Abstract
Blood pressure (BP) control is a critical part of managing patients with type 2 diabetes. Perhaps it is the single most important aspect of diabetes care, which unlike hyperglycemia and dyslipidemia can reduce both micro- and macrovascular complications. Hypertension is more prevalent in individuals with diabetes than general population, and in most cases its treatment requires two or more pharmacological agents (about 30% of individuals with diabetes need 3 or more medications to control BP). In this article we describe the key evidence that has contributed to our understanding that reduced BP translates into positive micro- and macrovascular outcomes. We review the data supporting current recommendation for BP target < 130/80 mmHg. Two studies suggest that a lower BP goal could be even more beneficial. We also present the comparative benefits of various antihypertensive drugs in reducing diabetes-related micro- and macrovascular complications. Finally we propose an evidence-based algorithm of how to initiate and titrate antihypertensive pharmacotherapy in affected individuals. Overall, achieving BP < 130/80 mmHg is more important than searching for the “best” antihypertensive agent in patients with diabetes.
Introduction
Diabetes is very prevalent and places high financial burden to our society. In the United States during 2009 to 2034 the number of persons with diabetes is anticipated to increase from 23.7 million to 44.1 million. The relative annual cost is also expected to rise from $113 billion to $336 billion during the same period.Citation1 Worldwide, 366 million individuals are projected to have diabetes by year 2030.Citation2 Type 2 diabetes, the predominant form, comprises 90% to 95% of all cases.
Macrovascular disorders are common in affected individuals. Specifically, cardiovascular disease (CVD) is 2 to 5 times more prevalent in persons with diabetes than general population.Citation3–Citation5 Importantly it is the most serious complication by contributing 70% to all-cause mortality in affected patients.Citation6 In the United States, diabetes is also the leading cause of microvascular disorders of end stage renal disease (ESRD)Citation7,Citation8 and retinopathy.Citation9
Hypertension is 1.5 to 2.0 times more common in patients with diabetes than without diabetes,Citation10 and more so in females than males.Citation11 For example, about 40% of individuals between ages 25 to 65 already have high blood pressure (BP) at the time of diagnosis of diabetes.Citation11 This figure increases further with age.Citation4,Citation11 Coexistence of hypertension with diabetes is likely due to the confounding effect of metabolic syndrome that often predates both conditions.
Hypertension is not only common but also a major cause of cardiovascular (CV) pathologyCitation11–Citation14 and thus mortality in individuals with diabetes. It is also a direct contributor to microvascular complications of nephropathyCitation7,Citation15,Citation16 and retinopathy.Citation16–Citation18 As described in the main text, many randomized clinical trials have documented that good BP control reduces both micro- and macrovascular complications. This could make hypertension the single most important determinant of diabetes-related morbidity and mortality compared to hyperglycemia that mainly causes microvascular disease and dyslipidemia that mostly contributes to macrovascular complications.
For this review article, we searched the literature for clinical studies related to treatment of hypertension in type 2 diabetes. We utilized PubMed to find trials published in 2005 to 2010. We then used citations from identified articles to select landmark studies printed before 2005. For this paper we chose mainly randomized clinical trials with large sample size and long duration of follow up. We narrowed further our selection to original works that emphasized renal and CV outcomes of various antihypertensive therapies in subjects with type 2 diabetes.
The purpose of this article is 5-fold. First, to provide evidence that reducing BP is beneficial in patients with diabetes; second, to demonstrate that optimal BP target is <130/80 mmHg; third, to show that hypertension is poorly controlled in clinical practice worldwide; fourth, to explain the rationale of choosing the right antihypertensive medications; and fifth, to provide a descriptive algorithm of how to initiate and titrate pharmacotherapy.
Reducing BP is beneficial
Critical evidence from 2 major trials, UKPDSCitation18,Citation19 and SHEP,Citation20 shows that reduced BP prevents complications in patients with type 2 diabetes.
UKPDS 38Citation18 was a landmark study that examined if decreased BP in persons with new type 2 diabetes lowered micro- and macrovascular complications. At study entry, 1148 subjects with less than 3 years of diabetes and mean BP 164/94 mmHg were randomized into “tight” BP and “less-tight” BP control groups. Patients in the tight BP control group received either angiotensin converting enzyme inhibitor (ACEi) captopril or β-blocker atenolol to bring BP to <150/85 mmHg. The less-tight BP control group could use medications other than ACEi or β-blocker to attain BP <180/105 mmHg.
After 8.4 years of follow up, the tight BP control group achieved a lower BP than the less-tight BP control arm (Δ10/Δ5 mmHg), resulting in greater relative reductions (P < 0.05) for both micro and macrovascular complications: 24% in any diabetes related end-points, 32% in diabetes-related deaths, 44% in strokes, 56% in heart failure (HF) and 34% in retinopathy. No difference in outcomes was seen in patients treated with either captopril or atenolol. Of note, about 30% of patients in the tight BP control group required 3 or more antihypertensive medications to achieve the desired BP.
UKPDS 39Citation19 was a 10-year observational study on the same group of patients who participated in the original UKPDS 38Citation18 trial. It examined if reduced vascular complications obtained in the UKPDS 38 were maintained 10 years after the end of randomization. Subjects (N = 884) underwent post-trial monitoring by clinic visits for the first 5 years and then by questionnaires for the next 5 years. The following 2 results were observed. The BP difference between groups, obtained during the original study, was lost within 2 years of the observational phase. More importantly, the significant relative reductions achieved in the tight BP control arm during UKPDS 38Citation18 were not sustained 10 years later. It is prudent to conclude that UKPDS 39Citation19 shows the significance of not only decreasing BP in patients with diabetes but also maintaining it indefinitely in order to keep a low incidence of micro- and macrovascular complications.
SHEPCitation20 examined if a low dose thiazide diuretic prevented major CV events in older patients with isolated systolic hypertension. At study entry, 12% of 4736 subjects had diabetes with mean systolic BP > 160 mmHg and diastolic BP <90 mmHg. Participants were randomized into 2 groups: chlorthalidone 12.5 to 25 mg/day or placebo. Primary outcome was the occurrence of fatal and nonfatal strokes, fatal and nonfatal myocardial infarction (MI), major CV events, or all-cause mortality.
After 5 years of follow up, the chlorthalidone group achieved a lower BP than the placebo arm (Δ9.8/Δ2.2 mmHg), resulting in greater relative reductions (P < 0.05): 34% in major CV events, 54% in fatal and nonfatal MIs and 56% in major coronary heart disease (CHD) events. Patients with diabetes experienced an absolute benefit twice greater than nondiabetic individuals. This most likely reflected the fact that baseline CV risk was higher in persons with diabetes.
In summary, UKPDS 38,Citation18 UKPDS 39,Citation19 SHEPCitation20 and other studies like HDFP,Citation12 Syst-Euro,Citation21 HOT,Citation22 normotensive ABCDCitation16 and HOPECitation23 provide firm evidence that even small BP reductions translate to significant decrease in both micro and macrovascular complications in persons with type 2 diabetes. These findings have major consequences given that hypertension contributes directly to CV pathology, which in turn is the most common cause of mortality in diabetic individuals.Citation6 Therefore it is imperative that providers screen and treat hypertension aggressively in patients with diabetes.
Evidence for BP less than 130/80 mmHg
Clear evidence supports the current recommendation that target BP must be <130/80 mmHg in patients with diabetes.Citation24–Citation28 This comes primarily from results of HOTCitation22 and Normotensive ABCDCitation16 clinical trials.
