Abstract
Background and purpose — Few studies have addressed the association between early migration of femoral stems and late aseptic revision in total hip arthroplasty. We performed a meta-regression analysis on 2 parallel systematic reviews and meta-analyses to determine the association between early migration and late aseptic revision of femoral stems.
Patients and methods — Of the 2 reviews, one covered early migration data obtained from radiostereometric analysis (RSA) studies and the other covered long-term aseptic revision rates obtained from survival studies with endpoint revision for aseptic loosening. Stems were stratified according to the design concept: cemented shape-closed, cemented force-closed, and uncemented. A weighted regression model was used to assess the association between early migration and late aseptic revision, and to correct for confounders. Thresholds for acceptable and unacceptable migration were determined in accordance with the national joint registries (≤ 5% revision at 10 years) and the NICE criteria (≤ 10% revision at 10 years).
Results — 24 studies (731 stems) were included in the RSA review and 56 studies (20,599 stems) were included in the survival analysis review. Combining both reviews for the 3 design concepts showed that for every 0.1-mm increase in 2-year subsidence, as measured with RSA, there was a 4% increase in revision rate for the shape-closed stem designs. This association remained after correction for age, sex, diagnosis, hospital type, continent, and study quality. The threshold for acceptable migration of shape-closed designs was defined at 0.15 mm; stems subsiding less than 0.15 mm in 2 years had revision rates of less than 5% at 10 years, while stems exceeding 0.15 mm subsidence had revision rates of more than 5%.
Interpretation — There was a clinically relevant association between early subsidence of shape-closed femoral stems and late revision for aseptic loosening. This association can be used to assess the safety of shape-closed stem designs. The published research is not sufficient to allow us to make any conclusions regarding such an association for the force-closed and uncemented stems.
Over 1 million total hip arthroplasties (THAs) are performed every year worldwide, and this number is expected to double within the next 2 decades (CitationPivec et al. 2012). The design and method of fixation of a THA determines the stability of the implant, and these are therefore crucial factors for achievement of long-term survival. However, most of the new THA designs have been introduced onto the market without demonstrating good performance (CitationSheth et al. 2009). This has led to several THAs having high failure rates, such as the Charnley Elite Plus (CitationHauptfleisch et al. 2006). To prevent future disasters with orthopedic implants, several countries have developed guidelines to guarantee patient safety, e.g. the NICE guidelines (NHS). Furthermore, it has become increasingly evident that a phased evidence-based introduction, as is common with pharmaceuticals, is necessary to regulate the introduction of new THA designs to the market (CitationMalchau 2000, CitationMcCulloch et al. 2009, CitationSchemitsch et al. 2010). This should include systematic assessment and early detection of aseptic loosening in small groups of patients.
Although it may take as long as 10 years for aseptic loosening of implants to become manifest, it is possible to detect the loosening process as early as 1–2 years postoperatively, using radiostereometric analysis (RSA). Since RSA allows in vivo, 3D measurement of the migration of THAs with an accuracy of 0.2 mm for translations and 0.5 degrees for rotations, only a small number of patients is needed to compare a new innovative design to a gold-standard design (CitationGrewal et al. 1992, CitationKarrholm et al. 1994, CitationRyd et al. 1995, CitationThanner et al. 1995, CitationHauptfleisch et al. 2006, CitationNieuwenhuijse et al. 2012). Thus, only a few patients will have been exposed if that design turns out to be a poor one. RSA could therefore play an important role in phased evidence-based market introduction of new THA designs (CitationFaro and Huiskes 1992, CitationBulstrode et al. 1993, CitationMalchau 1995, Citation2000, CitationNelissen et al. 2011).
Following on from our 2 earlier studies on the association between early migration and late aseptic revision of tibial components and acetabular cups, this systematic review and meta-analysis focused on the femoral stem (CitationPijls et al. 2012a, Citationb). We hypothesized that early migration, as measured with RSA, is associated with late revision for aseptic loosening. We systematically reviewed the association between early migration and late revision for aseptic loosening of the femoral stem in primary THA. This could eventually lead to clinical guidelines, to be used in a phased introduction of new THA designs.
