Abstract
Adenocarcinoma is the most common type of malignant pulmonary tumor, but osseous metaplasia of this tumor is extremely rare. To date, only 21 cases have been reported in the literature worldwide. Here, we report a case of primary pulmonary adenocarcinoma with benign osseous stromal metaplasia in a 60-year-old woman and discuss the pathogenesis of intratumoral ossification and review the relevant literature. We found that pulmonary adenocarcinoma with osseous metaplasia may be more likely to occur in early tumor stages.
Introduction
Metaplasia is a process in which a differentiated cell type is replaced by another mature differentiated cell type. Although rare, osseous stromal metaplasia has been described in the literature for both benign and malignant neoplasms. Here, we report a unique case of primary pulmonary carcinoma with osseous metaplasia. We believe that this is a case of minimum bone formation (approximately 1.25 mm × 0.85 mm) in a primary pulmonary carcinoma.
Case report
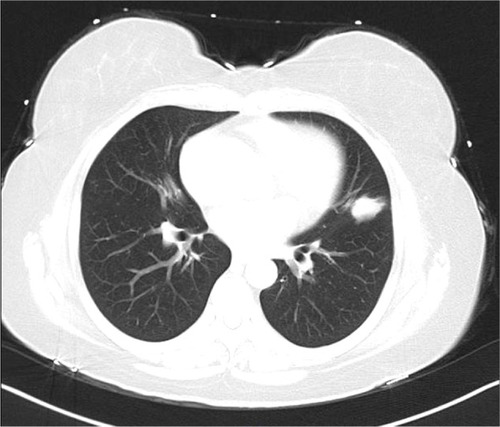
A 60-year-old Chinese woman presented with the symptom of bloody sputum, which she had noticed for 2 weeks. Enhanced computed tomography (CT) showed an irregular abnormal soft tissue mass located in the left upper lobe that was approximately 1.7 cm× 0.8 cm in size and obviously enhanced with contrast medium (). The CT value in the enhanced arterial phase was approximately 40–60 Hounsfield units, while the venous phase CT value was approximately 72 Hounsfield units. Minimal calcification was not apparent in the tumor. The patient denied any history of gastric carcinoma or digestive symptoms. On the basis of her history and imaging studies, the patient was diagnosed with a malignant pulmonary tumor and underwent lobectomy. The tumor had a heterogeneous off-white appearance and was solid with unclear boundaries. No depressions or varicose veins were found in the pleura.
Figure 1 Computed tomography scan showed an irregular abnormal soft tissue mass located in the left upper lobe.
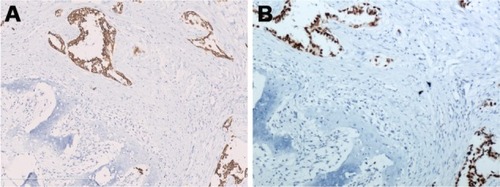
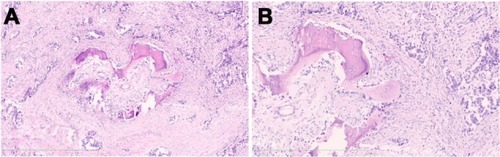
Hematoxylin and eosin-stained sections showed that the alveolar structure had disappeared within the tumor and that the tumor cells were distributed into round or oval glands with a central lumen. There was no mucin in the tumor cell cytoplasm or glandular cavity. The tumor cell nuclei were ovoid and dark-stained, with prominent nucleoli. The mitotic activity was approximately two mitoses per ten high-powered fields. New bone formation was observed at the center of the tumor (approximately 1.25 mm × 0.85 mm, ). The bone island consisted of mature bone tissue and was surrounded by osteoblast cells that were accompanied by proliferating fibroblasts (). No bone marrow cells were present in the bone tissue. Immunohistochemical staining showed that the tumor cells were positive for cytokeratin-7 () and thyroid transcription factor-1 (), but the metaplastic bone tissue was negative for these factors. However, the tumor cells were negative for caudal-related homeodomain protein 2, which ruled out the possibility of gastrointestinal adenocarcinoma metastasis to the lung, and the Ki-67 labeling index was approximately 35%. An epidermal growth factor receptor exon 19 deletion mutation was found in this patient, but the echinoderm microtubule-associated protein-like 4-anaplastic lymphoma kinase rearrangement was not found. On the basis of histologic and immunohistochemical findings, this tumor was diagnosed as an invasive pulmonary adenocarcinoma with a predominant acinar pattern, accompanied by osseous metaplasia in tiny lesions and without lymphatic metastasis. This diagnosis was based on the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system for standard lung adenocarcinoma.Citation1
Figure 2 (A) Tumor showing the moderately differentiated adenocarcinoma growing with a born formation. Hematoxylin and eosin staining, original magnification ×50. Scale bar 1 mm. (B) Mature bony trabeculae in the abundant fibroblastic stroma were surrounded by osteoblasts. Hematoxylin and eosin staining, original magnification ×100. Scale bar 600 μm.
