Abstract
Aim: The first systematic review and meta analysis investigating the prevalence of delirium in Iran and the importance of delirium in the health status of patients. Method: This study is a review article to determine the overall prevalence of delirium in patients admitted to the hospitals in Iran, with search time frame to 12 October 2000–12 October 2018. The study examined the prevalence of delirium in general wards and ICUs of Iran according to published article in domestic and foreign journals. The methodological quality of the papers was based on a tool used in previous studies. Data was analyzed using comprehensive meta-analysis (CMA) software. Findings: The findings showed the prevalence of delirium in hospitalized patients in Iran is 21.8% (CI: 17.5–27.5%). The prevalence of delirium in hospitalized patients in Iran based on the hospitalization in ICU is 24.7% (CI: 18.1–32.7%) and in the general ward is 17.5% (CI: 13.6–22.3%). Conclusion: Due to the relatively high prevalence of delirium in patients admitted to hospitals in Iran, prevention is necessary to reduce the incidence of delirium.
Delirium is a disorder characterized by changes in acute changes in cognition and sensory perception, abnormal thinking and improper behavior. This condition is one of the common problems in patients admitted to ICUs with considerable prevalence [Citation1,Citation2]. As physicians and nurses cannot diagnose all cases of delirium [Citation3], this disorder may not be diagnosed or diagnosed as a psychiatric disorder if no accurate evaluation is performed on the patient [Citation4]. Delirium is a sudden outbreak associated with altered sensory perception, short-term memory impairment and turbulent behavior. The person loses focus and this disorder leads to lack of attention, temporary loss of memory, sleep disturbances, restlessness and illusion [Citation5,Citation6].
Early diagnosis and reduction of risk factors affecting delirium requires the knowledge and awareness of physicians and nurses of the intensive care unit about the nature of delirium syndrome, the symptoms of the disease, as well as the standard tools for screening delirium and the factors that affect it [Citation6–9]. The causes of delirium are complex and are effected by various factors [Citation10,Citation11]. Among the factors affecting delirium are infection [Citation12], age [Citation13], pain [Citation14], physical restraints [Citation15], non relieved pain [Citation16], each of which has different effects on the development of delirium.
Delirium various side effects, including increase in the hospitalization time, increase in the need for nursing care, the incidence of hospital pneumonia, the risk of falling, urinary incontinence and skin disorders [Citation7,Citation17–19]. Furthermore, the nurses working in ICUs have more stress in the care for patients with delirium [Citation20]. Although about 30-40% of delirium can be prevented [Citation13,Citation21,Citation22], most hospitals do not have a systematic protocol for preventing delirium [Citation4,Citation13,Citation23,Citation24]. Thus, attention to delirium is of significant importance [Citation25].
Nursing interventions can reduce the amount of delirium in patients by simulating the environment [Citation6] including for family-centered orientation programs [Citation26] and music therapy [Citation27,Citation28]. Considering the important role of nurses in delirium management, it is necessary to have complete information about the prevalence of this disease [Citation29]. In order to reduce the amount of delirium, its prevalence should be carefully identified and detailed and accurate information should be provided.
In previous studies in Iran, reviews article of delirium have not been conducted, but in other countries, the prevalence has been studied, so that in reviews article by Krewulak et al. [Citation30] and Systematic Review by Fadayomi et al. [Citation31] in the field of delirium. The mentioned studies [Citation30,Citation31] have been carried out in other countries and in Iran there has not been a study aimed at determining the prevalence of delirium through systematic review. For this reason, the present study is innovative.
Aim
Considering the importance of delirium in improving the health status of patients, and as no studies have been conducted on the prevalence of delirium in Iran, the present study was conducted as the first systematic and meta-analytic review study in this regard.
