Abstract
A new hypervirulent variant of Klebsiella pneumoniae has emerged. In contrast to classic Klebsiella pneumoniae, it can cause serious and life-threatening infection. It has the ability of spreading from the gastrointestinal and genitourinary systems in non immunocompromised patients to the liver, lung, brain and the eye. High morbidity and mortality have been reported especially if there is a CNS involvement. A prompt search for a distant infective metastasis and its early treatment can improve the outcome. This is a report of a patient presenting with delayed obstructive hydrocephalus secondary to an obstructive urosepsis.
A new hypervirulent variant of Klebsiella pneumoniae (hvKP) has emerged over last few years initially in the Asian Pacific Rim and it is being increasingly reported in Western countries. In contrast to classic K. pneumoniae, it can cause serious, life-threatening community-acquired infections in younger healthy hosts presenting with liver abscess, pneumonia, meningitis and endophthalmitis. It can also spread from the gastrointestinal and genitourinary systems in the non immunocompromised patients. This is unusual for an enteric Gram-negative Bacilli [Citation1].
This new variant named hypermucoviscous K. pneumoniae as it shows a so called positive ‘string test’ in the laboratory. The string test is considered positive when a bacteriology inoculation loop or needle is able to generate a viscous string >5 mm in length by stretching bacterial colonies on an agar plate [Citation1].
The infection with hvKP has a high morbidity and mortality rate, with mortality rates ranging from 3 to 42%. The CNS involvement has a reported mortality ranging from 38 to 91% [Citation1,Citation2].
This report documents a patient who developed delayed obstructive hydrocephalus secondary to a hvKP ventriculitis in the context of an obstructive urosepsis. This is the first such report.
Case report
An 80-year-old immunocompetent female was admitted with the left lower quadrant abdominal pain and fever on a background of known kidney stone. She was diagnosed with obstructive urosepsis. She underwent cystoscopy and insertion of a ureteric stent.
K. pneumoniae was grown in the urine and blood cultures with a positive ‘string test’. She was commenced on piperacillin-tazobactam 4.5 g intravenously (iv.) 8 hourly. On the third day of admission, she became confused but was able to open her eyes spontaneously and obey commands (E4, M6, V4 as per Glascow Coma Scale). A CT scan of the brain was normal.
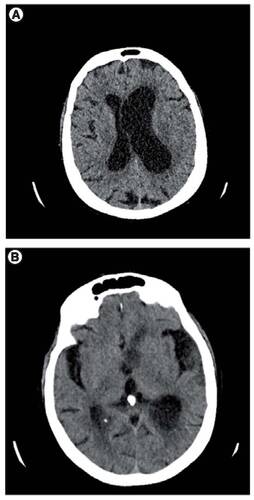
During next few days, she continued to deteriorate and remained febrile. Another cystoscopy was performed to remove the renal stone and the ureteric stent was replaced. Postoperatively, she improved clinically but remained confused (E4M6V4). Her iv. antibiotic was changed to oral amoxicillin and clavulanate. She also had a trial of acyclovir for a possibility of Herpes simplex virus CNS infection even though the infectious disease team were not convinced this was necessary. Around 2 weeks into her admission while being on oral antibiotic for past 3 days, she deteriorated again to a stage that her best motor response was localizing the pain with her eyes only opening to a painful stimulus. She was confused with an inappropriate verbal response (E2, V3, M5 as per Glascow Coma Scale). During her physical examination, a right sided hemiparesis was noted. A repeat CT scan of the brain showed asymmetrical hydrocephalus with layering of debris within the occipital horns indicating ventriculitis ().
(A) Showing prominence of the ventricles with marked asymmetrical dilatation of the left lateral ventricle. (B) Layering of debris within the occipital horns.
Following the neurosurgical consultation, a left frontal external ventricular drain (EVD) was inserted uneventfully. Postoperatively, she improved and she was commenced on ceftriaxone iv. cerebrospinal fluid (CSF) analysis showed elevated white cell count and protein level in favor of a bacterial infection. No microorganism was grown on CSF culture and the viral PCR was negative.