Discussion
Malignant neoplasms accompanied by osseous metaplasia have been sporadically reported in the kidney,Citation2 gastrointestinal tract,Citation3,Citation4 thyroid,Citation5 soft tissue,Citation6 endometrium,Citation7 bladder,Citation8 brain,Citation9 and urachus;Citation10 however, heterotopic ossification within a primary pulmonary carcinoma is extremely rare. Only 21 cases of pulmonary adenocarcinoma with heterotopic ossification have been previously reportedCitation11–Citation22 in patients whose ages ranged from 46 to 76 (mean 62.4) years. The male to female ratio in these patients was 11:10, and the tumor sizes ranged from 1.5 cm to 7 cm (mean 3.59 cm). One patient received radiotherapy. Two patients also presented with osteoplastic metastasis. Follow-up information was available for 14 patients and indicated that one patient died after 33 months, while one patient developed a recurrence after 60 months of follow-up. In contrast with patients having conventional lung adenocarcinoma, which usually presents as an advanced cancer,Citation23 lung adenocarcinoma with osseous metaplasia seems to be more frequent in early-stage disease, given that patients with stage I, II, III, and IV disease accounted for 57.1% (n=12), 14.3% (n=3), 19.0% (n=4), and 4.8% (n=1) of the cases, respectively; staging information was not available for one patient. The stage of the patient presented in this paper was IA, which is consistent with this phenomenon ().
Table 1 Summary of previously reported cases of heterotopic mesenteric ossification
The mechanism responsible for osseous histogenesis in malignant neoplasms remains obscure. Several studies have documented that osseous metaplasia results from osteoblast metaplasia of pulmonary fibroblasts.Citation22 Other studies reported abnormally high serum calcium levels (hypercalcemia) in patients with malignant neoplasms; these levels were closely associated with bone formation. However, the serum calcium level was within normal limits in this patient. Most authors report that multipotent stromal stem cells are involved in the metaplastic process, resulting in bone formation.Citation24 Some cytokines such as bone morphogenetic protein 7 promote bone formation by inducing differentiation of pluripotent cells, mesenchymal cells, or fibroblasts into osteoprogenitor cells.Citation25 Further, some studies showed that bone formation might occur as a result of local or systemic inflammation. Inflammatory cells, including monocytes and macrophages, produce cytokines such as tumor necrosis factor-alpha and interleukin-1. Tumor necrosis factor-alpha and interleukin-1 are reported to stimulate activated cells to produce transforming growth factor beta and bone morphogenetic protein 7, which act as local cellular regulators of ectopic bone formation.Citation26,Citation27
Osseous histogenesis in malignant neoplasms is a rare and interesting phenomenon, but the prognostic implications of this occurrence are not very clearly described in the literature. Some studies suggest that cerebral ventricle ependymoma with ossification might exhibit more aggressive clinical behavior.Citation9 However, ossification has been suggested to be a marker of favorable prognosis in patients with renal cell carcinoma.Citation28 Therefore, investigations of the prognosis in patients with pulmonary adenocarcinoma and bone formation remain worthwhile. The lack of evidence of recurrence and metastasis in this patient at a 26-month follow-up indicated that ossification in pulmonary adenocarcinoma might not have adverse prognostic implications, but a longer follow-up period and more case studies are needed to illustrate this rare phenomenon.
Disclosure
The authors report no conflicts of interest in this work.
