Abstract
Syringocystadenoma papilliferum (SCAP) is an uncommon benign adnexal tumor of the skin. It is frequently seen in association with other benign adnexal lesions, such as nevus sebaceous, apocrine nevus, tubular apocrine adenoma, apocrine hidrocystoma, apocrine cystadenoma, and clear cell syringoma. The unusual reported locations of SCAP include the head and neck, the buttock, the vulva, the scrotum, the pinna, the eyelid, the outer ear canal, the forehead, the back, the scalp, the thigh, the nipple, the axilla, and the postoperative scar. The occurrence of SCAP in the right lower abdomen is distinctly uncommon. Herein, we report an unusual case of a 41-year-old man with SCAP occurring in the right lower abdomen that did not develop malignancy, despite a long disease course and an absence of medical treatment. The clinical and histopathologic features and the differential diagnosis of SCAP are also discussed.
Keywords:
Introduction
Syringocystadenoma papilliferum (SCAP) is a rare, benign adnexal tumor that, in 50% of cases, is present at birth or in early childhood, while in another 15%–30% of cases, develops during puberty.Citation1,Citation2 Although benign, its transition to basal cell carcinoma, metastatic adenocarcinoma, and ductal carcinoma may occur.Citation3,Citation4 SCAP often occurs in association with other benign adnexal lesions, such as nevus sebaceous,Citation5 apocrine nevus,Citation6 tubular apocrine adenoma,Citation7,Citation8 apocrine hidrocystoma, apocrine cystadenoma,Citation9 and clear cell syringoma.Citation10
According to Shams et al,Citation11 there have been 261 reported cases. Roughly 50% present at birth or in early childhood.Citation11 Most often, SCAP is asymptomatic. It can have a variable clinical presentation, appearing as a solitary papule or a linear arrangement of several papules. With increasing size, a more prominent papillary configuration develops, and the surface can become scabbed. Macroscopically, the mature lesion consists of clusters of generally pinkish-brown nodules, 2–10 mm in diameter, with an occasional central opening. During puberty, SCAP may increase in size and develop a crusted and papillomatous texture.Citation12 The most common location is the head and neck,Citation13–Citation15 and it is really rare to see SCAP located in the abdomen. We report here a fourth case of SCAP in the right lower abdomen that did not develop malignancy, despite a long disease course and an absence of medical treatment.
Case report
A 41-year-old man was referred to the Department of Surgical Oncology, Taizhou Hospital (Linhai, People’s Republic of China) in November 2012, with a giant sessile, moist, pinkish tumor located in the right lower abdomen. He reported having a small elevated nodular swelling in the right lower abdomen for the past three decades. The patient reported that during this time, the tumor had slowly, but consistently, increased in size and over the past 2 years had become more noticeable, combined with painful itching and bleeding on touching. In November 2012, the patient finally sought treatment because of local pain and bleeding from the tumor. Physical examination revealed a giant 4.0 × 2.0 cm brownish, verrucous tumor (). The tumor surface was a moist, pinkish mass with a few hemorrhagic areas. Though the clinical suspicion was either a squamous cell or a basal cell carcinoma, the initial pathologic diagnosis of a small wedge biopsy specimen was SCAP, with no evidence of malignancy. The mass was excised along with a 3 mm margin of healthy skin. The final pathologic diagnosis of the excised specimen confirmed the initial report.
Figure 1 Clinical appearance before surgery.

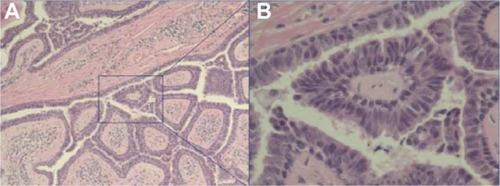
Histopathologically, the tumor was characterized by a number of cystic invaginations extending downwards from the epidermis ( and B). Numerous papillary projections extended into the lumen of these invaginations. The papillary projections were lined with a two-layer epithelium comprising an inner cylindrical and an outer cuboidal layer. A dense dermal cellular infiltrate, consisting primarily of plasma cells and lymphocytes, was prominent in the papillary projections. The histological findings were consistent with a verrucous form of SCAP ( and B).
Figure 2 (A) Low power view showing a double-layered epithelial lining comprised of tubular structures, with dense plasma cells and lymphocyte infiltrate in the stroma (original magnification ×100); (B) High power view showing a double layer of epithelium lining the papillary surfaces, with a columnar layer on the luminal side and a cuboidal layer on the other (original magnification ×400).
Discussion
SCAP is an uncommon skin adnexal tumor of sweat gland origin that usually occurs as a solitary lesion. Although most lesions are not clinically distinctive and require biopsy for diagnosis, the tumor is usually described as a skin-colored to pink, hairless, firm plaque of grouped nodules or as a solitary nodule, but verrucous, papillary, hyperkeratotic, moist, fleshy excrescences have also been described. Some tumors may show central umblication, through which small fistulae may discharge fluid.
