Abstract
Background. Outsourcing radiological examinations from public university hospitals affects the patient, who has to attend a different clinic or hospital for the radiological examination. We currently have a limited understanding of how patients view outsourcing and their care related to MR examinations.
Aim. To examine the experiences of patients who are sent to private radiology units when their referrals for MR examinations are outsourced from a university hospital, as well as to explore factors which influence patient satisfaction regarding the quality of care related to the MR examination.
Methods. A group of patients (n = 160) referred for MR examinations and either examined at a university hospital or at an external private unit were interviewed. The interview was designed as a verbal questionnaire. Data were analyzed using Student’s t test, analysis of variance (ANOVA), and Pearson’s correlation.
Results. Sixty-nine percent of the patients could neither choose nor influence the location at which they were examined. For those who could, aspects that influenced the patient’s choice of radiology department were: short waiting time 79% (127/160), ease of traveling to the radiology department 68% (110/160), and short distance to their home or work 58% (93/160). For 40% (60/160) of the patients, a short time in the waiting room was related to a positive experience of the MR examination.
Conclusion. If patients were informed about outsourcing and could also choose where to have their examination, key factors contributing to patient satisfaction could be met even when MR examinations are outsourced.
Introduction
About 60 million magnetic resonance (MR) examinations are performed annually worldwide (Citation1), and numbers have increased over recent years. The ability of magnetic resonance imaging (MRI) to provide high soft-tissue contrast resolution images without ionizing radiation is important for many diagnoses, and this contributes to the modality being highly coveted (Citation2). According to a report on the Census of the Radiology Workforce in the UK in 2008, 18% of radiology clinics outsourced a number of radiological imaging procedures, the median of the requested MR examinations being 49% (Citation3). In Sweden, increased demand for MR examinations has resulted in longer waiting times for these examinations. In this setting, many public hospitals in Sweden outsource a proportion of their referrals for radiological examinations, including MR examinations, to external hospitals or units, usually private radiology departments. Outsourcing radiological examinations from a university hospital to external private units affects the patient, who has to attend a different clinic or hospital for the radiological examination. We currently have a limited understanding of how patients feel when their MR examination is outsourced and how they view the quality of their care related to these examinations.
The aim of this study was to examine the patients’ reactions about being sent to private radiology units when their referrals for MR examinations are outsourced from a university hospital, as well as to explore factors which influence patient satisfaction regarding the quality of care related to the MR examination.
Material and methods
This study was conducted at the two private radiological units that received most outsourced referrals and at Karolinska University Hospital in Stockholm, Sweden. A total of 160 patients who were referred for MR examinations, either to the Karolinska University Hospital or to external private units, were interviewed over a two-month period. The interviews took place in the radiology departments just after the patients had completed their MR examination. For practical reasons, the interviews were scheduled on three days per week over a two-week period in each radiology department: Monday, Tuesday, and Wednesday during the first week, and Wednesday, Thursday, and Friday during the second week. Sixty patients at each private unit and 40 patients at the University Hospital were interviewed. The average duration of each interview was 20 min. Participation was voluntary, and all informants were free to make an independent decision about taking part in the study. Each patient gave consent verbally before the interview. All participants were verbally informed about the overall purpose of the research and its main features. All participants were ensured confidentiality about their identity and were also informed that the data from the interviews would only be used in this study for the purpose of providing knowledge through understanding their experience. Data were collected by one of the researchers (P.T.O.). The project in its entirety was approved as quality assurance by the Regional Ethical Review Board at the Karolinska Institute.
