Abstract
Background. Studies about work stress and the risk of coronary heart disease (CHD) have yielded inconsistent results. This meta-analysis aimed to investigate the association between job strain and the risk of CHD.
Methods. We searched PubMed and Embase databases for studies reporting data on job strain and the risk of CHD. Studies were included if they reported multiple-adjusted relative risk (RR) with 95% confidence interval (CI) with respect to CHD from job strain.
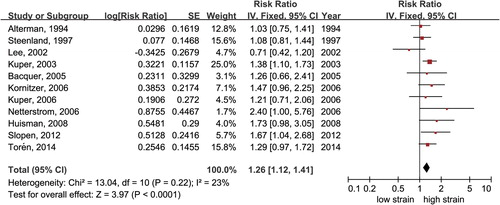
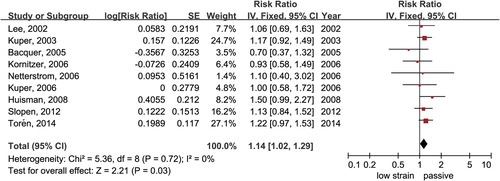
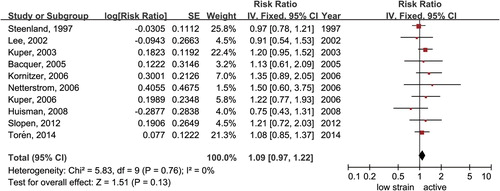
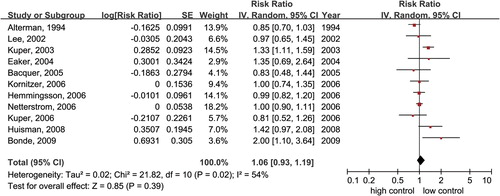
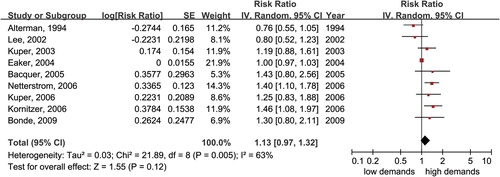
Results. Fourteen prospective cohort studies comprising 232,767 participants were included. The risk of CHD was increased in high-strain (RR 1.26; 95% CI 1.12–1.41) and passive jobs (RR 1.14; 95% CI 1.02–1.29) but not in active jobs (RR 1.09; 95% CI 0.97–1.22), when compared with low-strain group. The increased risk of CHD in high-strain and passive jobs was mainly driven by studies with a follow-up duration of ≥ 10 years. Neither the low-control (RR 1.06; 95% CI 0.93–1.19) nor high-demand (RR 1.13; 95% CI 0.97–1.32) dimension was independently associated with the risk of CHD.
Conclusions. Individuals with high-strain and passive jobs were more likely to experience a CHD event. Intervention programs incorporating individual and organizational levels are crucial for reducing job strain and the risk of CHD.
The Demand-Control Model divides the job strain into four categorical quadrants: high-strain, active, passive, and low-strain.
The risk of coronary heart disease was increased in high-strain and passive jobs but not in active jobs.
Intervention programs incorporating individual and organizational levels are crucial for reducing job strain and the risk of CHD.
Introduction
Extensive research has provided evidence that psychosocial stressors can increase the risk of cardiovascular disease (CVD), including hypertension (Citation1), coronary heart disease (CHD) (Citation2), arrhythmia (Citation3), and stroke (Citation4). The association between job strain and CVD has been investigated since the introduction of the Demand-Control Model (DCM), a two-dimensional model for work characteristics that considers psychosocial job control and demands (Citation5). By combining the characteristics of job control and job demands, DCM divides the work stress characteristics into four categorical quadrants: high-strain (low control, high demands), active (high control, high demands), passive (low control, low demands), and low-strain (high control, low demands) (Citation5,Citation6).
Since Robert Karasek proposed that high-strain jobs may increase the risk of CHD (Citation7), the association between job strain and the risk of CHD has received considerable attention. A study from Denmark has shown that a high-strain job is associated with more than doubling the risk of CHD (Citation8), but results from other studies argue that this risk is much more modest (Citation9,Citation10), and some other studies failed to find any association (Citation11,Citation12). Furthermore, it is controversial as to whether the classification of ‘job strain’ by DCM has stronger effects on CHD than when the two scales of job demands and control are observed separately.