The great majority of SCAP arise on the head and neck.Citation13 Other unusual reported locations of SCAP include the buttock,Citation16 vulva and scrotum,Citation17,Citation18 pinna,Citation19 eyelid,Citation20–Citation22 outer ear canal,Citation23 postoperative scar,Citation24 scalp,Citation25 nipple,Citation26 thigh,Citation27 axilla,Citation28 and back,Citation29 but only three cases in the right lower abdomen were previously reported.Citation30–Citation32 To our knowledge, this is the fourth case reported. Most of the lesions develop and enlarge gradually, although a few can attain considerable size within a few months. Clinically, SCAP presents with a range of nonspecific lesions. Diagnosis may be confirmed by histopathology. One study reported that ultrastructurally, although there were some variations in the electron density of the cells, the constituent epithelial cells were mainly divided into three types: luminal cells, basal cells, and clear cells.Citation33
The differential diagnosis of SCAP includes hidradenoma papilliferum, papillary eccrine adenomas, warty dyskeratoma, and inverted follicular keratosis. Clinically, SCAP presents as raised warty plaques on the head and neck, often in the setting of nevus sebaceus. Ducts invaginate from the surface into the dermis. Papillary fronds extend upward from the base, while plasma cells are common in the core of each frond.Citation9 Hidradenoma papilliferum similarly differentiates towards the secretory portion of the sweat gland but is more common on the vulva, breast, or eyelid, and unlike SCAP, there is no epidermal connection with hidradenoma papilliferum (it “hides” in the dermis). The dermal nodule of hidradenoma papilliferum consists of ducts that are arborized in a mazelike pattern, without plasma cell cores. Papillary eccrine adenomas are composed of multiple, dermal, dilated, duct-like spaces containing papillary projections. Similar to SCAP, warty dyskeratoma and inverted follicular keratosis show an endophytic pattern. However, warty dyskeratomas are lined by elongated dermal papillae with suprabasilar acantholysis of keratinocytes, some of which are dyskeratotic, and inverted follicular keratosis resembles an expanded hair follicle, with squamous eddies (whorls of mature squamous epithelium).
The histogenesis of SCAP is uncertain. Whether SCAP is derived from apocrine or eccrine glands is undetermined.Citation11,Citation34 Immunohistochemical studies conducted by Mazoujian and MargolisCitation35 support an apocrine origin, whereas ultrastructural analysis favors an eccrine derivation.Citation36 Alternatively, it has been speculated that SCAP might arise from pluripotent stem cells.Citation33 This would support a mix of apocrine and eccrine elements.
Cases of SCAP are limited. The only treatment for SCAP is excision biopsy, which also confirms the diagnosis. CO2 laser excision of SCAP of the head and neck is a clinical treatment option in anatomic areas that are unfavorable for excision and grafting.Citation37 SCAP has also been successfully treated with Mohs micrographic surgery.Citation38
In conclusion, SCAP is an uncommon sweat gland tumor with a widely variable clinical appearance. The peculiarity of our case lies in the rarity of SCAP and its location in the right lower abdomen. We believe that the present case is the fourth report of SCAP in the right lower abdomen. Our case represents an unusual presentation of an uncommon tumor at a rare location, with significant impairment in quality of life that improved after surgical excision.
Acknowledgments
This work was supported by Zhejiang Provincial Medical and Healthy Science and Technology Projects (Grants No 2011KYB137), the Science Research Fund of Taizhou (Grants No A102KY09 and A121KY08), and the Enze Medical Research Fund (Grants No 12EZA1).
Disclosure
The authors report no conflicts of interest in this work.
