Abstract
Osteoporosis is a bone disorder with remarkable changes in bone biologic material and consequent bone structural distraction, affecting millions of people around the world from different ethnic groups. Bone fragility is the worse outcome of the disease, which needs long term therapy and medical management, especially in the elderly. Many involved genes including environmental factors have been introduced as the disease risk factors so far, of which genes should be considered as effective early diagnosis biomarkers, especially for the individuals from high-risk families. In this review, a number of important criteria involved in osteoporosis are addressed and discussed.
Introduction
Osteoporosis is a skeletal characterized by decreased bone mass and microarchi-tectural deterioration of bone tissue resulting in less bone tension and strength and increased risk of fragility fracture.Citation1,Citation2 Osteoporosis is a major threat to elderly people, a fast-growing population of the world, in whom the risk of fracture increases with continued aging of the population.Citation3
Impact of bone density and bone quality on the fracture risk
Bone geometry, microarchitecture and size are the factors influencing the ability of bone to withstand trauma. However, 75%–90% of variance in bone strength is related to bone mineral density (BMD).Citation4 Indeed, bone strength arises from the integration of bone density and bone quality. The World Health Organization has defined the criteria including T-score and z score for evaluating bone status. T-score is explained as the number of SDs which fall below the young adult mean value in osteoporosis (the World Health Organization defines osteoporosis as a T-score of <−2.5), and z score is the expected BMD for the individual’s age and sex. BMD is expressed as a correlation of the T-score and the z score.Citation5 Dual-energy X-ray absorptiometry is the most widely utilized quantitative method for measuring BMD and appraisement of fracture risk.Citation6
Prevalence of fractures
Worldwide, osteoporosis causes >8.9 million fractures annually, with the greatest number of osteoporotic fractures occurring in Europe (34.8%).Citation7 The most serious clinical consequence of osteoporosis is osteoporotic fracture. Fractures of the hip, vertebrae and distal forearm are considered as osteoporotic fractures with common epidemiologic characteristics: the fracture incidences are higher in women compared to men, and they increase steeply with advancing age and occur at body positions with a large proportion of trabecular bone. Besides, osteoporosis can lead to fractures at other sites. These include fractures of the humerus, ribs, tibia (in women), pelvis femoral fractures.Citation4
Ethnicity and race are important factors influencing the prevalence of osteoporosis. Older Asian men are reported to have 50% lesser risk of sustaining a hip fracture over their lifetime than Caucasian men. Similar to men, Asian women also have lower fracture risk than Caucasian women. Moreover, there are differences in drug treatment response for osteoporosis based on ethnicity and race.Citation9 A study conducted on different populations support the fact that BMD is higher in African American women than in white women at every level of body weight and is consistent with their lower fracture rates.Citation10 The prevalence of both lifestyle-related metabolic disorders and osteoporosis is increasing in Asia. Metabolic syndrome may be associated with bone loss in Asian men, and atherosclerosis is associated with increased fractures.Citation11
Bone fractures of hip
Hip fracture is one of the seriously occurring osteoporotic fractures resulting in drastic morbidity, disability, diminished quality of life and mortality events.Citation12 Proximal femur (hip) fractures which demonstrate about 20% of all osteoporotic fractures are the most destructive ones and responsible for the most payments related to health care resources.Citation13 Hip fractures are associated with an 8%–36% excess mortality within 1 year, with a higher mortality in men than in women.Citation14 Since 1990, the number of fractures has continued to increase as the population ages. It is estimated that the annual worldwide hip fracture occurrence will increase up to >6 times by 2050, compared to the 1990 hip fracture rate in Europe and North America.Citation14 As the number of elderly people is increasing most rapidly in Asia, Latin America, the Middle East and Africa, it is expected that over 70% of the 6.26 million hip fractures will occur in these regions by year 2050 and Asian countries will contribute more to the pool of hip fractures in coming years.Citation15 A total of 72 studies from 63 countries by Kanis et alCitation250 showed a remarkable heterogeneity in hip fracture risk between the populations. The highest annual incidences were observed in countries from North Western Europe (Denmark [574/100,000 individuals], Norway [563/100,000 individuals] and Sweden [539/100,000 individuals]). But the hip fracture rate in men was approximately half of that was reported in women.Citation16 This low prevalence in men has been attributed to 12%–13% greater bone mass in men.Citation12 However, mortality rate following hip fracture is substantially higher in men than in women.Citation17,Citation18 These findings showed that the variation in hip fracture incidence between countries was much greater than the differences between genders within a country.Citation16
Bone fractures of vertebral bodies
Osteoporosis-related vertebral fractures as a hallmark of osteoporosis are common problems for the aged people.Citation19,Citation20 However, it has been estimated that only about one-third of them seek clinical attention due to the absence of recognizable symptoms.Citation20 Older white women with clinically recognized incident vertebral fracture experience substantial increases in back pain associated with decreased quality of life and functional limitation due to back pain.Citation21,Citation22 In Europe, the incidence of new vertebral fracture was 10.7/1,000 per year in women and 5.7/1,000 per year in men aged 50–79 years. The prevalence of vertebral fracture was greater in Scandinavia compared with other European regions, while the geographic heterogeneity of vertebral fracture rate was less than that observed for hip fracture.Citation23 Vertebral fracture rate increases exponentially with age in the same way as for hip fracture, and the risk of death is associated with the number of vertebral fractures. This raises the possibility that prevention of further vertebral fractures might decrease the mortality rate.Citation24 Vertebral fracture cascade is a term referring to the occurrence of subsequent vertebral fracture after sustaining an initial vertebral fracture, and the risk of second vertebral fracture within a year following the first incident vertebral fracture in women is reported to be ~20%.Citation25 Women with vertebral osteoporotic fractures have reduced vertebral BMD and vertebral dimensions compared with controls with no history of fracture.Citation26 Similar findings exist for men.Citation27 Intravertebral distribution of bone mass, bone quality parameters, vertebral macroarchitecture, amount of intervertebral disc degeneration and balance control are factors varying significantly between individuals with and without vertebral fractures.Citation28
Bone fractures of the distal forearm
Fracture of the distal forearm is a common osteoporotic fracture accounting for up to 18% of all fractures in the above 65 years age groupCitation29 and 75% of fractures of the forearm.Citation30 Recent data show an increase in incidence of distal radius (wrist) fractures for the pediatric, adult and elderly populations in recent years.Citation29 Brogren et al documented comparable differences between men and women in the age group of 49–65, wherein they found that women had almost double the rate of fracture compared with men, likely due to the early onset of osteoporosis in women.Citation31 A research by O’Neill et al identified that the incidence of forearm fractures in 3,161 adult British men and women aged 35 years and over was 36.8/10,000 person-years in women and 9.0/10,000 person-years in men.Citation32 The age distribution of the wrist fractures is typically bimodal, with peaks found in the age groups 5–14 years and above 60 years.Citation30 The prevalence of distal radius fractures in the adult population is significantly lower than in elderly groups.Citation31 However, it has been suggested that this fracture is the most common injury in adult population and is more predominant than hip fractures. The rate of forearm fractures in Denmark was somewhat higher in both genders than that recently imputed from hip fracture rates and was close to the rates previously reported in studies from Norway and Sweden.Citation33 Urban/rural differences in BMD are a risk factor contributing to the fracture rate difference. A study showed that women residing in urban areas have a higher BMD than those in rural areas, which is entirely consistent with a 30% increased risk of sustaining a forearm fracture.Citation34 The occurrence of a distal forearm fracture convincingly predicts future fracture risk.Citation35 Overall, a 1.5-fold increase in the risk of a subsequent hip fracture among 2,252 Swedish women ≥40 years of age with a forearm fracture in 1968–1972Citation36 and also a 1.8-fold increase among 1,162 Danish women ≥20 years of age with a forearm fracture in 1976–1984 support the present hypothesis.Citation37 Fractures are also common among children, which result from mild or moderate trauma, endocrine dysfunction, chronic illnesses, genetic disorders, lack of weight-bearing physical activity and obesity.Citation38
Risk factors for osteoporosis and osteoporotic fractures
Osteoporosis is initiated by an imbalance between bone resorption and formation.Citation39,Citation40 Research studies point to a number of risk factors for osteoporosis that are modifiable, including diet and lifestyle factors, while some factors are non-modifiable (Box 1).
Nutritional deficiency (especially consumption of junk food) and sedentary lifestyle
Health-promoting behaviors, such as consuming a healthy diet, could lessen the impact of chronic diseases such as osteoporosis and cardiovascular diseases.Citation41 It was previously recognized that maternal diet can influence bone mass in the offspring and a good general nutritional status with adequate dietary protein, calcium, vitamin D, fruits and vegetables has a positive influence on bone health, while a high-caloric diet and heavy alcohol consumption have been associated with lower bone mass and higher rates of fracture.Citation42 It is now proven that a dietary pattern with high intake of dairy products, fruits and whole grains may contribute positively to bone health and dietary pattern-based strategies could have potential in promoting bone health.Citation43 Confirming this evidence and similar investigations, a study on Chinese older women in Hong Kong showed that higher “vegetables–fruits” and “snacks–drinks–milk products” pattern scores were associated with reduced risk of cognitive impairment.Citation44
Moreover, absence of vitamin K, particularly as vitamin K2, in junk food results in impairment of the calcium removal process and increases the risk of calcification of the blood vessels. An increased intake of vitamin K2 could be a means of lowering calcium-associated health risks.Citation45 In addition, the recent trends in avoiding sunbathing and eating fewer fish products have resulted in a high prevalence of vitamin D deficiency in the general Japanese population.Citation46
Use of alcohol and its relation to BMD
In 2013, Sommer et al demonstrated the results from Osteoporosis Risk Factor and Prevention-Fracture Prevention Study (OSTPRE-FPS) which suggested that low-to-moderate alcohol intake may exert protective effects on bone health in elderly women.Citation47 Nevertheless, osteoporotic patients should be counseled regularly about cigarette cessation, alcohol intake, and estrogen status.Citation48 Recently, a meta-analysis identified a nonlinear association between alcohol consumption and the risk of hip fracture. Light alcohol consumption was inversely significantly associated with hip fracture risk, whereas heavy alcohol consumption was associated with an elevated hip fracture risk.Citation49 Alcohol consumption (low and moderate/high) may have a detrimental impact on bone health in both the cortical and trabecular compartments at the distal radius in men, and similar results were found in the trabecular and distal tibia compartments of women with minimal alcohol and low alcohol consumptions, respectively, suggesting that avoidance of alcohol may be beneficial for bone health.Citation50
Smoking
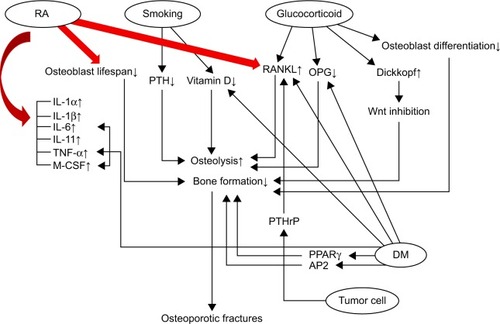
Cigarette smoking is considered as a risk factor for osteoporosis and is related to a loss of bone mass and increased risk of osteoporotic fractures.Citation51,Citation52 Krall and Dawson-HughesCitation53,Citation54 reported decreased BMD at the radius, femoral neck and whole in smokers than in nonsmokers. However, other investigators found no link between smoking and fracture risk in women.Citation55,Citation56 Parathyroid hormone (PTH) and vitamin D metabolites play a vital role in the regulation of calcium homeostasis and bone metabolism.Citation57,Citation58 Notably, serum PTH showed an increasing level in heavy smokers, which is consistent with the result of a similar study by Ortego-Centeno et al in young male smokers.Citation51 Smokers had about 10% decrease of circulating levels of 1,25-dihydroxyvitamin D (1,25(OH)2D).Citation59 Smoking is associated with increased follicle stimulating hormone and luteinizing hormone, which directs the estrogen levels to decrease and results in rapid bone loss.Citation52 The influence of some of the osteoporosis risk factors and their role in the bone formation pathway regulation and bone diseases is illustrated in .
Figure 1 Common osteoporosis risk factors involved in pathways associated with bone formation and osteoporotic fractures.
