Abstract
One interpretation of re-experiencing symptoms in post-traumatic stress disorder (PTSD) is that memories related to emotional information are stored strongly, but with insufficient specificity, so that stimuli which are minimally related to the traumatic event are sufficient to trigger recall. If so, re-experiencing symptoms may reflect a general bias against encoding background information during a learning experience, and this tendency might not be limited to learning about traumatic or even autobiographical events. To test this possibility, we administered a discrimination-and-transfer task to 60 Veterans (11.2% female, mean age 54.0 years) self-assessed for PTSD symptoms in order to examine whether re-experiencing symptoms were associated with increased generalization following associative learning. The discrimination task involved learning to choose the rewarded object from each of six object pairs; each pair differed in color or shape but not both. In the transfer phase, the irrelevant feature in each pair was altered. Regression analysis revealed no relationships between re-experiencing symptoms and initial discrimination learning. However, re-experiencing symptom scores contributed to the prediction of transfer performance. Other PTSD symptom clusters (avoidance/numbing, hyperarousal) did not account for significant additional variance. The results are consistent with an emerging interpretation of re-experiencing symptoms as reflecting a learning bias that favors generalization at the expense of specificity. Future studies will be needed to determine whether this learning bias may pre-date and confer risk for, re-experiencing symptoms in individuals subsequently exposed to trauma, or emerges only in the wake of trauma exposure and PTSD symptom development.
Introduction
Among the symptoms of post-traumatic stress disorder (PTSD) are re-experiencing symptoms that reflect frequent, unintentional and intrusive memories of the traumatic event. These memories can be triggered by situations or stimuli that reflect aspects of the traumatic event or can occur in the absence of external stimuli (Elzinga & Bremner, Citation2002). Concurrently, individuals with PTSD tend to have relatively impoverished memories for specific details of their trauma (Brewin, Citation2014; Brewin et al., Citation2010).
A possible explanation for the development of re-experiencing symptoms in PTSD invokes generalization. Generalization can occur when learned responses are applied to new or altered stimuli, or to familiar stimuli presented in a new context. If individuals with PTSD have a bias toward generalization, rather than specificity, in memory coding, this would make their memories of traumatic events vulnerable to be triggered by a wide range of stimuli that would not normally provoke recall (Tryon, Citation1998).
Increased generalization is not confined to memories of the traumatic event associated with PTSD. Thus, for example, when given specific cue words and asked to retrieve specific autobiographical memories, those with PTSD typically recall fewer specific episodes and the retrieved memories have fewer details (Brown et al., Citation2012; McNally et al., Citation1995). Increased generalization is also observed in associative learning tasks involving purely cognitive, impersonal information (Kostek et al., Citation2014; Levy-Gigi et al., Citation2015). For example, a contextual processing task with positive and negative outcomes showed increased generalization of negative context in individuals with clinically diagnosed PTSD. When a negative outcome (context) was initially paired with a cue, individuals with PTSD had difficulty subsequently learning to associate that same cue with a now positive outcome (Levy-Gigi et al., Citation2015).
Another study used an acquired equivalence task where subjects learned to associate stimuli with outcomes (Kostek et al., Citation2014). Some stimuli were equivalent (i.e. paired with the same outcome). Subjects later learned to associate some of the stimuli with a different outcome. Veterans with higher levels of PTSD re-experiencing symptoms showed an increased tendency to generalize with the assumption that the equivalent stimuli should also be paired with the new outcomes.
The present study examined whether increased generalization would also be observed in a different type of associative learning task that involved concurrent discrimination learning followed by a transfer test that assessed generalization when irrelevant stimulus features were altered. We administered this task to a group of Veterans self-assessed for presence and severity of PTSD symptoms. Our central hypothesis focused on the relationship between PTSD re-experiencing symptoms and generalization (i.e. transfer errors). We predicted that there would not be a relationship between PTSD symptoms and initial discrimination learning. However, we predicted that there would be facilitated transfer performance (increased generalization) in those with more severe PTSD re-experiencing symptoms. We also predicted that other variables associated with PTSD risk (i.e. personality factors and combat history) would not account for significant additional variance in generalization.
