Abstract
The primary aim of computer-assisted knee arthroplasty is to improve the alignment of the implanted prostheses. Accurate component alignment is dependent on the establishment of accurate anatomical reference points. Current techniques for establishing the center of the ankle joint, especially in the coronal plane, rely solely on clinical judgment in relation to the position of the center of the ankle joint. The aim of this study was to determine if an algorithm could be developed, based on establishing the most prominent points on the medial and lateral malleoli on 3D CT scans, to accurately and reproducibly establish the position of the center of the ankle joint. To determine this, images of 20 ankles were obtained and axial, coronal, and sagittal 2D reconstructions were manipulated on a workstation. Two observers independently performed relevant measurements and calculations. The calculated data was found to be reproducible with a very small standard deviation in each plane. This algorithm is able to provide accurate measurements of the ankle joint in knee navigation surgery. Caution must be exercised in anatomically abnormal ankles, as the calculations of the ankle center were found to be significantly different.
Introduction
Total knee arthroplasty (TKA) is widely regarded as a highly effective method of treating degenerative joint disease. The outcome of TKA is generally successful, but potential for failure inevitably exists Citation[1]. Such failures may result from component loosening, instability, dislocation, fracture or infection, and occur at an incidence of 5–8% Citation[2], Citation[3]. The outcome of TKA is particularly sensitive to variations in surgical technique Citation[4]. Incorrect positioning or orientation of the component prostheses and improper alignment of the limb can lead to accelerated implant wear and loosening, as well as sub-optimal functional performance Citation[5].
A number of studies have demonstrated that alignment errors in excess of 3° are associated with more rapid failure and less satisfactory functional results following TKA Citation[6–8]. Even a small (2.5 mm) anteroposterior displacement of the femoral component has been shown to alter the knee's range of motion by as much as 20° Citation[9]. A significant amount of evidence exists implying that the most common cause for revision TKA is error in the initial surgical technique.
The use of mechanical alignment guides has improved the accuracy with which implants can be inserted. However, errors in tibial and femoral alignment exceeding 3° still occur in approximately 10% of TKA procedures Citation[5]. Teter et al. reported that 8% of tibial cuts were malaligned by more than 4° in the coronal plane when an extramedullary alignment guide was used Citation[10]. This is due to the fact that fundamental problems exist in such alignment systems that limit their ultimate accuracy. The accuracy of arthroplasty procedures is also limited by inherent errors in standard preoperative radiographs.
It is important to recognize that even the most sophisticated mechanical instrumentation systems ultimately rely on visual inspection and clinical judgment to confirm the accuracy of limb and implant alignment, as well as the stability at the conclusion of the TKA procedures Citation[5]. In addition, alignment guides are designed based on standardized bone geometry. Optimal placement of the components may therefore not be achieved when the patient's bones differ from the assumed bone geometry used in the instrument design process Citation[1].
The primary aim of computer-assisted knee replacement surgery is to improve the alignment of the implanted prostheses. Computer-based alignment systems have been developed to address the limitations inherent in mechanical instrumentation systems used in TKA Citation[11], Citation[12]. Navigation systems augment mechanical instrumentation through the addition of measurement probes that can be used to locate joint centers, track surgical tools, and align prosthetic components Citation[5].
Despite the potential for improved accuracy with the use of computer navigation, accurate alignment of the prostheses still relies on the initial establishment of accurate anatomical landmarks and reference points. Current techniques for establishing the location of the center of the ankle joint continue to rely on the clinical judgment of the surgeon in estimating the location of this point.
The intention of this study was to determine whether an algorithm based on the establishment of the most prominent points on the medial and lateral malleoli on a 3D CT scan could be developed and reproducibly used to identify the position of the center of the ankle joint.
Materials and methods
Images of 20 ankles were obtained on a Toshiba Aquilion four-detector-row multi-slice CT scanner. Scans of 0.5 mm thickness were performed at 0.4-mm intervals. Axial, coronal and sagittal multi-planar 2D reconstructions were generated and manipulated on a workstation. The scans obtained included 17 normal ankles, 2 ankles with evidence of degenerative joint disease and 1 ankle that had previously been fractured. Two independent observers, registered training orthopaedic registrars, performed the measurements and calculations described subsequently.