Methods
Study protocol
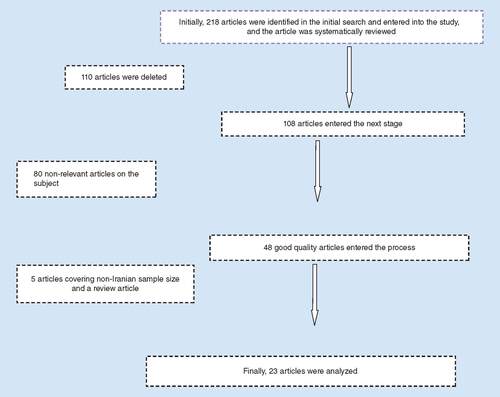
This study is a systematic review with PRISMA guidelines [Citation32] to determine the prevalence of delirium in patients admitted to the hospitals in Iran, with search time frame to 12 October 2000–12 October 2018 ().
Search strategy
The study with aim the prevalence of delirium in general wards and ICUs of Iran according to published article in domestic and foreign journals. The search for papers was done independently by a nurse and an anesthetist to prevent any kind of bias, and if there was a controversy between the two researchers, the specialized search was done by a third colleague specialist in systematic and meta-analytic review studies.
Inclusion criteria & data extraction
At the beginning of the search all articles regarding delirium in Persian and English on the internal databases of Iran (such as IranDoc, SID, Magiran and Iranmedex) and international databases (such as Springer, Science Direct, Medlib, Scopus, PubMed, Ebsco, Web of Science, Wiley Online Library and Cochrane) were gathered. The keywords were ‘delirium’, ‘prevalence’, ‘Iran’ and a combination of them. It should be noted that the references of the articles were evaluated to improve the quality of the search. In this study, interventional and observation articles, letters to the editor, presented in the summary of congresses, as well as existing dissertations, were excluded from the study. Exclusion criteria were irrelevance to the subject, case reports, being interventional, extracted papers being qualitative, and repetitive studies.
The methodological quality of the papers was based tool had five study design items, a comparison group, and descriptions of the characteristics of sample studied, sample size and the tools used. Each item received a score of 0–3, with the higher score showing a higher quality of the methodology of studies [Citation33–36].
Data extraction
After the extraction of the studies the papers were recorded using a checklist with the name of the author, the paper publication year, the location (ward) of the patients under study, the sample size and the prevalence of delirium.
The ethical considerations in the study were observing ethics in research in the publication of results and obtaining a code of ethics from Kermanshah University of Medical Sciences.
Statistical analysis
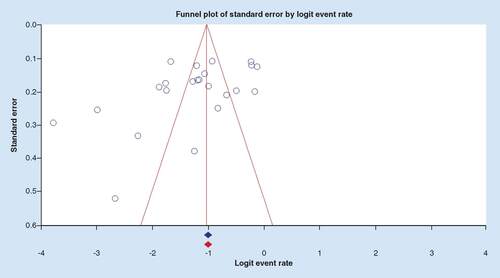
Comprehensive meta-analysis (CMA) software was applied to data analysis. Heterogeneity of prevalence of delirium was checked by tests of Cochran's Q I2 (the heterogeneities of the studies were divided into; less than 25% (low heterogeneity), 25% to 75% (moderate heterogeneity) and more than 75% (high heterogeneity). Regarding the high heterogeneity (I2 = 94.88, Q = 430.02m, p < 0.001) we used DerSimonian and Laird’s random effects model to combine the studies prevalance, Kendal’s tau in Begg and Manzumdar test and Funnel plot were applied for checking the publication bias.