References
- WarthAMuleyTMeisterMThe novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system of lung adenocarcinoma is a stage-independent predictor of survivalJ Clin Oncol2012301438144622393100
- PuppaGGervasioAYorukogluKColombariRDe MarchiFCanzonieriVHuge renal cyst with parietal renal cell carcinoma, osseous metaplasia and a papillary adenoma: a case report with unique clinico-pathological features and literature reviewVirchows Arch200845232533018080136
- WilsherMJAdenocarcinoma arising in a traditional serrated adenoma of the rectosigmoid colon with osseous metaplasiaPathol Int20116123924221418396
- ZapataECastiellaAZubiaurreLAgirreARodriguezJOsseous metaplasia in a gastric adenomatous polypEndoscopy201244E8122396294
- PontikidesNBotsiosDKarikiEVassiliadisKKrassasGEExtramedullary hemopoiesis in a thyroid nodule with extensive bone metaplasia and mature bone formationThyroid20031387788014588103
- OruiHIshikawaATsuchiyaTTakaharaMItoMOginoTChondro-osseous differentiation in fat tissue tumors: magnetic resonance imaging with pathological correlationSkeletal Radiol20002945946511026714
- ParenteRCPatriarcaMTde Moura NetoRSGenetic analysis of the cause of endometrial osseous metaplasiaObstet Gynecol20091141103110820168113
- DudleyAGTomaszewskiJJHughesAHDaviesBJIncidentally discovered osseous metaplasia within high-grade urothelial carcinoma of the bladderUrology201279e59e6021862118
- WangXZhangSYeYChenYLiuXEpendymoma with cartilaginous metaplasia might have more aggressive behavior: a case report and literature reviewBrain Tumor Pathol20122917217622228122
- Lopez-BeltranANogalesFDonnéCHSayagJLAdenocarcinoma of the urachus showing extensive calcification and stromal osseous metaplasiaUrol Int1994531101137801415
- McLendonRERoggliVLFosterWLJrBecseyDCarcinoma of the lung with osseous stromal metaplasiaArch Pathol Lab Med1985109105111533931607
- MiyataSNakagawaTMaedaSMiwaAKitagawaMTakashimaTA case of adenocarcinoma of the lung with calcification on chest CTJpn J Lung Cancer198828107111
- YoshidaKMorinagaSGemmaAShimosatoYTsuchiyaREguchiKAdenocarcinoma with stromal bone metaplasia of the lungJpn J Lung Cancer1988288792
- FukuseTKohTOkumuraNKuwabaraMSuzukiYA case of primary lung cancer with stromal ossificationJpn J Lung Cancer199030267272
- HayakawaKMurataOIshizekiKA case of pulmonary ossified adenocarcinoma with marked osteoplastic bone metastasisLung Cancer1997182652689444652
- HaraHIwabuchiKShinadaJYoshimuraHKameyaTPulmonary adenocarcinoma with heterotopic bone formationPathol Int20005091091311107069
- HosodaHIzumiHAtarashiKShinoharaNSunamoriMLung adenocarcinoma with stromal ossificationJpn J Lung Cancer2002425154
- TsuchiyaTNishimuraYFunadaYPulmonary adenocarcinoma with central ossificationNihon Kokyuki Gakkai Zasshi200038283287 Japanese10879031
- UeshimaYKuriokaHYamadaRTakumiCHiraokaNOnoSStromal bone formation by lung adenocarcinomaNihon Kokyuki Gakkai Zasshi200543523526 Japanese16218421
- UsamiNYoshiokaHMoriSImaizumiMNagasakaTUedaYPrimary lung adenocarcinoma with heterotopic bone formationJpn J Thorac Cardiovasc Surg20055310210515782573
- KatoFIwasakiAMiyoshiTA case of primary adenocarcinoma of the right lung with ossificationJournal of the Japanese Association for Chest Surgery200620856859
- KimGYKimJKimTSHanJPulmonary adenocarcinoma with heterotopic ossificationJ Korean Med Sci20092450451019543517
- CrinòLWederWvan MeerbeeckJFelipEESMO Guidelines Working GroupEarly stage and locally advanced (non-metastatic) non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-upAnn Oncol201021103115
- XieLZhangNMarsanoAVunjak-NovakovicGZhangYLopezMJIn vitro mesenchymal trilineage differentiation and extracellular matrix production by adipose and bone marrow derived adult equine multipotent stromal cells on a collagen scaffoldStem Cell RevJuly282013 [Epub ahead of print]
- ToyranSLinAYEdwardDPExpression of growth differentiation factor-5 and bone morphogenic protein-7 in intraocular osseous metaplasiaBr J Ophthalmol20058988589015965172
- DayerJMEvidence for the biological modulation of IL-1 activity: the role of IL-1 RaClin Exp Rheumatol2002201420
- ChaoCCHuSShengWSTsangMPetersonPKTumor necrosis factor-alpha mediates the release of bioactive transforming growth factor-beta in murine microglial cell culturesClin Immunol Immunopathol1995773583657586747
- BielsaOLloretaJArangoOSerranoSGelabert-MasABone metaplasia in a case of bilateral renal cell carcinomaUrol Int200166555611150957