The current study also collected information on combat exposure and behavioral inhibition, which have been found to be associated with PTSD vulnerability. We assessed whether these variables were associated with a tendency for increased generalization beyond their common association with PTSD symptoms.
Methods
Participants
Participants were 60 Veterans from VA New Jersey Health Care System in East Orange, NJ (11.2% female, mean age 54.0 years, SD 10.3, mean education 14.4 years, SD 2.6) and from the same population used in our prior acquired equivalence study (Kostek et al., Citation2014). Thirty-eight Veterans (63.3%) self-identified as African-American, 18 (30.0%) as Caucasian and the remaining 4 (6.7%) as Other or Mixed-race; 7 (13.7%) self-identified ethnicity as Hispanic. When asked about conflicts in which they had served, 24 reported serving in Vietnam, 22 in peacetime or no specific conflict and the remainder in other conflicts (Gulf War/Operation Desert Storm, Operation Enduring Freedom/Operation Iraqi Freedom, Granada or Panama).
When asked about medications, 22 Veterans (36.7%) self-reported antidepressant use, while another 9 reported use of other psychoactive medications (typically sleep aids). Because many participants could not provide more specific information about their medications, detailed analysis of possible medication effects was not possible in this sample.
This study was approved by the IRB at VA NJHCS and followed guidelines established by the Federal Government for the protection of human subjects. Subjects received $20/h for participation in a 2-h session. Written informed consent was obtained from all subjects prior to initiating any testing.
Procedures
Neuropsychological testing
Subjects completed a short battery of self-assessment questionnaires, including the PTSD Checklist-Military version (PCL-M; Blanchard et al., Citation1996), the Combat Exposure Scale (CES; Keane et al., Citation1989) and the Adult and Retrospective Measures of Behavioral Inhibition (AMBI/RMBI; Gladstone & Parker, Citation2005).
The PCL-M (Blanchard et al., Citation1996) is a 17-item questionnaire that self-assesses the presence and frequency of PTSD symptoms in response to stressful military events, including but not limited to combat. Specific PCL-M questions correspond to DSM-IV symptom clusters, subscores can be generated for each symptom cluster (cluster B = re-experiencing, cluster C = avoidance/numbing and cluster D = hyperarousal). A total PCL-M score of 50 or greater has been used as an indicator of PTSD in military samples (Weathers et al., Citation1993). The CES (Keane et al., Citation1989) consists of seven items that assesses frequency, duration and amount of exposure to combat. Veterans with a total CES score <8 were classified as non-combat, while those scoring ≥8 were classified as having a history of exposure to combat, as done in previous studies (Ginsberg et al., Citation2008; Myers et al., Citation2012a, Citation2013). The 16-item AMBI and 18-item RMBI (Gladstone & Parker, Citation2005) assess current (adult) and retrospective (childhood) behavioral inhibition, defined as a tendency to withdraw from or avoid novel social and non-social situations; AMBI scores have been shown to correlate with measures of anxiety proneness (Gladstone & Parker, Citation2005; Gladstone et al., Citation2005) and with self-reported PTSD symptoms (Myers et al., Citation2012a, Citation2012b).
Discrimination-and-transfer task
The discrimination-and-transfer task was performed as previously described (Levy-Gigi et al., Citation2012). In brief, the task had a training phase comprised of six training stages followed by a transfer phase. On each trial in training stage 1, subjects saw a pair of objects, of which one was designated as the rewarded object (); the rewarded object could appear on either the left or the right. Subjects used keyboard keys labeled “LEFT” and “RIGHT” to select one of the objects, which was then raised and, if it was the rewarded stimulus, a smiley face was revealed underneath (). Once participants reached criterion performance on this pair (two consecutive correct responses), training stage 2 began with a new pair introduced, and trials with this pair and the old pair were intermixed until the participant reached criterion on both pairs (four consecutive correct responses). For subsequent stages, this process was repeated with four new pairs, until the subject was responding correctly to six pairs (12 consecutive correct responses) or to a maximum of 72 trials. Three pairs differed in shape but not color (i.e. brown mushroom vs. brown square), and three pairs differed in color but not shape (i.e. red cat's-eye vs. yellow cat's-eye). Thus, in each pair, one feature was relevant and predictive, and one was redundant and therefore irrelevant. For each of the six training stages, data were scored as total errors.