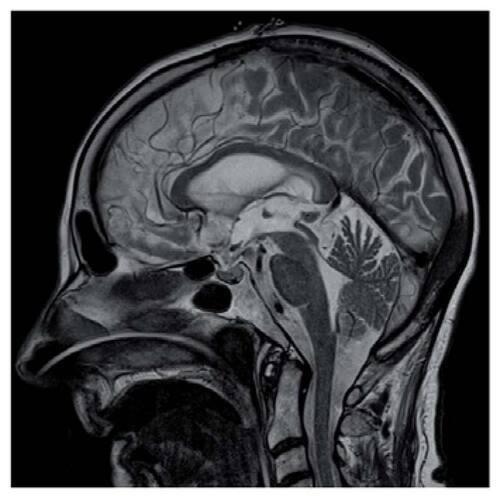
Subsequent MRI brain confirmed features of ventriculitis with abnormal enhancement and inflammatory debris within the occipital horns of lateral ventricles bilaterally (). A web in the cerebral aqueduct was thought to be secondary to the ventriculitis ().
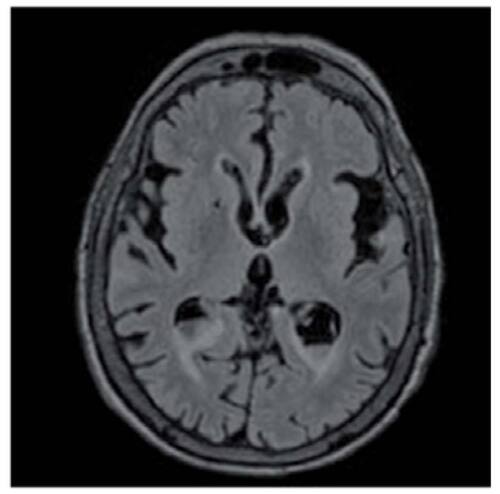
The EVD was removed after 2 weeks without any need for a CSF diversion intervention like insertion of a ventriculoperitoneal shunt. She remained GCS 14 without any neurological deficits for the rest of admission and was diagnosed with hypoactive delirium and transferred to a rehabilitation center. On outpatient review after 6 weeks, she was GCS 15 without any neurological deficits. All the imaging changes in favor of ventriculitis (lateral ventricles ependymal enhancement and debris) were resolved on the follow-up MRI.
Discussion
K. pneumoniae is a common cause of healthcare associated infections including pneumonia, urinary tract infections and bloodstream infections. Unlike the classic K. pneumoniae, the new hvKP is infecting healthy people in community settings and causing severe infections and has the potential to spread to other organs causing metastatic infective sources including pyogenic liver abscess, endophthalmitis and meningitis [Citation3,Citation4]. The CNS involvement is considered to have a very high mortality rate [Citation5]. Concerning this new variant’s CNS infection, there have been relatively few reports [Citation3,Citation6].
This new phenotype has been determined to be conferred by two genes: RmpA, which regulates capsule production [Citation1] and MagA, which is associated with the hypermucoviscous phenotype [Citation7]. These genes encoding are considered virulence factors [Citation4]. Capsule types K1 and K2 are also highly associated with hvKP and may play a more significant role in virulence than RmpA and MagA [Citation4,Citation8].
Hyun et al.l reported a metastatic CNS infection with K. pneumoniae renal abscess in a diabetic patient who developed seizure-like activity during admission in context of a renal abscess. In contrast to our case, they could not successfully perform the drainage of the infective source due to inadequate liquefaction of the abscess at the time of admission and only proper antibiotics have been commenced according to in vitro susceptibility [Citation6]. Another point worth mentioning is the delayed presentation of ventriculitis in our case report. Our patient developed clinical and radiological features of ventriculitis 14 days into her admission versus day 6 for the patient in their study.