Given these inconsistent results, a meta-analysis of prospective cohort studies may help to clarify these issues. Therefore, the objectives of the present study include: 1) investigating the association between CHD risk and categories of job strain accessed by DCM; and 2) evaluating whether this relationship is caused by job control or job demands as observed separately.
Methods
Search strategy and selection criteria
According to the recommendations of the Meta-analysis of Observational Studies in Epidemiology Group (Citation13), we searched PubMed and Embase for prospective cohort studies published up to 30 October 2014, using a combined text and MeSH heading search strategy with the terms ‘burnout, professional’, ‘stress at work’, ‘work stress’, ‘job stress’, ‘occupational stress’, ‘occupational strain’, ‘job strain’, ‘job control’, ‘decision latitude’, ‘job demand’, ‘demand-control model’; and ‘cardiovascular disease’, ‘cardiovascular events’, ‘coronary artery disease’, ‘coronary heart disease’, ‘ischemic heart disease’, ‘myocardial ischemia’, ‘myocardial infarction’, and ‘angina’. Potentially suitable studies were searched by using cross-references from original articles and reviews. We restricted the search to human studies with no restrictions on language or time period. The detailed search strategy for PubMed is presented in Supplementary File 1 (available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2015.1075658), and the strategy for the Embase search was similar and adapted where necessary.
Studies were eligible if they met the following criteria: 1) prospective cohort study; 2) job strain categories or their components were measured at baseline; 3) follow-up duration ≥ 3 years with assessment of CHD; 4) the study reported multivariate-adjusted relative risks (RRs) or hazard ratios (HRs) and 95% confidence intervals (CIs) for events associated with high-strain, active, or passive jobs versus low-strain jobs, or if RRs and 95% CIs were reported for high demands versus low demands or low control versus high control, respectively.
Studies were excluded if 1) the relative risks were unadjusted or only adjusted for age and sex; 2) enrollment depended on having a specific risk factor condition (e.g. diabetes mellitus, hypertension, or other baseline chronic disease); or 3) data were derived from the same cohort or meta-analysis of other cohort studies. Data from the most recent publication were used for analysis if there were multiple publications from the same cohort.
Data extraction and quality assessment
Two authors (S.X. and Y.H.) selected potentially relevant studies and extracted the data independently according to the aforementioned criteria. For each included study we recorded baseline characteristics including participant characteristics, follow-up duration, and outcome assessment in the specially designed form.
We evaluated the quality of each study according to the Newcastle–Ottawa Quality Assessment Scale (NOS) for included studies (Citation14), in which the quality of a study was judged on three broad perspectives: selection (four items, one star each), comparability (one item, up to two stars), and exposure/outcome (three items, one star each). A star represents a high-quality choice of individual study. The detailed assessment list of NOS is presented in Supplemental File 2 (available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2015.1075658). In this analysis, studies were graded as good quality if they had ≥ 7 awarded stars.
Data synthesis and analysis
The primary outcome considered was the RR of CHD in subjects with high-strain, active, or passive jobs compared with low-strain jobs. The secondary outcome was the RR of CHD in individuals with low-control or high-demand jobs observed separately. Subgroup analyses of all groups was conducted according to sex (men versus women), follow-up duration (< 10 years versus ≥ 10 years), and adequate adjustment for risk factors (yes versus no). Adequate adjustment was defined as adjustment of at least five of seven factors among age, sex, diabetes mellitus or other measure of blood glucose, body mass index or other measure of overweight/obesity, cholesterol, smoking, and hypertension/blood pressure.
We analyzed multivariate-adjusted outcome data (expressed as RR or HR and 95% CI). After log-transformation of study-specific estimates, the inverse variance approach was used for analysis.
The I2 statistic was used to test heterogeneity (P < 0.10 or I2 > 50% represented significant heterogeneity). Results of studies were pooled using a fixed-effect model, if appropriate, after consideration of heterogeneity among studies. Otherwise, a random-effects model was used. Publication bias was assessed by inspecting funnel plots for each outcome in which the ln(RR) was plotted against standard error, as well as Egger's test (linear regression method). All analyses were performed with RevMan software version 5.2 for Windows (The Cochrane Collaboration, Copenhagen, Denmark) and Stata version 12.0 (Stata Corp LP, College Station, TX, USA). All P values are two-tailed, and the statistical significance was set at 0.05.