Figure 1. The discrimination-and-transfer test. (A) Two sample discrimination trials, with a pair of objects that differ in one relevant feature (on the top, color is the relevant feature and on the bottom, shape is the relevant feature). (B) The subject chooses an object, which is raised; if correct, a smiley face is revealed underneath. (C) Two sample transfer phase trials, in which the irrelevant feature of each object pair is changed (on the top, shape is the irrelevant feature that has changed and on the bottom, color is the irrelevant feature that has changed).
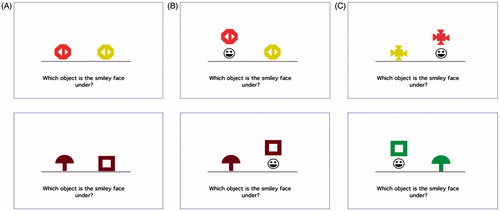
For participants who reached criterion on training stage 6, the transfer phase began without warning to the participant. This phase was a transfer test where relevant features remained the same in each pair, but irrelevant features were altered. Original valences remained unchanged; thus, if the red object was rewarded in training stage 6, it was also rewarded in the transfer phase (). None of the new colors or shapes had previously appeared in training stage 6. Transfer phase continued to a criterion of 12 consecutive correct responses or to a maximum of 72 trials. Data from transfer were scored as total errors.
To test our central hypothesis regarding relationships between PTSD re-experiencing symptoms and generalization, we used hierarchical linear regression. For both training stage 6 and transfer phase total errors, regression was conducted with demographic information (age, sex, education) entered at the first step, PTSD cluster B score entered at the second step and the remaining variables (PTSD cluster C and D scores, CES, AMBI, RMBI) entered at the final step.
Results
Questionnaire scores
Mean scores for the questionnaires are shown in . Mean PCL-M score was 46.4 (19.6), similar to what has been found in other Veteran samples not specifically selected for PTSD (i.e. Eisen et al., Citation2012; Peitrzak et al., Citation2010); 26 participants (43.3%) scored at or above the cut-off of 50, which has been proposed as an indicator of PTSD in military samples (Blanchard et al., Citation1996; Weathers et al., Citation1993). Mean CES score was 9.0 (11.5); the majority of Veterans were non-combat (66.7% scored below the cut-off of 8). As would be expected, PCL-M cluster subscores were highly intercorrelated; AMBI scores showed strong relationships with cluster subscores. RMBI scores were highly correlated with AMBI but not with any other score ().
Table 1. Mean (and SD) scores on the self-report questionnaires, and correlations between pairs of scores.
Discrimination and transfer test: training phase
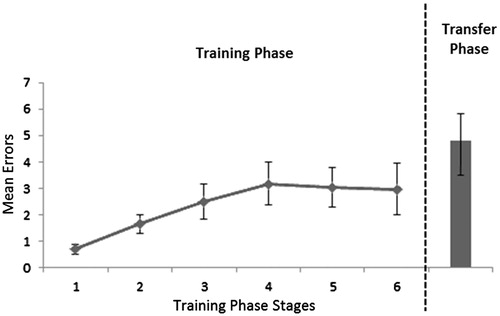
Mean number of errors increased across the six training stages (; rmANOVA with Greenhouse–Geisser correction, F(2.88, 170.1) = 4.24, p = 0.007). All but four subjects reached the learning criterion in training stage 6. Of these four “non-solvers”, all had successfully reached criterion in stage 4 or 5 or both, but failed to reach criterion in stage 6; these subjects were retained in the analyses.