Abbreviations: IL, interleukin; M-CSF, macrophage colony stimulating factor; OPG, osteoprotegerin; PPARγ, peroxisome proliferator-activated receptor-γ; PTH, parathyroid hormone; RA, rheumatoid arthritis; RANKL, RANK with its ligand; TNF, tumor necrosis factor; DM, diabetes mellitus; AP2, adipocyte fatty acid binding protein 2; RANK, receptor activator of nuclear factor κ.
There is no clear evidence to show the direct causal relationship between passive cigarette smoking and osteoporosis. Furthermore, the underlying mechanism is unknown. The bone turnover biochemical markers in urine and serum and also the bone microarchitecture by micro-computed tomography were compared with the control group exposed to normal ambient air. In the cell culture experiments, MC3T3-E1 and RAW264.7 mouse cell lines used as osteoblast and osteoclast, respectively, were treated with the sera obtained from BALB/c mice exposed to 4% cigarette smoke during 14 weeks. Their actions on cell viability, differentiation and function on these bone cells were assessed. The urinary mineral and deoxypyridinoline levels and also serum alkaline phosphatase (ALP) activity were significantly higher in the 4% smoking group when compared with the control group, indicating an elevated bone metabolism after cigarette smoking. In addition, femoral osteopenia was observed in the 4% smoking group, as shown by a decrease in relative bone volume and trabecular thickness. In isolated cell studies, osteo-blast differentiation and bone formation were inhibited, while osteoclast differentiation was increased. The current mouse smoking model and the isolated cell studies demonstrate that passive cigarette smoke could induce osteopenia by exerting a direct detrimental effect on bone cells differentiation and further on bone remodeling process.Citation60
Genetic factors
The genetics of osteoporosis represents one of the greatest challenges and the most active area of research in bone biology. It is well established that the variation in BMD is determined by our genes. Several candidate gene polymorphisms in relation to osteoporosis have been implicated as determinants of BMD. The vitamin D receptor (VDR) gene, the collagen type I α1 (COLIA1) gene and the estrogen receptor-α (ERα) gene are among those most intensively studied. VDR modulates the transcription of target genes involved in calcium uptake or bone formation, including calcium-binding proteinsCitation61–Citation63 and osteocalcin (OC).Citation64 The VDR gene maps to chromosome 12q13-14 and possesses at least 11 exons.Citation65 Allelic variants of the gene encoding VDR are recognized by ApaI (allele A/a), BsmI (allele B/b), FokI (allele F/f) and TaqI (allele T/t) restriction endonucleases.Citation66–Citation69 All these polymorphisms are restriction fragment length polymorphisms.Citation70 VDR BsmI polymorphism, genotype bb showed the maximum influence on BMD in combination with other alleles and has been associated with higher rate of calcium absorption compared to that in women with the BB genotype.Citation71 Furthermore, BMD levels were consistently higher in women with the VDR bb genotype.Citation72 The BB genotype had a greater set point for the feedback inhibition of PTH initiated by an increase in 1,25-(OH)2D, more active bone resorption and breakdown of type I collagen, and greater concentrations of 1,25(OH)2D, compared with the bb genotype.Citation71 The assessment of BsmI polymorphism in a group of normal and osteoporotic Iranian women confirmed that BsmI polymorphism of VDR gene is significantly associated with BMD in the lumbar spine and may have a minor effect on the proximal femur BMD.Citation73 BsmI polymorphism could influence expression of the VDR gene and alter BMD through different mechanisms, including disruption of a splice site for VDR mRNA transcription and changes in mRNA stability or in the intronic regulation element.Citation74,Citation75 BMD was also associated with polymorphisms at other marker loci of the VDR gene, including the TaqICitation76 and FokI.Citation77 Genotype TT for the TaqI polymorphism had lower rate of bone loss than those with other genotypes. Given the tight linkage disequilibrium of the b allele with the T allele, the bb individuals had lesser bone loss.Citation78 FokI is an independent polymorphism, and FF genotype is associated with higher BMD at the femoral neck,Citation79 spine and hip.Citation80 The FF individuals had greater calcium absorption and BMD values than Ff and ff genotypes. This leads to the conclusion that the VDR alleles act differentially on intestinal calcium absorption.Citation71 Another polymorphism, the start codon polymorphism (SCP), is identified by the FokI polymorphism and is located at the translation initiation site in exon II of VDR. Unlike the above polymorphisms, which do not result in amino acid changes, the SCP changes the VDR structure. SCP makes the F allele VDR three amino acids shorter than the f allele, leading to altered receptor function.Citation78 Recently, a novel polymorphism in the Cdx-2–binding site of the VDR gene promoter region was identified. Polymorphic region function, which is also called the human VDR-sucrose-isomaltase footprint 1 sequence, was analyzed using an intestinal cell line as a model system.Citation81,Citation82 Cdx-2 was able to activate VDR gene transcription by binding to the human VDR-sucrase-isomaltase footprint 1 sequence. Mutations of the sequence suppressed transacti-vation activity.Citation81 VDR also regulates OC which plays a role in bone mineralization and calcium ion homeostasis. Higher OC levels have been reported in premenopausal Japanese women with the BB genotype.Citation83,Citation84 However, Willing et al found no such association between the BB genotype and either OC levels or their change over a 3-year period.Citation72
In addition to VDR, estrogen receptors (ERs) also play an important role in controlling skeletal growth and maintenance of bone mass. Two functional ERs, ERα and ERβ, are encoded by different genes and have similar structure and considerable homology in the DNA-binding and ligand-binding domain. The human ERα gene (ESR1) is located on chromosome 6q25, and consists of eight exons and spans >140 kb. The ERβ gene (ESR2) is located on chromosome 14q23-24.1.Citation85 Decreased BMD in mice lacking functional ERα supports the hypothesis that ERα is probably a candidate gene for osteoporosis.Citation86–Citation89 Several polymorphisms of this gene have been studied, including the T→C and the A→G in intron 1 and the TA repeat in the promoter region, codon 325 (CCC→CCG),Citation90 T262C of exon 1,Citation91 G2014A of exon 8Citation92 and G261C of exon 1.Citation93 Furthermore, the TA repeat polymorphism is located within the promoter region 1,174 bp upstream from exon 1, which affects BMD by changing the production or stability of mRNA leading to changes in ER number. Linkage of two intronic PvuII and XbaI polymorphisms with BMD has been extensively studied. In general, the XX and pp genotypes (or the X and p alleles) were associated with greater BMD, as compared with the xx and PP genotypes (or the x and P alleles).Citation72,Citation94–Citation97 Pouresmaeili et alCitation98 observed a majority of PX haplotypes among 200 pre- and/or postmenopausal Iranian women, which is in contrast with the frequencies for Caucasians with a reduced PX haplotype.Citation99
Potentially, there is a physiologic functional relationship between the ER and VDR.Citation100 We observed that BMD levels were consistently higher in women with the VDR bb genotype and the (−/−) PvuII and Xba I ER genotypes.Citation17 However, a significant gene-by-gene interaction effect indicated that women who were homozygous (−/−) at the PvuII or Xba I loci had significantly different BMD levels according to their VDR status.Citation72
Osteoporosis may also be caused by mutations in the Collagen I alpha 1 (COL1A1) gene that has been consistently associated with fracture risk.Citation101 The Sp1 polymorphism stems from a G→T substitution at the first base of a consensus site in the first intron in the COLIA1 gene for the transcriptional factor, Sp1.Citation102,Citation103 BMD was greater for the G/G (SS) genotype than for the G/T (Ss) and T/T (ss) genotypes. The s allele had greater affinity than the S allele for Sp1 protein. Brown et alCitation104 found that lumbar spine bone loss was greater in the ss and Ss genotypes than in the SS genotype.
Most genetic polymorphisms are associated with the genes encoding the important pathways of bone metabolism, including transforming growth factor-β1 (TGF-β1), interleukin-6 (IL-6), insulin-like growth factor (IGF)-I, calcitonin (CT), calcitonin receptor (CTR) and interleukin-1 receptor antagonist (IL-1ra). The TGF-β1 gene has seven exons, of which exons 5–7 encode the active TGF-β1. Keen et alCitation105 reported that the T→C polymorphism of intron 5 was associated with femoral neck BMD. Yamada et alCitation106 studied the 509 C→T polymorphism in postmenopausal Japanese women and found a link with lumbar spine and total body BMD. Activation of cytokine expression in bone is a feature of postmenopausal women, leading to bone loss. IL-6, a pleiotropic cytokine, mediates estrogen deficiency-related bone loss in patients.Citation107 Several studies have demonstrated the relationship of polymorphisms of the IL-6 gene with BMD, including the variable number tandem repeat (VNTR) polymorphism in the 3′ flank region of the gene,Citation108 the CA repeat polymorphismCitation109 and the −174 G→C polymorphism.Citation110 IGF-I is produced by osteoblasts and is involved in bone metabolism.Citation111 Serum IGF-I concentrations were correlated with BMD in humans.Citation112,Citation113
CT is a polypeptide hormone secreted by the thyroid gland and inhibits osteoclastic bone resorption. The human CTR belongs to a family of G-protein-coupled receptors. In a study in 663 postmenopausal and 52 premenopausal Italian women, the Alul restriction enzyme polymorphism of the CTR gene was associated with spine BMD.Citation114 The TaqI polymorphism and the T→C polymorphism are two polymorphisms of the CTR gene which are related to lumbar and femoral neck BMD.Citation115,Citation116
IL-1 acts as a powerful stimulant of bone resorption by inhibiting osteoclast apoptosis. IL-1ra competes with both IL-1α and IL-1β, the two isoforms of IL-1, for binding with IL-1 receptors. Postmenopausal increase in IL-1 and IL-1ra production results in bone loss.Citation117
The human IL-1ra gene consists of four exons.Citation118 The VNTR is due to an 86 bp repeat within intron 2 of the gene. VNTR polymorphism is associated with spinal bone loss.Citation117
Wong et al’s Citation119 study assessed the correlation between BMD and allele E4 of apolipoprotein E (ApoE4) in the Chinese population. One hundred and ninety women aged 55–59, 267 women aged 70–79 and 235 men aged 70–79 were studied. High frequency of ApoE4 and a higher incidence of femoral neck fractures in Caucasians were shown in other studies.Citation120,Citation121 presents some of the genes known to be involved in the etiology of bone disorders.