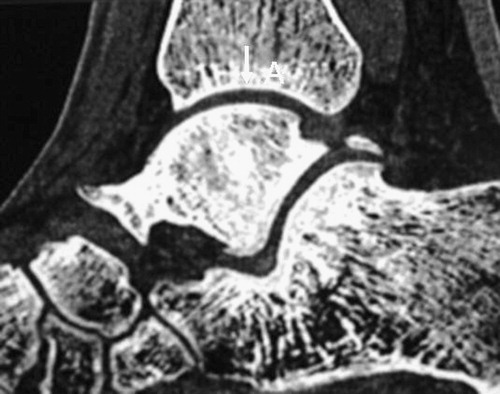
There are no strict anatomical references for the true center of the ankle joint. For the purposes of this study, the center of the ankle joint was defined in the sagittal plane as corresponding to the highest, most proximal point of the talar dome (). In the coronal plane the center of the ankle joint was defined as the mid-point of the talus in this plane.
Figure 1. In the sagittal plane, the center of the ankle is defined as the high point of the talar dome and the corresponding high point of the tibial articular surface.
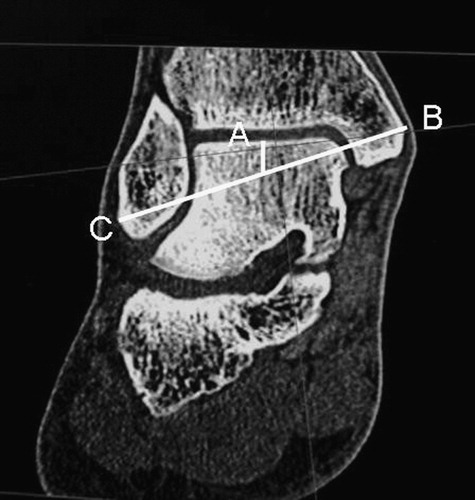
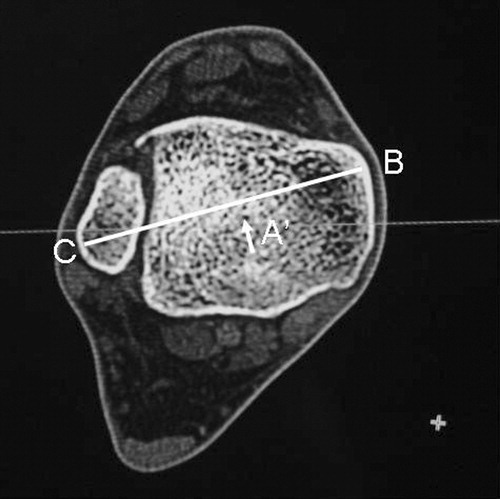
Alternating between transverse, sagittal and coronal scans as required, the most peripheral points of the medial and lateral malleoli were determined. A line adjoining these points was calculated and produced by the computer software. The center of the ankle joint was identified in the sagittal and coronal planes ().
Figure 2. Example of CT image with the center of the ankle and the medial/lateral malleolar axis inserted (diagrammatic). A = anatomically defined center of ankle joint; B = most medial point; C = most lateral point.
The following measurements were calculated in the coronal plane: i) the total distance between the most peripheral points on the medial and lateral malleoli; ii) the distance from the most peripheral point on the medial malleolus to the center of the ankle, as defined previously; and iii) the distance from the most peripheral point on the lateral malleolus to the center of the ankle, as defined previously.
Measurements were taken in the coronal and sagittal planes. The coronal measurements were based on the previously described computer-generated lines. The recorded measurements were: the total inter-malleolar distance; the distance from the medial malleolar point to the marked center of the ankle joint; and the distance from the lateral malleolus to the marked center of the ankle joint. Subsequent calculated ratios were:
medial malleolus to center distance: total inter-malleollar distance
lateral malleolus to center distance: total inter-malleolar distance
medial malleolus to center distance: lateral malleolus to center distance
Following this data collection, statistical analysis was performed using ANOVA, paired t-tests, and regression analysis as appropriate. In addition to analyzing the results of the complete set of ankles, calculations were made for the normal ankles, the arthritic ankles, and the previously fractured ankle. The results for these separate groups were then compared against each other.
