Abstract
Objectives
Adenocarcinoma (AC) of the uterine cervix has a poor prognosis and is usually fatal. The aim of this study was to evaluate the clinical outcome and toxicity of intraoperative electron beam radiation therapy (IOERT) in advanced AC.
Methods
Twenty-seven women were treated with IOERT. Surgery consisted of gross negative surgical margins in 19 patients, positive surgical margins in two patients, and close surgical margins in six patients. Twenty-three patients received chemotherapy.
Results
The 5-year overall survival and disease-free survival rates were 21/27 (77.8%) and 19/27 (70.4%), respectively. A significantly better survival rate was found in patients with AC compared to patients with adenosquamous carcinoma. Tumor recurrence and metastasis were observed in seven patients (25.9%). No central failure occurred whether or not the resection margins were positive. Two (7.4%) patients developed peripheral neurotoxicity.
Conclusion
IOERT plus surgery may be feasible and effective with a low risk of toxicity, even in patients with positive resection margins.
Background
Adenocarcinoma (AC) of the uterine cervix currently accounts for 5%–20% of all cervical malignancies, and appears to be increasing in prevalence,Citation1 presumably due to its rise in incidence in young women.Citation2 Moreover, it has been reported that these tumors tend to metastasize to the lymph nodes, and are less sensitive to radio- and chemotherapy than squamous cell carcinoma (SCC).Citation3 Most of our knowledge about the treatment of cervical cancer comes from studies where the majority of patients had SCC; however, few studies have reported on patients who have AC of the cervix.Citation4–Citation6 The little that is known about this disease points to the fact that it has a poor prognosis and is usually fatal. Thus, improvement in the therapy of AC of the uterine cervix is urgently needed.
Although the National Comprehensive Cancer Network guidelines include consideration of both intraoperative electron beam radiation therapy (IOERT) at the time of surgical exploration and resection as treatment options for patients with locoregional disease relapse, data to support this recommendation are scarce. IOERT is an innovative boosting technique which delivers a single high-dose fraction of radiotherapy directly to the resection bed during surgery to irradiate selective anatomical areas that have been identified during the surgical procedure as high risk and/or residual disease sites, while at the same time avoiding surrounding dose-limiting structures. This allows noncancerous intra-abdominal organs to be protected from receiving full doses of irradiation, which ultimately decreases the incidence of severe enteritis and increases the local control rates.Citation7 Studies of IOERT in multiple anatomical sites have produced valuable results in terms of locoregional control and toxicity.Citation8,Citation9 It has been applied with some success in gynecologic malignancies, including endometrioid, cervical, vaginal, and ovarian cancers.Citation10–Citation13 Since 1997, IOERT has been used in patients at our institution for the treatment of a variety of gynecologic malignancies, particularly when resection margins are in doubt. The current study evaluated survival and patterns of relapse and toxicity for patients undergoing IOERT for AC.
Methods
Patients
This study was a nonrandomized trial. Between January 1999 and January 2007, 202 women with cervical cancer were treated with IOERT at the First Affiliated Hospital of Medical College of Xi’an Jiaotong University. Among them, 27 women with AC were diagnosed with International Federation of Gynecology and Obstetrics (FIGO) stage IIB. Patients with prior postoperative adjuvant treatments, such as chemotherapy, were allowed to enter the study. The present study was approved by the ethics committee of the First Affiliated Hospital of Medical College of Xi’an Jiaotong University. All patients gave signed informed consent for IOERT. Inclusion criteria were: 1) histologically proven AC; 2) FIGO stage IIB; 3) age <75 years; 4) no evidence of pelvic or para-aortic lymph node metastasis on a computed tomography (CT) scan; 5) no evidence of metastasis on chest X-ray; 6) normal liver and kidney function; 7) normal blood count; and 8) hemoglobin >9 g/L. Patients with SCC or previous pelvic radiotherapy were excluded from this analysis. The following criteria were studied: initial FIGO stage, initial performance status, response to IOERT, time and sites of relapse, overall survival (OS), and disease-free survival (DFS). Disease progression was defined as: new lesions that were consistent with new sites of disease on imaging that included CT, magnetic resonance imaging, ultrasound, and/or plain X-ray; biopsy/histology of new lesions; and new signs on clinical exams or symptoms consistent with new sites of disease.
Preoperative therapy
Patients underwent weekly intracavitary brachytherapy (dose of 12–14 Gy to International Commission on Radiation Units and Measurements reference Point A in two insertions using 192Ir was delivered).
