary for patients with complications, whereas chemoradiotherapy in combination with targeted agents appears safe and seems a suitable alternative for patients without complications.Citation23 After resection of the primary tumor, adjuvant therapy should be promptly undertaken as a delay may decrease its efficacy.Citation24 According to Galizia et al, this occurrence may be balanced by a better response rate to chemotherapy in selected patients before primary tumor debulking.Citation25 The current analysis doesn’t suggest that primary tumor resection is a safe and effective treatment of asymptomatic patients with Stage IV CRC when not radically resectable.
Liver tumor burden has been recognized as an independent risk factor for poor outcome, regardless of therapy. Thus, patients with extensive (>75%) hepatic tumor involvement carry an extremely unfavorable prognosis.Citation26 Hepatic parenchymal replacement is significantly related to survival. Hepatic tumor burden > 50% is related to poor overall survival.Citation27 Bilobar liver involvement is related with an even greater unfavorable prognosis.Citation28
In palliative treatment of uncomplicated patients affected by CRC with unresectable liver metastases, chemoradiotherapy combined with biological agents is a suitable alternative to surgical resection of the primary tumor.
Asymptomatic patients with a liver metastasis involving <50% of the parenchyma, when undergoing resection of the primary tumor, display a survival rate similar to patients on chemotherapy alone ( and ). In asymptomatic patients with a replaced liver volume of 50%–75%, surgery showed no benefits in terms of survival over NOM (posttreatment mortality 33.3% versus 20%), as recently shown by Kleespies et al.Citation27 This data is even more significant in patients with metastases involving >75% of the liver volume (posttreatment mortality 50% versus 25%) ( and ).
Local neoplastic extension is not an independent predictor of survival.Citation29 In the current study, it was demonstrated that in Stage T3 and T4 local extension of the primary tumor, elective surgery presents no benefit in terms of survival compared to NOM (posttreatment mortality Stage T3: 30% versus 16.7% and Stage T4: 28.6% versus 21%) ( and ).
Peritoneal carcinomatosis is an independent prognostic factor,Citation30 and it is also recognized as an important risk factor for obstruction.Citation31 In the current study, peritoneal carcinomatosis appeared not to influence posttreatment mortality.
The main bias of this study was the small number of patients analyzed in a retrospective way. With the exception of overall risk of death, which was higher after elective surgery, no significant difference in 30-day mortality and overall survival was found between the two groups of patients.
Conclusion
This study shows that in palliative treatment of asymptomatic unresectable Stage IV CRC, the risk of all-cause death was significantly higher after elective surgery compared to patients receiving chemotherapy only. However, in the literature, there is no substantial difference between these two treatments.Citation32 Therefore, it is crucial to undertake new studies to evaluate and compare the results in terms of quality of life in both groups of patients.
Disclosure
The authors report no conflicts of interest in this work.
References
- ParkinDMBrayFFerlayJPisaniPGlobal cancer statistics, 2002CA Cancer J Clin20055527410815761078
- EdwardsBKWardEKohlerBAAnnual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future ratesCancer2010116354457319998273
- FerlayJAutierPBoniolMHeanueMColombetMBoylePEstimates of the cancer incidence and mortality in Europe in 2006Ann Oncol200718358159217287242
- ManfrediSLepageCHatemCCoatmeurOFaivreJBouvierAMEpidemiology and management of liver metastases from colorectal cancerAnn Surg2006244225425916858188
- SimmondsPCPrimroseJNColquittJLGardenOJPostonGJReesMSurgical resection of hepatic metastases from colorectal cancer: a systematic review of published studiesBr J Cancer200694798299916538219
- DawsonLERussellAHTongDWisbeckWMAdenocarcinoma of the sigmoid colon: sites of initial dissemination and clinical patterns of recurrence following surgery aloneJ Surg Oncol198322295996823134
- ChuDZLangNPThomsonCOsteenPCWestbrookKCPeritoneal carcinomatosis in nongynecologic malignancy: a prospective study of prognostic factorsCancer19896323643672910444