Results
The described observations and calculations yielded a set of statistically significant results in relation to the description of the location of the center of the ankle joint in the investigated planes of assessment. In the coronal plane, the calculations and analyses displayed a strong correlation in the values attained by each individual observer. The average inter-malleolar distance was determined to be 70.2 mm (95% CI, 68.3–72.0). It should be noted that this is not an actual physical value, but rather a computer-derived measurement, as the actual values are scaled by the computer for viewing. However, the absolute values are not important as all the calculations are based on ratios.
Of the calculated ratios for the normal ankles, the strongest correlation was observed with the ratio of lateral distance to total inter-malleolar distance (r = 0.854) (). This ratio of lateral distance to total inter-malleolar distance was observed at 0.57 (95% CI, 0.56–0.58) in the normal ankle sample. The range of values in this group was from 0.49 to 0.63. The validity of this ratio, in this sample of normal ankles, was further substantiated (beta = 0.569) using linear regression analysis with no constant (). In the sample of arthritic ankles, the observed ratio was 0.48 (95% CI, 0.46–0.50). The sample of the previously fractured ankle displayed a ratio of 0.57 (95% CI 0.15–0.99). In this sample, the confidence interval is large due to the small sample size. The differences in ratio values were noted to be statistically significant at the 5% level (p < 0.02) when compared using ANOVA.
Table I. Correlations for various measures in normal ankles.
Table II. Linear regression coefficients for predicting lateral from total with no constant.
In the sagittal plane, the observed individual measurements of each observer demonstrated a poor level of correlation (r = 0.218). However, the mean distances from the calculated line to the true center of the ankle joint were not statistically different. The true center of the ankle joint was observed to always lie posterior to the calculated line (). The calculated values were 4.2 mm (95% CI, 2.5–5.9) and 2.8 mm (95% CI, 1.7–3.8). In combination, this data describes that the mean distance of the true center of the ankle joint from the calculated inter-malleolar line averages 3.2 mm (95% CI, 2.3–4.0).
Figure 3. Illustration showing how the mid-point of the ankle joint in the sagittal plane (A, illustrated on a coronal view) passes posterior to the axis joining the most prominent points on the medial (B) and lateral (C) malleoli.
The observed and calculated data in this series displayed a high degree of reproducibility. Using the calculated 95% confidence intervals, the projected angular error in tibial alignment generated by a computer-assisted navigational surgical system is less than 1° (0.02°) in both planes in 95% of ankle joints. This calculation is based on a given center of the knee joint, and assumes a tibial length of 300 mm.
Discussion
The overall outcome of TKA depends on several factors, including patient selection, prosthetic design, soft tissue balancing, and accurate limb alignment Citation[1]. Accurate rotational and translational alignment of the prosthetic components is a critical factor having a significant influence on the outcome of TKA Citation[13]. An error in alignment of the prosthetic components in any of the anatomical planes can have a significant detrimental effect on the outcome Citation[1]. Inaccuracy in positioning or orientation of prosthetic implants can result in accelerated rates of wear, loosening of components, and consequent degraded functional performance Citation[14], Citation[15].
The introduction of computer-assisted knee arthroplasty surgery has the potential to reduce surgical errors in the alignment and rotation of prosthetic components, and therefore potentially improve the long-term outcomes and functional levels of patients who undergo TKA. This long-term surgical outcome is critically reliant on the accuracy of identification of the mechanical axis of the limb Citation[16]. Most computer-assisted systems for TKA currently use the mechanical axis of the tibia as a reference for the calculation of correct limb and prosthesis alignment and rotation Citation[17].
In the calculation of the mechanical axis of the tibia, a generally accepted method is to use the center of the ankle joint as an initial reference point. In determining this, the location of the center of the ankle joint may vary significantly depending on the position and number of points digitized on the skin, the anatomical structure, and potential variations of the subject's ankle, as well as the potential for variations in the interpretation of appropriate landmarks by the individual surgeon. Any consequent inaccuracy in the identification of the center of the ankle joint can significantly contribute to resultant inadequacies in the placement of prosthetic components. By definition, this has the potential to detrimentally influence the overall long-term outcome and success of knee arthroplasty surgery. Even with the use of currently available surgical navigation systems, the center of the ankle joint in the coronal plane is still estimated by the surgeon in the same manner as in standard non-navigated techniques. This offers the potential for error with no overall improvement in alignment.