Results
Selected studies and characteristics
After screening the titles and abstracts of 1,474 reports retrieved in the initial search, 58 qualified for full review. Ultimately 14 prospective cohort studies (Citation4,Citation8–12,Citation15–22) comprising 232,767 individuals satisfied the study inclusion criteria and were analyzed ().
Figure 1. Flow of selection for studies. *Only the latest published data from the same cohort were included if duplicated reports offered the same outcome messages. CI = confidence interval; RR = relative risk.
summarizes the key characteristics of the included studies. Ages ranged between 16 and 74 years, and the duration of follow-up ranged from 3.2 years (Citation10) to 25 (Citation22) years. Five studies were from the United States (Citation11,Citation12,Citation15,Citation16,Citation22), and nine were from European countries (Citation4,Citation8–10,Citation17–21). All studies were graded as good quality according to the NOS. Details of the quality assessment are presented in Supplemental File 3 (available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2015.1075658).
Table I. Study characteristics.
Association between job strain categories and the risk of CHD
Eleven studies including 168,690 participants reported the RRs of CHD with high-strain, active, or passive job groups compared with the low-strain job group (Citation4,Citation8–12,Citation15,Citation18,Citation19,Citation21,Citation22). As there was no significant heterogeneity among all studies (all I2 < 50%), we used a fixed-effect model for the analyses.
High-strain and passive jobs were associated with an increased risk of CHD (RR 1.26, 95% CI 1.12–1.41, ; RR 1.14, 95% CI 1.02–1.29, ), while in active groups the associated risk of CHD was insignificant (RR 1.09, 95% CI 0.97–1.22, ). We did not find any evidence of publication bias by visual inspection of the funnel plot (Supplementary Figures 1–3, available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2015.1075658) or by using Egger's test (all P > 0.05).
Association between high-strain components and the risk of CHD
Eight studies (Citation8–10,Citation12,Citation17,Citation19,Citation21,Citation22) in the primary outcome analysis of DCM also reported the RRs of CHD with low control or high demands respectively, and these were included in the secondary outcome analysis. Furthermore, another three studies (Citation16,Citation17,Citation20) that reported CHD risk to be associated with low-control or high-demand jobs separately were also included, although DCM was not used in these studies. Data were pooled and calculated using the random-effects model, as there was significant heterogeneity (I2 > 50%) in both groups. Neither low control (RR 1.06, 95% CI 0.93–1.19, ) nor high demand (RR 1.13, 95% CI 0.97–1.32, ) was associated with an increased risk of CHD.
Subgroup analyses and sensitivity analyses
We performed subgroup analysis according to sex, follow-up duration, and adjustment of confounders, and the results are presented in . High-strain jobs were associated with an increased risk of CHD in males (RR 1.21, 95% CI 1.04–1.40) but not in females (RR 1.14, 95% CI 0.69–1.87). However, the difference between males and females was not significant (P = 0.83). The risk of CHD was increased in high-strain (RR 1.33, 95% CI 1.16–1.53) and passive subgroups (RR 1.20, 95% CI 1.05–1.36) with follow-up duration of longer than 10 years, but not in those with less than 10 years of follow-up (P ≥ 0.05). Furthermore, the risk of CHD-associated high-strain jobs was increased in studies with adequate adjustment of confounders (RR 1.18, 95% CI 1.04–1.34) and was much more pronounced in those with inadequate adjustment (RR 1.66, 95% CI 1.27–2.16).
Table II. Subgroup analyses of the association between job strain and CHD.
We used several methods to test the sensitivity and confirmed that the outcomes were not influenced by the use of fixed-effect or random-effects model, or odds ratios rather than RRs.
Discussion
In this study we found that, after controlling for multiple cardiovascular risk and socio-economic factors, high-strain (high demands, low control) and passive (low demands, low control) jobs were significantly associated with an increased risk of CHD compared with low-strain jobs (low demands, high control), especially in studies with a follow-up duration of more than 10 years. However, neither job control nor job demands were able to predict the risk of CHD when observed separately.