Intraoperative electron beam radiation therapy
After a break of 1 to 2 weeks, all 27 patients underwent a simple hysterectomy with dissection of a palpable pelvic lymph node or tumor resection. During the operation, whole pelvic radiotherapy of 18–20 Gy was delivered intraoperatively using 12 Mev electron beam (Varian 1800, Varian, Palo Alto, CA, USA). All treatments were accomplished using a single IOERT field. The superior border of the field was at the bifurcation of common iliac vessels, while the inferior border covered 2 cm inferior to the operated vaginal vault, and laterally covered 1 cm beyond the lateral margin of external and common iliac vessels. The electron intraoperative applicator was 10–12 cm in diameter. The bladder, intestines, and sigmoid colon were shifted out of the radiation field, and the rectum was shielded with a 6 mm thick lead sheet. The portion of the obturator nerve in the pelvic region was partially shifted out of the radiation field.Citation8
Postoperative therapy
After 2 weeks of IOERT, chemotherapy was implemented with cisplatin and 5-fluorouracil at our institution. Cisplatin was given at a dose of 40 mg/m2/day for 3 days, and 5-fluorouracil was given by continuous fusion at a dose of 500 mg/m2/day from the first to fifth day. The cycles were repeated every 3 weeks. Seventeen patients received four to six courses of chemotherapy, 2 to 3 weeks after IOERT. Six patients were treated with two courses of chemotherapy; four patients refused chemotherapy ().
Table 1 Patient characteristics
Evaluation of acute and late toxicities
Acute and late toxicities were graded by the Common Terminology Criteria for Adverse Events version 3.0.Citation14 Complications that occurred within 90 days from the start of primary treatment were considered acute complications, and those that occurred more than 90 days after the start of treatment were considered late complications.
Follow-up
After the completion of treatment, patients were followed-up at 3-month intervals for 1 year, 6-month intervals for 3 years, and annually thereafter.
Statistics
OS and DFS curves were calculated according to the Kaplan– Meier method. P-values less than 0.05 were considered statistically significant.
Results
Patient characteristics
The median age of the 27 patients with AC at the time of diagnosis was 46.2 years (range, 21–74 years). All patients with primary tumors were diagnosed with FIGO stage IIB. Sixteen patients had AC (59.3%), ten (37.0%) had adenosquamous carcinoma (ASC), and one (3.7%) had clear cell carcinoma. Dissection of a palpable pelvic lymph node was performed for eleven patients (57.8%), and two of these patients (18.2%) had lymph node metastasis. Patient characteristics are outlined in . The final pathology review following surgery revealed grossly negative surgical margins in 19 patients, positive surgical margins in two patients, and close surgical margins (in which the resected tumor had been adherent to unresectable vascular structures) in six patients.
During the follow-up interval, six (22.2%) patients died; five patients (18.5%) died of tumor-related disease, and one patient died of causes unrelated to cancer. No central failure occurred. Tumor recurrence and metastasis were observed in seven patients (25.9%). Of the entire group, only two patients (7.4%) relapsed due to locoregional failure (outside the IOERT boost), and five patients (18.5%) had distant metastasis alone (including two cases of relapse para-aortic nodal metastasis, one case of liver metastasis, one case of multiple metastasis, and one case of lung metastasis). Among them, isolated local recurrence was detected in one patient (3.7%), and combined local failure and distant metastasis were detected in one patient (3.7%). The mean time to recurrence was 12 months (range, 8–24 months).
OS and DFS
The mean follow-up time was 81 months (range, 11–121 months). The 5-year OS and DFS rates in all 27 patients were 77.8% (21/27) and 19/27 (70.4%), respectively. In total, six patients died. Among the five patients who died of tumor-related disease, 17.6% (3/17) were patients who were treated with chemotherapy for four to six courses compared to 20% (2/10) of patients who had less than four courses of chemotherapy or patients without chemotherapy. The 5-year OS and DFS in patients who had four to six courses of chemotherapy were 76.4% (13/17) and 70.6% (12/17), respectively. A P>0.05 was found for patients with less than four courses of chemotherapy (8/10), or patients without chemotherapy (7/10), as shown in and . However, a significantly better survival rate was found in patients with AC (OS, 15/16; DFS, 14/16) compared to patients with adenosquamous carcinoma (OS, 6/10; DFS, 5/10) (P=0.034, P=0.031) ( and and ). The rates of distant metastasis were similar between patients (4/16 and 2/10, respectively; P=0.768). Local relapse was detected in 7.4% (2/27) of patients and central control (within the IOERT field) was 100% whether or not the resection margins were positive. No local failures occurred in any of the eight patients who underwent subtotal resection.
Figure 1 Survival analysis in advanced adenocarcinoma of the uterine cervix after IOERT.
Abbreviations: CT, computed tomography; Cum, cumulative; EBRT, external beam radiation therapy; IOERT, intraoperative electron beam radiation therapy.