Figure 2. Mean errors for each of the six training stages of the discrimination-and-transfer task and mean errors for the transfer phase.
To examine whether any demographic or questionnaire variables predicted training performance, hierarchical linear regression was conducted on the total number of training errors (summed across training stages 1–6). In the first step, demographic information (age, sex, education) was entered; the resulting model did not significantly predict training errors (R = 0.230, R2 = 0.053, p = 0.381). In the second step, PTSD cluster B scores were entered, and again the resulting model did not significantly predict training errors (R = 0.246, R2 = 0.061, R2-change = 0.008, p = 0.505). The remaining variables (cluster C, cluster D, CES, RMBI, AMBI) were entered in the third step and, again, the resulting model did not significantly predict training errors (R = 0.453, R2 = 0.205, R2-change = 0.144, p = 0.127).
As hierarchical regression can hide relationships between the dependent variable and predictors entered in later stages of the model, we also examined bivariate correlation between each possible predictor and training errors; no significant relationships were found (all r ≤ ±0.260, all p > 0.046).
Discrimination and transfer test: transfer phase
As shown in , most participants made few errors during the transfer phase (21 subjects made no errors and 48 made five or fewer errors). The number of transfer phase errors was strongly correlated with training stage 6 errors (r = 0.670, p < 0.001) and with the number of errors summed across the six training stages (r = 0.555, p ≤ 0.001). Accordingly, in analysis of transfer phase data, training stage 6 errors were entered as another predictor variable in the regression model.
shows that the number of transfer phase errors tended to decrease as the number of self-reported re-experiencing symptoms increased. This suggests an increased generalization as the severity of re-experiencing symptoms increase. To further investigate this effect, we conducted hierarchical linear regression with the number of transfer phase errors as the dependent variable. Demographic variables (age, sex, education) entered at the first step did not significantly predict performance (R = 0.295, R2 = 0.087, p = 0.162). At the second step, the number of training stage 6 errors was entered, which resulted in a significant prediction of transfer performance (R = 0.706, R2 = 0.499, R2-change = 0.412, p < 0.001). Adding cluster B scores in the third step significantly increased prediction of transfer performance (R = 0.735, R 2 = 0.541, R2-change = 0.042, p = 0.030). Adding the remaining variables (clusters C and D, CES, RMBI, AMBI) to the model did not account for any residual variance (R = 0.770, R2 = 0.593, R2-change = 0.053, p = 0.294).
Figure 3. Transfer phase performance. (A) Mean errors on the transfer phase decreased with increasing number of PTSD Cluster B symptoms endorsed. (B) There was also a negative correlation between transfer errors and educational attainment.
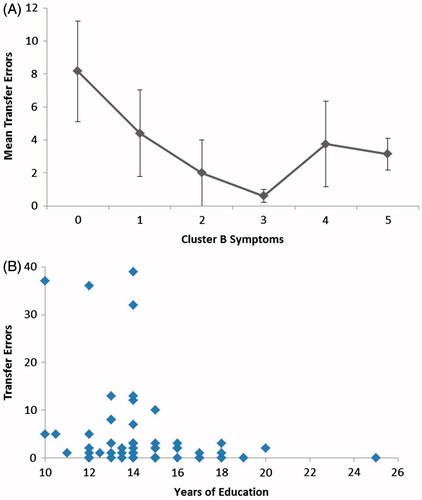
Other than the expected strong relationship between training stage 6 errors and transfer phase errors (r = 0.670), no other predictor variable reached corrected significance (all r ≤ ±0.266, all p > 0.040). The only variable that approached corrected significance was education, which negatively correlated with transfer errors (r = −0.266, p = 0.040; i.e. positively correlated with generalization). shows the relationship between the number of transfer errors and education. The four subjects who performed very poorly on the task had fairly low levels of education, while no subject with 16 or more years of education made more than three errors during the transfer phase.