Material and methods
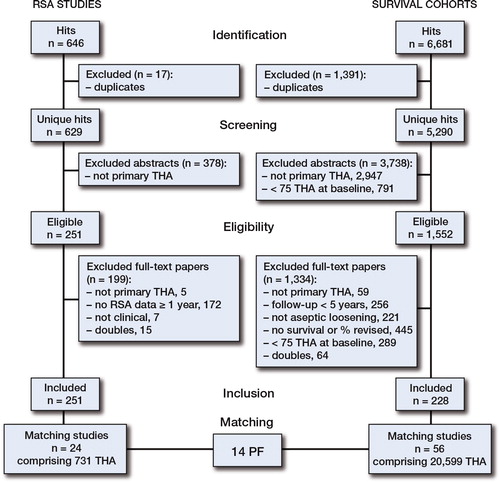
We performed a meta-regression analysis (international registration number NTR3129; www.trialregister.nl) combining RSA migration data with survival analysis data for each stem design, to assess the association between early migration and late aseptic revision. To this end, 2 parallel systematic reviews () and meta-analyses were performed on studies of patients treated with THA for primary osteoarthritis (OA), secondary osteoarthritis (SA), and fractures of the proximal femur (FF). One review covered early migration data on femoral stems, obtained from RSA studies. The other review covered long-term aseptic revision rates obtained from survival studies, with revision for aseptic loosening of femoral stems as the endpoint. The data were stratified according to the design concept of the femoral stem (i.e. cemented shape-closed, cemented force-closed, and uncemented) (CitationHuiskes et al. 1998). During all phases of the review process, author RN with over 20 years of experience of both RSA and THA, was available for consultation.
Figure 1. PRISMA flow chart of both reviews. Details of the 14 PF combinations can be found in Table 1.
Systematic review of RSA studies
Literature search. A literature search was performed in cooperation with a medical librarian (JP), to minimize publication bias (CitationVochteloo et al. 2010). The search strategy and bibliographies used were the same as in the systematic review and meta-analysis on early migration of acetabular cups in relation to late aseptic revision (CitationPijls et al. 2012a). Relevant articles were screened for additional references. Then a separate search was conducted in 9 leading orthopedic and biomechanical journals (Acta Orthop, Bone Joint J, Clin Orthop Relat Res, J Arthroplasty, J Bone Joint Surg Am, Knee Surg Sports Traumatol Arthrosc, J Orthop Res, J Biomech, and Clin Biomech). Finally, Google Scholar was used to search for additional relevant studies. Articles in English, French, Italian, Spanish, Dutch, and German were considered. The search strategy consisted of the following components—each defined by a combination of controlled vocabulary and free text terms: (1) RSA, and (2) joint replacement. More details of the strategy and glossary terms used can be found in the Appendix (see Supplementary data).
Inclusion and exclusion analysis. Initial screening based on the title and abstract of RSA studies was performed by BP to identify studies on patients treated with THA for OA, SA, or FF. In cases where the information in the abstract did not suffice or where there was any doubt, studies remained eligible. The full text of eligible studies was independently evaluated in duplicate by 2 reviewers (BP and MN). The inclusion criteria for RSA studies were (1) primary THA, and (2) a minimum RSA follow-up of 1 year, measuring femoral stem migration.
Data extraction. Migration data from RSA studies was independently extracted in duplicate by PV and MN. Since the failure mechanism of femoral stems involves subsidence and retroversion, the data extraction of RSA studies focused on subsidence and retroversion of the femoral stem in the first 2 postoperative years (CitationKarrholm et al. 1994). Data concerning patient demographics and regional influences were extracted to allow for confounder correction (CitationPijls et al. 2011). The design concept of different femoral stems (i.e. cemented shape-closed, cemented force-closed, or uncemented) was determined by RN.
Quality assessment. The quality of the RSA studies was independently appraised in duplicate by PV and JJ at the level of outcome using the AQUILA methodological score (CitationPijls et al. 2011). For the RSA studies, we modified the AQUILA score by removing items that were not considered relevant for appraisal of early migration: long-term follow-up and revision assessment.
Systematic review of survival studies
Literature search. The search strategy and bibliographies were comparable to those used in the RSA review, with the exception of the components of the search strategy. The search strategy for the survival studies consisted of the following components, each defined by a combination of controlled vocabulary and free text terms: (1) joint replacement, (2) implant failure, and (3) survival analysis. See http://informahealthcare.Appendix (Supplementary data) for more details of the strategy and glossary terms.