The HOT study examined the lowest diastolic BP that could have the greatest impact in reducing CV events in patients with hypertension. At study entry, 8% of 18790 participants with mean BP 170/105 mmHg had diabetes. Subjects were randomized into 3 different treatment intensities so that final diastolic BP in each group was ≤80, ≤85 or ≤90 mmHg. Treatment was intensified based on BP response. Primary outcome was the occurrence of fatal or nonfatal MI, fatal or nonfatal strokes, or deaths from any CV cause.
After 3.8 years of follow up, the 3 groups achieved the following diastolic BPs: 81.1, 83.2 and 85.2 mmHg. Importantly, among 1501 patients with diabetes, the composite primary outcomes occurred remarkably 51% less (P =0.005) in the arm with target diastolic BP ≤ 80 mmHg than in the one with target ≤90 mmHg. The HOTCitation22 trial clearly demonstrates the need to achieve a diastolic BP ≤ 80 mmHg in patients with diabetes.
The normotensive ABCDCitation16 trial examined if further reduction of normal BP could prevent more vascular complications in patients with diabetes. At the time, BP < 140/90 mmHg was considered normal. At study entry, 480 participants with type 2 diabetes and mean BP 136/84 mmHg were randomized into ACEi enalapril, calcium channel blocker (CCB) nisoldipine, or placebo arm. The goal was to lower the diastolic BP from baseline by 10 mmHg in the treatment groups and maintain it at 80 to 89 mmHg in the placebo arm.
After 5.3 years of follow up, the enalapril and nisoldipine groups achieved a BP 128/75 mmHg and placebo arm a BP 137/81 mmHg. The lower BP treatment groups experienced significantly less strokes (P = 0.03), retinopathy (P =0.019) and progression of normoalbuminuria (P =0.012) or microalbuminuria (P =0.028) than the placebo arm. Similar benefits were seen between patients receiving either enalapril or nisoldipine.
In conclusion, results from both HOTCitation22 and normotensive ABCDCitation16 trials have clearly established that BP < 130/80 mmHg is an appropriate target for treatment of hypertension in patients with diabetes.
Could a lower BP target be more optimal?
Some evidence implies that even a lower BP goal than 130/80 mmHg could be beneficial in decreasing micro and macrovascular complications of type 2 diabetes. Data from prospective observational UKPDS 36Citation29 study and randomized interventional ABCD-2Citation30 trial are suggestive of this possibility.
UKPDS 36 examined the relationship between systolic BP and rate of vascular complications in 3642 individuals with new diabetes and mean systolic BP 135 mmHg. Primary outcome was the occurrence of any diabetes-related complications or all-cause mortality. After 10.5 years of follow up, a linear relationship was observed between systolic BP and complications from diabetes. Every 10 mmHg decrease in systolic BP was associated with significant reductions in final outcomes by: 12% in diabetes related complications, 15% in diabetes-related deaths, 11% in MIs and 13% in microvascular complications. Remarkably, there was no minimal systolic BP threshold at which complication rates stabilized or worsened. The lowest risk was seen in subjects with systolic BP < 120 mmHg.
The randomized ABCD-2Citation30 trial examined if angiotensin receptor blocker (ARB) valsartan could prevent progression of normo or microalbuminuria in patients with type 2 diabetes, who had normal BP and kidney function. At enrollment, 129 subjects with mean BP 126/84 mmHg were randomized to receive either valsartan 80 mg/day or placebo. After 1.9 years of follow up, the valsartan arm achieved a BP 118/75 mmHg and placebo group a BP 124/80 mmHg (P < 0.001). The primary outcome, which was the progression of albuminuria, occurred significantly less in the tight BP arm than in the placebo group (P = 0.007), implying that the relative decrease in albuminuria was a direct consequence of reduced BP.
However, no differences in glomerular filtration rate (GFR) or retinopathy were detected between groups, which could be explained by the short duration of the trial. The study outcome is important given the well known association of microalbuminuria with the risk of renal insufficiencyCitation31 and CVD.Citation32,Citation33 For example, HOPE trial showed clearly that every 0.4 mg/mmol rise in urine albumin/creatinine ratio contributed to 5.9% increase in risk of CV events.Citation32
In conclusion, both UKPDS 36 and ABCD-2 studies suggest a possible benefit in reducing BP further to a target < 120/75 mmHg in patients with diabetes. However longer randomized clinical trials using various antihypertensive drugs are needed to test this hypothesis rigorously. Such trials must also include high risk subjects with multiple comorbidities.
Blood pressure is uncontrolled in clinical practice
Although BP control is the most important variable in preventing micro and macrovascular complications, observational studies consistently show that BP target is not achieved in most patients with type 2 diabetes. It is estimated that only 2.7% to 30% of individuals reach BP goal < 130/80 mmHg.Citation34–Citation40 For example, a large analysis of 49,420 individuals with diabetes and hypertension, from 24 original studies conducted in different countries between 1990 and 2004, found that although 87% of patients were receiving antihypertensive therapy, only 12% had achieved BP target < 130/85 mmHg.Citation38
The 2005 to 2006 National Health and Nutrition Examination Survey (NHANES) documented 29.3% control rate of BP among 481 individuals with diabetes.Citation36 A recent observational study from the Swedish National Diabetes Register conducted in 4570 patients with type 2 diabetes and CHD found that although 94% of subjects were taking antihypertensive medications, only 23% had achieved BP < 130/80 mmHg. Surprisingly, it was observed that among the three major risk factors for diabetes-related complications, BP target was attained in fewer subjects than were glycemic and cholesterol goals: hemoglobin A1c < 7% and low density lipoprotein < 100 mg/dL were reached in 52% and 63% of individuals respectively.Citation35 The 2005–2006 NHANES and observational study by McFarlane et al also found that BP was the least frequently controlled variable of all three major risk factors.Citation36,Citation37
Two important factors contribute to poor BP control in patients with diabetes: adherence to therapy and clinical inertia. Adherence is most commonly measured by the medication possession ratio (MPR), which was defined originally in 2000 by Bertholet.Citation41 Adherence to antihypertensive treatment was evaluated recently by a systematic review of 53 original studies published in 2000 to 2005. Results showed that 12-month MPR was only 67%, indicating that patients were not on therapy 33% of the time over a 1-year period.Citation42 Although the review was performed in hypertensive individuals, adherence is expected to be even lower in patients with diabetes, given their tighter BP goal and need for more medication use.Citation18,Citation36,Citation43
Adherence to treatment is challenging in all clinical populations. Although many barriers to therapy exist, style of clinician counseling can be fundamental in ensuring adherence. Behavior change techniques like motivational intervention are promising in engaging patients to face ambivalence to treatment, identify barriers to therapy, and discus treatment decisions.Citation44,Citation45 Future research is required to adapt these techniques into routine clinical practice for optimal results.Citation44,Citation46
Clinical inertia quantifies the failure of providers to escalate treatment in the face of the obvious need to do so.Citation47 The prospective study ABATe evaluated clinical inertia for treatment of hypertension in 1169 patients with diabetes from 9 Veteran Administration facilities during 2005 to 2006.Citation48 Although average systolic BP was >140/90 mmHg on 2 consecutive years – at the time of clinic visit, 51% of individuals did not receive intensified therapy. Treatment change was even less likely to occur if BP was between 130/80 and 140/90 mmHg. In a large cross-sectional study of 35,424 subjects with elevated BP, conducted in 2003 to 2004, clinical inertia for management of hypertension was 37%. Coexistence of diabetes in these individuals was associated with significantly higher rates of clinical inertia.Citation49
Physicians’ conflicting demands of care, time constraints and perceived patient resistance can contribute to clinical inertia. Methods like registries with graphical depiction of BP trends can help providers identify patients with chronic high BP measurements.Citation50 This could ultimately help reduce clinical inertia. Increasing evidence also supports the role of other team members in using protocol-driven antihypertensive therapy to achieve optimal outcomes.Citation44,Citation46,Citation51
Therapeutic options
Angiotensin converting enzyme inhibitors (ACEi)
In this section we show key evidence from trials BENEDICTCitation52, CAPPPCitation53,Citation54 and HOPECitation23 that ACEi are superior to other drug classes in preventing nephropathy and CVD in patients with diabetes. These benefits are independent of the BP-lowering effect, thus making ACEi ideal first-line antihypertensive agents in individuals with type 2 diabetes.