Table 1 Candidate genes associated with osteoporosis
Medication
Synthetic glucocorticoids are administered to treat disorders caused by autoimmune, pulmonary and gastrointestinal diseases, as well as in patients receiving organ transplantation and with malignancies.Citation122 Glucocorticoids cause profound effects on the skeleton, and glucocorticoid-induced osteoporosis is the most common secondary cause of osteoporosis.Citation122,Citation123 Glucocorticoids induce a biphasic bone loss with a rapid initial phase showing 10%–20% bone loss in as little as 3 months of therapy and a slower phase of 2%–5% bone loss annually.Citation124 They increase the expression of receptor activator for nuclear factor κ-B ligand (RANKL) and decrease the expression of its soluble decoy receptor, osteoprotegerin (OPG), in stromal and osteoblastic cells, leading to elevated bone resorption.Citation123 Glucocorticoids inhibit osteoblast cell differentiation by increasing the expression of dickkopf, an inhibitor of Wnt signaling, and opposing Wnt signaling.Citation125 Glucocorticoids suppress IGF-I gene transcriptionCitation123 which is responsible for bone formation and the synthesis of type I collagen.Citation126
Hyperparathyroidism
Primary hyperparathyroidism (PHPT) is a calcium metabolic disorder with the highest incidence in postmenopausal women.Citation127 Several studies have shown decreased BMD in patients with PHPT.Citation128 Vestergaard et alCitation129 reported high fracture risk of the forearms and the vertebrae in a group of 674 patients with PHPT. PTH is normally the major regulator of calcium homeostasis and functions mainly on kidney and bone.Citation130 It acts on kidney cells by increasing the renal tubular reabsorption of calcium and as well as the conversion of 25-hydroxy vitamin D (25-(OH)D) to 1,25(OH)2D through activation of 1α-hydroxylase.Citation131,Citation132 In vitro and in vivo studies confirm that PTH directly activates survival signaling in osteoblasts and increases osteoblast number.Citation133 Indeed, the preosteoblastic precursors and preosteoblasts possess receptors for PTH, which induces differentiation from the precursor to osteoblast.Citation134 The fibroblast growth factor-2, which primarily produced by osteocytes in bone, regulating phosphate metabolism through its inhibitory effects on the renal sodium-phosphate contransporter.Citation135 However, increased secretion of PTH in PHPT leads to elevated serum calcium levels due to release from the bone stores. This has been shown to increase the risk of osteoporosis by increasing the rate of bone turnover.Citation130
Rheumatoid arthritis (RA)
RA is the most common form of inflammatory disease in adults characterized by progressive and systemic inflammation.Citation136 RA is associated with osteoporosis due to active systemic inflammation, immobilization and the use of glucocorticoids.Citation137 Osteoporosis occurs in two forms in RA: 1) generalized bone loss with axial distribution including the spine, pelvis, hips, ribs and humerus and 2) periarticular or localized bone loss in the proximity of the inflamed joints.Citation138 Several studies reported that the rate of spine or hip fractures is higher in patients with RA compared with primary osteoporotic patients.Citation139–Citation142 Histomorphometric and biochemical markers analysis indicates that generalized bone loss in RA is related to a decrease in bone formation and increase in bone resorption.Citation143 Rheumatoid synovial tissues are enriched with bone-resorbing cytokines including IL-1α and IL-1β, tumor necrosis factor (TNF)-α, macrophage colony-stimulating factor, IL-6, IL-11, PTH-related peptide and the newly described T-cell–derived cytokine IL-17.Citation144–Citation150 The interaction of RANK with its ligand (RANKL) has been identified as a common pathway to control the differentiation, proliferation and survival of osteoclasts.Citation151 Expression of RANKL is upregulated by inflammatory cytokines. RANKL, also known as TRANCE (TNF-related activation induced cytokine), is a membrane-bound TNF receptor. RANKL is expressed on osteoblast precursor cells that interact with RANK on the osteoclast surface. OPG, a soluble decoy receptor protein, is produced by osteoblast/stromal cells that bind to RANKL and prevent its binding to RANK on the preosteoclast cells.Citation152–Citation154 OPG protects against TNF-induced bone loss.Citation155 TNF, as a potent inducer of dickkopf-related protein 1 (DKK-1), can inhibit the wingless (Wnt) signaling pathway and expression of OPG, leading to bone formation limitation.Citation156 TNF-α promotes the production of proinflammatory cytokines (eg, IL-1, IL-6 and IL-8) in RA. TNF-α also prolongs osteoclasts’ lifespan or it may promote osteoclast formation by directly stimulating its precursors.Citation157,Citation158
Diabetes mellitus
Diabetes mellitus is a debilitating metabolic disease with substantial morbidity characterized by hyperglycemia resulting from defects in insulin secretion and/or insulin action.Citation159 In the USA, about 8% of youth have diabetesCitation160 and it has been predicted that the number of Americans with diabetes will rise from 11 million in 2000 to 29 million in 2050.Citation161
Reports about the prevalence of diabetes mellitus in Saudi Arabia estimate the current prevalence to be around 17%, with expectations that it will peak to >20% by the year 2030. Advanced age, oral hypoglycemic agents and vitamin D deficiency are determinants of decreased BMD in Saudi women with type 2 diabetes.Citation162 Skeletal disorders in diabetes may be caused by multiple mechanisms including changes in insulin and IGF levels, hypercalciuria associated with glycosuria, reduced renal function, obesity, higher concentrations of advanced glycation end products (AGEs) in collagen, angiopathies, neuropathies and inflammation.Citation163–Citation166 Comparison of BMD values in type 1 and type 2 diabetic patients of similar age showed that type 1 diabetes mellitus (T1DM) is associated with reduction in BMD. However, type 2 diabetes mellitus (T2DM) can be related to increased BMD.Citation167 It can be speculated that T1DM and T2DM are associated with higher fracture risk.Citation168 Schwartz et al in a study of osteoporotic fractures, confirmed that women with T2DM experience higher fracture rates in hip, humerus and foot than nondiabetic women.Citation169 A previous research by Nicodemus and FolsomCitation170 evaluated the incidence of hip fracture (1.6 per 1,000 person-years). A statistically significant positive association between T2DM and hip fracture incidence was found. Women with T1DM had 12.25 (95% CI 5.05–29.73) times higher risk of hip fracture compared with nondiabetic women. Women with T2DM were 1.70-fold more likely than women without diabetes to sustain a hip fracture.Citation170,Citation171 This rate is consistent with that reported in a similar survey by the National Hospital Discharge.Citation172 Women with T2DM who were treated with insulin and nondiabetic women had similarly lower risk for hip fracture.Citation173 Diabetic patients usually have an elevated risk of falling because of vision-related risk factors including diabetic retinopathy, advanced cataracts, laser therapy for retinopathy, hypoglycemia and also balance-related risk factors such as peripheral neuropathy, foot ulcers, polyuria, nocturia and decreased reflexes.Citation169,Citation174 Hip fracture risk increases in both T1DM and T2DM due to increased risk of falling and not decreased BMD.Citation174 Insulin has been proposed to be an anabolic agent in bone, capable of stimulating osteoblast proliferation and differentiation. It has been reported that insulin stimulates increase of human osteoblastic cell line MG-6 in a time- and dose-dependent manner, and blockade of both MAPK and PI3K pathways could inhibit cell proliferation.Citation175 Data obtained in this study suggested that insulin promoted ALP activity, which is a bone formation enzyme secreted by osteoblasts,Citation176 the secretion of type I collagen, OC gene expression and mineralized nodule formation. Insulin also upregulates osterix (Osx) and IGF-1 expression through ERK and significantly downregulates runt-related transcription factor 2 (Runx2) expression through MAPK pathway.Citation175,Citation177 High glucose inhibits cell growth, mineralization and expression of osteogenic markers including Runx2, collagen I, OC and osteonectin.Citation177 Adipogenesis or lipogenesis is still active in diabetic type I bone, and the number of lipid-dense adipocytes and the expression of adipogenic markers (peroxisome proliferator-activated receptor-γ [PPARγ2], resistin, adipocyte fatty acid binding protein [aP2] and adipsin) are increased.Citation178 PPARγ levels lead to increased adipogenesis in mice with a dominant suppressive influence on osteogenesis.Citation178,Citation179 It is recognized that fatty acids can activate PPARγ2 and suppress ALP expression in osteoblastic cells.Citation180 In addition to hyperglycemia, impaired leptin function may indirectly be related to osteoporosis in DM, since leptin receptor knockout mice showed an increase in bone mass compared to normal mice.Citation181,Citation182 Some BMP and TGF-β signaling pathway inhibitors including DKK-1,Citation183,Citation184 sclerostin,Citation185 gremlin,Citation186 PTH,Citation187 angiotensin II (Ang-II),Citation188 IL-6Citation189 and TNFsCitation190 are overexpressed in DM. DM also sequesters the overexpression of vitamin D required for the normal growth of osteoblasts.Citation191 Vitamin D increases the uptake of calcium and phosphorus and improves calcium reabsorption by the kidney, thus resulting in maintenance of mineral homeostasis and regulation of bone remodeling.Citation192 DM decreases the expression of endothelial progenitor cells derived from bone and, consequently, the rate of angiogenesis required for bone healing.Citation193 Pancreatic β cells also produce amylin and preptin. It is known that amylin causes bone formation and blocks bone resorption. Preptin induces osteoblast differentiation and mineralization and also decreases osteoblast apoptosis. DM reduces the production of OC that regulates osteogenesis positively.Citation194 It can be speculated that formation of AGEs plays a crucial role in the pathogenesis of diabetic neuropathy.Citation195 Under hyperglycemic conditions, levels of methylglyoxal, 3-deoxyglucosone and glyceraldehyde increase, leading to the formation of AGEs which signal through the receptor for advanced glycation end product expressed on the nerve cells, resulting in different types of cytokine production, which may have roles in nerve damage as well as deleterious effect on nerve cells because they modify neuronal proteins including tubulin, neurofilament, laminin and actin through glycation, and thereby sequester the nerve function.Citation196 In a recent study, Catalano et al have shown that lower bone formation and increased bone resorption, although not statistically significant, were observed in patients with poor metabolic control in comparison to patients with good metabolic control. Therefore, poor metabolic control may worsen the quality of bone in T1DM. Phalangeal quantitative ultrasound could be considered as a tool to screen T1DM women for osteoporosis in premenopausal age.Citation197 However, Neumann et al showed that trabecular bone score was lower in T1DM patients with prevalent fractures in comparison to healthy controls, suggesting an alteration of bone strength in this subgroup of patients.Citation198
Walsh and Vilaca believe that BMI is positively associated with BMD, and the mechanisms of this association in vivo may include increased loading, adipokines such as leptin and higher aromatase activity. However, some fat depots could have negative effects on bone; T2DM is also associated with higher BMD, but increased overall and hip fracture risk. There are some similarities between bone in obesity and T2DM, but T2DM seems to have additional harmful effects where glycation of collagen may be an important factor. Higher BMD but higher fracture risk presents challenges in fracture prediction in obesity and T2DM. It seems that osteoporosis treatment does reduce the fracture risk in obesity and T2DM with generally similar efficacy to that in other patients.Citation199 A very recent meta-analysis strongly supported the association between T2DM and increased risk of overall fracture. These findings emphasize the need for fracture prevention strategies in patients with diabetes.Citation200
Dementia
Osteoporosis and Alzheimer’s disease (AD) are common chronic degenerative disorders prevalent in elderly people. The large majority of AD cases occur sporadically by genetic mutation, aging and environmental factors as pathogenic mechanisms. Osteoporosis is a multifactorial, mostly polygenetic disease, and no single factor can completely account for their occurrence as well. Common risk factors in both diseases include body mass loss, vitamin D deficiencies, less exposure to sunlight and less physical activity.Citation201 Evatt et alCitation251 showed a substantial incidence of vitamin D deficiency among Parkinson’s disease cohort patients compared with the AD patients and control cohorts. It can be speculated that Parkinson’s disease may cause patients to have decreased activity levels and lower sunlight exposure. In 2003, Weller and Schatzker from Canada observed that femoral neck fractures were more prevalent in patients with AD compared to those without the disease.Citation202 The incidence of hip fracture, the most common type of fracture, among patients with AD (17.4 per 1,000 person-years) was consistently higher than in patients without AD (6.6 per 1,000 person-years). In both men and women with AD, the incidence rate of sustaining a hip fracture was the same. Among the patients who experienced a hip fracture, approximately one-third (32.4%) of AD patients and 18.8% of non-AD patients did not survive >1 year after a hip fracture,Citation203 which is consistent with another study in which Haasum et alCitation204 confirmed that hip fractures occurred in 16% of the people with dementia and 3% of the people without dementia. AD also could increase the incidence rate of osteoporosis through the neurotoxic effects of amyloid beta (Aβ), a 40–42 aminoacid peptide considered to play a role in the development of AD.Citation205 Aβ leads to increased levels of H2O2, one of the main reactive oxygen species (ROS), resulting in free radical damage.Citation206 H2O2 and peroxides are potent inducers of osteoclastogenesis.Citation207 Osteoclasts are cells that are derived from the monocyte–macrophage cell lineage and strongly participate in bone resorption. It is known that different types of mediators including nuclear factor κB (NF-κβ), RANKL, osteopontin, PTH, macrophage colony stimulating factor and angiotensin-II play outstanding roles to induce osteoclastogenesis.Citation208 RANKL is a key element derived from osteoblasts and stromal cells and stimulates the differentiation of preosteoclast to osteoclast through activating NF-κβ, as well as induces nuclear factor of activated T cells (NFAT) by ROS-mediated pathway.Citation207,Citation209 Park et alCitation210 found that RANKL stimulation induces a novel signaling pathway that leads to generation of ROS and calcium oscillations and is essential for osteoclastogenesis. The constant RANKL-induced calcium oscillations result in activation of NFATc1 and osteoclast differentiation to mediate bone remodeling.Citation211 Hence, it is seen that OC, a marker of bone matrix synthesis, increases in osteoporosis (63%) and substantially in AD (76%) versus controls, while there is no change visible in cases with mild cognitive impairment.Citation212
Cancer
Cancer-induced bone disease can originate from the primary disease itself or from therapies administered to treat the cancer. Bone metastases are a common consequence of cancer, leading to pathologic fractures. Bone is the most common site for metastasis in cancer and is of particular clinical importance in breast and prostate cancers because of the prevalence of these diseases. At postmortem examination, ~70% of patients dying of these cancers have evidence of metastatic bone disease.Citation213 It has estimated that ~350,000 people in the USA die annually of bone metastases.Citation214 Bone metastases predominantly includes osteolytic or osteoblastic metastases. Osteolysis might be caused by parathyroid-hormone-related peptide (PTHrP) released by tumor cells in the bone microenvironment that stimulate the production of the cytokine RANKL leading to osteoclast activation.Citation214,Citation215 Osteoblastic metastases are caused by osteoblast proliferation, differentiation and bone formation.Citation216 On the other hand, treatment-induced osteoporosis may occur as a result of androgen deprivation therapy (ADT), glucocorticoid therapy, chemotherapy-induced ovarian failure and estrogen deprivation therapy.Citation217
ADT as a treatment for metastatic prostate cancer increases the risk of osteoporosis in men with prostate cancer associated with a gradual decline in BMD at the hip.Citation218 ADT administration by orchiectomy (surgical removal of the testes) or by luteinizing hormone releasing hormone injections suppresses the production of testosterone which is necessary to maintain bone mineralization.Citation219,Citation220 Radiation treatment for prostate cancer also leads to bone injury through a fall in blood flow and bone tissue oxygenation as well as reduction of bone-forming cells and bone atrophy.Citation221 Dickman et al showed that the risk of hip fracture from diagnosis until death was 1.6 in men exposed to ADT within 6 months of diagnosis, compared to control men in a Swedish population.Citation221 Breast and prostate cancer treatments that cause hypogonadism disrupt the normal bone remodeling process because estrogen and testosterone have been shown to play a key role in bone health in both men and women.Citation223
Pharmacologic treatment
Most of the studies have focused on the effects of anabolic therapies and antiresorptive therapies on generalized bone loss.