Several mechanisms may be involved in the association between work stress and the risk of CHD. First, individuals with high work stress may develop an unhealthy lifestyle involving smoking, sleep disturbances, reduced physical activity, and poor eating habits, which may accelerate the progress toward incident CHD (Citation23,Citation24). Second, work stress was associated with many cardiovascular risk factors, such as metabolic syndrome, overweight, impaired glucose metabolism, and dyslipidemia, which are also known as traditional risk factors for CHD (Citation25–27). A prior meta-analysis (Citation28) showed that the age- and gender-adjusted risk of CHD was increased in high-strain jobs, but the risk became insignificant after adjustment for risk factors and potential mediators. However, in our study the risk of CHD associated with high-strain jobs was still increased in studies with adequate adjustment of cardiovascular risk factors (RR 1.18, 95% CI 1.04–1.34). These results indicated that traditional cardiovascular risk factors could not fully explain the CHD risks in persons with work stress. Some novel mediators, such as activation of the hypothalamic-pituitary-adrenal axis and sympathetic nervous system, elevated inflammation, and enhanced cortisol secretion, may also account for the increased risk of CHD (Citation29–31).
Prior studies generally suggested that active or passive jobs did not contribute to the risk of CVD, and they thus received much less attention than high-strain jobs (Citation9,Citation22). Several meta-analyses, which defined job strain as a binary exposure model (high strain versus no strain [all other combinations]), suggested that individuals exposed to job strain had a significantly higher risk of CHD (Citation32–34). However, in the present study we used the typical exposure model (high strain, active, or passive vs. low strain) to define work stress and found that passive jobs were also associated with an increased risk of CHD, especially in studies with a follow-up duration of longer than 10 years. Therefore, we suggest that active, passive, and low-strain jobs could not be combined as ‘no strain,’ and that binary exposure classification of job strain may have underestimated the RR of high strain in prior studies.
It remains controversial as to whether the classification of work stress by DCM has better predictive effects on CVD than when the two scales of job demands or control are observed separately (Citation35). The Whitehall II study (Citation35) showed that low job control was associated with a 1.76-fold risk of CHD after adjustment for pre-employment factors. A larger-scale Danish study (Citation18) also showed that subjects with low job control had an increased risk of CHD. However, both of these studies were not adequately adjusted for traditional cardiovascular risk factors. In the present study we found that neither job control nor job demands could predict the risk of CHD when observed separately after controlling for multiple risk factors. These findings demonstrate that DCM, the combination of job control and job demands characteristics of work stress, is more important for identifying those individuals at higher risk of CHD.
As CHD is the leading cause of mortality worldwide (Citation36,Citation37), successful interventions aimed at reducing the prevalence of job strain could have a major impact on public health. A comprehensive Health Promotion Enterprise Program Study suggested that intervention programs incorporating both individual-level and organizational-level factors effectively reduced participants’ job stress levels and the probability of absenteeism related to depression (Citation38). Moreover, lifestyle modifications such as smoking cessation, a balanced diet, and exercise are essential for reducing the risk of CHD (Citation39). A recent study indicated that physical activity and exercise were useful tools to reduce stress and, therefore, the risk of developing cardiovascular disease (Citation40).
To the best of our knowledge, this is the first meta-analysis to clarify the risks of CHD in individuals with differing job strain. Our research comprises a large sample size (> 230,000 participants), and only prospective cohort studies with multivariate-adjusted RRs were included for analysis. These factors could reduce the selection and recall biases. However, there are some limitations in the study. First, the association between high-strain jobs and the risk of CHD in females was not significant, which may be due to the limited number of studies included. Furthermore, there was no significant difference in CHD risk between men and women, so this finding should be interpreted with caution. Further studies are needed to clarify the association between job strain and the risk of CHD in women. Second, as all included studies were from Europe and the United States, further analyses should be conducted in other regions, especially in developing countries. Third, job strain in most of the included studies was measured at a single time point. Data from the Whitehall II study manifested that the use of single-time exposure measures may underestimate the status of long-term job strain as a CHD risk factor (Citation41). Moreover, job changes during the follow-up period could weaken possible associations (Citation42).
In conclusion, this study showed that being exposed to high-strain or passive jobs is associated with an increased risk of CHD. It is of vital importance for subjects with occupations involving high stress to modify an unhealthy lifestyle. Intervention programs incorporating individual and organizational levels are crucial for reducing work stress and the subsequent risk of CHD.