Inclusion and exclusion analysis. The procedure for screening of the survival studies for eligibility and subsequent inclusion and exclusion analysis was identical to the procedures for the RSA studies with the exception of the inclusion and exclusion criteria. The inclusion criteria for survival studies were (1) primary THA; (2) follow-up time of 5, 10, 15, 20, or 25 years (in the final analysis, only 10 years of follow-up was used); (3) endpoint being revision surgery for aseptic loosening of the femoral stem, or indication for revision surgery when there was poor general health or patient decline; and (4) survival or percentage revised being available for a specific follow-up period (see point 2). Studies with less than 75 THAs at baseline were excluded.
Data extraction. Revision rates for aseptic loosening of the femoral stem at 5-year intervals from survival studies were independently extracted in duplicate by PV and JJ. Data concerning patient demographics and regional influences were also extracted to allow for confounder correction. The design concept of different femoral stems was determined by RN.
Quality assessment. The quality of the survival studies was independently appraised in duplicate by PV and JJ at the level of outcome using the AQUILA methodological score (CitationPijls et al. 2011).
Analysis
The data were analyzed according to the same methodology as previously used in the systematic review and meta-analysis on early migration of acetabular cups in relation to late aseptic revision (CitationPijls et al. 2012a). A detailed description of the analysis, methodology, and a worked example are available in the online Appendix (see Supplementary data). The association between early migration and late revision was determined by matching the results from the RSA review to the results of the survival analysis review according to the type of prosthesis and fixation method (e.g. cemented or uncemented), here abbreviated to PF combination. Matching according to PF combination prevents confounding by PF combination, since PF combination is determined by technical factors known to be associated with both migration and a high likelihood of revision for aseptic loosening (CitationAJR 2013, CitationNJR 2012, CitationSHAR 2011). PF combinations were subsequently stratified according to design concept (i.e. cemented shape-closed, cemented force-closed, or uncemented). Depending on the studies available, it is possible that there would be more than 1 combination of matching of RSA and survival studies for a particular PF combination. For instance, if there are 3 RSA studies and 2 survival studies of the same PF combination, then there would be 6 possible combinations (3 × 2). All combinations were considered in the analysis. A meta-analysis for the revision rates at 10 years was performed. A model for the censoring mechanism was employed to reconstruct the data, and then a generalized linear mixed model with study as a random effect was applied to estimate the survival at 10 years and its confidence interval (CitationFiocco et al. 2009a, Citationb, CitationPutter et al. 2010, CitationFiocco et al. 2012). Regarding the RSA studies, pooling of migration results at the level of PF combinations was based on weights according to study size (N).
The 10-year results of THA with high revision rates are not likely to be published once 5-year published results show high revision rates. Since 10-year revision rates in the registries are on average 1.7 times higher than 5-year revision rates, any missing 10-year results were estimated from 5-year results by applying the factor 1.7. This method was validated by comparing the estimated 10-year results with the known 10-year results for the complete cases (CitationAJR 2013, CitationNJR 2012, CitationSHAR 2011).
Adjustment for confounding
Since RSA migration data and survival analysis data were extracted from different studies, it may be possible that differences between study populations might confound the observed association. In order to address this issue, we determined the degree of similarity of the study population between the RSA data and survival analysis data for the same stem design, expressed by a match score, for age, sex, diagnosis, hospital type, and continent. The match score has been constructed according to the results of a Delphi survey among an international group of 37 independent experts and can vary between 0 (poor) and 5 (excellent) (CitationPijls et al. 2011). This RSA study and the survival study combination scored 1 point for each of the following criteria (up to a maximum of 5 points): (1) the difference in mean age between patients from the RSA study and those from the survival study was 5 years or less; (2) the difference in percentage of females between the RSA study and the survival study was 10% or less; (3) the difference in percentage of patients diagnosed with primary osteoarthritis between the RSA study and the survival study was 10% or less; (4) the RSA study and the survival study were performed in a similar type of hospital (e.g. both in university medical centers); and (5) the RSA study and the survival study were performed on the same continent. All other cases scored zero points. We used a weighted regression model to assess the association between early migration and late aseptic revision, corrected for the influence of match score, quality of RSA study, quality of survival study, number of THAs in the RSA studies, and number of THAs in the survival studies.