Our secondary hypothesis concerned possible relationships between generalization and PTSD risk factors, including combat history and behavioral inhibition. None of these variables emerged as predictive in the regression analyses, and tests of bivariate correlation revealed no significant relationships between transfer phase errors and AMBI, RMBI or CES scores, regardless of whether or not training stage 6 errors were partialed out (all r < ±0.210, all p > 0.100).
Discussion
In the current study, we administered a discrimination-and-transfer task to Veterans self-assessed for PTSD symptoms. While there was no particular relationship between PTSD symptoms and initial learning of discrimination pairs, there was a positive relationship between re-experiencing symptoms and generalization when irrelevant stimulus information was altered.
Increased generalization has now been observed in three different studies of PTSD: in the first study, participants recruited from the same Veteran population as the current study were assessed on an acquired equivalence task (Kostek et al., Citation2014), and in the second, trauma-exposed individuals from a very different population (individuals with clinically-diagnosed PTSD and a single exposure to trauma) were assessed on a contextual processing task (Levy-Gigi et al., Citation2015). The current study assessed a different type of generalization: the ability to transfer learning when relevant stimulus features remain stable and irrelevant stimulus features are altered. Despite differences in the population and type of generalization assessed, all three studies converge to suggest that there is increased generalization in those with PTSD symptoms, especially those with greater re-experiencing symptoms. A previous study (that used the same acquired equivalence task used by Kostek et al., Citation2014) observed an opposite generalization effect: individuals with PTSD showed a selective deficit in generalization to unlearned, novel pairings (Levy-Gigi et al., Citation2012), although some subjects with PTSD did show an ability to generalize. In that study, PTSD was clinically diagnosed (meeting criteria A, E and F) via interview and all participants had been exposed to trauma. The severity of re-experiencing symptoms was not quantified, so it is possible that those with higher levels of re-experiencing symptoms may have demonstrated increased generalization.
The idea that re-experiencing symptoms are associated with increased generalization is consistent with the dual representation theory of PTSD, which posits that re-experiencing symptoms may be due to a disconnect between sensory-bound representations (S-Reps) and abstract, contextualized representations (C-Reps) that depend on the medial temporal lobe structures (e.g. hippocampus) (Brewin et al., Citation2010). Flashbacks occur when an S-Rep is created by an emotional event without an appropriate representation from a corresponding C-Rep. Such a disconnect can result in memories of traumatic events lacking contextualization, causing traumatic memories to be experienced as though they were occurring in the present day.
In fact, many learning tasks used to assess generalization are dependent on the medial temporal lobes. The discrimination-and-transfer test used here was previously examined in amnesic patients with hippocampal damage (Myers et al., Citation2008), who showed spared initial learning but impaired transfer. One interpretation is that the hippocampus and associated medial temporal lobe structures are important for the flexibility with which learning can be applied to changing task conditions (Eichenhaum et al., Citation1992; Squire & Knowlton, Citation1995). Given that hippocampal volume often has been found to be reduced in PTSD (Gilbertson et al., Citation2002; Levy-Gigi et al., Citation2015; Smith, Citation2005), we might have expected that patients with PTSD would show impaired generalization. However, the medial temporal lobe includes several structures, each with distinct anatomy and physiology and presumably with distinct function. In particular, it has been suggested that medial temporal cortices including entorhinal and parahippocampal cortex may serve to compress co-occurring cues into configural representations while the hippocampus (including dentate gyrus) may differentiate representations to help distinguish highly-similar inputs (Eichenbaum et al., Citation1992; Myers et al., Citation1995). If so, etiologies where the latter subregions are preferentially disrupted might produce increased generalization, while preferential disruption of the former subregions might reduce generalization. Consistent with this possibility, a recent neuroimaging study of this task in healthy adults showed an inverse relationship between learning-related hippocampal activity and subsequent generalization (Fera et al., Citation2014). Further imaging studies in individuals with PTSD would be useful to determine whether reduced hippocampal volume and/or activity similarly correlate with generalization and/or re-experiencing symptoms.