Renal outcomes
It is well documented that ACEi are renoprotective in persons with diabetes, who have either hypertension, microalbuminuria or renal insufficiency.Citation52,Citation55–Citation59 An important example is the BENEDICTCitation52 study, in which 1204 individuals with diabetes, mean BP 150/87 and normoalbuminuria received either placebo, ACEi, CCB or ACEi + CCB combination therapy. After 3 years of follow up, BP values were similar among all groups (about 140/80 mmHg), yet microalbuminuria occurred significantly less in subjects treated with ACEi-based therapy than in those receiving CCB or placebo.
In conclusion, BENEDICTCitation52 and other randomized clinical trials, like those by Ahmad et alCitation55 and Lewis et alCitation56 show clearly that ACEi reduce microalbuminuria and rate of nephropathy in patients with type 2 diabetes apart from their antihypertensive effect.
Cardiovascular outcomes
More importantly, several trials document that ACEi decrease diabetes-related CV complications apart from their antihypertensive effect. The first study to address this issue was CAPPP.Citation53,Citation54 It examined if the ACEi captopril lowers macrovascular outcomes more than a diuretic or β-blocker in patients with diastolic BP ≥ 100 mmHg. At study entry, 4.9% of 10,985 subjects had diabetes. After 6.1 years of follow up, study groups achieved similar BP 154/89 mmHg but with different end-points. Patients with diabetes receiving captopril experienced greater significant reductions than those treated with a diuretic or β-blocker: 41% in combined primary outcomes (fatal and nonfatal MI, fatal and nonfatal strokes, or CV deaths), 66% in nonfatal MIs and 46% in total mortality.
It is worth pointing that although CAPPP trial showed superiority of ACEi over β-blockers, the same benefit was not seen in the UKPDS 38Citation18 study. This discrepancy could be explained by the fact that subjects enrolled in the UKPDS were recently diagnosed with diabetes and therefore of low baseline CV risk.
Evidence from the HOPECitation23 trial further supports the CV benefits of ACEi independently of their BP-lowering effect. At study entry, 3577 subjects with diabetes had mean BP 142/80 mmHg, coronary artery disease (CAD), peripheral arterial disease (PAD) or stroke. Participants were randomized to receive either ramipril 10 mg/day or placebo. Primary outcome was the occurrence of MI, stroke or CVD, with overt nephropathy being a substudy end-point. Subjects were followed for 4.5 years; however, the trial was terminated 6 months earlier due to consistent benefits of ACEi over placebo. The ramipril group achieved a slightly lower BP than the placebo arm (Δ2.4/Δ1.0 mmHg).
However when BP differences were adjusted, patients with diabetes receiving ramipril experienced greater significant reductions than those treated with placebo: 24% in overt nephropathy, 22% in MI, 33% in strokes, 37% in CV deaths and 25% in combined CV events. After the trial ended and the randomization was lost, participants were monitored for an additional 2.6 years.Citation60 The use of ACEi was similar in both groups, but patients who were previously in the ramipril arm experienced additional 19%, 16% and 34% relative reductions in MIs, revascularizations and incidence of new diabetes respectively.
CAPPPCitation53,Citation54 and HOPECitation23 trials have shown clearly the CV benefits of ACEi compared to placebo, diuretics or β-blockers. Positive CV outcomes of ACEi over diuretics were also seen in the ANBP2Citation61 study during 4.1 years of observation. Similarly, 3 major randomized trials; hypertensive ABCD,Citation62 STOP-2Citation63 and FACET,Citation64 reveal the superiority of ACEi over dihydropyridine CCB in reducing macrovascular events and especially MI, in hypertensive subjects with diabetes. These results were seen over a period of 3.5 to 5 years and were independent of the BP-lowering effect of ACEi.Citation62–Citation64 Collectively the above 6 studies support the use of ACEi as first-line therapy for hypertension in patients with type 2 diabetes.
Angiotensin receptor blockers (ARB)
Data suggests that ARB could also be first-line treatment of hypertension in individuals with diabetes. Over the last decade, several randomized clinical studies have shown that interruption of the renin-angiotensin system by ARB is equally beneficial in lowering BP and rate of diabetic nephropathy. However their relative importance in preventing CV outcomes is rather inconsistent.
Renal outcomes
Three key randomized trials, RENAAL,Citation65 IDNTCitation66 and Parving et alCitation67 have established that ARB are renoprotective in diabetes, apart from their antihypertensive effect.
The RENAAL study compared ARB losartan with placebo in 1513 patients with diabetes, mean BP 153/82 mmHg and baseline serum creatinine 1.9. After 3.4 years of follow up, both groups achieved similar BP values, but subjects receiving losartan experienced 25% more reduction in serum creatinine doubling (P <0.05) and 28% greater decrease in development of ESRD (P < 0.05) than those treated with placebo.
IDNTCitation66 trial had a similar design. Subjects (N = 1715) with diabetes, mean BP 159/87 mmHg and baseline serum creatinine 1.66 were randomized into the ARB irbesartan, CCB amlodipine, or placebo groups. After 2.6 years of follow up, the irbesartan arm experienced 23% and 20% more significant reductions in composite end-points of serum creatinine doubling, ESRD, or death from any cause than the amlodipine and placebo group, respectively. Results were independent of the BP-lowering effects.
A third trial, by Parving et alCitation67 compared irbesartan at 2 doses (150 mg/day and 300 mg/day) with placebo in preventing nephropathy in 590 patients with diabetes, who had mean BP 153/90 mmHg and normal renal function, but baseline microalbuminuria. After 2 years of follow up, when adjusted for differences in initial urinary albumin excretion (UAE) and final BP values, nephropathy – defined by UAE > 200 μg/min or 30% rise from baseline – occurred significantly less in the irbesartan 150 mg/day and irbesartan 300 mg/day groups than in the placebo arm by 39% and 70%, respectively.
However, it is important to add that ARB might be harmful in a subset of patients at high risk for vascular complications. In the recent randomized TRANSCENDCitation68 trial (N = 5926), after 4.6 years of observation, telmisartan 80 mg/day increased creatinine doubling 59% more than placebo, although no difference in the occurrence of dialysis was detected between groups. Diabetes was present in 36% of participants.
In conclusion, ARB are overall more effective than CCB and placebo in decreasing microalbuminuria and rate of nephropathy in persons with diabetes, independently of their BP-lowering effect.
Cardiovascular outcomes
There is conflicting evidence whether ARB prevent CVD apart from their antihypertensive effect in patients with diabetes.