Migration thresholds
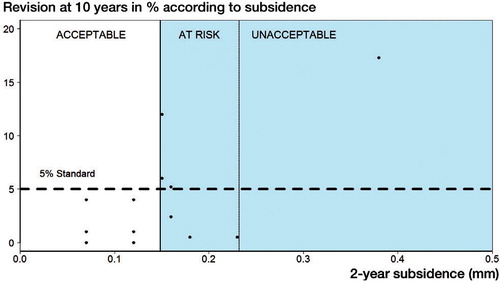
According to the principle of “primum non nocere“, new implant designs should perform at least as well as the revision standard of national registries with high validity: ≤ 3% revision at 5 years and ≤ 5% revision at 10 years according to the Swedish Hip Arthroplasty Register and the Australian National Joint Replacement Registry (CitationAJR, CitationSHAR). To have a safe margin, these more conservative criteria were chosen over the NICE criteria thresholds (i.e. 5% revision at 5 years and 10% revision at 10 years) (NHS). Based on the revision standard of the national registries, the following 3 categories were constructed for the phased introduction of new THA: “acceptable”, “at risk”, and “unacceptable”. The category “acceptable” was defined as the level of migration up to which all survival studies have lower revision rates than the standard. The category “unacceptable” was defined as the level of migration from which all revision rates are higher than the standard. The category “at risk” was defined as the migration interval between the “acceptable” and “unacceptable” thresholds, in which studies with revision rates lower and higher than the standard were observed.
Appraisal of publication bias
We assessed the potential effect of publication bias by comparing the results from the meta-analysis to the results from national joint registries, since they do not suffer from publication bias (CitationAJR 2013, CitationNJR 2012, CitationSHAR 2011). Accordingly, the PF combinations that perform better than average in the meta-analysis should also perform better than average in the national joint registries. The same principle also applies to PF combinations that perform worse than average. For this purpose, the pooled migration per specific combination of prosthesis type and fixation method was sorted according to revision rate and visualized in a dot chart.
Results
RSA studies. The literature search yielded 629 hits for the RSA review, and 24 studies (marked with • in the reference list) were included comprising 731 femoral stems (). The mean AQUILA methodological quality score of the RSA studies on a 7-point scale was 5.2 (SD 1.2). Subsidence of the femoral stem was the most frequently reported migration value: 1-year and 2-year subsidence was reported in 22 and 20 out of 27 RSA studies, respectively. Retroversion at 1 year and 2 years was reported in 10 and 13 RSA studies, respectively. Posterior head migration (translation along the z-axis) was reported infrequently and inconsistently, and did not allow a meaningful analysis.
Survival studies. The literature search generated 5,290 hits for the survival analysis review and 56 studies (marked with • in the reference list) were included with a total of 20,599 femoral stems (). The mean AQUILA methodological quality score of the survival studies on an 11-point scale was 7.0 (SD 2.1).
Early migration and late revision. The matching procedure resulted in 14 different PF combinations (i.e. type of prosthesis and fixation method) and 100 combinations of RSA and survival studies (). In the entire heterogeneous group of different PF combinations, there was no statistically significant (p > 0.05) association between migration, either subsidence or retroversion, and prosthesis survival (). Then we divided the PF combinations into more homogenous groups according to design concept: cemented shape-closed, cemented force-closed, and uncemented (CitationHuiskes et al. 1998). For the shape-closed femoral stems, there was an association between subsidence of shape-closed femoral stems and implant survival (). For every 0.1-mm increase in 2-year subsidence in shape-closed designs, there was a 4.2% (95% CI: 1.3–7.1; p < 0.05) increase in the aseptic revision rate at 10 years. This association remained significant after correction for RSA study quality, survival study quality, number of femoral stems in the RSA study, number of femoral stems in the survival study, and match score (all p-values < 0.05) (). The force-closed stems, consisting exclusively of the polished Exeter stem in the current meta-analysis, showed excellent long-term survival with no stems exceeding the revision threshold of 5% at 10 years (). Further analysis for the force-closed stems was considered inappropriate given the small number of PF combinations and the lack of contrast in revision rates (i.e. no high revision rates (> 5 %)) (). For the same reason, no meaningful analyses could be carried out for the uncemented stems since only 1 PF combination (Ribbed uncoated stem) showed a revision rate of more than 5% at 10 years. None of the design concepts showed an association between retroversion or continuous migration (i.e. 2-year migration minus 1-year migration) and implant survival.
Table 1. Details of prosthesis and fixation (PF) combinations
Figure 2. Scatter plot showing the subsidence at 2 years (in mm) and revision rate for aseptic loosening of the femoral stem at 10 years (percentage), categorized according to design concept (i.e. shape-closed, force-closed, uncemented).