The interview had a structured design which consisted of alternative questions and a few open-ended questions (Citation4). The interview questions also included background questions, which sought to obtain patient socio-demographic data, such as age, education level, occupation, and physical and psychological well-being. The remaining questions were divided into a number of domains concerning patients’ expectations of care such as: the caring attitude of the staff, waiting time, availability, and the patient’s freedom of choice regarding selection of radiology clinic. These questions were based on two criteria: comprehensiveness and importance, e.g. each question regarding health care experiences and related to the MR examination was followed by a question about the importance of the question (Citation5). The interview consisted of 34 questions of which 10 questions were follow-up questions. In these follow-up questions patients were asked to indicate on a five-point scale (a = 5, of greatest importance; b = 4, of great importance; c = 3, of little importance; d = 2, of no importance; e = 1, cannot take a position on the issue) how important they considered the subject. Degree of perceived satisfaction was measured on a five-point scale: E = 1, very bad; D = 2, bad; C = 3, neither good nor bad; B = 4, good; and A = 5, very good. Degree of information quality was also measured on a similar five-point scale. Degree of access, including waiting times for radiological examinations, was measured on a five-point scale: E = 1, do not know; D = 2, three months or more; C = 3, one to two months; B = 4, one to four weeks; and A = 5, less than a week. Degree of satisfaction regarding the staff at the radiology department where the patients had their MR examinations was assessed on a three-point scale: 1 = do not know; 2 = no; and 3 = yes. In total, 20 of the items about patient experiences had a five-point response scale, three had a four-point scale, and seven questions hade a three-point scale (see Appendix).
Analysis
Statistical analyses were carried out using SPSS software, version 20. The patients’ satisfaction with their care was calculated by the mean satisfaction scores in each dimension, compared with patient characteristics using Student’s t test and ANOVA to compare differences between independent and dependent variables, as appropriate. Correlations were analyzed by Pearson’s test, where satisfaction was defined for p < 0.05.
Analysis of the text from open-ended questions proceeded as follows. In order to pick up relevant information, only those sentences in the responses that were clear and created context were transcribed. The data were organized in a commonly used spreadsheet format with Microsoft Office Excel 2010 11.6560.6568 SP3 software by Microsoft® and Microsoft Word 2010 (Citation6,7). Two questions guided analysis of these responses. First, what specific aspects of care or outsourcing MR examinations are the interview texts discussing? Second, what are the issues regarding care or outsourcing MR examinations that are of concern to the patients interviewed? In order to identify common themes each response was read carefully. The second step was to develop coding categories for each response. Data were organized through coding categories so that text providing similar context on a given theme could be separated from the other data. The third step was labeling each response with one or several coding categories. The final step was to find out what categories were related to each other and to identify the common theme. The most common types of coding categories that emerged in this study were: codes of situation (which define a setting: for example, patients’ views on the staff’s work) and codes of activity (related to commonly occurring varieties of behavior: for example, patients’ visits to the radiology department). A total of four themes emerged: Quality of patient care, Office waiting time, Choice of radiology department, and Improvement of the patient’s satisfaction.
Results
Of the 160 patients who participated in this study, 67 were men and 93 were women, between 18 and 81 years old (median age for men was 43, and for women 61). also shows the other characteristics of the socio-demographic background of the patients interviewed, such as education and occupational status.
Table I. Socio-demographic characteristic background of the patients interviewed.
Thirty-three patients (20.6%) considered their physical health to be very good; 71 (44.4%) good; 28 (17.5%) neither good nor bad; 27 (17%) bad; and 1 (0.6%) very bad. Sixty-four patients (40%) judged their psychological health to be very good; 72 (45%) good; 10 (6.3%) neither good nor bad; 9 (5.6%) bad; and 5 (3.1%) very bad.