Findings
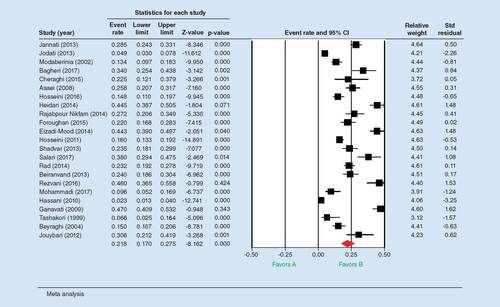
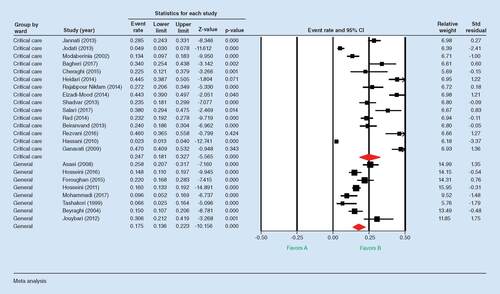
In this paper, 23 studies between 2000 and 2018 were introduced into a quantitative meta-analysis process. 5339 patients were included in these studies in total (). The Cheraghi et al. (2015) study had the lowest number of patients at 40, whilst the Hosseini et al. (2011) had 600 patients, making this the study with the most patients. The highest prevalence of delirium was found in Heidari et al. (2014) in Isfahan with a prevalence of 44.5% and the lowest prevalence rate in Ashraflashkari et al. in Ahwaz, with an incidence of 6.66%. Studies with numbers 1-2-4-5-11-14-15-19-20 have the same hospitalization characteristics due to one type of heart disease and studies with numbers 3-7-8-9-16-17 admitted to intensive care units. shows the characteristics of the articles used in this study. According to the findings of the study, 23 studies were conducted to investigate the prevalence of delirium in general and special sectors ().
Table 1. Delirium prevalence in different patient populations within hospitals in Iran.
The findings of show the prevalence of delirium in hospitalized patients in Iran. According to the findings, this figure is 21.8% (CI: 17.5–27.5%; Q = 430.029 p < 0.001, I2 = 94.884, Z = 8.162, p < 0.001).
The findings of show the prevalence of delirium in hospitalized patients in Iran based on hospitalization in critical care units. According to the findings, this figure is 24.7% (CI: 18.1–32.7%) and in the general ward is 17.5% (CI: 13.6–22.3%). The findings of show the bias in the publication of the articles (Z = 1.58, p = 0.113).
Discussion
Meta-analysis studies provide researchers with relevant evidence [Citation57].The findings showed that the prevalence of delirium in Iran was 21.8%, which is relatively high. The rate in special critical care units is 24.7% and in the general unit is 17.5%. Delirium causes complex complications for patients, which is why it is very important to pay attention [Citation59,Citation60].
According to the findings of this study, the delirium prevalence in critical care was 24.7%, consistent with the results of the study by Collet et al. [Citation61]. Delirium outbreaks in critical wards was found to be 19% in Tilouche and colleagues in Tunisia [Citation62], which is less than the results of the present study. In some studies, the prevalence of delirium in these wards was much higher than the present study. For example, the McNicoll et al. study in the USA reported a prevalence of 31% [Citation63] In a study by Limpawattana et al. in Thailand, it was 44.4% [Citation52,Citation64], in Ely et al. in the USA, it was 81.3% [Citation65], in Thomason et al. in the USA it was 48% [Citation66], in the study by Micek et al., it was 47% [Citation67] and it was 45% in the Roberts study [Citation68]. The difference between Tilouche and colleagues [Citation62] and Ely et al. [Citation65] with the results of the present study can be noted that the study was a cross-sectional descriptive study and examined a specific number of patients with a sample size of 206 and 48 patients. While the present study is a systematic review study with a sample size of 5339 patients, other differences can be noted that in the present study patients in different units have been studied. In the studies mentioned, only patients in the intensive care units have been examined.
One of the strengths of the present study is that the delirium prevalence has been investigated in all parts of the hospital and can provide useful information in this regard. The weaknesses of this study can be attributed to the diversity of studies (considering simple randomized sampling studies), which has led to the creation of heterogeneity. The researcher has analyzed the subgroup to reduce the amount of heterogeneity and provide more accurate findings based on the type of hospitalization. Other strengths of this study are the fact that the delirium prevalence has been studied over a long period of time. In this study, the delirium 18-year prevalence in Iran was studied. One of the weak point of this study is that the same tool was not used to study the delirium prevalence, and the method of conducting studies that make up the review varied.
Due to the fact that the delirium prevalence rate was significant in the study, it is recommended that screening be performed at the beginning of the patient’s arrival in the hospital. After that, nurses will receive the necessary training for each patient. It is also suggested that necessary educational interventions for nurses and nursing students should be made to become acquainted with the importance of delirium and so the necessary measures can be taken to reduce this.