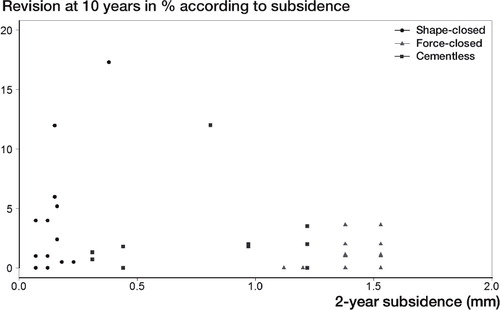
Figure 3. Scatter plot showing the association between 2-year subsidence (in mm) and revision rate for aseptic loosening of the shape-closed femoral stem at 10 years (percentage). The colored lines are derived from weighted regression according to match quality, survival study quality, and RSA quality (the coefficients and 95% CIs are presented in Table 2).
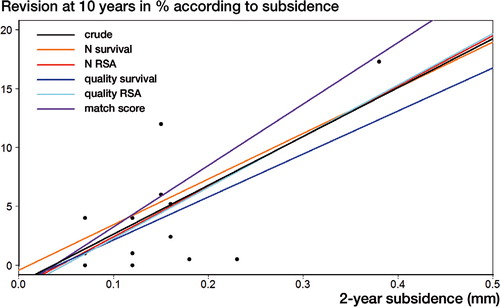
Table 2. Association between 2-year subsidence of shape-closed femoral stems and revision rate for aseptic loosening at 10 years. Increase in 10-year revision rate (%) for each 0.1-mm increase in subsidence at 2 years. In the crude analysis (unadjusted), 4.2% (95% CI: 1.3–7.1; p < 0.05) was added to the 10-year revision rate for every 0.1-mm increase in subsidence at 2 years
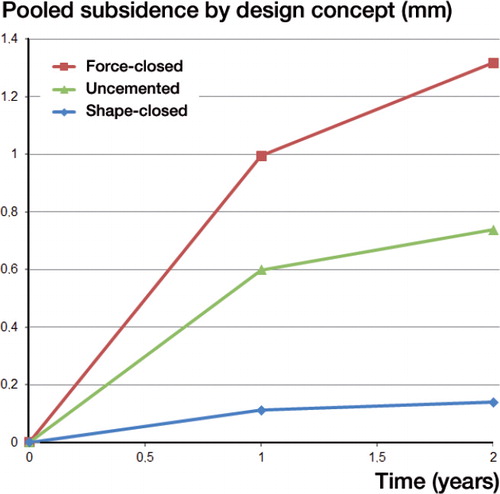
Early migration. The force-closed stems showed the largest amount of early subsidence, with a pooled mean subsidence of 1.0 mm (SE 0.05) and 1.3 mm (SE 0.01) at 1 and 2 years, respectively (). The pooled subsidence of the uncemented stems was in-between that of cemented force-closed and shape-closed stems. The uncemented stems showed a pooled mean subsidence of 0.6 mm (SE 0.08) at 1 year and 0.7 mm (SE 0.07) at 2 years. The shape-closed stems showed a pooled mean subsidence of 0.11 mm (SE 0.01) and 0.14 mm (SE 0.01) at 1 and 2 years, respectively.
Figure 4. Line chart of the pooled subsidence (in mm) up to 2 years, according to design concept (i.e. shape-closed, force-closed, uncemented). The standard errors were 0.05 mm and 1 mm (force-closed), 0.08 mm and 0.07 mm (uncemented), and 0.01 mm and 0.01 mm (shape-closed) at 1 and 2 years, respectively.
Migration thresholds. shows the 3 categories of the stems. Subsidence at 2 years was between 0 and 0.15 mm; there was no stem with more than 5% revision for aseptic loosening at 10 years. In the case of 2-year subsidence of more than 0.23 mm, there was no stem with less than 5% revision for aseptic loosening at 10 years. This indicates that accepting 5% revision at 10 years resulted in a threshold of 0.15 mm for acceptable subsidence at 2 years. The threshold for unacceptable subsidence is less distinct, given the lack of data points with an excessive revision rate. However, stems with a subsidence of more than 0.15 mm are at risk of early revision. Adoption of the NICE criteria (10% revision at 10 years) does not alter the threshold of acceptable subsidence of 0.15 mm at 10 years.