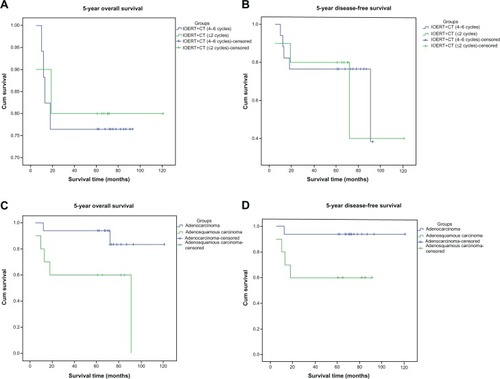
Table 2 Five-year disease-free and overall survival rates stratified by patient group
Toxicities
Generally, IOERT was well tolerated. The only noted toxicities were those potentially related to the local effects from local treatments. Toxicity related to chemotherapy was not included. In addition, no radiation-induced nausea or vomiting was observed, and no delayed wound healing occurred. None of the patients suffered from enteritis during the entire follow-up period. The major complication observed was peripheral neuropathy, which two (7.4%) patients developed after 8 months and 17 months. The incidence of developing neuropathy was present while the peripheral nerve was included in the IOERT field. In addition, one patient suffered from abdominal pain (3.7%). Other toxicities related to surgery, such as urinary tract infection, developed in 3.7% of the patients. All cases were manageable by conservative treatment.
Discussion
AC has been always managed in the same manner as SCC. However, the majority of studies showed that AC carries a worse prognosis than SCC, with 10%–20% differences in 5-year OS rates.Citation15 Baalbergen et alCitation16 demonstrated in a study of 305 patients that 5-year OS rates of stage I AC were 80%, of stage II were 37%, and of stage IIIb were 11%. Therefore, innovative treatments to improve the survival and local control of AC are urgently needed.
In this study, we found IOERT to be both well tolerated and effective in patients with stage II AC in regard to survival benefit (the 5-year OS rate was 77.8%) and lower number of toxicities. In addition, the findings from this study suggest that the OS in AC is higher than that in ASC. This is consistent with reports that ASC of the cervix has a poorer prognosis than AC.Citation17,Citation18 Although the patients with AC got survival benefit from IOERT, the 5-year OS rate and DFS rate seems still lower than that of the patients with SCC who were treated with IOERT.Citation19 It seems to be in accord with the studies showed that AC carries a worse prognosis than SCC.Citation15,Citation16
IOERT also appeared to confer a disease control benefit to surgical resection, as no patient experienced disease relapse within the IOERT field, despite positive resection margins in two patients, and close margins in another six patients. Disease control was also satisfactory, with only two local failures. Thus, IOERT could potentially sterilize any microscopic residual disease in the operative bed. The aggressive surgical resection of recurrent disease can result in long-term freedom from disease. However, in some cases, extensive surgery is not technically feasible, as the risk of morbidity from a resection, such as pelvic exenteration, would be too great. However, by combining surgery with IOERT, an appropriate balance of surgical aggressiveness and patient treatment-induced morbidity was achieved.
In addition, our study showed that five patients (18.5%) had distant metastasis (including two cases of relapse para-aortic nodal metastasis, one case of liver metastasis, one case of multiple metastasis, and one case of lung metastasis), which was consistent with some studies that reported differences in patterns of disease dissemination for patients with AC histology compared to SCC of the cervix. Patients with AC had a significantly higher rate of ovarian metastasis, consistent with a number of studies that have demonstrated higher rates of distant metastasis with AC histology, such as ascites, abdominal carcinomatosis, and para-aortic spread.Citation20
Some studies have reported that systemic chemotherapy and the addition of adjuvant radiotherapy plays a greater importance in the treatment of AC compared to SCC in improving survival and reducing the risk of recurrence. This may be because they harbor more micro-metastasis than SCC, and can therefore be potentially eradicated by RT and have more to gain from the added systemic effect of extra chemotherapy courses. Additionally, further analyses of all patients receiving chemotherapy found that higher numbers of chemotherapy courses were associated with improved progression-free and overall survival.Citation20 However, in this study, the difference in OS and DFS did not reach statistical significance between patients who had four to six courses of chemotherapy, less than four courses of chemotherapy, or no chemotherapy. Further studies about this should be anticipated.
In conclusion, IOERT may be feasible and effective as a boosting technique for advanced or recurrent AC. IOERT plus surgery may achieve high locoregional disease control and survival benefit with a low risk of toxicity, even in patients with positive resection margins. With this combined modality approach, we expect some patients with AC to experience long-term freedom from recurrence. The findings of this study confirm our clinical impressions and provide important information with which to move forward in developing better therapies for advanced AC of the uterine cervix.