The current study also found a positive relationship between generalization and educational attainment. Although this was not reported in prior studies with this discrimination-and-transfer test, prior studies generally used smaller sample sizes that may have had a more restricted educational range, which could hinder the detection of a correlation. Nevertheless, as shown in , the relationship with education in the current study was largely due to five subjects: four performed very poorly on the transfer phase, and one self-reported 25 years of education. It will be important to confirm whether this relationship is present in other samples, especially given that prior studies have found more education to be associated with reduced, not greater, risk for PTSD (Brewin et al., Citation2000).
Finally, no significant relationships were observed between generalization and any of the other questionnaire scores (CES, AMBI, RMBI). Our sample size is relatively small; future studies with larger sample sizes will be needed to confirm whether the absence of relationships reflects reliable findings or may have resulted from inadequate statistical power. Even so, the absence of relationship in the current sample suggests that: (1) exposure to combat is not alone sufficient to produce increased generalization, and (2) increased generalization and behavioral inhibition are not related beyond their common association with PTSD symptoms. We recognize that the majority of our sample had little to no combat experience; later studies could incorporate Veterans with more combat experience to verify the absence of a relationship among combat experience and generalization. We also acknowledge that increased generalization may be attributed to other factors aside from PTSD symptomatology, including trauma exposure. Future studies could examine the role of trauma exposure and how it may affect this learning bias. Additionally, longitudinal studies would be required to fully answer the question of whether increased generalization confers risk for PTSD symptoms or emerges as PTSD symptoms develop; such studies remain a direction for future work.
Acknowledgements
For assistance with data collection, the authors wish to thank Yasheca Williams and John Kostek.
Declaration of interest
This work was supported by the NSF/NIH Collaborative Research in Computational Neuroscience (CRCNS) program and NIAAA R01 AA018737, by Award Number I01CX000771 from the Clinical Science Research and Development Service of the VA Office of Research and Development, and by the SMBI. The authors affirm that they have no relationships that could constitute potential conflict of interest.
References
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. (1996). Psychometric properties of the PTSD checklist (PCL). Behav Res Ther 34(8):669–73
- Brewin CR. (2014). Episodic memory, perceptual memory, and their interaction: foundations for a theory of posttraumatic stress disorder. Psychol Bull 140(1):69–97
- Brewin CR, Andrews B, Valentine JD. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 68(5):748–66
- Brewin CR, Gregory JD, Lipton M, Burgess N. (2010). Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychol Rev 117(1):210–32
- Brown AD, Root JC, Romano TA, Chang LJ, Bryant RA, Hirst W. (2012). Overgeneralized autobiographical memory and future thinking in combat veterans with posttraumatic stress disorder. J Behav Ther Exp Psychiatr 44(1):129–34
- Eichenbaum H, Otto T, Cohen NJ. (1992). The hippocampus – what does it do? Behav Neural Biol 57:2–36
- Eisen SV, Schultz MR, Vogt D, Glickman ME, Elwy AR, Drainoni M, Osei-Bonsu PE, Martin J. (2012). Mental and physical status and alcohol and drug use following return from deployment to Iraq or Afghanistan. Am J Public Health 102(S1):66–73
- Elzinga BM, Bremner JD. (2002). Are the neural substrates of memory the final common pathway in posttraumatic stress disorder (PTSD)? J Affect Disord 70(1):1–17