For example, LIFECitation69 demonstrated that ARB losartan reduced CV events greater than β-blocker atenolol in individuals with diabetes. At study entry, 13% of 9193 subjects with diabetes, mean BP 174/98 and left ventricular hypertrophy (LVH) were randomized to receive either losartan or atenolol. After 4 years of follow up, although BP decreased similarly in both groups (Δ30/Δ17 mmHg), combined CV events (death, MI or stroke) and strokes occurred significantly less in the ARB group than in the β-blocker arm by 13% and 25%, respectively.
Of interest, the following significant differences were observed in the losartan group compared to atenolol arm: less adverse effects, fewer cases of new-onset diabetes and greater decrease in LVH. In conclusion, like ACEi captopril in the CAPPPCitation53, Citation54 trial, ARB losartan performed better than β-blocker in preventing CV events in patients with diabetes. This was independent of BP-lowering effect and likely due to direct reduction of the left ventricular mass.
However, there are some contrary results from trials, SCOPE,Citation70 VALUECitation71 and TRANSCEND.Citation72 ARB blocker was not superior to placebo in SCOPE (N = 4964), or to CCB in VALUE study (N = 15245) in reducing composite CV outcomes over a period of about 4 years. In both studies diabetes was present in 12% and 34% of participants, respectively. However, in SCOPE, the ARB did reduce the secondary outcome of nonfatal strokes 28% more than placebo (P < 0.05).
Recently, TRANSCENDCitation72 examined the efficacy of telmisartan versus placebo in preventing CV events in high risk patients, who were intolerable to ACEi. At enrollment, of 5926 individuals with CAD, PAD or stroke, 36% had diabetes. After 4.6 years of observation, ARB therapy lowered BP significantly more than placebo (Δ3.2/Δ1.3 mmHg). Unexpectedly, however, telmisartan 80 mg/day did not reduce the composite primary outcomes of CV death, MI, stroke, or HF hospitalizations more than placebo.
In conclusion, the overall evidence supports the usefulness of ARB in decreasing the rate of nephropathy apart from their BP-lowering effect. However, given the inconsistent benefits in preventing CV outcomes compared to CCB and placebo, ARB could be less favorable than ACEi as first-line agent for treatment of hypertension in type 2 diabetes (indirect evidence).
ACEi versus ARB
In this section we show the direct evidence documenting equivalence between ACEi and ARB in preventing renal and CV outcomes; therefore, suggesting the use of ARB as a first-line agent. We also demonstrate that their combination is not more beneficial than each drug alone in patients with type 2 diabetes.
Renal outcomes
Two important randomized trials, DETAILCitation73 and by Lacourciere et alCitation74 show that ACEi and ARB therapies are equally renoprotective in diabetes. DETAIL examined if telmisartan was equivalent to enalapril in retarding worsening of renal insufficiency in subjects with type 2 diabetes, mean BP 152/85 mmHg and early nephropathy. At study entry, 250 participants with GFR of >90 mL/min were randomized into enalapril 20 mg/day or telmisartan 80 mg/day groups. After 5 years of follow up, no significant differences in BP reduction or GFR decline (primary outcome) were detected between the two groups.
Analogous results were seen between ACEi enalapril and ARB losartan in persons with diabetes in a smaller randomized trial (N = 92) by Lacourciere et al. At 1 year, enalapril and losartan treatments were equivalent in lowering BP, and delaying both the progression of albuminuria and GFR fall.Citation74 In summary the smaller studies, DETAILCitation73 and by Lacourciere et alCitation74 suggest that ACEi and ARB are equally renoprotective in patients with type 2 diabetes.
Cardiovascular outcomes
Equivalence between ARB and ACEi therapy in preventing CV events in persons with diabetes comes from two important randomized trials, ONTARGETCitation75 and VALIANT.Citation76
ONTARGET compared ARB and ARB + ACEi combination treatment against ACEi therapy alone. Subjects (N = 25,620) with mean BP 142/82 mmHg and established CAD, PAD, or stroke were randomized to receive either telmisartan, enalapril, or both. At study entry, 37% of participants had diabetes. Primary outcome was the occurrence of MI, stroke, CV death, or hospitalization from HF. After 4.6 years of follow up, the telmisartan and telmisartan + enalapril groups achieved a slightly lower BP than the enalapril arm (Δ0.9/Δ0.6 and Δ2.4/Δ1.4 mmHg respectively). However, the small difference in BP did not translate into improved composite primary outcomes in those receiving either telmisartan or telmisartan + enalapril therapy.
Two important observations were seen in subjects treated with both ACEi and ARB compared to ACEi alone. First, the ACEi + ARB combination group experienced a 9% significant relative rise in composite end-points of dialysis, creatinine doubling or death.Citation77 Second, the combined therapy caused significantly more adverse events in the form of hypotension, syncope and renal insufficiency than ACEi. On the other hand, the telmisartan and enalapril groups achieved similar outcomes with similar overall side effects.
Analogous results were seen in the VALIANTCitation76 trial, which compared ACEi captopril versus ARB valsartan versus both in preventing macrovascular complications in normotensive subjects with acute MI. Of 14,808 individuals, 23% had diabetes. After 2.6 years of follow up, although the ACEi + ARB group achieved a slightly lower BP than the ACEi arm (Δ2/Δ1 mmHg, P < 0.05), the primary outcome – all cause mortality, CV mortality, recurrent MI, or hospitalization from HF – occurred similarly among all three interventional groups. In addition, patients treated with ACEi + ARB experienced more hypotensive episodes than those receiving ACEi alone (P < 0.05), thus resulting in frequent lowering or withdrawal of the combined therapy with ACEi + ARB.
In conclusion, ONTARGETCitation75 and VALIANTCitation76 show that ARB and ACEi treatments are equivalent in preventing CV outcomes in high risk patients with diabetes. This suggests that ARB could be first-line antihypertensive therapy as well in diabetes. However, the combination of ARB with ACEi was nonsuperior in end-points and caused more adverse events than the ACEi alone. This makes the ARB + ACEi combined regimen undesirable for treatment of hypertension in persons with type 2 diabetes.
CCB, diuretics and β-blockers
Given that most patients with diabetes will require 2 or more drugs to treat hypertension,Citation18,Citation36,Citation43 it is important to find the most suitable second-line therapeutic agent. This applies also to patients who are intolerant of ACEi or ARB. Such information could be extrapolated from results of 4 major trials: ALLHAT,Citation78 INSIGHT,Citation79 NORDILCitation80 and INVEST.Citation81
ALLHAT examined 33,357 subjects with mean BP 146/84 mmHg and established CHD, of which 36% had diabetes. Participants were randomized into 4 treatment groups: diuretic chlorthalidone, CCB amlodipine, ACEi lisinopril or α-blocker doxazosin. Primary outcome was the occurrence of combined fatal CHD and nonfatal MI. The doxazosin arm was terminated early due to increased incidence of HF. After 4.9 years of observation, the primary outcome was similar among all three antihypertensive drugs.
However, for secondary end-points, the following differences were seen: the incidence of new HF in the amlodipine group, and combined CVD in the lisinopril arm occurred more commonly than in the chlorthalidone group by 38% and 10%, respectively (P < 0.05). This was perhaps due to chlorthalidone causing a slightly lower, but significant, systolic BP than amlodipine and lisinopril. Similar results were seen in patients with and without diabetes. Overall, the three antihypertensive drug classes, ACEi, CCB and thiazide, were equivalent in decreasing combined fatal CHD and nonfatal MI in high risk patients with diabetes.