Following on from this paper, it is suggested that global studies should be conducted on the prevalence of delirium in different countries. It is also suggested that the results of the delirium prevalence in Iran be compared with other countries.
Conclusion
The findings show the prevalence of delirium in hospitalized patients in Iran is 21.8% (CI: 17.5–27.5%). Due to the relatively high prevalence of delirium in patients admitted to hospitals in Iran, prevention is necessary to reduce the incidence of delirium.
The present study investigates the prevalence of delirium in patients in Iran.
The findings show the prevalence of delirium in hospitalized patients in Iran is 21.8% (CI: 17.5–27.5%).
The findings show the prevalence of delirium in hospitalized patients in Iran based on the hospitalization in ICU according to the findings is 24.7% (CI: 18.1–32.7%) and in the general ward is 17.5% (CI: 13.6–22.3%).
Due to the relatively high prevalence of delirium in patients admitted to hospitals in Iran, prevention is necessary to reduce the incidence of delirium.
Ethical conduct
Research ethics committee of Kermanshah University of Medical Sciences approved this study with ethics code of IR.KUMS.REC.1397.837.
Financial & competing interests disclosure
This study was approved by Student Research committee of research deputy of Kermanshah University of Medical Sciences, Kermanshah, IR Iran with Grant Number: 30097769. The authors thank the officials of this committee and research deputy. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Additional information
Funding
References
- von GuntenA, MosimannUP, AntoniettiJ-P. A longitudinal study on delirium in nursing homes. Am. J. Geriatr. Psychiatry21(10), 963–972 (2013).
- UrdenLD, StacyKM, LoughME. Thelan’s Critical Care Nursing: Diagnosis and Management. Mosby, MO, USA (2006).
- Van RompaeyB, SchuurmansMJ, Shortridge-BaggettLM, TruijenS, ElseviersM, BossaertL. A comparison of the CAM-ICU and the NEECHAM confusion scale in intensive care delirium assessment: an observational study in non-intubated patients. Crit. Care12(1), R16 (2008).
- JannatiY, SohrabiM, Bagheri-NesamiM. Delirium and its diagnostic tools: a new approach to nursing. Clin. Excellence1(2), 85–96 (2013).
- KhanBA, ZawahiriM, CampbellNL, FoxGC, WeinsteinEJ, NazirAet al.Delirium in hospitalized patients: implications of current evidence on clinical practice and future avenues for research – a systematic evidence review. J. Hosp. Med.7(7), 580–958 (2002).
- ZeighamiR, AlipourHeydari M, BabaeeR. The effect of a multifactorial intervention on the incidence of delirium in cardiac surgery unit. J. Nurs. Educ.3(4), 48–57 (2006).
- ZolfaghariM, ArbabiM, PedramRazi S, BiatK, BaviA. Effectiveness of a multifactor educational intervention on delirium incidence and length of stay in patients with cardiac surgery. J. Hayat.18(1), 67–78 (2012).
- EttemaR, van HartenD, HoogerduijnJ, HoekstraT, SchuurmansM. Nurses opinions regarding delirium care in the older general hospital population and in older cardiac surgery patients specifically: a multicentre survey among Dutch nurses. Int. J. Clin. Exp. Med.5(21), 1352 (2014).
- LuJH, ChanDK, O’RourkeF, OngB, ShenQ, ReutensSet al.Management and outcomes of delirious patients with hyperactive symptoms in a secured behavioral unit jointly used by geriatricians and pyschogeriatricians. Arch. Gerontol. Geriatr.52(1), 66–70 (2011).
- PatersonR, LongD, SchiblerA, DeYoung A, DowB, WarrenJet al.Risk factors for delirium in an Australian paediatric intensive care unit. Australian Crit. Care31(2), 117 (2018).
- LauT, RussellS. A complex case of delirium: from theory to clinical management. In: ShivakumarK, AmanullahS (Eds). Complex Clinical Conundrums in Psychiatry, Springer, Cham, Switzerland (2018).
- Van GoolWA, Vande Beek D, EikelenboomP. Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet375(9716), 773–775 (2010).