Supplementary material available online
Supplementary Materials (Supplementary File 1, Supplementary File 2, Supplementary File 3 and Supplementary Figure 1–3) available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2015.1075658.
iann_a_1075658_sm5298.zip
Download Zip (303.9 KB)Acknowledgements
Shuxian Xu and Yuli Huang contributed equally to this work.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of interest: The authors declare that they have no competing interests.
References
- Gafarov V, Panov D, Gromova E, Gagulin I, Gafarova A. The influence of job stress on 16-th years risk of an arterial hypertension and myocardial infarction in female population aged 25-64 years in Russia (based on WHO epidemiological program MONICA-psychosocial). Global Heart. 2014;9:e49.
- Kivimaki M, Nyberg ST, Fransson EI, Heikkila K, Alfredsson L, Casini A, et al. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ. 2013;185:763–69.
- Hintsa T, Maattanen I, Hintsanen M, Swan H, Toivonen L, Kontula K, et al. Work stress and the long QT syndrome: high job strain and effort-reward imbalance at work associated with arrhythmic risk in the long QT syndrome. J Occup Environ Med. 2013;55:1387–93.
- Toren K, Schioler L, Giang WK, Novak M, Soderberg M, Rosengren A. A longitudinal general population-based study of job strain and risk for coronary heart disease and stroke in Swedish men. BMJ Open. 2014;4.
- Karasek R, Baker D, Marxer F. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health. 1981;71:694–705.
- Karasek R, Choi B, Ostergren PO, Ferrario M, De Smet P. Testing two methods to create comparable scale scores between the Job Content Questionnaire (JCQ) and JCQ-like questionnaires in the European JACE Study. Int J Behav Med. 2007;14:189–201.
- Karasek RA, Theorell T, Schwartz JE, Schnall PL, Pieper CF, Michela JL. Job characteristics in relation to the prevalence of myocardial infarction in the US Health Examination Survey (HES) and the Health and Nutrition Examination Survey (HANES). Am J Public Health. 1988;78:910–18.
- Netterstrom B, Kristensen TS, Sjol A. Psychological job demands increase the risk of ischaemic heart disease: a 14-year cohort study of employed Danish men. Eur J Cardiovasc Prev Rehabil. 2006;13: 414–20.
- Kuper H, Adami HO, Theorell T, Weiderpass E. Psychosocial determinants of coronary heart disease in middle-aged women: a prospective study in Sweden. Am J Epidemiol. 2006;164:349–57.
- De Bacquer D, Pelfrene E, Clays E, Mak R, Moreau M, De Smet P, et al. Perceived job stress and incidence of coronary events: 3-year follow-up of the Belgian job stress project cohort. Am J Epidemiol. 2005;161:434–41.
- Steenland K, Johnson J, Nowlin S. A follow-up study of job strain and heart disease among males in the NHANES1 population. Am J Ind Med. 1997;31:256–60.
- Lee S, Colditz G, Berkman L, Kawachi I. A prospective study of job strain and coronary heart disease in US women. Int J Epidemiol. 2002;31:1147–53.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2014. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Slopen N, Glynn RJ, Buring JE, Lewis TT, Williams DR, Albert MA. Job strain, job insecurity, and incident cardiovascular disease in the women's health study: results from a 10-year prospective study. PLoS One. 2012;7.
- Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino SRB, Benjamin EJ. Does job strain increase the risk for coronary heart disease or death in men and women? The Framingham Offspring Study. Am J Epidemiol. 2004;159:950–8.
- Bonde JP, Munch-Hansen T, Agerbo E, Suadicani P, Wieclaw J, Westergaard-Nielsen N. Job strain and ischemic heart disease: a prospective study using a new approach for exposure assessment. J Occup Environ Med. 2009;51:732–8.
- Huisman M, Van Lenthe F, Avendano M, Mackenbach J. The contribution of job characteristics to socioeconomic inequalities in incidence of myocardial infarction. Soc Sci Med. 2008;66:2240–52.
- Kornitzer M, DeSmet P, Sans S, Dramaix M, Boulenguez C, DeBacker G, et al. Job stress and major coronary events: results from the Job Stress, Absenteeism and Coronary Heart Disease in Europe study. Eur J Cardiovasc Prev Rehab. 2006;13:695–704.