- Fera F, Passamonti L, Herzallah MM, Myers CE, Veltri P, Morganti G, Quattrone A, Gluck MA. (2014). Hippocampal BOLD response during category learning predicts subsequent performance on transfer generalization. Hum Brain Mapp 35(7):3122–31
- Gilbertson M, Shenton M, Ciszewski A, Kasai K, Lasko N, Orr S, Pitman RK. (2002). Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nat Neurosci 5(11):1111–13
- Ginsberg JP, Ayers E, Burriss L, Powell DA. (2008). Disruption of bradycardia associated with discriminative conditioning in combat veterans with PTSD. Neuropsychiatr Dis Treatment 4:635–46
- Gladstone GL, Parker G. (2005). Measuring a behaviorally inhibited temperament style: development and initial validation of new self-report measure. Psychiatry Res 135:133–43
- Gladstone GL, Parker GB, Mitchell PB, Wilhelm KA, Malhi GS. (2005). Relationship between self-reported childhood behavioral inhibition and lifetime anxiety disorders in a clinical sample. Depress Anxiety 22(3):103–13
- Keane TM, Fairbank JA, Caddell JM. (1989). Clinical evaluation of a measure to assess combat exposure. Psychol Assess 1:53–5
- Kostek JA, Beck KD, Gilbertson MW, Orr SP, Pang KCH, Servatius RJ, Myers CE. (2014). Acquired equivalence in veterans with symptoms of posttraumatic stress disorder (PTSD): re-experiencing symptoms are associated with greater generalization. J Trauma Stress 27(6):717–20
- Levy-Gigi E, Kéri S, Myers CE, Lencovsky Z, Sharvit-Benbaji H, Orr S, Gluck MA. (2012). Individuals with post-traumatic stress disorder show a selective deficit in generalization of associative learning. Neuropsychology 26:758–67
- Levy-Gigi E, Szabo C, Richter-Levin G, Kéri S. (2015). Reduced hippocampal volume is associated with overgeneralization of negative context in individuals with PTSD. Neuropsychology 29(1):151–61
- McNally RJ, Lasko NB, Macklin ML, Pitman RK. (1995). Autobiographical memory disturbance in combat-related posttraumatic stress disorder. Behav Res Ther 33(6):619–30
- Myers CE, Gluck M, Granger R. (1995). Dissociation of hippocampal and entorhinal function in associative learning: a computational approach. Psychobiology 23(2):116–38
- Myers CE, Hopkins R, DeLuca J, Moore N, Wolansky L, Sumner J, Gluck MA. (2008). Learning and generalization deficits in patients with memory impairments due to anterior communicating artery aneurysm rupture or hypoxic brain injury. Neuropsychology 22(5):681–6
- Myers CE, Moustafa AA, Sheynin J, VanMeenen KM, Gilbertson MW, Orr SP, Beck KD, et al. (2013). Learning to obtain reward, but not avoid punishment, is affected by presence of PTSD symptoms in male veterans: empirical data and computational model. PLoS One 8(8):e72508
- Myers CE, VanMeenen K, McAuley JD, Beck KD, Pang KCH, Servatius RJ. (2012a). Facilitated acquisition of eyeblink conditioning in veterans with high behavioral inhibition, a risk factor for post-traumatic stress disorder (PTSD). Stress 15(1):31–44
- Myers CE, VanMeenen KM, Servatius RJ. (2012b). Behavioral inhibition and PTSD symptoms in veterans. Psychiatry Res 196:271–6
- Peitrzak RH, Johnson DC, Goldstein MB, Malley JC, Rivers AJ, Morgan CA, Southwick SM. (2010). Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operaction Enduring Freedom and Iraqi Freedom: the role of resilience, unit support, and postdeployment social support. J Affect Disord 120:188–92
- Smith M. (2005). Bilateral hippocampal volume reduction in adults with post-traumatic stress disorder: a meta-analysis of structural MRI studies. Hippocampus 5:798–807
- Squire L, Knowlton B. (1995). Memory, hippocampus, and brain systems. In: Gazzaniga M, editor. The cognitive neurosciences. Cambridge, MA: MIT Press; p 825–37
- Tryon W. (1998). A neural network explanation of posttraumatic stress disorder. J Anxiety Disord 12:373–85
- Weathers FW, Litz B, Herman D, Huska J, Keane T. (1993). The PTSD checklist (PCL): reliability, validity, and diagnostic utlility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX