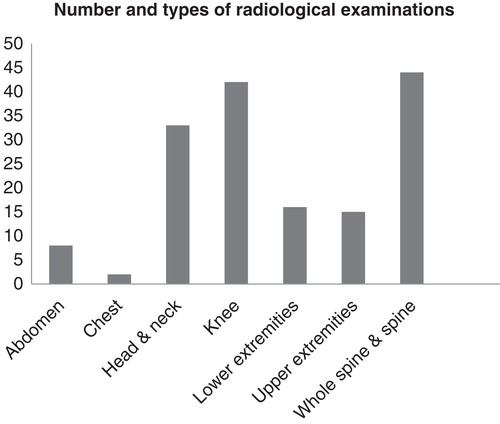
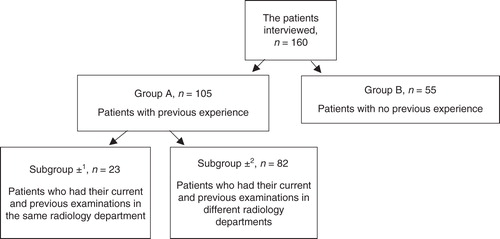
The most common MR examinations the patients had undergone were those of the knee or spine, which together constituted 58% of the examinations (). Two different groups of patients were separated in the analysis: those who had previously had an MR examination (Group A, n = 105; 66%) and those who had not (Group B, n = 55; 34%). Group A consisted of two smaller subgroups, namely patients who had both their current and previous MR examinations in the same radiology department (Subgroup α1, n = 23; 14%) and patients who had their previous and current MR examinations in different radiology departments (Subgroup α2, n = 82; 51%) ().
Figure 2. Number of patients interviewed, stratified according to previous experience and radiology department.
Patients’ satisfaction and the caring attitude of the staff
Based on the result of this study, patients’ satisfaction levels with the four dimensions of care quality (information given by radiology staff, communication between the staff and patients, level of expertise, and caring attitude of the staff) are presented in . The majority of the patients were very satisfied with the amount of information given by the radiology staff. This included both written and oral information in 64/160 (40%), radiographers’ communication skills in 94/160 (58.8%), perceived level of expertise in 142/160 (88.8%), and the staff’s caring attitude 145/160 (90.6%). Fifty-nine percent (94/160) of the patients answered that the attitude of the staff was of major importance, 40% (64/160) of great importance, and 1% (2/160) of no importance. In general, the majority of patients, 146/160 (91%), were very satisfied with their care during their visit to a radiology department, while others, 14/160 (9%), were quite satisfied. Fifty-three percent (84/160) believed this point was of major importance, 44% (70/160) of great importance, 2% (4/160) of no importance, and 1% (2/160) could not take a position.
Table II. Patients’ level of satisfaction within four dimensions of assessment of care quality.
Sixty-six patients (41.2%) who were dissatisfied with radiographers’ communication skills were of the opinion that radiographers’ communication during the performance of MR examinations is very important and necessary in order to increase the patient’s sense of security.
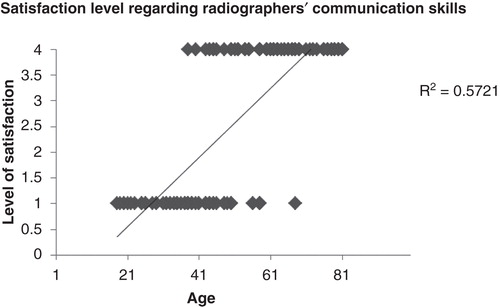
Patient satisfaction regarding the staff’s ability to provide care, the quality and amount of information, and patient age were inversely related. Radiographers’ communication skills were significantly lower according to reports from patients between 18 and 58 years old (mean age = 34.8) than from patients between 45 and 81 years old (mean age = 68) ().
Figure 3. Satisfaction with the radiographers’ communication skills and patient age was correlated at the level of about r = 0.76 and R2 = 0.57.
Patients in both groups (A and B) reported high satisfaction relative to their MR examination. No significant correlations were found between satisfaction and patient age or gender.
Waiting time including office waiting time
Twenty-nine percent (46/160) of the patients had waited less than one week between their referral and the MR examination; 60% (96/160) between one and four weeks; 6% (10/160) between one and two months; 2% (3/160) had waited three months or more; and 3% (5/160) did not know their waiting time. When patients were asked what an acceptable waiting time for an MR examination would be, 23.1% (37/160) answered less than one week; 64.4% (103/160) one to four weeks; 9.4% (15/160) one to two months; and 3.1% (5/160) did not have an opinion. The reported acceptable waiting time was significantly (p < 0.001) lower among the patients between 18 and 38 years old than among the patients between 48 and 81 years old who specified that an acceptable waiting time was between one and four weeks. The age of the 15 patients who reported that it was acceptable to wait one to two months for an MR examination was between 69 and 81 years old.
For 40% (64/160) of the patients, a short time in the waiting room was related to a positive response regarding returning for a further MR examination.
Choice of radiology department and patients’ freedom of choice
When patients were asked whether they could choose or influence where their MR examination would be performed, 27.5% (44/160) of the patients answered yes; 69.4% (111/160) answered no; and 3.1% (5/160) replied partly. When patients were asked how important this freedom of choice was, 23.1% (37/160) replied that it was of major importance; 30% (48/160) of great importance; 24.3% (39/160) of little importance; 11.3% (18/160) of no importance; and 11.3% (18/160) had no opinion on the issue. Ninety of the patients in this study (56.3%) believed that it was their physician who decided where their MR examination should be performed.
Aspects that influenced the patient’s choice of radiology department were: short waiting time 79.4% (127/160); ease of traveling to the radiology department 68.8% (110/160); and short distance to their home or work 58% (93/160).
Improvement of the patients’ satisfaction
Forty-eight percent (77/160) of the patients suggested that better information about the examination would increase their satisfaction related to the MR examination, and 52% (83/160) desired more instructions during the procedure.
Discussion
The main finding of this study is that the majority of patients referred for an MR examination (140/160; 91%) were satisfied with the level of care that they received in the radiology department, whether it was the one in the university hospital or the external caregiver, indicating that the patients’ perception was that they received the same level of care at either public or private radiology departments.
Fifty-six percent of the patients (90/160) believed that it was their referring physician who decided where the MR examination should be performed. It is natural that the patients, being unaware of the hospital’s policies, generally expect the referring physician to take on the role of decision-maker (Citation8). In reality, this decision is made in the radiology department and depends mostly on the inflow of referrals. The physician is the closest link between the patient and radiology. Although radiologists play a crucial role in patients’ health, they are invisible to patients (Citation9) and are not perceived as decision-makers in the health care process.
Sixty percent of the patients in this study waited between one and four weeks from when their referrals were written until the MR examinations were performed, and 65% of the patients regarded that as acceptable. This indicates that radiology departments within university hospitals and private radiology units are, together, meeting the patients’ expectations fairly well.
Results showed that older patients were generally more satisfied with the staff’s ability to communicate, including the quality and amount of information they received. It is important to note that the nature of expectations could be different between older and younger patients, as well as between those patients who had previously had an MR examination versus those undergoing one for the first time (Citation10). Satisfaction with care usually arises when there is no discrepancy between patients’ expectations and the care received (Citation11).
According to the results of this study, more instructions during MR examinations and better information about the examination itself would increase patients’ satisfaction relative to the MR examination. One definite way to increase patient satisfaction is to focus on the patients’ views about the care they receive and their expectations of it (Citation12).
The advantage of using structured interviews, i.e. the verbal questionnaire, was that the questions could be clarified for the informants if necessary. This diminished the risk of collecting an incorrect response or partial non-response. We believe that a written questionnaire would have been of limited use in this study, because of the chance that patients would fail to recall situations.
Both alternative questions and open-ended questions were used in the interview. The goal was to attract the strengths and minimize the limitations of the quantitative and qualitative analyses (Citation13). We believe that the combination of quantitative and analytical open-ended questions followed by text analyses provides a better understanding of patients’ expectations, satisfaction, and communication about outsourcing their MR examination, because the experience of satisfaction cannot be measured fully by statistical methods alone. But this study also has several limitations to consider. The interviews may result in a biased sample by attracting respondents who could or were willing to participate. The result showed high satisfaction with the patient care, which could be caused by the fact that displeased patients did not participate (Citation14). For this reason, we may not be able to generalize the results. Despite this, we believe that this study could be of interest to other public hospitals which choose outsourcing as one solution for making their radiology departments more efficient. Another limitation in this study is that we studied those dimensions of care quality during MR examinations that were most related to patient nursing. However, the quality of care related to MR examinations involves other factors, such as the radiologist’s level of expertise, work experience, knowledge, work-load pressure, as well as work satisfaction, all of which may have a major impact on the quality of the interpretation. Indeed these factors should be studied further. Patients undergoing MR examinations usually come into contact with radiographers but they seldom have direct contact with radiologists (Citation15).
In conclusion, the patients interviewed in this study were unaware of the university hospital’s policy regarding the outsourcing of MR referrals. When considering outsourcing, the patients’ desires and requirements regarding information must be considered. If this information is adequate, patients are likely to feel that they have experienced a high level of care irrespective of whether their MR examination is outsourced or not. Ways to improve communication between patients and the referring physicians regarding their radiological examinations should be studied further.
Appendix
Download MS Word (38.2 KB)Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sutton R, Kanal E, Wilkoff BL, Bello D, Luechinger R, Jenniskens I, et al. Safety of magnetic resonance imaging of patients with a new Medtronic EnRhythm MRI SureScan pacing system: clinical study design. Trials. 2008;9:68.
- Götte MJ, Rüssel IK, de Roest GJ, Germans T, Veldkamp RF, Knaapen P, et al. Magnetic resonance imaging, pacemakers and implantable cardioverter-defibrillators: current situation and clinical perspective. Neth Heart J. 2010;18:31–7.
- The Royal College of Radiologists. Teleradiology and outsourcing census. London: The Royal College of Radiologists; 2010. Available at http://www.rcr.ac.uk/docs/radiology/pdf/BFCR(10)8_Teleradiology_census.pdf. Accessed 9 Apr 2012.
- Kirk SA, Reid WJ. Science and social work: a critical appraisal. New York: Columbia University Press; 2002.
- Wilde-Larsson B, Larsson G. Development of a short form of the Quality from the Patient’s Perspective (QPP) questionnaire. J Clin Nurs. 2002;11:681–7.
- Morgan DL. Qualitative content analysis: a guide to paths not taken. Qual Health Res. 1993;3:112–21.
- Mossholder KW, Settoon RP, Harris SG, Armenakis AA. Measuring emotion in open-ended survey responses: an application of textual data analysis. J Manage. 1995;21:335–55.
- Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients’ desire for autonomy: decision-making and information-seeking preferences among medical patients. J Gen Intern Med. 1989;4:23–30.
- Margulis AR, Sostman HD. Radiologist-patient contact during the performance of cross-sectional examinations. J Am Coll Radiol. 2004;1:162–3.
- Shikiar R, Rentz AM. Satisfaction with medication: an overview of conceptual, methodological, and regulatory issues. Value Health. 2004;7:204–15.
- Auquier P, Pernoud N, Bruder N, Simeoni MC, Auffray JP, Colavolpe C, et al. Development and validation of a perioperative satisfaction questionnaire. Anesthesiology. 2005;102:1116–23.
- Scardina SA. SERVQUAL: a tool for evaluating patient satisfaction with nursing care. J Nurs Care Qual. 1994;8:38–46.
- Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educ Res. 2004;33:14–26.
- Kinnersley P, Egbunike JN, Kelly M, Hood K, Owen-Jones E, Button LA, et al. The need to improve the interface between in-hours and out-of-hours GP care, and between out-of-hours care and self-care. Fam Pract. 2010;27:664–72.
- Camponovo EJ. Radiologist-patient contact: a different perspective. J Am Coll Radiol. 2004;12:998–9. author reply 1000 Comment on Radiologist-patient contact during the performance of cross-sectional examinations. J Am Coll Radiol. 2004.