Anabolic therapy
This type of osteoporosis therapy refers to the usage of drug components, that is, recombinant hormones such as rhPTH (1–34); hPTH (1–84) for strengthening, stimulating bone synthesis and treating the disease;Citation224 calcium supplements to prevent bone resorption and to increase BMD;Citation223 short-term treatment with calcimimeticsCitation225 and PTH to increase trabecular bone mass and cortical bone mass.Citation225
Antiresorptive therapy
This kind of therapy is applied for osteoporosis treatment due to its effect on strengthening the bone. The therapy consists of five types of chemical components, that is, bisphosphonate, a class of antiresorptive drugs which can affect osteoclast activity,Citation226,Citation227 hormone replacement therapy for the treatment of osteoporosis and particularly for relief of menopausal symptoms,Citation228 tibolone, a synthetic steroid used for early post menopausal women, leading to increase BMD due to extend of estrogen replacement therapy therapy,Citation229 selective ER modulators such as raloxifene used for the treatment of postmenopausal osteoporosis increase BMD and reduce the risk of vertebral fracture,Citation230 bazedoxifene inhibits estrogen-induced responses in mammary glands in animal modelsCitation231 and in conjugation with estrogen is used for the treatment of menopausal osteoporosis,Citation227 and anti-RANKL antibodyCitation226 and cathepsin K inhibitors, inducing bone mineral density (BMD) gain in a phase II study in postmenopausal osteoporosis patients.Citation232
Influence of lifestyle on osteoporosis risk
Different societies have different information and awareness about health. In a report about knowledge and health beliefs on osteoporosis in a sample of 262 men aged 36–55 years, it was revealed that level of osteoporosis knowledge and perceived susceptibility were low. Given the increased prevalence of osteoporosis-related fracture in men, there is a need to develop methods to increase knowledge and awareness.Citation233 Observational findings suggest weight-bearing physical activity may influence bone strength due to favorable geometric adaptation, independent of changes in BMD. Overall, young healthy individuals with “average” baseline bone mass are unlikely to display notable changes in parameters of bone strength. While exercise interventions in pediatric cohorts have been primarily jump-based programs, exercise protocols in older adult trials have varied by mode, intensity, frequency and duration.Citation234 Among physical activities, walking is not effective in osteoporosis prevention, as it only provides a modest increase in the loads on the skeleton above gravity.Citation235 The menopausal women may improve the muscle strength and physical activities levels by exercise intervention for reducing the osteoporotic and sarcopenic risk.Citation236
Discussion
Osteoporosis originates from loss of bone mass along with microarchitectural deterioration of the skeleton. Bone mass starts decreasing among men and women in their 40s, leading to increased risk of fragility fractures. However, women lose bone more rapidly, particularly during the first 5–10 years after menopause due to estrogen deficiency, while men experience a slow loss of bone.Citation237 Multiple risk factors are associated with low bone density-related fractures. Significant associations include advancing age, white race, history of prior fractures and genetic factors. Modifiable factors such as increased alcohol consumption and smoking are also prominent. Furthermore, chronic glucocorticoid use, hypogonadism, diabetes, dementia and RA were discussed as secondary causes of osteoporosis in the current review.
Since osteoporosis is asymptomatic, early diagnosis can help in deciding treatment strategies and preventing disease progress. On the other hand, many metabolic bone diseases including hyperparathyroidism and osteomalacia also are associated with low BMD. Thus, a conclusive test is essential to diagnose osteoporosis and future fracture risk prediction. Several methods of imaging have been developed to measure bone density and decide treatment strategies.Citation238 Fracture Risk Assessment Tool is an algorithm used to evaluate the 10-year probability of hip fracture and major osteoporotic fracture (spine, proximal humerus and forearm) risk in either men or women that integrates clinical risk factors (individual’s age, sex, weight, height, prior fracture, parental history of hip fracture, smoking, long-term use of glucocorticoids, RA and alcohol consumption) and BMD at the femoral neck in its calculations.Citation239 With regard to the clinical consequenses and heavy economic burden of fractures in the aging population, significant efforts to decrease fracture risk are needed. Our study updates reviews on available treatments for osteoporosis.
The two key elements in treating osteoporosis are increasing the bone mass by using anabolic therapies and decreasing bone resorption through antiresorptive therapies.
First and foremost, regular physical activity is recommended in all age groups to maximize peak bone mass and maintain bone strength.Citation240 Physical activity has been suggested as a nonpharmacologic intervention for increasing bone density in youth and preventing bone loss in the elderly.Citation241 Both aerobic exercise and resistance training, the best forms of weight-bearing exercise, increase the rate of bone remodeling in postmenopausal women. However, resistance exercise training induces more effective favorable changes in BMD status than aerobic exercise training in postmenopausal women.Citation242 These findings are consistent with a previous study which showed that resistance exercise had a significant protective influence on several changes associated with loss of BMD, unfavorable changes in serum and urinary bone markers and hypercalciuria.Citation243 A 10% increase in peak bone mass was predicted to delay the development of osteoporosis by 13 yearsCitation244 and reduce the risk of fragility fractures after menopause by 50%.Citation245 Adequate daily calcium and vitamin D is required to maximize bone mass and for the subsequent maintenance of bone health.Citation246 The National Osteoporosis Foundation recommends that postmenopausal women should consume at least 1,200 mg per day of calcium and 800–1,000 international units of vitamin D per day.Citation247 With an unhealthy diet, calcium and vitamin D supplementations may be needed. Dietary supplementation with calcium and vitamin D reduced bone loss and the rate of nonvertebral fractures in both 65-year-old men and women during a 3-year study.Citation248 Other active osteoporosis therapies should be considered for adjunctive treatment with calcium and vitamin D.Citation249 Osteoporosis is a challenging human disease. In spite of using various therapeutic approaches for the prevention or treatment of osteoporosis, their side effects are undeniable. Increasing our knowledge about the signaling pathways involved in bone remodeling will help us to design new therapeutic options for osteoporosis.
Acknowledgments
We would like to express our sincere thanks to Ms Atieh Abedin from the medical genetics group, Shahid Beheshti University of Medical Sciences, for her efforts in manuscript editing.
Disclosure
The authors report no conflicts of interest in this work.
References
- BouillonRBurckhardtPChristiansenCConsensus development conference: prophylaxis and treatment of osteoporosisAm J Med1991901071101986575
- KanisJAMeltonLJChristiansenCJohnstonCCKhaltaevNThe diagnosis of osteoporosisJ Bone Miner Res19949113711417976495
- ConsensusNDevelopment panel on osteoporosis: prevention, diagnosis and therapyJAMA200128578579511176917
- HolroydCCooperCDennisonEEpidemiology of osteoporosisBest Pract Res Clin Endocrinol Metab20082267168519028351
- LaneNEEpidemiology, etiology, and diagnosis of osteoporosisAm J Obstet Gynecol2006194S3S1116448873
- RoubenoffRKehayiasJJThe meaning and measurement of lean body massNutr Rev1991491631752046978
- JohnellOKanisJAAn estimate of the worldwide prevalence and disability associated with osteoporotic fracturesOsteoporos Int2006171726173316983459
- KepleyALNishiyamaKKZhouBDifferences in bone quality and strength between Asian and Caucasian young menOsteoporos Int20172854955827638138
- LeiSChenYXiongDLiLDengHEthnic difference in osteoporosis-related phenotypes and its potential underlying genetic determinationJ Musculoskelet Neuronal Interact200663616675888
- CauleyJADefining ethnic and racial differences in osteoporosis and fragility fracturesClin Orthop Relat Res20114691891189921431462
- SugimotoTSatoMDehleFCBrnabicAJWestonABurgeRLifestyle-related metabolic disorders, osteoporosis, and fracture risk in Asia: a systematic reviewValue Health Reg Issues20169495627881259
- MeltonLJThe prevalence of osteoporosisJ Bone Miner Res199712176917719383680
- KlibanskiAAdams-CampbellLBassfordTLOsteoporosis prevention, diagnosis, and therapyJAMA200128578579511176917
- CooperCCampionGMeltonLRHip fractures in the elderly: a world-wide projectionOsteoporos Int199222852891421796
- MeltonLHip fractures: a worldwide problem today and tomorrowBone199314188442996
- SterlingRSGender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and functionClin Orthop Relat Res20114691913191821161737
- HaentjensPMagazinerJColón-EmericCSMeta-analysis: excess mortality after hip fracture among older women and menAnn Intern Med201015238039020231569
- HawkesWGWehrenLOrwigDHebelJRMagazinerJGender differences in functioning after hip fractureJ Gerontol A Biol Sci Med Sci20066149549916720747
- MeltonLJKanSHFryeMAWahnerHWO’FallonWMRiggsBLEpidemiology of vertebral fractures in womenAm J Epidemiol1989129100010112784934
- CooperCO’NeillTSilmanAEVOS GroupThe epidemiology of vertebral fracturesBone1993148997
- OglesbyAKMinshallMEShenWXieSSilvermanSLThe impact of incident vertebral and non-vertebral fragility fractures on health-related quality of life in established postmenopausal osteoporosis: results from the teriparatide randomized, placebo-controlled trial in postmenopausal womenJ Rheumatol2003301579158312858462
- NevittMCEttingerBBlackDMThe association of radiographically detected vertebral fractures with back pain and function: a prospective studyAnn Intern Med19981287938009599190
- FelsenbergDSilmanALuntMIncidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS)J Bone Miner Res20021771672411918229
- FurlleipnlszAVertebral fractures and mortality in older womenArch Intern Med19991591215122010371229
- LicataAGeusensPFlowersKSeemanERisk of new vertebral fracture in the year following a fractureJAMA2001285332032311176842
- DuanYParfittAMSeemanEVertebral bone mass, size, and volumetric density in women with spinal fracturesJ Bone Miner Res1999141796180210491228
- VegaEGhiringhelliGMautalenCRey ValzacchiGScagliaHZylbersteinCBone mineral density and bone size in men with primary osteoporosis and vertebral fracturesCalcif Tissue Int1998624654699541527
- BriggsAGreigAWarkJThe vertebral fracture cascade in osteoporosis: a review of aetiopathogenesisOsteoporos Int20071857558417206492
- NellansKWKowalskiEChungKCThe epidemiology of distal radius fracturesHand Clinics20122811312522554654
- ShinEJupiterJCurrent concepts in the management of distal radius fracturesActa Chir Orthop Traumatol Cech20077423324617877939
- BrogrenEPetranekMAtroshiIIncidence and characteristics of distal radius fractures in a southern Swedish regionBMC Musculoskeletal Disorders200784817540030