However, the study has its own limitation. The study’s results are limited by its retrospective design and the data is from a single institution. Thus, the plans for a randomized trial would be anticipated in the future.
Conclusion
IOERT may be feasible and effective as a boosting technique for advanced AC. IOERT plus surgery may achieve high locoregional disease control and survival benefit with a low risk of toxicity, even in patients with positive resection margins. With this combined modality approach, some patients with AC will be able to experience long-term freedom from recurrence.
Acknowledgments
This work is supported by the National Natural Science Foundation of China (No 81071838 and No 81301937), the Shaanxi Province Department of Health Key Program (No 2010A02), the International Cooperation Foundation of Shaanxi Province of China (No 2013KW-27-03), and the Foundation of the First Affiliated Hospital of Medical College of Xi’an Jiaotong University (No 2010YK3).
Disclosure
The authors declare no conflicts of interest in this work.
References
- WangSSShermanMEHildesheimALaceyJVDevesaSCervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and black women in the United States for 1976–2000Cancer200410051035104414983500
- QuinnMAAdenocarcinoma of the cervix – are there arguments for a different treatment policy?Curr Opin Obstet Gynecol19979121249090477
- GrisaruDCovensAChapmanBDoes histology influence prognosis in patients with early-stage cervical carcinoma?Cancer200192122999300411753977
- LancianoRCalkinsABundyBNRandomized comparison of weekly cisplatin or protracted venous infusion of fluorouracil in combination with pelvic radiation in advanced cervix cancer: a gynecologic oncology group studyJ Clin Oncol200523338289829516230678
- MonkBJWangJImSGynecologic Oncology GroupSouthwest Oncology GroupRadiation Therapy Oncology GroupRethinking the use of radiation and chemotherapy after radical hysterectomy: a clinical-pathologic analysis of a Gynecologic Oncology Group/Southwest Oncology Group/Radiation Therapy Oncology Group trialGynecol Oncol200596372172815721417
- RotmanMSedlisAPiedmonteMRA phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group studyInt J Radiat Oncol Biol Phys200665116917616427212
- WillettCGSuitHDTepperJEIntraoperative electron beam radiation therapy for retroperitoneal soft tissue sarcomaCancer19916822782831906369
- GundersonLLRationale and results of intraoperative radiation therapyCancer19947425375418033030
- AzinovicIMartinez MongeRJavier AristuJIntraoperative radiotherapy electron boost followed by moderate doses of external beam radiotherapy in resected soft-tissue sarcoma of the extremitiesRadiother Oncol200367333133712865183
- GaoYLiuZChenXLuoWZhangLWangJIntraoperative radiotherapy electron boost in advanced and recurrent epithelial ovarian carcinoma: a retrospective studyBMC Cancer20111143921989202
- DowdySCMarianiAClibyWARadical pelvic resection and intra-operative radiation therapy for recurrent endometrial cancer: technique and analysis of outcomesGynecol Oncol2006101228028616321431
- BarneyBMPetersenIADowdySCBakkum-GamezJNHaddockMGLong-term outcomes with intraoperative radiotherapy as a component of treatment for locally advanced or recurrent uterine sarcomaInt J Radiat Oncol Biol Phys201283119119721985942
- TranPTSuZHaraWHusainATengNKappDSLong-term survivors using intraoperative radiotherapy for recurrent gynecologic malignanciesInt J Radiat Oncol Biol Phys200769250451117560736
- National Cancer Institute3312003Cancer Therapy Evluation Program. Common Terminology Criteria for Adverse Events. Version3.0 Available from http://cteo.cancer.govAccessed July 20, 2013
- DavyMLDoddTJLukeCGRoderDMCervical cancer: effect of glandular cell type on prognosis, treatment, and survivalObstet Gynecol20031011384512517643
- BaalbergenAEwing-GrahamPCHopWCStruijkPHelmerhorstTJPrognostic factors in adenocarcinoma of the uterine cervixGynecol Oncol200492126226714751169
- FarleyJHHickeyKWCarlsonJWRoseGSKostERHarrisonTAAdenosquamous histology predicts a poor outcome for patients with advanced-stage, but not early-stage, cervical carcinomaCancer20039792196220212712471
- WangSSShermanMESilverbergSGPathological characteristics of cervical adenocarcinoma in a multi-center US-based studyGynecol Oncol2006103254154616697450
- LiuZGaoYSoongYLIntraoperative electron beam radiotherapy for primary treatment of stage IIB cervical cancer: a retrospective studyJ Int Med Res20124062346235423321192
- GienLTBeaucheminMCThomasGAdenocarcinoma: a unique cervical cancerGynecol Oncol2010116114014619880165
- PetersWALiuPYBarrettRJConcurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervixJ Clin Oncol20001881606161310764420