INSIGHTCitation79 (N = 6321) compared the dihydropyridine CCB nifedipine with diuretics, and NORDILCitation80 (N = 10881) evaluated the non-dihydropyridine CCB diltiazem versus diuretic or β-blocker based therapies in preventing CV events in patients with hypertension. In both studies, diabetes was present in 20.6% and 6.5% of participants, respectively. Participants were followed for a period of 4 to 5 years. No major differences in final BP values or in combined primary outcomes of CV deaths, stroke, or MIs were seen between interventional groups.
INVESTCitation81 was a shorter duration study that compared the efficacy of non-dihydropyridine CCB verapamil against β-blocker atenolol in preventing CV events in patients with hypertension and CAD. Primary end-points were occurrence of nonfatal MI, nonfatal stroke, or death from any cause. At enrollment, 28% of 22576 subjects had diabetes. After 2.7 years of follow up, no significant differences in BP measurements or primary outcomes were detected between the two groups.
In conclusion, ALLHAT,Citation78 INSIGHT,Citation79 NORDILCitation80 and INVESTCitation81 show that CCB (dihydropyridine or non-dihydropyridine), thiazide diuretic and β-blocker are overall equivalent in lowering BP and rate of CV events in individuals with diabetes. By extrapolation, one could infer that any of the three classes can be added to the initial ACEi or ARB antihypertensive therapy. For those intolerant of ACEi or ARB, a CCB, thiazide or β-blocker could be used as first-line treatment of high BP in patients with diabetes.
A case for CCB as second-line therapy
More reliable data in choosing the second-line antihypertensive therapy after ACEi or ARB in patients with diabetes come from ACCOMPLISHCitation82 and GUARDCitation83 randomized trials. ACCOMPLISH evaluated if ACEi + CCB (benazepril + amlodipine) was superior to ACEi + hydrochlorothiazide (benazepril + HCTZ) combination therapy in preventing CV events in subjects with mean BP 145/80 mmHg and established MI, CAD, previous coronary revascularization or stroke. At study entry, 60% of 11,506 participants had diabetes. Primary outcome was the occurrence of CV death, MI, stroke, hospitalization from angina, coronary revascularization, or resuscitation after sudden cardiac arrest.
The trial was terminated early at 3 years due to clear benefits in the benazapril + amlodipine arm: ACEi + CCB combination group achieved a lower BP (Δ0.9/Δ1.1 mmHg, P < 0.001) and 20% greater reduction (P < 0.001) in composite primary outcomes than the ACEi + HCTZ arm. Similar results were noted among patients with diabetes. However, for renal outcomes in individuals with diabetes, secondary analysis revealed that serum creatinine doubling or ESRD occurred similarly in both interventional groups (HR = 0.78, P < 0.48).Citation84
In contrary, the smaller study GUARDCitation83 showed that the same ACEi + CCB combined therapy used in ACCOMPLISHCitation82 could be more beneficial than ACEi + HCTZ regimen in preventing diabetic nephropathy. At enrollment, 332 subjects with diabetes, albuminuria and mean BP 151/88 mmHg received either the benazepril + amlodipine or benazepril + HCTZ combination therapy. After 1 year of follow up, individuals treated with ACEi + CCB achieved a lower diastolic BP (Δ2 mmHg, P < 0.05) and higher GFR (Δ11.6 mL/min, P < 0.05) than those receiving the ACEi + HCTZ regimen.
It is worth noting that dihydropyridine and non-dihydropyridine CCB seem to be equivalent in reducing albuminuria and BP in diabetic individuals.Citation85 Indirect evidence also suggests their similarity in preventing CV outcomes in persons with diabetes.Citation78–Citation81 In conclusion, ACCOMPLISHCitation82 and GUARDCitation83 suggest that a dihydropyridine CCB could be a better second-line agent than a diuretic thiazide in lowering BP and risk of CV disease in individuals with hypertension and type 2 diabetes. However, its relative benefit in preventing diabetic nephropathy is somewhat inconsistent.
Aldosterone antagonists, renin inhibitor and α-blockers
Aldosterone antagonists, renin inhibitor and α-blockers can also be utilized to bring BP to goal in patients with type 2 diabetes. Unfortunately no significant comparative data of these agents with ACEi, ARB, CCB, diuretics or β-blockers are available in persons with diabetes. The one exception is α-blocker doxazosin, which increased the incidence of HF more than diuretic chlorthalidone in participants of the ALLHAT trial.Citation78
Evidence suggests that aldosterone antagonists could be critical in treating diabetic individuals with resistant hypertension – defined by the use of ≥3 BP-lowering drugs. For example, in the observational study ASCOT-BPLA,Citation86 spironolactone 25 to 50 mg/day reduced the BP markedly by Δ22/Δ9 mmHg in 1411 subjects with refractory hypertension over a 1.3-year period. In another observational trial of 7 to 15 months’ duration, spironolactone 25 to 100 mg/day lowered BP by Δ16/Δ9 mmHg (P < 0.001) in 175 subjects with resistant high BP.Citation87 In both studies, diabetes was present in 40% and 33% of participants, respectively. It is worth noting that about 15% of individuals with type 2 diabetes and refractory hypertension have primary hyperaldosteronism,Citation88 for which aldosterone antagonist spironolactone or eplerenone would be an ideal therapy.
The renin inhibitor aliskiren, the newest antihypertensive drug class, could be renoprotective apart from its BP-lowering effect in persons with diabetes. For example, in the AVOIDCitation89 trial, 599 subjects with type 2 diabetes, mean BP 135/78 mmHg and baseline macroalbuminuria – already treated with the ARB losartan 100 mg/day – were randomized to receive aliskiren 300 mg/day or placebo. After 6 months of follow up, the renin inhibitor reduced proteinuria 20% more than placebo (P < 0.001). This outcome was independent of the antihypertensive effect of aliskiren.
In conclusion, aldosterone antagonists, renin inhibitor and α-blockers can be added to mainstream therapies of ACEi, ARB, CCB, diuretics or β-blockers, if necessary, to reduce BP to <130/80 mmHg in patients with type 2 diabetes.
Fixed combination therapy improves BP control
One method to improve adherence and reduce clinical inertia among individuals with diabetes and hypertension is to offer a 2-drug fixed dose combination therapy. This is a good rationale since most patients will require more than one drug class to reduce BP to goal.Citation18,Citation36,Citation43
The best evidence comes from ADVANCECitation90 trial, which examined if fixed ACEi + thiazide (perindopril + indapamide) treatment was superior to other antihypertensive regimens in lowering vascular complications in subjects (N = 11140) with type 2 diabetes and mean BP 145/81 mmHg. Primary outcome was the occurrence of combined micro- and macrovascular complications – defined by CV death, nonfatal MI, nonfatal stroke, retinopathy and nephropathy.
After 4.3 years of follow up, the fixed perindopril + indapamide group experienced a lower BP (Δ5.6/Δ2.2 mmHg, P < 0.05) and less composite primary outcomes (Δ9%, P < 0.05) than the control arm. In regard to secondary end points, the fixed ACEi+Thiazide group also experienced significantly fewer CVD and deaths from any cause than its counterpart by 18% and 14% respectively.
Results of two smaller randomized trials also support the beneficial use of fixed dose combination therapy for treatment of hypertension in type 2 diabetes. In the PREMIERCitation91 study, 481 subjects with diabetes, mean BP 158/93 mmHg and albuminuria were randomized to receive fixed ACEi + thiazide (perindopril + indapamide) therapy or ACEi (enalapril) alone. Medication doses were increased based on BP response. Primary outcome was the difference in the albumin excretion rate and supine BP measurements. After 12 months of follow up, the fixed perindopril + indapamide group achieved a lower BP (Δ3/Δ1.5 mmHg, P < 0.05) and less urinary albumin excretion than the enalapril arm.