- O’neillTCooperCFinnJUK Colles’ Fracture StudyIncidence of distal forearm fracture in British men and womenOsteoporos Int20011255555811527052
- NevittMCCummingsSRType of fall and risk of hip and wrist fractures: the study of osteoporotic fracturesJ Am Geriatr Soc199341122612348227898
- OmslandTKAhmedLAGrønskagAMore forearm fractures among urban than rural women: the NOREPOS study based on the Tromsø study and the HUNT studyJ Bone Miner Res20112685025621061241
- CuddihyMTGabrielSECrowsonCO’FallonWMeltonLJForearm fractures as predictors of subsequent osteoporotic fracturesOsteoporos Int1999946947510624452
- MallminHLjunghallSPerssonINaessénTKrusemoUBBergströmRFracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-upCalcif Tissue Int1993522692728467406
- LauritzenJBSchwarzPMcNairPLundBTransbølIRadial and humeral fractures as predictors of subsequent hip, radial or humeral fractures in women, and their seasonal variationOsteoporos Int199331331378481589
- GouldingARisk factors for fractures in normally active children and adolescentsDalyRMPetitMAOptimizing Bone Mass and StrengthBaselKarger Publishers2007102120
- TeitelbaumSLBone resorption by osteoclastsScience20002891504150810968780
- ZaidiMSkeletal remodeling in health and diseaseNat Med20071379180117618270
- CohenJEWakefieldCECohnRJNutritional interventions for survivors of childhood cancerCochrane Database Syst Rev20168CD009678
- LevisSLagariVSThe role of diet in osteoporosis prevention and managementCurr Osteoporos Rep20121029630223001895
- ShinSSungJJoungHA fruit, milk and whole grain dietary pattern is positively associated with bone mineral density in Korean healthy adultsEur J Clin Nutr20156944244825351648
- ChanRChanDWooJA cross sectional study to examine the association between dietary patterns and cognitive impairment in older Chinese people in Hong KongJ Nutr Health Aging20131775776524154648
- MareszKProper calcium use: vitamin K2 as a promoter of bone and cardiovascular healthIntegr Med (Encinitas)2015143439
- WatanabeDHottaMIchiharaAOsteomalacia, severe thoracic deformities and respiratory failure in a young woman with anorexia nervosaIntern Med20155492993425876575
- SommerIErkkilaATJarvinenRAlcohol consumption and bone mineral density in elderly womenPublic Health Nutr20131670471222800300
- NachtigallMJNazemTGNachtigallRHGoldsteinSROsteoporosis risk factors and early life-style modifications to decrease disease burden in womenClin Obstet Gynecol20135665065324100599
- ZhangXYuZYuMQuXAlcohol consumption and hip fracture riskOsteoporos Int20152653154225266483
- PaccouJEdwardsMHWardKRelationships between bone geometry, volumetric bone mineral density and bone microarchitecture of the distal radius and tibia with alcohol consumptionBone20157812212925959415
- Ortego-CentenoNMunoz-TorresMJodarEHernandez-QueroJJurado-DuceAde la Higuera Torres-PucholJEffect of tobacco consumption on bone mineral density in healthy young malesCalcif Tissue Int1997604965009164822
- KlineJTangALevinBSmoking, alcohol and caffeine in relation to two hormonal indicators of ovarian age during the reproductive yearsMaturitas20169211512227621248
- KrallEADawson-HughesBSmoking and bone loss among postmenopausal womenJ Bone Miner Res199163313381858519
- KrallEADawson-HughesBSmoking increases bone loss and decreases intestinal calcium absorptionJ Bone Miner Res1999142152209933475
- JensenJChristiansenCRødbroPCigarette smoking, serum estrogens, and bone loss during hormone-replacement therapy early after menopauseN Engl J Med19853139739754047104
- JickHPorterJMorrisonARelation between smoking and age of natural menopause: report from the Boston Collaborative Drug Surveillance Program, Boston University Medical CenterThe Lancet197730913541355
- TalmageRVMobleyHCalcium homeostasis: reassessment of the actions of parathyroid hormoneGen Comp Endocrinol20081561818160068
- NormanAWVitamin D metabolism and calcium absorptionAm J Med197967989998229729
- BrotCJorgensenNSorensenOThe influence of smoking on vitamin D status and calcium metabolismEur J Clin Nutr19995392092610602348
- KoCHChanRLSiuWSDeteriorating effect on bone metabolism and microstructure by passive cigarette smoking through dual actions on osteoblast and osteoclastCalcif Tissue Int20159638940025694359
- BunceCMBrownGHewisonMVitamin D and hematopoiesisTrends Endocrinol Metab1997824525118406812
- FerrariSBonjourJPRizzoliRThe vitamin D receptor gene and calcium metabolismTrends Endocrinol Metab1998925926518406281
- WaltersMRNewly identified actions of the vitamin D endocrine systemEndocr Rev1992137197641333949
- MorrisonNAYeomanRKellyPJEismanJAContribution of transacting factor alleles to normal physiological variability: vitamin D receptor gene polymorphism and circulating osteocalcinProc Natl Acad Sci U S A199289666566691353882
- HausslerMRWhitfieldGKHausslerCAThe nuclear vitamin D receptor: biological and molecular regulatory properties revealedJ Bone Miner Res1998133254499525333
- KurabayashiTMatsushitaHTomitaMAssociation of vitamin D and estrogen receptor gene polymorphism with the effects of longterm hormone replacement therapy on bone mineral densityJ Bone Miner Metab20042224124715108066
- MorrisonNAQiJCTokitaAPrediction of bone density from vitamin D receptor allelesNature19943672842878161378
- SainzJVan TornoutJMLoroMLSayreJRoeTFGilsanzVVitamin D–receptor gene polymorphisms and bone density in prepubertal American girls of Mexican descentN Engl J Med199733777829211676
- GennariLBecheriniLMasiLVitamin D and estrogen receptor allelic variants in Italian postmenopausal women: evidence of multiple gene contribution to bone mineral densityJ Clin Endocrinol Metab1998839399449506753
- LiuYZLiuYJReckerRRDengHWMolecular studies of identification of genes for osteoporosis: the 2002 updateJ Endocrinol200317714719612740006
- Dawson-HughesBHarrisSSFinneranSCalcium absorption on high and low calcium intakes in relation to vitamin D receptor genotypeJ Clin Endocrinol Metab199580365736618530616
- WillingMSowersMAronDBone mineral density and its change in white women: estrogen and vitamin D receptor genotypes and their interactionJ Bone Miner Res1998136957059556070
- PouresmaeiliFJJAzargashbESamangoueeSAssociation between vitamin D receptor gene BsmI polymorphism and bone mineral density in a population of 146 Iranian womenCell J2013157882
- ChengJBelgraderPZhouXMaquatLEIntrons are cis effectors of the nonsense-codon-mediated reduction in nuclear mRNA abundanceMol Cell Biol199414631763258065363
- NesicDChengJMaquatLESequences within the last intron function in RNA 3′-end formation in cultured cellsMol Cell Biol199313335933697684497
- SpectorTKeenRArdenNInfluence of vitamin D receptor genotype on bone mineral density in postmenopausal women: a twin study in BritainBMJ1995310135713607787536
- GrossCEccleshallTRMalloyPJVillaMLMarcusRFeldmanDThe presence of a polymorphism at the translation initiation site of the vitamin D receptor gene is associated with low bone mineral density in postmenopausal Mexican-American womenJ Bone Miner Res199611185018558970885
- AraiHMiyamotoKITaketaniYA vitamin D receptor gene polymorphism in the translation initiation codon: effect on protein activity and relation to bone mineral density in Japanese womenJ Bone Miner Res1997129159219169350
- ZajíčkováKOfkováIBahbouhRKřepelováAVitamin D receptor gene polymorphisms, bone mineral density and bone turnover: FokI genotype is related to postmenopausal bone massPhysiol Res20025150150912470203
- MitraSDesaiMKhatkhatayMIVitamin D receptor gene polymorphisms and bone mineral density in postmenopausal Indian womenMaturitas200655273516464547
- AraiHMiyamotoKIYoshidaMThe polymorphism in the caudal-related homeodomain protein Cdx-2 binding element in the human vitamin D receptor geneJ Bone Miner Res2001161256126411450701
- YamamotoHMiyamotoKILiBThe caudal-related homeodo-main protein Cdx-2 regulates vitamin D receptor gene expression in the small intestineJ Bone Miner Res1999142402479933478
- YoonKRutledgeSBuenagaRFRodanGACharacterization of the rat osteocalcin gene: stimulation of promoter activity by 1, 25-dihydroxyvitamin D3Biochemistry198827852185263265336
- TokitanAMatsumotoHMorrisonNAVitamin D receptor alleles, bone mineral density and turnover in premenopausal Japanese womenJ Bone Miner Res199611100310098797122
- GennariLMerlottiDDe PaolaVEstrogen receptor gene polymorphisms and the genetics of osteoporosis: a HuGE reviewAm J Epidemiol200516130732015692074
- KorachKSEstrogen receptor knock-out mice: molecular and endocrine phenotypesJ Soc Gynecol Investig20007S16S17
- VidalOLindbergMKHollbergKEstrogen receptor specificity in the regulation of skeletal growth and maturation in male miceProc Natl Acad Sci U S A2000975474547910805804
- WindahlSVidalOAnderssonGGustafssonJ-AOhlssonCIncreased cortical bone mineral content but unchanged trabecular bone mineral density in female ERβ−/− miceJ Clin Invest199910489590110510330
- LindbergMAlataloSHalleenJMohanSGustafssonJAOhlssonCEstrogen receptor specificity in the regulation of the skeleton in female miceJ Endocrinol200117122923611691642
- JuradaSMarcJPreželjJKocijančičAKomelRCodon 325 sequence polymorphism of the estrogen receptor α gene and bone mineral density in postmenopausal womenJ Steroid Biochem Mol Biol200178152011530279
- OngphiphadhanakulBChanprasertyothinSPayattikulPAssociation of a T262C transition in exon 1 of estrogen-receptor-α gene with skeletal responsiveness to estrogen in post-menopausal womenJ Endocrinol Invest20012474975511765043
- OngphiphadhanakulBChanprasertyothinSPayattikulPAssociation of a G2014A transition in exon 8 of the estrogen receptor-α gene with postmenopausal osteoporosisOsteoporos Int2001121015101911846326
- LangdahlBLLøkkeECarstensMStenkjaerLLEriksenEFA TA repeat polymorphism in the estrogen receptor gene is associated with osteoporotic fractures but polymorphisms in the first exon and intron are notJ Bone Miner Res2000152222223011092403
- KobayashiTSugimotoTKobayashiAChiharaKVitamin D receptor genotype is associated with cortical bone loss in Japanese patients with primary hyperparathyroidismEndocr J1998451231259625456
- KobayashiNFujinoTShiroganeTEstrogen receptor α polymorphism as a genetic marker for bone loss, vertebral fractures and susceptibility to estrogenMaturitas20024119320111886765
- MizunumaHHosoiTOkanoHEstrogen receptor gene polymorphism and bone mineral density at the lumbar spine of pre- and postmenopausal womenBone1997213793839356730
- AlbaghaOMMcGuiganFEReidDMRalstonSHEstrogen receptor α gene polymorphisms and bone mineral density: haplotype analysis in women from the United KingdomJ Bone Miner Res20011612813411149476
- PouresmaeiliFRoohiATehraniMOsteoporosis and its association with estrogen receptor-alpha gene polymorphism in a population of iranian women referring to loghman hospitalInt J Endocrinol Metab20092009193199
- van MeursJBSchuitSCWeelAEAssociation of 5′ estrogen receptor alpha gene polymorphisms with bone mineral density, vertebral bone area and fracture riskHum Mol Genet2003121745175412837697
- NawataHTanakaSTanakaSAromatase in bone cell: association with osteoporosis in postmenopausal womenJ Steroid Biochem Mol Biol1995531651747626449
- TranBNNguyenNDCenterJREismanJANguyenTVEnhancement of absolute fracture risk prognosis with genetic marker: the collagen I alpha 1 geneCalcif Tissue Int20098537919789904
- ChuMDe WetWBernardMRamirezFFine structural analysis of the human pro-alpha 1 (I) collagen gene. Promoter structure, AluI repeats, and polymorphic transcriptsJ Biol Chem1985260231523202857713