It should be noted that this series demonstrates a significant difference in the calculation of the mid-point of the ankle joint in patients with anatomical variations, such as arthritic degeneration. It would therefore seem particularly relevant to exclude such degenerative change with the use of pre-operative X-ray assessment of the ipsilateral ankle joint.
The described method of determining the center of the ankle joint displayed a high degree of correlation and reproducibility between the values obtained by individual observers. Very narrow confidence intervals were obtained in each plane. It is therefore apparent that this algorithm can be relied on to give accurate measurements of the distances and ratios involved in the ankle joint in relation to computer-assisted knee navigation surgery. We advocate the use of such an algorithm as a tool to decrease the potential for surgical error in prosthetic alignment. Rather than encouraging complete reliance on such an algorithm, at the expense of intra-operative clinical judgment, the most relevant ongoing application of such a system would appear to be as a significant checkpoint in the surgical process of knee joint arthroplasty.
References
- Delp S L., Stulberg S D., Davies B, Picard F, Leitner F. Computer assisted knee replacement. Clin Orthop 1998; 354: 49–56
- Stern S H., Insall J N. Posterior stabilised prosthesis: results after follow-up of nine to twelve years. J Bone Joint Surg Am 1992; 74: 980–6
- Vince K G., Insall J N, Kelly M A. The total condylar prosthesis: 10 to 12 year results of a cemented knee replacement. J Bone Joint Surg Br 1989; 71: 793–7
- Dorr L D., Boiardo R A. Technical considerations in total knee arthroplasty. Clin Orthop 1986; 205: 5–11
- Stulberg S D., Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am 2002; 84(suppl 2)90–8
- Jeffery R S., Morris R W., Denham R A. Coronal alignment after total knee replacement. J Bone Joint Surg Br 1991; 73: 709–14
- Ritter M A., Faris P M., Keating E M., Meding J B. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop 1994; 299: 153–6
- Ecker M L., Lotke P A., Windsor R E., Cella J P. Long-term results after total condylar knee arthroplasty: significance of radiolucent lines. Clin Orthop 1987; 216: 151–8
- Garg A, Walker P S. Prediction of total knee motion using a three-dimensional computer-graphics model. J Biomech 1990; 23: 45–58
- Teter K E., Bregman D, Colwell C W. Accuracy of intramedullary versus extramedullary tibial alignment cutting systems in total knee arthroplasty. Clin Orthop 1995; 321: 106–10
- Stulberg S D., Picard K, Saragaglia D. Computer-assisted total knee replacement arthroplasty. Op Tech Orthop 2000; 10: 25
- Matsen F A., Garbini J L., Sidles J A., Pratt B, Baugarten P, Kaiura R. Robotic assistance in orthopaedic surgery: a proof of principle using distal femoral arthroplasty. Clin Orthop 1993; 296: 178–86
- Berger R A., Rubash H E., Seel M J., Thompson W H., Crossett L S. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop 1993; 286: 40–7
- Oswald M H., Jakob R P., Schneider E, Hoogewoud H M. Radiological analysis of normal axial alignment of femur and tibia in view of total knee arthroplasty. J Arthroplasty 1993; 8: 419–26
- Wasielewski R C., Galante J O., Leighty R M., Natarajan R N., Rosenberg A G. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop 1994; 299: 31–43
- Krackow K A., Bayers-Thering M, Phillips M J., Bayers-Thering M, Mihalko W M. A new technique for determining proper mechanical axis alignment during total knee arthroplasty: progress toward computer-assisted total knee arthroplasty. Orthopedics 1999; 22: 698–702
- Nofrini L, Slomczykowski M, Iacono F, Marcacci M. Evaluation of accuracy in ankle center location for tibial mechanical axis identification. J Invest Surg 2004; 17: 23–9