In the SHIELDCitation92 trial, 214 individuals with diabetes and mean BP 156/97 mmHg were randomized to receive either fixed ACEi + CCB (benazepril + amlodipine) therapy or ACEi (enalapril) alone. Medication doses were increased in both groups if BP ≥ 130/80 mmHg. At 3 months, 63% of subjects in the fixed ACEi + CCB therapy group had achieved the BP goal compared to only 37% of those treated with enalapril. The difference was statistically significant (P = 0.002).
In summary, early initiation of 2-drug fixed dose combination therapy with ACEi + CCB or thiazide improves BP control more than monotherapy in patients with hypertension and diabetes.
Recommendations
Hypertension is not only the main contributor of increased CV morbidity and mortality in patients with type 2 diabetes, but also the least controlled variable compared to hyperglycemia and dyslipidemia risk factors.Citation35–Citation37 This calls for an aggressive approach in reducing BP under 130/80 mmHg in all individuals with diabetes. Perhaps a lower target might be considered in the future.Citation29,Citation30 Similar to guidelines by several major organizations,Citation24–Citation28 we recommend that if BP is persistently ≥130/80 mmHg, then life-style intervention should be initiated. However, if BP ≥ 140/90 mmHg, pharmacotherapy must be started as well.
Life-style changes that reduce BPCitation93 are low sodium diet < 1.5 g/day,Citation94 increased potassium intake >4.7 g/day, BMI <25 kg/m2, weight loss by >4.5 to 5.0 kg,Citation95,Citation96 increased intake of fruits and vegetables (8 to 10 servings/day), decreased consumption of dairy products that are rich in fat (2 to 3 servings/day), avoidance of excessive alcohol use (≤2 drinks/day/men and ≤1 drink/day/women) and increased physical activity.Citation96,Citation97 Studies in patients without diabetes have shown that these measures are equivalent to drug monotherapy for mild hypertension.Citation94 But unlike medication monotherapy, life-style interventions in the form of exercise and weight loss could help control other aspects of diabetes such as hyperglycemia and dyslipidemia.
If life-style changes are unsuccessful or BP ≥ 140/90 mmHg then pharmacotherapy should be added immediately. Beta-blocker must be given to all patients with established CAD or MI.Citation98 In we present 2 different protocols based on initial BP value. In the first, when BP is 130/80 to 140/90 mmHg, we advise first-line monotherapy with either an ACEi or ARB, depending on availability, cost and tolerability. Equivalence of ARB with ACEi was documented in the trials DETAIL,Citation73 ONTARGETCitation75 and VALIANT.Citation76
Figure 1 Algorithm for treatment of hypertension in inividuals with diabetes. Maximize dose before starting the next drug.
First line = ACEi or ARB (equivalence seen in DETAILCitation73 ONTARGETCitation75 and VALIANTCitation76).
Both reduce microalbuminuria and rate of nephropathy independently of their antihypertensive effect.
ACEi preferred over ARB (indirect evidence for cardiovascular outcomes; SCOPE,Citation70 VALUECitation71 and TRANSCENDCitation72).
Recommend against concomitant use of ARB with ACEi (ONTARGETCitation75 and VALIANTCitation76).
Second line = CCB or diuretic
Dihydropyridine CCB favored over diuretic (ACCOMPLISHCitation82 and GUARDCitation83) or in the presence of electrolyte anomalies.
Diuretic preferred in heart failure or edematous conditions.
Loop diuretic recommended if GFR ≤ 30 mL/min due to marked state of fluid overload.
If needed, CCB and diuretic can be combined.
Third line = β-blocker, primarily due to side effect profile. However, it is indicated in all patients with established CAD and MI.
Fourth line = Aldosterone antagonist (ASCOT-BPLACitation86).
Fifth line = Renin inhibitor or α-blocker, not enough comparative data from clinical trials for clear recommendation.
Peripheral α-blocker, due to orthostatic hypotension and results of ALLHAT.Citation78 It could be used earlier in patients with symptomatic BPH.
arenal artery stenosis, hyperaldosteronism, Cushing’s syndrome or pheochromocytoma.
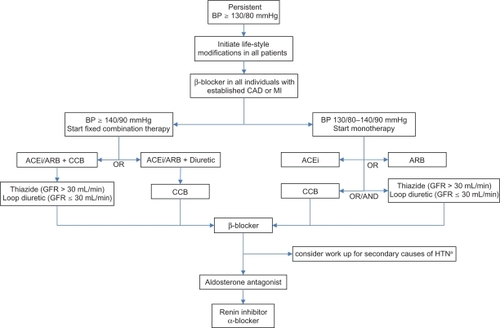
In the second protocol, when BP is ≥ 140/90 mmHg, we recommend starting a low-dose fixed combination regimen containing either ACEi or ARB. Here we also consider patient adherence, clinical inertia and the fact that most individuals will require 2 or more drugs to control their hypertension. Early initiation of combined therapy is increasingly recommended for glucose management as well.Citation99 Based on indirect evidence from SCOPE,Citation70 VALUE,Citation71 and TRANSCEND,Citation72 one could favor treatment with ACEi over ARB. Given the results of ONTARGETCitation75 and VALIANT,Citation76 we advise against concomitant use of ACEi with ARB, since together they cause significantly higher rates of adverse events without additional benefits.
In both protocols, for second-line therapy we suggest using dihydropyridine CCB over diuretics, based on outcomes from ACCOMPLISHCitation82 and GUARD.Citation83 The choice would also depend on relative contraindications of each drug class. For example, a CCB is favored over a thiazide in an individual with electrolyte anomalies but less so in someone who suffers from HF or edematous conditions. A loop diuretic is recommended over a thiazide if GFR ≤ 30 mL/min due to patients’ state of fluid overload. The dose of medications must be increased or maximized based on BP response. If BP is still uncontrolled then we recommend adding either a CCB or diuretic, whichever is not part of the current combination therapy.
If BP goal is not achieved, we suggest adding a β-blocker. We chose β-blockers to be third-line agents primarily due to poor side effect profile of bradycardia and worsening of insulin resistance,Citation100,Citation101 although UKPDS,Citation18 NORDILCitation80 and INVESTCitation81 clearly show their equivalence to ACEi and CCB. At this point we also consider screening for secondary causes of hypertension like renal artery stenosis, hyperaldosteronism,Citation88 Cushing’s syndrome or pheochromocytoma.
As a fourth-line therapy, we choose aldosterone antagonists due to their BP-lowering potency, revealed in the ASCOT-BPLACitation86 trial. Finally, the renin inhibitors and α-blockers can also be utilized, if necessary, to control BP in persons with diabetes. We advise peripheral α-blockers to be a last-line therapeutic option based on results of ALL-HATCitation78 and their propensity to cause orthostatic hypotension – although they could be used earlier in someone with benign prostate hyperplasia.
In conclusion, hypertension continues to be a key determinant of morbidity and mortality in type 2 diabetes. Despite clear evidence for a BP goal < 130/80 mmHg, most patients do not achieve optimal results. Early initiation of fixed-dose combination therapy and aggressive titration of medications can improve patient adherence, reduce clinical inertia and bring BP to target, thereby reducing both micro- and macrovascular complications in individuals with diabetes.
Disclosures
The authors report no conflicts of interest in this work.