- InoueMOhtaMIuchiKBenefits of surgery for patients with pulmonary metastases from colorectal carcinomaAnn Thorac Surg200478123824415223436
- LucenaJRReseccion de metastasis pulmonares en cancer colorectal [Resection of lung metastases from colorectal cancer]Cir Esp2005786362365 Spanish.16420862
- IwasakiAShirakusaTYamashitaYNoritomiTMaekawaTHamadaTCharacteristic differences between patients who have undergone surgical treatment for lung metastasis or hepatic metastasis from colorectal cancerThorac Cardiovasc Surg200553635836416311973
- Van CutsemENordlingerBCervantesAAdvanced colorectal cancer: ESMO clinical practice guidelines for treatmentAnn Oncol201021Suppl 5v93v9720555112
- CirocchiRTrastulliSBoselliCRadiofrequency ablation in the treatment of liver metastases from colorectal cancer [review]Cochrane Database Syst Rev20126CD00631722696357
- McCahillLEYothersGASharifSA phase II trial of 5-fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) chemotherapy plus bevacizumab (bev) for patients (pts) with unresectable stage IV colon cancer and a synchronous asymptomatic primary tumor: results of NSABP C-10 [abstract]J Clin Oncol20102815 Suppl3527
- BokemeyerCKohneCRougierPStrohCSchlichtingMVan CutsemECetuximab with chemotherapy (CT) as first-line treatment for metastatic colorectal cancer (mCRC): analysis of the CRYSTAL and OPUS studies according to KRAS and BRAF mutation status [abstract]J Clin Oncol201028Suppl 15350620567016
- OcvirkJBrodowiczTWrbaFCetuximab plus FOLFOX6 or FOLFIRI in metastatic colorectal cancer: CECOG trialWorld J Gastroenterol201016253133314320593498
- CostiRDi MauroDGiordanoPImpact of palliative chemotherapy and surgery on management of stage IV incurable colorectal cancerAnn Surg Oncol201017243244019936838
- PoultsidesGAServaisELSaltzLBOutcome of primary tumor in patients with synchronous stage IV colorectal cancer receiving combination chemotherapy without surgery as initial treatmentJ Clin Oncol200927203379338419487380
- KarouiMSopraniACharachonAPrimary chemotherapy with or without colonic stent for management of unresectable stage IV colorectal cancerEur J Surg Oncol2010361586419926243
- CirocchiRFarinellaETrastulliSSafety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysisSurg Oncol2013221142123183301
- DamjanovNWeissJHallerDGResection of the primary colorectal cancer is not necessary in nonobstructed patients with metastatic diseaseOncologist2009141096396919819916
- DrippsRDNew classification of physical statusAnesthesiology196324111
- OkenMMCreechRHTormeyDCToxicity and response criteria of the Eastern Cooperative Oncology GroupAm J Clin Oncol1982566496557165009
- MuratoreAZorziDBouzariHAsymptomatic colorectal cancer with un-resectable liver metastases: immediate colorectal resection or up-front systemic chemotherapy?Ann Surg Oncol200714276677017103261
- BenoistSPautratKMitryERougierPPennaCNordlingerBTreatment strategy for patients with colorectal cancer and synchronous irresectable liver metastasesBr J Surg20059291155116016035135
- GaliziaGLietoEOrdituraMFirst-line chemotherapy vs bowel tumor resection plus chemotherapy for patients with unresectable synchronous colorectal hepatic metastasesArch Surg2008143435235818427022
- KonyalianVRRosingDKHaukoosJSThe role of primary tumour resection in patients with stage IV colorectal cancerColorectal Dis20079543043717504340
- KleespiesAFuesslKESeelingerHDeterminants of morbidity and survival after elective non-curative resection of stage IV colon and rectal cancerInt J Colorectal Dis20092491097110919495779
- MikMDzikiLGalbfachPTrzcinskiRSygutADzikiAResection of the primary tumour or other palliative procedures in incurable IV stage colorectal cancer patients?Colorectal Dis2010127 Onlinee61e6719486103
- StillwellAPHoYHVeitchCSystematic review of prognostic factors related to overall survival in patients with stage IV colorectal cancer and unresectable metastasesWorld J Surg201135368469221181473
- KatohHYamashitaKKokubaYSurgical resection of stage IV colorectal cancer and prognosisWorld J Surg20083261130113718340483
- TebbuttNCNormanARCunninghamDIntestinal complications after chemotherapy for patients with unresected primary colorectal cancer and synchronous metastasesGut200352456857312631671
- CirocchiRTrastulliSAbrahaINon-resection versus resection for an asymptomatic primary tumour in patients with unresectable stage IV colorectal cancer [review]Cochrane Database Syst Rev20128CD00899722895981