- Hemmingsson T, Lundberg I. Is the association between low job control and coronary heart disease confounded by risk factors measured in childhood and adolescence among Swedish males 40-53 years of age? Int J Epidemiol. 2006;35:616–22.
- Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health. 2003;57:147–53.
- Alterman T, Shekelle RB, Vernon SW, Burau KD. Decision latitude, psychologic demand, job strain, and coronary heart disease in the Western Electric Study. Am J Epidemiol. 1994;139:620–7.
- Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32:473–81.
- Nyberg ST, Fransson EI, Heikkila K, Alfredsson L, Casini A, Clays E, et al. Job strain and cardiovascular disease risk factors: meta-analysis of individual-participant data from 47,000 men and women. PLoS One. 2013;8.
- Menni C, Bagnardi V, Padmanabhan S, Facchetti R, Sega R, Ferrario MM, et al. Evaluation of how gene-job strain interaction affects blood pressure in the PAMELA study. Psychosom Med. 2011;73:304–9.
- Djindjic N, Jovanovic J, Djindjic B, Jovanovic M, Pesic M, Jovanovic JJ. Work stress related lipid disorders and arterial hypertension in professional drivers - a cross-sectional study. Vojnosanit Pregl. 2013;70: 561–8.
- Jarczok MN, Koenig J, Li J, Mauss D, Hoffmann K, Schmidt B, et al. Vagal tone mediates the association between workstress and glycemic status: results from the Mannheim Industrial Cohort Study (MICS). Psychosom Med. 2014;76:A–35.
- Kivimaki M, Virtanen M, Elovainio M, Kouvonen A, Vaananen A, Vahtera J. Work stress in the etiology of coronary heart disease - a meta-analysis. Scand J Work Environ Health. 2006;32:431–42.
- Non AL, Rimm EB, Kawachi I, Rewak MA, Kubzansky LD. The effects of stress at work and at home on inflammation and endothelial dysfunction. PLoS One. 2014;9.
- Thole ME, Fischer JE. Work stress is related to circadian cortisol secretion and moderated by socioeconomic status: findings from the Mannheim Industrial Cohort Study (MICS). Psychosom Med. 2014;76:A–125.
- Weber CS. Stress hormones in psychocardiology: old stories and new paradigms. J Psychosom Res. 2013;74:561.
- Kivimaki M, Nyberg ST, Batty GD, Fransson EI, Heikkila K, Alfredsson L, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491–7.
- Kivimaki M, Batty GD, Ferrie JE, Kawachi I. Cumulative meta-analysis of job strain and CHD. Epidemiology. 2014;25:464–5.
- Kivimaki M, Singh-Manoux A, Virtanen M, Ferrie JE, Batty GD, Rugulies R. IPD-Work consortium: pre-defined meta-analyses of individual-participant data strengthen evidence base for a link between psychosocial factors and health. Scand J Work Environ Health. 2015;41:312–21.
- Hintsa T, Shipley MJ, Gimeno D, Elovainio M, Chandola T, Jokela M, et al. Do pre-employment influences explain the association between psychosocial factors at work and coronary heart disease? The Whitehall II study. Occup Environ Med. 2010;67:330–4.
- Gaziano TA. Reducing the growing burden of cardiovascular disease in the developing world. Health Aff (Millwood). 2007;26:13–24.
- Dalen JE, Alpert JS, Goldberg RJ, Weinstein RS. The epidemic of the 20(th) century: coronary heart disease. Am J Med. 2014;127:807–12.
- Sun J, Buys N, Wang X. Effectiveness of a workplace-based intervention program to promote mental health among employees in privately owned enterprises in China. Popul Health Manag. 2013;16:406–14.
- Kakiashvili T, Leszek J, Rutkowski K. The medical perspective on burnout. Int J Occup Med Environ Health. 2013;26:401–12.
- Tonello L, Rodrigues FB, Souza JWS, Campbell CSG, Leicht AS, Boullosa DA. The role of physical activity and heart rate variability for the control of work related stress. Front Physiol. 2014;5:67.
- Kivimaki M, Head J, Ferrie JE, Brunner E, Marmot MG, Vahtera J, et al. Why is evidence on job strain and coronary heart disease mixed? An illustration of measurement challenges in the Whitehall II study. Psychosom Med. 2006;68:398–401.
- Backe EM, Seidler A, Latza U, Rossnagel K, Schumann B. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health. 2012;85: 67–79.