References
- HuangESBasuAO’GradyMCaprettaJCProjecting the future diabetes population size and related costs for the U.SDiabetes Care200932122225222919940225
- WildSRoglicGGreenASicreeRKingHGlobal prevalence of diabetes: estimates for the year 2000 and projections for 2030Diabetes Care20042751047105315111519
- HaffnerSMLehtoSRonnemaaTPyoralaKLaaksoMMortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarctionN Engl J Med199833942292349673301
- KannelWBMcGeeDLDiabetes and cardiovascular disease. The Framingham studyJAMA19792411920352038430798
- MansonJEColditzGAStampferMJA prospective study of maturity-onset diabetes mellitus and risk of coronary heart disease and stroke in womenArch Intern Med19911516114111472043016
- LaaksoMHyperglycemia and cardiovascular disease in type 2 diabetesDiabetes199948593794210331395
- SowersJREpsteinMDiabetes mellitus and associated hypertension, vascular disease, and nephropathy. An updateHypertension1995266 Pt 18698797490142
- MolitchMEDeFronzoRAFranzMJNephropathy in diabetesDiabetes Care200427Suppl 1S79S8314693934
- CiullaTAAmadorAGZinmanBDiabetic retinopathy and diabetic macular edema: pathophysiology, screening, and novel therapiesDiabetes Care20032692653266412941734
- SimonsonDCEtiology and prevalence of hypertension in diabetic patientsDiabetes Care198811108218273073072
- Hypertension in Diabetes Study (HDS): IPrevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complicationsJ Hypertens19931133093178387089
- Mortality findings for stepped-care and referred-care participants in the hypertension detection and follow-up program, stratified by other risk factors. The Hypertension Detection and Follow-up Program Cooperative Research GroupPrev Med19851433123352865725
- Hypertension in Diabetes Study (HDS): IIIncreased risk of cardiovascular complications in hypertensive type 2 diabetic patientsJ Hypertens19931133193258387090
- TurnerRCMillnsHNeilHARisk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23)BMJ199831671348238289549452
- MehlerPSJeffersBWEstacioRSchrierRWAssociations of hypertension and complications in non-insulin-dependent diabetes mellitusAm J Hypertens19971021521619037322
- SchrierRWEstacioROEslerAMehlerPEffects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokesKidney Int20026131086109711849464
- KohnerEMAldingtonSJStrattonIMUnited Kingdom Prospective Diabetes Study, 30: diabetic retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and associated risk factorsArch Ophthalmol199811632973039514482
- Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 UK Prospective Diabetes Study GroupBMJ199831771607037139732337
- HolmanRRPaulSKBethelMANeilHAMatthewsDRLong-term follow-up after tight control of blood pressure in type 2 diabetesN Engl J Med2008359151565157618784091
- CurbJDPresselSLCutlerJAEffect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research GroupJAMA199627623188618928968014
- TuomilehtoJRastenyteDBirkenhagerWHEffects of calcium-channel blockade in older patients with diabetes and systolic hypertension. Systolic Hypertension in Europe Trial InvestigatorsN Engl J Med1999340967768410053176
- HanssonLZanchettiACarruthersSGEffects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study GroupLancet19983519118175517629635947
- Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study InvestigatorsLancet2000355920025325910675071
- RydenLStandlEBartnikMGuidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD)Eur Heart J20072818813617220161
- RosendorffCBlackHRCannonCPTreatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and PreventionCirculation2007115212761278817502569
- ChobanianAVBakrisGLBlackHRSeventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureHypertension20034261206125214656957
- K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAm J Kidney Dis2002392 Suppl 1S1S26611904577
- Executive summary: Standards of medical care in diabetes – 2010Diabetes Care33Suppl 1S4S1020042774
- AdlerAIStrattonIMNeilHAAssociation of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational studyBMJ2000321725841241910938049
- EstacioROCollJRTranZVSchrierRWEffect of intensive blood pressure control with valsartan on urinary albumin excretion in normotensive patients with type 2 diabetesAm J Hypertens200619121241124817161769
- MogensenCEMicroalbuminuria predicts clinical proteinuria and early mortality in maturity-onset diabetesN Engl J Med198431063563606690964
- GersteinHCMannJFYiQAlbuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individualsJAMA2001286442142611466120
- MattockMBMorrishNJVibertiGKeenHFitzgeraldAPJacksonGProspective study of microalbuminuria as predictor of mortality in NIDDMDiabetes19924167367411587400
- GodleyPJMaueSKFarrellyEWFrechFThe need for improved medical management of patients with concomitant hypertension and type 2 diabetes mellitusAm J Manag Care200511420621015839181
- GudbjornsdottirSEeg-OlofssonKCederholmJZetheliusBEliassonBNilssonPMRisk factor control in patients with Type 2 diabetes and coronary heart disease: findings from the Swedish National Diabetes Register (NDR)Diabet Med2009261536019125761
- MannDMWoodwardMYeFKrousel-WoodMMuntnerPTrends in medication use among US adults with diabetes mellitus: glycemic control at the expense of controlling cardiovascular risk factorsArch Intern Med2009169181718172019822830
- McFarlaneSIJacoberSJWinerNControl of cardiovascular risk factors in patients with diabetes and hypertension at urban academic medical centersDiabetes Care200225471872311919131
- McLeanDLSimpsonSHMcAlisterFATsuyukiRTTreatment and blood pressure control in 47,964 people with diabetes and hypertension: a systematic review of observational studiesCan J Cardiol2006221085586016957803
- PrevostGPhanTMMounier-VehierCFontainePControl of cardiovascular risk factors in patients with type 2 diabetes and hypertension in a French national study (Phenomen)Diabetes Metab200531547948516357792
- RaumELietzauSStegmaierCBrennerHRothenbacherDFor the majority of patients with diabetes blood pressure and lipid management is not in line with recommendations. Results from a large population-based cohort in GermanyPharmacoepidemiol Drug Saf200817548549418383562
- BertholetNFavratBFallab-StubiCLBrunnerHRBurnierMWhy Objective Monitoring of Compliance is Important in the Management of HypertensionJ Clin Hypertens (Greenwich)20002425826211416658
- CramerJABenedictAMuszbekNKeskinaslanAKhanZMThe significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a reviewInt J Clin Pract2008621768717983433
- ZidekWNaditch-BruleLPerliniSFarsangCKjeldsenSEBlood pressure control and components of the metabolic syndrome: the GOOD surveyCardiovasc Diabetol200985119754934
- StuckeyHLDellasegaCGraberNJMaugerDTLendelIGabbayRADiabetes nurse case management and motivational interviewing for change (DYNAMIC): study design and baseline characteristics in the Chronic Care Model for type 2 diabetesContemp Clin Trials200930436637419328244
- GabbayRADurdockKThe use of motivational interviewing to improve elderly diabetic patient’s adherence to treatment recommendationsLignalliATHandbook of Type 2 Diabetes in the Middle Aged and ElderlyNova Science20095768
- SchroederKFaheyTEbrahimSHow can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trialsArch Intern Med2004164772273215078641
- PhillipsLSBranchWTCookCBClinical inertiaAnn Intern Med2001135982583411694107
- KerrEAZikmund-FisherBJKlamerusMLSubramanianUHoganMMHoferTPThe role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressureAnn Intern Med20081481071772718490685
- Gil-GuillénVOrozco-BeltránDPérezRPClinical inertia in diagnosis and treatment of hypertension in primary care: Quantification and associated factorsBlood Press201019131019929287
- KhanLMincemoyerSGabbayRADiabetes registries: where we are and where are we headed?Diabetes Technol Ther200911425526219344200