- InouyeSK, WestendorpRG, SaczynskiJS. Delirium in elderly people. Lancet383(9920), 911–922 (2014).
- KosarCM, TabloskiPA, TravisonTGet al.Effect of preoperative pain and depressive symptoms on the risk of postoperative delirium: a prospective cohort study. Lancet Psychiatry1(6), 431–436 (2014).
- SchiemannA, HadzidiakosD, SpiesC. Managing ICU delirium. Curr. Opin. Crit. Care17(2), 131–140 (2011).
- CheraghiMA, HazaryanM, BahramnezhadF, MirzaeipourF, HaghaniH. The relationship between pain and the incidence of delirium in patients undergoing cardiac surgery. Med. Surg. Nurs. J.4(3), 43 (2015).
- PieralliF, VannucchiV, ManciniA, GrazziniM, PaolacciG, MorettiniAet al.Delirium is a predictor of in-hospital mortality in elderly patients with community acquired pneumonia. Intern Emerg. Med.9(2), 195–200 (2014).
- BailK, BerryH, GrealishL, DraperB, KarmelR, GibsonDet al.Potentially preventable complications of urinary tract infections, pressure areas, pneumonia, and delirium in hospitalised dementia patients: retrospective cohort study. BMJ Open3(6), e00277 (2013).
- BalasMC, DeutschmanCS, Sullivan‐MarxEM, StrumpfNE, AlstonRP, RichmondTS. Delirium in older patients in surgical intensive care units. J. Nurs. Scholarsh.39(2), 147–154 (2007).
- ZamoscikK, GodboldR, FreemanP. Intensive care nurses’ experiences and perceptions of delirium and delirium care. Intensive Crit. Care Nurs.40, 94–100 (2017).
- InouyeSK, Bogardus JrST, CharpentierPA, Leo-SummersL, AcamporaD, HolfordTRet al.A multicomponent intervention to prevent delirium in hospitalized older patients. N. Engl. J. Med.340(9), 669–676 (1999).
- MarcantonioER, FlackerJM, WrightRJ, ResnickNM. Reducing delirium after hip fracture: a randomized trial. J. Am. Geriatr. Soc.49(5), 516–522 (2001).
- RestonJT, SchoellesKM. In-facility delirium prevention programs as a patient safety strategy: a systematic review. Ann. Intern. Med.158(5 Part 2), 375–380 (2013).
- Adib-HajbagheryM, GhapaniS, PoorabbasiM. The effects of environmental simulation on delirium incidence after coronary artery bypass graft surgery. J. Urmia Nurs. Midwifery Fac.16(5), 303–13 (2018).
- KangJ, LeeM, KoH, KimS, YunS, JeongYet al.Effect of nonpharmacological interventions for the prevention of delirium in the intensive care unit: a systematic review and meta-analysis. J. Crit. Care48, 372–384 (2018).
- KarimiV, HanifiN, BahraminejadN, FaghihzadehS. The effect of family-centered orientation program on prevention of delirium prevalence in patients with coronary artery disease: a clinical trial. Military Caring Sci.2(2), 104–114 (2015).
- JohnsonK, FleuryJ, McClainD. Music intervention to prevent delirium among older patients admitted to a trauma intensive care unit and a trauma orthopaedic unit. Intensive Crit. Care Nurs.47, 7–14 (2018).
- FraserV, CossetteS, MailhotT, BriseboisA, DubéV. Evaluation of an intervention with nurses for delirium detection after cardiac surgery. Worldviews Evid. Based Nurs.15(1), 38–44 (2018).
- NormanSL, TahaAA. Delirium knowledge, self-confidence, and attitude in pediatric intensive care nurses. J. Pediatr. Nurs.46, 6–11 (2019).
- KrewulakKD, StelfoxHT, LeighJP, ElyEW, FiestKM. Incidence and prevalence of delirium subtypes in an adult ICU: a systematic review and meta-analysis. Crit. Care Med.46(12), 2029–2035 (2018).
- FadayomiAB, IbalaR, BilottaF, WestoverMB, AkejuO. A systematic review and meta-analysis examining the impact of sleep disturbance on postoperative delirium. Crit. Care Med.46(12), e1204–e12 (2018).
- PRISMA. PRISMA Checklist. http://prisma-statement.org/PRISMAStatement/Checklist.aspx
- GheshlaghRG, EbadiA, DalvandiAet al.The relationship between mental health and resilience: a systematic review and meta-analysis. Iran Red Crescent Med. J.19(6), e13537 (2017).
- HoodinF, WeberS. A systematic review of psychosocial factors affecting survival after bone marrow transplantation. Psychosomatics44(3), 181–195 (2003).
- TsimicalisA, StinsonJ, StevensB. Quality of life of children following bone marrow transplantation: critical review of the research literature. Eur. J. Oncol. Nurs.9(3), 218–238 (2005).
- GhaneiGheshlagh R, NazariM, BaghiV, DalvandS, DalvandiA, SayehmiriK. Underreporting of needlestick injuries among healthcare providers in Iran: a systematic review and meta-analysis. J. Hayat.23(3), 201–213 (2017).
- JanatiY, BagheriNM, SohrabiM, YazdaniCJ, MazdaraniS. Factors associated with post-surgical delirium in patients undergoing open heart surgery. Oman Med J.9(5), 340–345 (2014).
- JodatiA, SafaieN, RaoofiMet al.Prevalence and risk factors of postoperative delirium in patients undergoing open heart surgery in northwest of Iran. J. Cardiovasc.Thorac. Res.5(3), 97–99( 2013).
- ModaberniaM, ForghanParast K, KhalkhaliS, NajafiK. Delirium in CCU. J. Guilan Univ. Med. Sci.11(41), 1–6 (2002).
- BagheriK, HonarmandA, HosseiniMSJ. Association of mean arterial pressure during cardiopulmonary pump and incidence of delirium after coronary artery bypass graft surgery. 35(449), 1358–1363 (2017).
- CheraghiMA, HazaryanM, BahramnezhadF, MirzaeipourF, HaghaniH. Study of the relationship between sleep quality and prevalence of delirium in patients undergoing cardiac surgery. Health Sci.5(9S), 38–43 (2016).
- AsaeeR, NasariH, HoseiniS. Prevalence of delirium in hospitalized internal medicine and surgical adult patients in Shohadaye ashayer hospital of Khoram abad. Yafteh10(3), 21–27 (2008).
- HosseiniF, ShajariA, HosseiniBS. Investigation of the frequency of delirium in different departments in the Yazd Shohadaye Kargar Hospital. SSU J.24(8), 640–648 (2016).
- HeidariA, DianatiM, MousaviG. Prevalence of delirium, its related factors and short-term outcomes in ICU wards of Kashan Shahid-Beheshti and Isfahan Kashani hospitals during 2012–2013. Feyz J. Kashan Univ. Med. Sci.18(1) 76–84 ( 2014).
- RajabpourNikfam M, GhanbariKhanghah A, KhaleghdoostMohammadi T, KazemnezhadLeili E, AshrafA. Study of predictors of delirium incidence in hospitalized patients in intensive care units. J. Holistic Nurs. Midwifery26(3), 25–35 (2014).
- Eizadi-MoodN, AghadavoudiO, NajarzadeganMR, FardMM. Prevalence of delirium in opium users after coronary artery bypass graft surgery. Int. J. Prev. Med.5(7), 900 (2014).
- HosseiniSH, MortazaviM. Frequency of referral rate and psychiatric diagnoses in Sari Imam Khomeini Hospital during 2008 and 2009. J. Mazandaran Univ. Med. Sci.20(80), 63–68 (2011).
- ShadvarK, BaastaniF, MahmoodpoorA, BilehjaniE. Evaluation of the prevalence and risk factors of delirium in cardiac surgery ICU. J. Cardiovasc. Thorac. Res.5(4), 157 (2013).
- SalariA, HasandokhtT, DadkhahTirani H, NourisaeedA, JavadzadehMoghtader A. The incidence of delirium after heart bypass surgery in patients with preoperative anxiety and depression. J. Guilan Univ. Med. Sci.26(101), 36–45 (2017).
- RadM, MohammadiN, SeyyedshohadaeeM, HaghaniH. Relationship of blood transfusion and CPB with delirium. 20(5), 801–807 (2014).
- BeiranvandA, FallahiKhoshkneb M, AshayeriH, RahgozarM. Comparison between prevalence of delirium after hip surgery and general surgery in hospitalized female elderly. Geriatric Nurs.1(1), 83–93 (2014).
- RezvaniM, AlikiaiiB, RamezaniS. The relationship of erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP) with an uncertain prognosis for the patients admitted to the intensive care unit in Alzahra hospital, Isfahan, Iran, during 2014–2015. 34(391), 835–840 (2016).
- MohammadiM. Epidemiology of psychiatric disorders in West Azarbaijan Province (2001). Urmia Med. J.14(4), 9–15 (2003).
- HassaniE, MahooriA, NorooziniaH, MehdizadehH, SepasiN. Evaluation of risk factors for adverse neurologic outcome after cardiac surgery. Urmia Med. J.21(2), 249–253 (2010).
- GanavatiA, ForoughiM, EsmaeiliS, HasantashS, BolourainA, ShahzamaniMet al.The relation between post cardiac surgery delirium and intraoperative factors. Irnanian J. Surg.1716–25 (2009).
- TashakoriA. Comparison of the incidence of postoperative delirium in patients with open heart surgery and general surgery in Ahvaz Golestan Hospital in 1999. Jundishapur Sci. Med. J.41(41), 37–43 (1999).
- HatefiBadfarGShohaniM NasirkandyMet al.Epidemiology of hepatitis B in pregnant Iranian women: a systematic review and meta-analysis. Arch. Virol.24163(32), 1319–330 (2019).
- JouybariL, HosseiniSFH, GhanaS, SaeediS, SanagooA. The incidence of delirium in patients after surgery in recovery room. Jorjani1(1), 23–29 (2012).
- GleasonLJ, SchmittEM, KosarCM, TabloskiP, SaczynskiJS, RobinsonTet al.Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg.150(12), 1134–1140 (2015).
- MarcantonioER. Delirium in hospitalized older adults. N. Engl. J. Med.377(15), 1456–1466 (2017).
- ColletMO, CaballeroJ, SonnevilleR, BozzaFA, NydahlP, SchandlAet al.Prevalence and risk factors related to haloperidol use for delirium in adult intensive care patients: the multinational AID-ICU inception cohort study. Intensive Care Med.44(7), 1081–1089 (2018).
- TiloucheN, HassenMF, AliHBS, JaouedO, GharbiR, ElAtrous SS. Delirium in the intensive care unit: incidence, risk factors, and impact on outcome. Indian J. Crit. Care Med.22(3), 144 (2018).
- McNicollL, PisaniMA, ZhangY, ElyEW, SiegelMD, InouyeSK. Delirium in the intensive care unit: occurrence and clinical course in older patients. J. Am. Geriatr. Soc.51(5), 591–598 (2013).
- LimpawattanaP, PanitchoteA, TangvoraphonkchaiK, SuebsohN, EammaW, ChanthonglarngBet al.Delirium in critical care: a study of incidence, prevalence, and associated factors in the tertiary care hospital of older Thai adults. Aging Ment. Health20(1), 74–80 (2016).
- ElyE, GautamS, MargolinR, FrancisJ, MayL, SperoffTet al.The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med.27(12), 1892–1900 (2016).
- ThomasonJW, ShintaniA, PetersonJF, PunBT, JacksonJC, ElyEW. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit. Care9(4), R375 (2005)
- MicekST, AnandNJ, LaibleBR, ShannonWD, KollefMH. Delirium as detected by the CAM-ICU predicts restraint use among mechanically ventilated medical patients. Crit. Care Med.33(6), 1260–1265 (2005).
- RobertsB, RickardCM, RajbhandariDet al.Multicentre study of delirium in ICU patients using a simple screening tool. Australian Crit. Care.18(1), 6–16 (2018).