- RossouwCVergeerWDu PlooySBernardMRamirezFDe WetWDNA sequences in the first intron of the human pro-alpha 1 (I) collagen gene enhance transcriptionJ Biol Chem198726215151151572822714
- BrownMAHaughtonMAGrantSFGunnellASHendersonNKEismanJAGenetic control of bone density and turnover: role of the collagen 1α1, estrogen receptor, and vitamin D receptor genesJ Bone Miner Res20011675876411316004
- KeenRSniederHMolloyHEvidence of association and linkage disequilibrium between a novel polymorphism in the transforming growth factor β1 gene and hip bone mineral density: a study of female twinsRheumatology200140485411157141
- YamadaYMiyauchiATakagiYTanakaMMizunoMHaradaAAssociation of the C–509→ T polymorphism, alone or in combination with the T869→ C polymorphism, of the transforming growth factor-β1 gene with bone mineral density and genetic susceptibility to osteoporosis in Japanese womenJ Mol Med (Berl)20017914915611357939
- RalstonSHAnalysis of gene expression in human bone biopsies by polymerase chain reaction: evidence for enhanced cytokine expression in postmenopausal osteoporosisJ Bone Miner Res199498838908079663
- MurrayRMcGuiganFGrantSReidDRalstonSPolymorphisms of the interleukin-6 gene are associated with bone mineral densityBone19972189929213013
- TsukamotoKYoshidaHWatanabeSAssociation of radial bone mineral density with CA repeat polymorphism at the interleukin 6 locus in postmenoposal Japanese womenJ Hum Genet19994414815110319577
- FerrariSGarneroPEmondSMontgomeryHHumphriesSGreenspanSA functional polymorphic variant in the interleukin-6 gene promoter associated with low bone resorption in postmenopausal womenArthritis Rheum20014419620111212160
- GrayTMohanSLinkhartTBaylinkDEstradiol stimulates invitro the secretion of insulin-like growth factors by the clonal osteoblastic cell line, UMR106Biochem Biophys Res Commun19891584074122916989
- KurlandESRosenCJCosmanFInsulin-Like Growth Factor-I in Men with Idiopathic Osteoporosis 1J Clin Endocrinol Metab199782279928059284699
- KurlandESChanFKRosenCJBilezikianJPNormal growth hormone secretory reserve in men with idiopathic osteoporosis and reduced circulating levels of insulin-like growth factor-I 1J Clin Endocrinol Metab199883257625799661647
- BragaVMottesMMirandolaSAssociation of CTR and COLIA1 alleles with BMD values in peri- and postmenopausal womenCalcif Tissue Int20006736136611136533
- MasiLBecheriniLColliEPolymorphisms of the calcitonin receptor gene are associated with bone mineral density in postmenopausal Italian womenBiochem Biophys Res Commun19982481901959675109
- TabouletJFrenkianMFrendoJFeingoldNJullienneADe VernejoulMCalcitonin receptor olymorphism is associated with a decreased fracture risk in post-menopausal womenHum Mol Genet19987212921339817931
- KeenRWoodford-RichensKLanchburyJSpectorTAllelic variation at the interleukin-1 receptor antagonist gene is associated with early postmenopausal bone loss at the spineBone1998233673719763149
- LennardAGormanPCarrierMCloning and chromosome mapping of the human interleukin-1 receptor antagonist geneCytokine1992483891385987
- WongSYSLauEMCLiMChungTShamAWooJThe prevalence of Apo E4 genotype and its relationship to bone mineral density in Hong Kong ChineseJ Bone Miner Metab20052326126515838630
- LingXAiminLXiheZXiaoshuCCummingsSRVery low rates of hip fracture in Beijing, People’s Republic of China: the Beijing Osteoporosis ProjectAm J Epidemiol19961449019078890668
- FujiwaraNKMartiBGutzwillerFHip fracture mortality and morbidity in Switzerland and Japan: a cross-cultural comparisonSozialund Präventivmedizin199338814
- BuehringBViswanathanRBinkleyNBusseWGlucocorticoid-induced osteoporosis: an update on effects and managementJ Allergy Clin Immunol20131321019103024176682
- CanalisEMechanisms of glucocorticoid action in boneCurr Osteoporos Rep200539810216131429
- Ramsey-GoldmanRMissed opportunities in physician management of glucocorticoid-induced osteoporosis?Arthritis Rheum2002463115312012483714
- OhnakaKTanabeMKawateHNawataHTakayanagiRGlucocorticoid suppresses the canonical Wnt signal in cultured human osteoblastsBiochem Biophys Res Commun200532917718115721290
- CanalisECentrellaMBurchWMcCarthyTLInsulin-like growth factor I mediates selective anabolic effects of parathyroid hormone in bone culturesJ Clin Invest198983602910920
- LundgrenERastadJThurfjellEÅkerströmGLjunghallSPopulation-based screening for primary hyperparathyroidism with serum calcium and parathyroid hormone values in menopausal womenSurgery19971212872949092129
- WishartJHorowitzMNeedANordinBRelationship between forearm and vertebral mineral density in postmenopausal women with primary hyperparathyroidismArch Intern Med1990150132913312353865
- VestergaardPMollerupCLFrøkjærVGChristiansenPBlichert-ToftMMosekildeLCohort study of risk of fracture before and after surgery for primary hyperparathyroidismBMJ200032159860210977834
- SneddonWBMagyarCEWillickGELigand-selective dissociation of activation and internalization of the parathyroid hormone (PTH) receptor: conditional efficacy of PTH peptide fragmentsEndocrinology20041452815282315016722
- van AbelMHoenderopJGvan der KempAWFriedlaenderMMvan LeeuwenJPBindelsRJCoordinated control of renal Ca(2+) transport proteins by parathyroid hormone. TRPV5 & TRPV6Kidney Int20056841708172116164647
- BrenzaHLKimmel-JehanCJehanFParathyroid hormone activation of the 25-hydroxyvitamin D3-1α-hydroxylase gene promoterProc Natl Acad Sci U S A199895138713919465024
- JilkaRLMolecular and cellular mechanisms of the anabolic effect of intermittent PTHBone2007401434144617517365
- KrollMHParathyroid hormone temporal effects on bone formation and resorptionBull Math Biol20006216318810824426
- RazzaqueMSLanskeBThe emerging role of the fibroblast growth factor-23–klotho axis in renal regulation of phosphate homeostasisJ Endocrinol200719411017592015
- GravalleseEBone destruction in arthritisAnn Rheum Dis200261ii84ii612379632
- CooperCCouplandCMitchellMRheumatoid arthritis, corticosteroid therapy and hip fractureAnn Rheum Dis19955449527880122
- Van StaaTGeusensPBijlsmaJLeufkensHCooperCClinical assessment of the long-term risk of fracture in patients with rheumatoid arthritisArthritis Rheumatism2006543104311217009229
- NampeiAHashimotoJKoyanagiJCharacteristics of fracture and related factors in patients with rheumatoid arthritisMod Rheumatol20081817017618297237
- AraiKHanyuTSugitaniHRisk factors for vertebral fracture in menopausal or postmenopausal Japanese women with rheumatoid arthritis: a cross-sectional and longitudinal studyJ Bone Miner Metab20062411812416502118
- De NijsRJacobsJBijlsmaJPrevalence of vertebral deformities and symptomatic vertebral fractures in corticosteroid treated patients with rheumatoid arthritisRheumatology2001401375138311752508
- PeelNMooreDBarringtonNBaxDEastellRRisk of vertebral fracture and relationship to bone mineral density in steroid treated rheumatoid arthritisAnn Rheum Dis1995548018067492217
- GoldringSRGravalleseEMMechanisms of bone loss in inflammatory arthritis: diagnosis and therapeutic implicationsArthritis Res199923311094416
- ChuCQFieldMFeldmannMMainiRLocalization of tumor necrosis factor α in synovial tissues and at the cartilage–pannus junction in patients with rheumatoid arthritisArthritis Rheumatology19913411251132
- ChuCQFieldMAllardSAbneyEFeldmannMMainiRDetection of cytokines at the cartilage/pannus junction in patients with rheumatoid arthritis: implications for the role of cytokines in cartilage destruction and repairRheumatology199231653661
- DeleuranBChuCQFieldMLocalization of interleukin-1α, type 1 interleukin-1 receptor and interleukin-1 receptor antagonist in the synovial membrane and cartilage/pannus junction in rheumatoid arthritisRheumatology199231801809
- RomasEMartinTCytokines in the pathogenesis of osteoporosisOsteoporos Int199774753
- KotakeSUdagawaNTakahashiNIL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesisJ Clin Invest19991031345135210225978
- ChabaudMDurandJMBuchsNHuman interleukin-17Arthritis Rheum19994296397010323452
- FunkJLCordaroLAWeiHBenjaminJBYocumDESynovium as a source of increased amino-terminal parathyroid hormone-related protein expression in rheumatoid arthritis. A possible role for locally produced parathyroid hormone-related protein in the pathogenesis of rheumatoid arthritisJ Clin Invest19981011362
- McClungMRole of RANKL inhibition in osteoporosisArthritis Res Ther20079Suppl 1S3
- LacativaPGSFariasMLFDOsteoporosis and inflammationArq Bras Endocrinol Metabol201054212313220485900
- MundyGROsteoporosis and inflammationNut Rev20076512 Pt 2S147S151
- TeitelbaumSLOsteoclasts: what do they do and how do they do it?Am J Pathol2007170242743517255310
- RouxCOsteoporosis in inflammatory joint diseasesOsteoporos Int2011222421433
- DiarraDStolinaMPolzerKDickkopf-1 is a master regulator of joint remodelingNat Med200713215616317237793
- WeitzmannMNPacificiRThe role of T lymphocytes in bone metabolismImmunol Rev200520815416816313347
- van StaaTPLeufkensHGCooperCThe epidemiology of corticosteroid-induced osteoporosis: a meta-analysisOsteoporos Int2002131077778712378366
- SchwartzAVDiabetes mellitus: does it affect bone?Calcif Tissue Int200373651551914517715
- MokdadAHFordESBowmanBAPrevalence of obesity, diabetes, and obesity-related health risk factors, 2001JAMA20032891767912503980
- BoyleJPThompsonTJGreggEWBarkerLEWilliamsonDFProjection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalencePopul Health Metr201082920969750
- Al-HomoodIASheshahIMohammedAGAGasimGIThe prevalence and risk factors of osteoporosis among a Saudi female diabetic populationOpen Access Maced J Med Sci20175217718128507624
- RaskaIJrBroulikPThe impact of diabetes mellitus on skeletal health: an established phenomenon with inestablished causesPrague Med Rep20051062137148
- WongdeeKCharoenphandhuNOsteoporosis in diabetes mellitus: possible cellular and molecular mechanismsWorld J Diabetes201123414821537459
- InzerilloAMEpsteinSOsteoporosis and diabetes mellitusRev Endocr Metab Disord2004526126815211098
- Leidig-BrucknerGZieglerRDiabetes mellitus a risk for osteoporosis?Exp Clin Endocrinol Diabetes2001109S493S51411460594
- TuominenJTImpivaaraOPuukkaPRönnemaaTBone mineral density in patients with type 1 and type 2 diabetesDiabetes Care19992271196120010388989
- IsidroMLRuanoBBone disease in diabetesCurr Diabetes Rev20106314415520380629
- SchwartzAVSellmeyerDEEnsrudKEStudy of Osteoporotic Features Research GroupOlder women with diabetes have an increased risk of fracture: a prospective studyJ Clin Endocrinol Metab2001861323811231974
- NicodemusKKFolsomARIowa Women’s Health StudyType 1 and type 2 diabetes and incident hip fractures in postmenopausal womenDiabetes Care20012471192119711423501
- JanghorbaniMVan DamRMWillettWCHuFBSystematic Review of Type 1 and Type 2 Diabetes Mellitus and Risk of FractureOxfordOxford Univ Press2007
- FarmerMEWhiteLRBrodyJABaileyKRRace and sex differences in hip fracture incidenceAm J Public Health19847412137413806507690
- CummingsSRNevittMCBrownerWSRisk factors for hip fracture in white womenN Engl J Med1995332127677747862179
- KumedaYOsteoporosis in diabetesClin Calcium2008185589599 Japanese18445876
- YangJZhangXWangWLiuJInsulin stimulates osteoblast proliferation and differentiation through ERK and PI3K in MG-63 cellsCell Biochem Funct201028433434120517899
- GolubEEBoesze-BattagliaKThe role of alkaline phosphatase in mineralizationCurr Opin Orthop200718444448