References
- BöniRXinHHohlDPanizzonRBurgGSyringocystadenoma papilliferum: a study of potential tumor suppressor genesAm J Dermatopathol2001232878911285401
- KargEKoromIVargaEBanGTuriSCongenital syringocystadenoma papilliferumPediatr Dermatol200825113213318304179
- AraiYKusakabeHKiyokaneKA case of syringocystadenocarcinoma papilliferum in situ occurring partially in syringocystadenoma papilliferumJ Dermatol200330214615012692383
- DiazRCBabuSCDuctal carcinoma arising from syringocystadenoma papilliferum in the external auditory canalOtol Neurotol200728687387417159662
- MamminoJJVidmarDASyringocystadenoma papilliferumInt J Dermatol199130117637661661711
- MisagoNNarisawaYSyringocystadenoma papilliferum with extensive apocrine nevusJ Dermatol200633430330516674800
- LeeCKJangKTChoYSTubular apocrine adenoma with syringocystadenoma papilliferum arising from the external auditory canalJ Laryngol Otol2005119121004100616354370
- YamaneNKatoNYanagiTOsawaRNaevus sebaceus on the female breast accompanied with a tubular apocrine adenoma and a syringocystadenoma papilliferumBr J Dermatol200715661397139917535243
- Rammeh-RommaniSFezaaBChelbiEKammounMRBen JilaniSBZermaniRSyringocystadenoma papilliferum: report of 8 casesPathologica200698317818017036946
- LinWLLinWCKuoTTChenCHHongHSAn unusual complex cutaneous adnexal tumor composed of syringocystadenoma papilliferum, apocrine hidrocystoma, and clear cell syringomaDermatol Surg200733787687917598859
- ShamsPNHardyTGEl-BahrawyMJoshiNSyringocystadenoma papilliferum of the eyelid in a young girlOphthal Plast Reconstr Surg20062216769
- KishimotoSWakabayashiSYamamotoMNodaYTakenakaHYasunoHApocrine acrosyringeal keratosis in association with syringocystoadenoma papilliferumBr J Dermatol2000142354354710735969
- YoshiiNKanekuraTSetoyamaMKanzakiTSyringocystadenoma papilliferum: report of the first case on the lower legJ Dermatol2004311193994215729871
- PhiliponeEChenSUnique case: syringocystadenoma papilliferum associated with an eccrine nevusAm J Dermatopathol200931880680719730225
- TownsendTCBowenARNobuharaKKSyringocystadenoma papilliferum: an unusual cutaneous lesion in a pediatric patientJ Pediatr2004145113113315238924
- SkeltonHG3rdSmithKJYoungDLuptonGPCondyloma acuminatum associated with syringocystadenoma papilliferumAm J Dermatopathol19941666286307864300
- StewartCJSyringocystadenoma papilliferum-like lesion of the vulvaPathology200840663863918752136
- GoshimaJHaraHOkadaTSuzukiHSyringocystadenoma papilliferum arising on the scrotumEur J Dermatol200313327112822557
- BakshiJParidaPKSyringocystadenoma papilliferum: report of first case on the pinnaJ Laryngol Otol200612012e4517105677
- AskarSKilincNAytekinSSyringocystadenoma papilliferum mimicking basal cell carcinoma on the lower eyelid: a case reportActa Chir Plast200244411711912661924
- BarbarinoSMcCormickSALauerSAMilmanTSyringocystadenoma papilliferum of the eyelidOphthal Plast Reconstr Surg2009253185188
- HelmiAAlarajAMAlkatanHReport of 3 histopathologically documented cases of syringocystadenoma papilliferum involving the eyelidCan J Ophthalmol201146328728921784220
- SuTCShenKHWangHKChuPYChenMLLipomatous apocrine adenoma with syringocystadenoma papilliferum arising from the external auditory canalHead Neck Oncol201133621854651
- SaricaogluHBaskanEBOzuysalSTunaliSA case of syringocystadenoma papilliferum: an unusual localization on postoperative scarJ Eur Acad Dermatol Venereol200216553453612428858
- LaxmishaCThappaDMMishraMMVermaSKLinear syringocystadenoma papilliferum of the scalpJ Eur Acad Dermatol Venereol200721227527617243981
- ShindoMYamadaNYoshidaYYamamotoOMorinoSSyringocystadenoma papilliferum on the male nippleJ Dermatol201138659359621914158
- MalhotraPSinghARameshVSyringocystadenoma papilliferum on the thigh: an unusual locationIndian J Dermatol Venereol Leprol200975217017219293506
- XuXLZhangGYZengXSWangQSunJFA case of zonal syringocystadenoma papilliferum of the axilla mimicking verruca vulgarisAm J Dermatopathol2010321495120098083
- GhoshSKBandyopadhyayDChatterjeeGBarCSyringocystadenoma papilliferum: an unusual presentationPediatr Dermatol200926675875920199464
- YapFBLeeBRBabaRSyringocystadenoma papilliferum in an unusual location beyond the head and neck region: a case report and review of literatureDermatol Online J20101610421062598
- SuzukiTIkedaHHamasakiYHatamochiAYamazakiSSyringocystadenoma papilliferum associated with apocrine poromaJ Dermatol200633424925116674787
- ShindoKHamadaTSyringocystadenoma papilliferum occurred on the lower abdomenSkin Research1991336660663 Japanese with abstract in English.
- YamamotoODoiYHamadaTHisaokaMSasaguriYAn immunohistochemical and ultrastructural study of syringocystadenoma papilliferumBr J Dermatol2002147593694512410704
- AktepeFDemirYDilekFHTubular apocrine adenoma in association with syringocystadenoma papilliferumDermatol Online J200391712639465
- MazoujianGMargolisRImmunohistochemistry of gross cystic disease fluid protein (GCDFP-15) in 65 benign sweat gland tumors of the skinAm J Dermatopathol198810128352459984
- NiizumaKSyringocystadenoma papilliferum: light and electron microscopic studiesActa Derm Venereol197656532733678616
- JordanJABrownOEBiavatiMJManningSCCongenital syringocystadenoma papilliferum of the ear and neck treated with the CO2 laserInt J Pediatr Otorhinolaryngol199638181879119597
- ChiCCTsaiRYWangSHSyringocystadenocarcinoma papilliferum: successfully treated with Mohs micrographic surgeryDermatol Surg200430346847115008887