In our patient, we are assuming that there was a case of hvKP as a hypermucoviscous K. pneumoniae was cultured from the primary site with positive ‘string sign’. Presumably, the CSF microbiological cultures were negative because she had been on the proper antibiotic therapy for nearly 2 weeks prior to CSF sampling. However, the clinical and radiological findings would strongly support a diagnosis of hvKP, given that classic Klebsiella does not behave in this fashion.
Mainstay of treatment is the antimicrobial therapy and the drainage of abscesses/closed space infections for source control and optimal outcome [Citation1,Citation9]. We used proper antibiotic according to in vitro sensitivity and performed a prompt EVD insertion. The early invasive treatment in our patient resulted in a favorable outcome.
This case serves to highlight the importance of clinical awareness of the possibility of CNS involvement in patients with known hvKP infection. Once a patient develops clinical signs, early surgical intervention may be required to prevent disease progression.
Although it has emerged in the Asian Pacific Rim, now increasingly being recognized in Western countries and requires western physicians to be more vigilant of this new hypervirulent variant and to look for distant metastatic infective source as soon as this variant has been isolated from a culture.
Conclusion
It is important that clinicians to be aware of the new hvKP because it can spread to other organs and cause life-threatening infections, including liver abscess, pneumonia, meningitis and endophthalmitis with distant infective metastasis. It should prompt a search for other sites of infection whenever this microorganism is grown on culture.
Prompt treatment which includes the antibiotic therapy with/without surgical drainage may improve outcome.
Future perspective
Clinicians in Western countries are less aware of the emergence of the new hvKP which let the pathogen follow its course and spread to other organs prior to being detected which may lead to less favorable outcome even with the appropriate treatment. This case report can increase the vigilance of clinicians about this pathogen and help them to detect distant infective metastasis of this new strain at the earliest time to prevent high rate of morbidity and mortality related to it.
A new hypervirulent variant of Klebsiella pneumoniae has emerged with capacity to spread from the gastrointestinal and genitourinary systems in non immunocompromised patients.
High morbidity and mortality have been reported especially if there is CNS involvement.
Hydrocephalus can be a delayed presentation of its CNS involvement.
Western physicians should be more vigilant of this new hypervirulent variant and to look for distant metastatic infective source as soon as this variant has been isolated from a culture.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Informed consent disclosure
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
References
- ShonAS, BajwaRPS, RussoTA. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae. Virulence4(2), 107–118 (2013).
- TangLM, ChenST, HsuWC, ChenCM. Klebsiella meningitis in Taiwan: an overview. Epidemiol. Infect.119(2), 135–142 (1997).
- JungJ, JangY, ChoiG, MinKW, HanK, ParkJ. A case of renal abscess associated with endogeneous endophthalmitis and septic pulmonary embolism by Klebsiella pneumoniae. Infect. Chemother.43(6), 485–489 (2011).
- MartinRM, BachmanMA. Colonization, infection, and the accessory genome of Klebsiella pneumoniae. Front. Cellular Infect. Microbiol.8, 4 (2018).
- LiliangPC, LinYC, SuTMet al.Klebsiella brain abscess in adults. Infection29(2), 81–86 (2001).
- HyunJI, KimYJ, JeonYHet al.A case of ventriculitis associated with renal abscess caused by serotype K1 Klebsiella pneumoniae. Infect. Chemother.46(2), 120–124 (2014).
- YuWL, KoWC, ChengKCet al.Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin. Infect. Dis.42(10), 1351–1358 (2006).
- YehKM, KurupA, SiuLet al.Capsular serotype K1 or K2, rather than magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae liver abscess in Singapore and Taiwan. J. Clin. Microbiol.45(2), 466–471 (2007).
- LeeTH, ChangWN, SuTMet al.Clinical features and predictive factors of intraventricular rupture in patients who have bacterial brain abscesses. J. Neurol. Neurosurg. Psych.78(3), 303–309 (2007).