- WangWZhangXZhengJYangJHigh glucose stimulates adipogenic and inhibits osteogenic differentiation in MG-63 cells through cAMP/protein kinase A/extracellular signal-regulated kinase pathwayMol Cell Biochem20103381–211512219949837
- BotolinSFaugereMCMallucheHOrthMMeyerRMcCabeLRIncreased bone adiposity and peroxisomal proliferator-activated receptor-γ2 expression in type I diabetic miceEndocrinology200514683622363115905321
- Lecka-CzernikBMoermanEJGrantDFLehmannJMManolagasSCJilkaRLDivergent effects of selective peroxisome proliferator-activated receptor-γ2 ligands on adipocyte versus osteoblast differentiationEndocrinology200214362376238412021203
- DiascroDDJrVogelRLJohnsonTEHigh fatty acid content in rabbit serum is responsible for the differentiation of osteoblasts into adipocyte-like cellsJ Bone Miner Res1998131961069443795
- ElefteriouFAhnJDTakedaSLeptin regulation of bone resorption by the sympathetic nervous system and CARTNature2005434703251452015724149
- ShiYYadavVKSudaNDissociation of the neuronal regulation of bone mass and energy metabolism by leptin in vivoProc Natl Acad Sci U S A200810551205292053319074282
- HieMIitsukaNOtsukaTTsukamotoIInsulin-dependent diabetes mellitus decreases osteoblastogenesis associated with the inhibition of Wnt signaling through increased expression of Sost and Dkk1 and inhibition of Akt activationInt J Mol Med201128345546221567076
- LinCLWangJYKoJYHuangYTKuoYHWangFSDick-kopf-1 promotes hyperglycemia–induced accumulation of mesangial matrix and renal dysfunctionJ Am Soc Nephrol201021112413520019166
- García-MartínARozas-MorenoPReyes-GarcíaRCirculating levels of sclerostin are increased in patients with type 2 diabetes mellitusJ Clin Endocrinol Metab201297123424122031520
- KaneRStevensonLGodsonCStittAO’BrienCGremlin gene expression in bovine retinal pericytes exposed to elevated glucoseBr J Ophthalmol200589121638164216299147
- AlyasinSMomenTKashefSAlipourAAminRThe relationship between serum 25 hydroxy vitamin d levels and asthma in childrenAllergy Asthma Immunol Res20113425125521966605
- ModestiABertolozziIGamberiTHyperglycemia activates JAK2 signaling pathway in human failing myocytes via angiotensin II-mediated oxidative stressDiabetes200554239440115677497
- KimHJKimSHYunJMFisetin inhibits hyperglycemia-induced proinflammatory cytokine production by epigenetic mechanismsEvid Based Complement Alternat Med2012201263946923320034
- GonzalezYHerreraMTSoldevilaGHigh glucose concentrations induce TNF-α production through the down-regulation of CD33 in primary human monocytesBMC Immunol2012131922500980
- BinkleyNVitamin D and osteoporosis-related fractureArch Biochem Biophys2012523111512222349359
- PalomerXGonzález-ClementeJBlanco-VacaFMauricioDRole of vitamin D in the pathogenesis of type 2 diabetes mellitusDiabetes Obes Metab200810318519718269634
- MenegazzoLAlbieroMAvogaroAFadiniGPEndothelial progenitor cells in diabetes mellitusBiofactors201238319420222488933
- HamannCKirschnerSGüntherKPHofbauerLCBone, sweet bone-osteoporotic fractures in diabetes mellitusNat Rev Endocrinol20128529730522249517
- SugimotoKYasujimaMYagihashiSRole of advanced glycation end products in diabetic neuropathyCurr Pharm Des2008141095396118473845
- JackMWrightDRole of advanced glycation endproducts and glyoxalase I in diabetic peripheral sensory neuropathyTransl Res2012159535536522500508
- CatalanoAMorabitoNDi ViesteGPhalangeal quantitative ultrasound and metabolic control in pre-menopausal women with type 1 diabetes mellitusJ Endocrinol Invest201336534735123027769
- NeumannTLodesSKastnerBTrabecular bone score in type 1 diabetes-a cross-sectional studyOsteoporos Int201627112713326187124
- WalshJSVilacaTObesity, type 2 diabetes and bone in adultsCalcif Tissue Int2017100552853528280846
- MoayeriAMohamadpourMMousaviSFShirzadpourEMohamadpourSAmraeiMFracture risk in patients with type 2 diabetes mellitus and possible risk factors: a systematic review and meta-analysisTher Clin Risk Manag20171345546828442913
- Tysiewicz-DudekMPietraszkiewiczFDrozdzowskaBAlzheimer’s disease and osteoporosis: common risk factors or one condition predisposing to the other?Ortop Traumatol Rehabil2007104315323 Polish
- WellerISchatzkerJHip fractures and Alzheimer’s disease in elderly institutionalized CanadiansAnn Epidemiol200414531932415177270
- BakerNLCookMNArrighiHMBullockRHip fracture risk and subsequent mortality among Alzheimer’s disease patients in the United Kingdom, 1988–2007Age Ageing2011401495421087990
- HaasumYFastbomJFratiglioniLJohnellKUndertreatment of osteoporosis in persons with dementia? A population-based studyOsteoporos Int20122331061106821499775
- ButterfieldDAAmyloid β-peptide (1-42)-induced oxidative stress and neurotoxicity: implications for neurodegeneration in Alzheimer’s disease brain. A reviewFree Radic Res200236121307131312607822
- BehlCDavisJLesleyRSchubertDHydrogen peroxide mediates amyloid β protein toxicityCell19947768178278004671
- JulesJZhangPAshleyJWMolecular basis of requirement of receptor activator of nuclear factor κB signaling for interleukin 1-mediated osteoclastogenesisJ Biol Chem201228719157281573822416138
- BiverEHardouinPCaverzasioJThe “bone morphogenic proteins” pathways in bone and joint diseases: translational perspectives from physiopathology to therapeutic targetsCytokine Growth Factor Rev2013241698122749766
- KimMSYangYMSonARANKL-mediated reactive oxygen species pathway that induces long lasting Ca2+ oscillations essential for osteoclastogenesisJ Biol Chem2010285106913692120048168
- ParkHSLeeSHParkDSequential activation of phosphati-dylinositol 3-kinase, βPix, Rac1, and Nox1 in growth factor-induced production of H2O2Mol Cell Biol200424104384439415121857
- BodmerJLSchneiderPTschoppJThe molecular architecture of the TNF superfamilyTrends Biochem Sci2002271192611796220
- LuckhausCMahabadiBGrass-KapankeBBlood biomarkers of osteoporosis in mild cognitive impairment and Alzheimer’s diseaseJ Neural Transm (Vienna)2009116790591119468818
- ColemanREClinical features of metastatic bone disease and risk of skeletal morbidityClin Cancer Res20061220 Pt 26243s6249s17062708
- MundyGRMetastasis to bone: causes, consequences and therapeutic opportunitiesNat Rev Cancer20022858459312154351
- ZhangJDaiJQiYOsteoprotegerin inhibits prostate cancer-induced osteoclastogenesis and prevents prostate tumor growth in the boneJ Clin Invest2001107101235124411375413
- BoydeAMaconnachieEReidSADellingGMundyGScanning electron microscopy in bone pathology: review of methods, potential and applicationsScan Electron Microsc1986Pt 4153715543544196
- RizzoliRBodyJJBrandiMLInternational Osteoporosis Foundation Committee of Scientific Advisors Working Group on Cancer-Induced Bone DiseaseCancer-associated bone diseaseOsteoporos Int201324122929295324146095
- LauYKLeeEPriorHJLixLMMetgeCJLeslieWDFracture risk in androgen deprivation therapy: a Canadian population based analysisCan J Urol20091664908491420003666
- BondySJIscoeNARothwellDMTrends in hormonal management of prostate cancer: a population-based study in OntarioMed Care200139438439611329525
- Falahati-NiniARiggsBLAtkinsonEJO’FallonWMEastellRKhoslaSRelative contributions of testosterone and estrogen in regulating bone resorption and formation in normal elderly menJ Clin Invest2000106121553156011120762
- DickmanPWAdolfssonJÅstrÖmKSteineckGHip fractures in men with prostate cancer treated with orchiectomyJ Urol20041726 Pt 12208221215538233
- HandforthCD’OronzoSColemanRBrownJCancer treatment and bone healthCalcified Tissue International2018114
- ReidIRIbbertsonHKCalcium supplements in the prevention of steroid-induced osteoporosisAm J Clin Nutr19864422872903728366
- LaneNEKelmanAA review of anabolic therapies for osteoporosisArthritis Res Ther20035521422212932280
- MosekildeLPrimary hyperparathyroidism and the skeletonClin Endocrinol (Oxf)200869111918167138
- CremersSCPillaiGPapapoulosSEPharmacokinetics/pharmaco-dynamics of bisphosphonates: use for optimisation of intermittent therapy for osteoporosisClin Pharmacokinet200544655157015932344
- KennelKADrakeMTAdverse effects of bisphosphonates: implications for osteoporosis managementMayo Clin Proc200984763263819567717
- CauleyJASeeleyDGEnsrudKEttingerBBlackDCummingsSREstrogen replacement therapy and fractures in older women. Study of Osteoporotic Fractures Research GroupAnn Intern Med199512219167985914
- BerningBKuijkCVKuiperJWBenninkHJKicovicPMFauserBCEffects of two doses of tibolone on trabecular and cortical bone loss in early postmenopausal women: a two-year randomized, placebo-controlled studyBone19961943953998894146
- DelmasPDEnsrudKEAdachiJDMulitple Outcomes of Raloxifene Evaluation InvestigatorsEfficacy of raloxifene on vertebral fracture risk reduction in postmenopausal women with osteoporosis: four-year results from a randomized clinical trialJ Clin Endocrinol Metab20028783609361712161484
- KharodeYBodinePVMillerCPLyttleCRKommBSThe pairing of a selective estrogen receptor modulator, bazedoxifene, with conjugated estrogens as a new paradigm for the treatment of menopausal symptoms and osteoporosis preventionEndocrinology2008149126084609118703623
- BoneHGMcClungMRRouxCOdanacatib, a cathepsin-K inhibitor for osteoporosis: a two-year study in postmenopausal women with low bone densityJ Bone Miner Res201025593794719874198
- BabatundeOTMarquezSTaylorAOsteoporosis knowledge and health beliefs among men in midlife yearsJ Nutr Educ Behav2017499759.e1763.e128655501
- HardingATBeckBRExercise, osteoporosis, and bone geometrySports2017529
- ZhuKPrinceRLLifestyle and osteoporosisCurr Osteoporos Rep2015131525925416958
- YangPChenCChiouHYLiYLHsuGSWThe exercise intervention may influence the dietary intake and reduce the risk of osteoporosis and sarcopenia in menopausal womenFASEB J201731967969
- ManolagasSCBirth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis 1Endocr Rev200021211513710782361
- Dawson-HughesBGoldDRodbardHPhysician’s Guide to Prevention and Treatment of OsteoporosisWashington, DC, USANational Osteoporosis Foundation2003
- KanisJAOdenAJohanssonHBorgströmFStrömOMcCloskeyEFRAX® and its applications to clinical practiceBone200944573474319195497
- VuoriIMDose-response of physical activity and low back pain, osteoarthritis, and osteoporosisMed Sci Sports Exerc2001336 SupplS551S58611427782
- DrinkwaterBLDoes physical activity play a role in preventing osteoporosis?Res Q Exerc Sport1994651972067973068
- AldahrMHSBone mineral status response to aerobic versus resistance exercise training in postmenopausal womenWorld Appl Sci J2012166806813
- ShackelfordLCLeBlancADDriscollTBResistance exercise as a countermeasure to disuse-induced bone lossJ Appl Physiol (1985)200497111912915220316
- HernandezCJBeaupreGSCarterDRA theoretical analysis of the relative influences of peak BMD, age-related bone loss and menopause on the development of osteoporosisOsteoporos Int2003141084384712904837
- BonjourJPChevalleyTRizzoliRFerrariSGene-environment interactions in the skeletal response to nutrition and exercise during growth. Optimizing Bone Mass and Strength. Karger PublishersMed Sport Sci200751648017505120
- WattsNBLewieckiEMMillerPDBaimSNational osteoporosis foundation 2008 clinician’s guide to prevention and treatment of osteoporosis and the world health organization Fracture Risk Assessment Tool (FRAX): what they mean to the bone densitometrist and bone technologistJ Clin Densitom200811447347718562228
- CouncilNrDRI (Dietary Reference Intakes) for Calcium, Phosphorus, Magnesium, Vitamin D, and FluorideWashington, DC, USANational Academy Press1997