- Improvingchroniccare.org [homepage on the Internet]. The chronic care model [updated 2009].http://www.improvingchroniccare.org/. Accessed April 28, 2010
- RuggenentiPFassiAIlievaAPPreventing microalbuminuria in type 2 diabetesN Engl J Med2004351191941195115516697
- HanssonLLindholmLHNiskanenLEffect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trialLancet1999353915361161610030325
- NiskanenLHednerTHanssonLLankeJNiklasonAReduced cardiovascular morbidity and mortality in hypertensive diabetic patients on first-line therapy with an ACE inhibitor compared with a diuretic/beta-blocker-based treatment regimen: a subanalysis of the Captopril Prevention ProjectDiabetes Care200124122091209611723089
- AhmadJSiddiquiMAAhmadHEffective postponement of diabetic nephropathy with enalapril in normotensive type 2 diabetic patients with microalbuminuriaDiabetes Care19972010157615819314638
- LewisEJHunsickerLGBainRPRohdeRDThe effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study GroupN Engl J Med199332920145614628413456
- RavidMBroshDLeviZBar-DayanYRavidDRachmaniRUse of enalapril to attenuate decline in renal function in normotensive, normoalbuminuric patients with type 2 diabetes mellitus. A randomized, controlled trialAnn Intern Med199812812 Pt 19829889625684
- RavidMLangRRachmaniRLishnerMLong-term renoprotective effect of angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus. A 7-year follow-up studyArch Intern Med199615632862898572838
- SanoTKawamuraTMatsumaeHEffects of long-term enalapril treatment on persistent micro-albuminuria in well-controlled hypertensive and normotensive NIDDM patientsDiabetes Care19941754204248062609
- BoschJLonnEPogueJArnoldJMDagenaisGRYusufSLong-term effects of ramipril on cardiovascular events and on diabetes: results of the HOPE study extensionCirculation200511291339134616129815
- WingLMReidCMRyanPA comparison of outcomes with angiotensin-converting – enzyme inhibitors and diuretics for hypertension in the elderlyN Engl J Med2003348758359212584366
- EstacioROJeffersBWHiattWRBiggerstaffSLGiffordNSchrierRWThe effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertensionN Engl J Med1998338106456529486993
- HanssonLLindholmLHEkbomTRandomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 studyLancet199935491921751175610577635
- TattiPPahorMByingtonRPOutcome results of the Fosinopril Versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDMDiabetes Care19982145976039571349
- BrennerBMCooperMEde ZeeuwDEffects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathyN Engl J Med20013451286186911565518
- LewisEJHunsickerLGClarkeWRRenoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetesN Engl J Med20013451285186011565517
- ParvingHHLehnertHBrochner-MortensenJGomisRAndersenSArnerPThe effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetesN Engl J Med20013451287087811565519
- MannJFSchmiederREDyalLEffect of telmisartan on renal outcomes: a randomized trialAnn Intern Med2009151111019451556
- DahlofBDevereuxRBKjeldsenSECardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenololLancet20023599311995100311937178
- LithellHHanssonLSkoogIThe Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trialJ Hypertens200321587588612714861
- JuliusSKjeldsenSEWeberMOutcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trialLancet200436394262022203115207952
- YusufSTeoKAndersonCEffects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: a randomised controlled trialLancet200837296441174118318757085
- BarnettAHBainSCBouterPAngiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathyN Engl J Med2004351191952196115516696
- LacourciereYBelangerAGodinCLong-term comparison of losartan and enalapril on kidney function in hypertensive type 2 diabetics with early nephropathyKidney Int200058276276910916100
- YusufSTeoKKPogueJTelmisartan, ramipril, or both in patients at high risk for vascular eventsN Engl J Med2008358151547155918378520
- PfefferMAMcMurrayJJVelazquezEJValsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or bothN Engl J Med2003349201893190614610160
- MannJFSchmiederREMcQueenMRenal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trialLancet2008372963854755318707986
- Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)JAMA2002288232981299712479763
- BrownMJPalmerCRCastaigneAMorbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT)Lancet2000356922736637210972368
- HanssonLHednerTLund-JohansenPRandomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) studyLancet2000356922735936510972367
- PepineCJHandbergEMCooper-DeHoffRMA calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trialJAMA2003290212805281614657064
- JamersonKWeberMABakrisGLBenazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patientsN Engl J Med2008359232417242819052124
- BakrisGLTotoRDMcCulloughPARochaRPurkayasthaDDavisPEffects of different ACE inhibitor combinations on albuminuria: results of the GUARD studyKidney Int200873111303130918354383
- BakrisGLSarafidisPAWeirMRDahlofBPittBJamersonKRenal Outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomized controlled trialLancet2010 Published online February 18, 2010, www.thelancet.com
- BakrisGLWeirMRSecicMCampbellBWeis-McNultyADifferential effects of calcium antagonist subclasses on markers of nephropathy progressionKidney Int20046561991200215149313
- ChapmanNDobsonJWilsonSEffect of spironolactone on blood pressure in subjects with resistant hypertensionHypertension200749483984517309946
- de SouzaFMuxfeldtEFiszmanRSallesGEfficacy of spironolactone therapy in patients with true resistant hypertensionHypertension55114715219858405
- UmpierrezGECanteyPSmileyDPrimary aldosteronism in diabetic subjects with resistant hypertensionDiabetes Care20073071699170317429062
- ParvingHHPerssonFLewisJBLewisEJHollenbergNKAliskiren combined with losartan in type 2 diabetes and nephropathyN Engl J Med2008358232433244618525041
- PatelAMacMahonSChalmersJEffects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trialLancet2007370959082984017765963
- MogensenCEVibertiGHalimiSEffect of low-dose perindopril/indapamide on albuminuria in diabetes: preterax in albuminuria regression: PREMIERHypertension20034151063107112654706
- BakrisGLWeirMRAchieving goal blood pressure in patients with type 2 diabetes: conventional versus fixed-dose combination approachesJ Clin Hypertens (Greenwich)20035320220912826783
- AppelLJBrandsMWDanielsSRKaranjaNElmerPJSacksFMDietary approaches to prevent and treat hypertension: a scientific statement from the American Heart AssociationHypertension200647229630816434724
- SacksFMSvetkeyLPVollmerWMEffects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research GroupN Engl J Med2001344131011136953
- NeterJEStamBEKokFJGrobbeeDEGeleijnseJMInfluence of weight reduction on blood pressure: a meta-analysis of randomized controlled trialsHypertension200342587888412975389
- StevensVJObarzanekECookNRLong-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase IIAnn Intern Med2001134111111187414
- WheltonSPChinAXinXHeJEffect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trialsAnn Intern Med2002136749350311926784
- SmithSCJrAllenJBlairSNAHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood InstituteCirculation2006113192363237216702489
- RodbardHWJellingerPSDavidsonJAStatement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic controlEndocr Pract200915654055919858063
- GressTWNietoFJShaharEWoffordMRBrancatiFLHypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. Atherosclerosis Risk in Communities StudyN Engl J Med20003421390591210738048
- GuptaAKDahlofBDobsonJSeverPSWedelHPoulterNRDeterminants of new-onset diabetes among 19,257 hypertensive patients randomized in the Anglo-Scandinavian Cardiac Outcomes Trial – Blood Pressure Lowering Arm and the relative influence of antihypertensive medicationDiabetes Care200831598298818235048