- Dawson-HughesBHarrisSSKrallEADallalGEEffect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or olderN Engl J Med1997337106706769278463
- KendlerDLMarinFZerbiniCAEffects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trialThe Lancet201839110117230240
- KanisJAOdénAMcCloskeyEVJohanssonHWahlDACooperCA systematic review of hip fracture incidence and probability of fracture worldwideOsteoporosis International20122392239225622419370
- EvattMLDeLongMRKhazaiNRosenATricheSTangprichaVPrevalence of vitamin D insufficiency in patients with Parkinson disease and Alzheimer diseaseArchives of Neurology200865101348135218852350
- DurrinLKHaileRWInglesSACoetzeeGAVitamin D receptor 3′-untranslated region polymorphisms: lack of effect on mRNA stabilityBiochimica et Biophysica Acta (BBA)-Molecular Basis of Disease19991453331132010101249
- RemesTVäisänenSBMahonenABone mineral density, body height, and vitamin D receptor gene polymorphism in middle-aged menAnnals of Medicine200537538339216179274
- LambrinoudakiIKaparosGArmeniEBsmI vitamin D receptor’s polymorphism and bone mineral density in men and premeno-pausal women on long-term antiepileptic therapyEuropean Journal of Neurology2011181939820500803
- WangLMaJMansonJEBuringJEGazianoJMSessoHDA prospective study of plasma vitamin D metabolites, vitamin D receptor gene polymorphisms, and risk of hypertension in menEuropean Journal of Nutrition20135271771177923262750
- IoannidisJPRalstonSHBennettSTDifferential genetic effects of ESR1 gene polymorphisms on osteoporosis outcomesJAMA2004292172105211415523071
- YamadaYAndoFNiinoNOhtaSShimokataHAssociation of polymorphisms of the estrogen receptor α gene with bone mineral density of the femoral neck in elderly Japanese womenJournal of Molecular Medicine200280745246012110951
- TangLChengG-LXuZ-HAssociation between estrogen receptor α gene (ESR1) PvuII (C/T) and XbaI (A/G) polymorphisms and hip fracture risk: evidence from a meta-analysisPloS One2013812e8280624482673
- OgawaSFujitaMIshiiYImpaired estrogen sensitivity in bone by inhibiting both estrogen receptor α and β pathwaysJournal of Biological Chemistry200027528213722137910806217
- LauHHoALukKKungAEstrogen receptor β gene polymorphisms are associated with higher bone mineral density in premeno-pausal, but not postmenopausal southern Chinese womenBone200231227628112151079
- ScarianoJSimplicioSMontoyaGGarryPBaumgartnerREstrogen receptor β dinucleotide (CA) repeat polymorphism is significantly associated with bone mineral density in postmenopausal womenCalcified Tissue International200474650150815354857
- KungAWLaiBMNgMYChanVShamPCT-1213C polymorphism of estrogen receptor beta is associated with low bone mineral density and osteoporotic fracturesBone20063951097110616777502
- MiyaoMHosoiTEmiMAssociation of bone mineral density with a dinucleotide repeat polymorphism at the calcitonin (CT) locusJournal of Human Genetics200045634635011185743
- MaganaJGomezRCisnerosBAssociation of the CT gene (CA) polymorphism with BMD in osteoporotic Mexican womenClinical Genetics200670540240817026622
- TuralSKaraNAlayliGTomakLAssociation between osteoporosis and polymorphisms of the bone Gla protein, estrogen receptor 1, collagen 1-A1 and calcitonin receptor genes in Turkish postmenopausal womenGene2013515116717223137636
- HosoiTMiyaoMInoueSAssociation study of parathyroid hormone gene polymorphism and bone mineral density in Japanese postmenopausal womenCalcified Tissue International199964320520810024376
- MinagawaMYasudaTWatanabeTAssociation between AAAG repeat polymorphism in the P3 promoter of the human parathyroid hormone (PTH)/PTH-related peptide receptor gene and adult height, urinary pyridinoline excretion, and promoter activityThe Journal of Clinical Endocrinology & Metabolism20028741791179611932319
- NapoliNRastelliAMaCGenetic polymorphism at Val80 (rs700518) of the CYP19A1 gene is associated with aromatase inhibitor associated bone loss in women with ER (+) breast cancerBone201355230931423643682
- ZmudaJMCauleyJAKullerLHFerrellREA common promoter variant in the cytochrome P450c17α (CYP17) gene is associated with bioavailable testosterone levels and bone size in menJournal of Bone and Mineral Research200116591191711341336
- SharpLCardyAHCottonSCLittleJCYP17 gene polymorphisms: prevalence and associations with hormone levels and related factors. a HuGE reviewAmerican Journal of Epidemiology2004160872974015466495
- HuizengaNAde LangePKoperJWHuman adrenocorticotro-pin-secreting pituitary adenomas show frequent loss of heterozygosity at the glucocorticoid receptor gene locusThe Journal of Clinical Endocrinology & Metabolism19988339179219506748
- TsukamotoKOrimoHHosoiTAssociation of bone mineral density with polymorphism of the human calcium-sensing receptor locusCalcified Tissue International200066318118310666491
- LangdahlBLStenkjaerLCarstensMToftengCEriksenEA CAG repeat polymorphism in the androgen receptor gene is associated with reduced bone mass and increased risk of osteoporotic fracturesCalcified Tissue International200373323724314667136
- LangdahlBLCarstensMStenkjærLEriksenEFPolymorphisms in the transforming growth factor beta 1 gene and osteoporosisBone200332329731012667558
- RivadeneiraFHouwing-DuistermaatJJVaessenNAssociation between an insulin-like growth factor I gene promoter polymorphism and bone mineral density in the elderly: the Rotter-dam StudyThe Journal of Clinical Endocrinology & Metabolism20038883878388412915683
- ArkoBPreželjJKocijančičAKomelRMarcJAssociation of the osteoprotegerin gene polymorphisms with bone mineral density in postmenopausal womenMaturitas200551327027915978970
- Garcia-UnzuetaMRianchoJZarrabeitiaMAssociation of the 163A/G and 1181G/C osteoprotegerin polymorphism with bone mineral densityHormone and Metabolic Research2008400321922418348083
- JuradoSNoguésXAguedaLPolymorphisms and haplo-types across the osteoprotegerin gene associated with bone mineral density and osteoporotic fracturesOsteoporosis International2010;21228729619436932
- MencejSAlbaghaOMPreželjJKocjanTMarcJTumour necrosis factor superfamily member 11 gene promoter polymorphisms modulate promoter activity and influence bone mineral density in postmenopausal women with osteoporosisJournal of Molecular Endocrinology200840627327918502820
- HoshinoSHosoiTShirakiMOrimoHOuchiYInoueSAssociation of tumor necrosis factor receptor 1 gene polymorphism with bone mineral densityGeriatrics & Gerontology International200332101105
- GrantSFReidDMBlakeGHerdRFogelmanIRalstonSHReduced bone density and osteoporosis associated with a polymorphic Sp1 binding site in the collagen type I α 1 geneNature Genetics19961422038841196
- LauEChoyDLiMWooJChungTShamAThe relationship between COLI A1 polymorphisms (Sp 1) and COLI A2 polymorphisms (Eco R1 and Puv II) with bone mineral density in Chinese men and womenCalcified Tissue International200475213313715085313
- ChenHYTsaiHDChenWCWuJYTsaiFJTsaiCHRelation of polymorphism in the promotor region for the human osteocalcin gene to bone mineral density and occurrence of osteoporosis in postmenopausal Chinese women in TaiwanJournal of Clinical Laboratory Analysis200115525125511574953
- McGuiganFKumarJIvaskaKKObrantKJGerdhemPÅkessonKOsteocalcin gene polymorphisms influence concentration of serum osteocalcin and enhance fracture identificationJournal of Bone and Mineral Research20102561392139920200947
- ZebboudjAFImuraMBoströmKMatrix GLA protein, a regulatory protein for bone morphogenetic protein-2Journal of Biological Chemistry200227764388439411741887
- EichnerJEFriedrichCACauleyJAAlpha 2-HS glycoprotein phenotypes and quantitative hormone and bone measures in postmenopausal womenCalcified Tissue International19904763453491705475
- JohnstonJMCauleyJAGanguliMAPOE 4 and hip fracture risk in a community-based study of older adultsJournal of the American Geriatrics Society199947111342134510573444
- CauleyJAZmudaJMYaffeKApolipoprotein E polymorphism: A new genetic marker of hip fracture risk–The Study of Osteoporotic FracturesJ Bone Miner Res19991471175118110404018
- VilladsenMMBüngerMHCarstensMStenkjærLLangdahlBLMethylenetetrahydrofolate reductase (MTHFR) C677T polymorphism is associated with osteoporotic vertebral fractures, but is a weak predictor of BMDOsteoporosis International200516441141615300362
- UranoTInoueSGenetics of osteoporosisBiochemical and Biophysical Research Communications2014452228729325139232
- DouroudisKTarassiKAthanassiadesTHLA alleles as predisposal factors for postmenopausal osteoporosis in a Greek populationTissue Antigens200769659259617498269
- AltshulerDHirschhornJNKlannemarkMThe common PPARγ Pro12Ala polymorphism is associated with decreased risk of type 2 diabetesNature Genetics20002617610973253
- AlbaghaOMcGuiganFReidDRalstonSNovel polymorphism in the human Fos related antigen-1gene is associated with bone mineral density in women from the UKPaper presented at: Journal of Bone and Mineral Research2002
- VaughanTPascoJAKotowiczMANicholsonGCMorrisonNAAlleles of RUNX2/CBFA1 gene are associated with differences in bone mineral density and risk of fractureJournal of Bone and Mineral Research20021781527153412162506
- DoeckeJDDayCJStephensASAssociation of functionally different RUNX2 P2 promoter alleles with BMDJournal of Bone and Mineral Research200621226527316418782
- KawanoKIOgataNChianoMKlotho gene polymorphisms associated with bone density of aged postmenopausal womenJournal of Bone and Mineral Research200217101744175112369777
- OgataNShirakiMHosoiTKoshizukaYNakamuraKKawaguchiHA polymorphic variant at the Werner helicase (WRN) gene is associated with bone density, but not spondylosis, in postmenopausal womenJournal of Bone and Mineral Metabolism200119529630111498731
- BabijPZhaoWSmallCHigh bone mass in mice expressing a mutant LRP5 geneJournal of Bone and Mineral Research200318696097412817748
- AiMHolmenSLVan HulWWilliamsBOWarmanMLReduced affinity to and inhibition by DKK1 form a common mechanism by which high bone mass-associated missense mutations in LRP5 affect canonical Wnt signalingMolecular and Cellular Biology200525124946495515923613
- GiraudeauFSMcginnisREGrayICCharacterization of common genetic variants in cathepsin K and testing for association with bone mineral density in a large cohort of perimenopausal women from ScotlandJournal of Bone and Mineral Research2004191314114753734
- BabuLRWilsonSDickIIslamFDevineAPrinceRBone mass effects of a BMP4 gene polymorphism in postmenopausal womenBone200536355556115777683
- PetterssonUAlbaghaOMMiroloMPolymorphisms of the CLCN7 gene are associated with BMD in womenJournal of Bone and Mineral Research200520111960196716234969
- KornakUOstertagABrangerSBenichouOde VernejoulM-CPolymorphisms in the CLCN7 gene modulate bone density in postmenopausal women and in patients with autosomal dominant osteopetrosis type IIThe Journal of Clinical Endocrinology & Metabolism2006913995100016368748
- LeeS-HRhoJJeongDv-ATPase V 0 subunit d2–deficient mice exhibit impaired osteoclast fusion and increased bone formationNature Medicine200612121403
- MariniFFalchettiASilvestriSModulatory effect of farnesyl pyrophosphate synthase (FDPS) rs2297480 polymorphism on the response to long-term amino-bisphosphonate treatment in postmenopausal osteoporosisCurrent Medical Research and Opinion20082492609261518687167
- GartlandASkarrattKKHockingLJPolymorphisms in the P2X7 receptor gene are associated with low lumbar spine bone mineral density and accelerated bone loss in post-menopausal womenEuropean Journal of Human Genetics201220555922234152