Figure 5. Scatter plot showing the 2-year subsidence and revision rate of shape-closed femoral stems for aseptic loosening at 10 years. The threshold of 0.15 mm for acceptable subsidence is shown. The threshold of 0.23 mm for unacceptable subsidence could be defined less precisely and is also shown. Adoption of the NICE criteria (10% revision at 10 years) did not alter these thresholds.
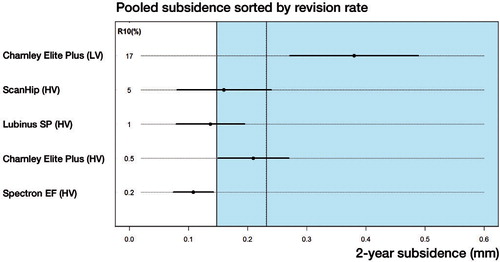
Publication bias. The pooled 2-year migration, ranked by the pooled 10-year revision rate for each PF combination, is presented in . The PF combinations that migrate less than the acceptable threshold (i.e. Lubinus SP and Spectron EF) have been—according to the Swedish Register—the most and the fourth most commonly used femoral components during the past 10 years, with survival rates of 98% and 97% at 10 years (SHAR). Conversely, the PF combinations that are classified as unacceptable on the basis of their pooled migration (i.e. Charnely Elite Plus) have been abandoned, and are no longer used (CitationHauptfleisch et al. 2006). These examples show that the possible influence of publication bias on the results is small.
Figure 6. Dot chart showing the pooled 2-year subsidence of shape-closed femoral stems ranked by the pooled 10-year revision rate for each PF combination. The threshold of 0.15 mm for acceptable subsidence is shown and the less precisely definable threshold for unacceptable subsidence (0.23) is also shown.
Discussion
The results of this meta-regression analysis, combining data from RSA studies and survival studies, show a clinically relevant association between early subsidence of shape-closed femoral stem designs, as measured with RSA, and clinical failure (i.e. aseptic revision surgery) at 10-year follow-up, corrected for age, sex, diagnosis, type of hospital, region, size of study, and quality of study. For every 0.1-mm increase in subsidence, the 10-year revision rate increases by mean 4% (95% CI: 1.3–7.1). The force-closed stem designs, which in the current meta-analysis consisted of only polished Exeter stems, showed the greatest amount of early subsidence and had excellent long-term survival with none of the stems exceeding the revision threshold of 5% at 10 years. This suggests that subsidence is beneficial for force-closed stems. However, more research with different force-closed stems is necessary to confirm this idea. The subsidence of the uncemented stems varied between that of cemented shape-closed stems and force-closed stems, and there was only 1 PF combination with a revision rate of more than 5% (Ribbed uncoated stem). The available data did not provide a clear pattern for identification of unsafe uncemented designs. Perhaps stabilization of migration is more suitable than the absolute value of migration for identification of unsafe uncemented femoral stems.
The results of our systematic review demonstrate that RSA studies can identify unsafe shape-closed femoral stems as early as 2 years postoperatively. Next to tibial components and acetabular components, our finding is another example of the potential of RSA for early identification of prostheses that perform less optimally (CitationPijls et al. 2012a, Citationb). Compared to the present policy of introduction of new prostheses, RSA has the potential to prevent widespread use of unsafe prostheses and save numerous patients from revision surgery.
The strengths of our systematic review have been the large number of studies included (78) and the large number of patients (> 20,000), which resulted in 14 different PF combinations. Although no association could be found between early migration and long-term aseptic revision for all PF combinations, the large variation in PF combinations gives us insight in the migration patterns of femoral stems. Since the migration and revision rates were from different studies, the RSA data could not have been used (incorporated) in the decision to perform a revision, so there was no incorporation bias. We considered that the influence of publication bias for the shape-closed femoral stems was small, since the results from the meta-analysis were similar to those from the national joint registries. Confounders only had a small influence on the association between early migration and long-term aseptic revision.
We should also consider some limitations. We were unable to find an association for the complete group of PF combinations and only found an association for the subgroup of shape-closed designs. This was due to the high variation in migration patterns of different PF combinations. The design concept (i.e. shape-closed, force-closed, or uncemented) of a THA determines its migration pattern, and every design concept should therefore be analyzed separately (CitationHuiskes et al. 1998). More research on each design concept is necessary to give a better understanding of acceptable and unacceptable migration for each of the concepts.
Furthermore, the quality of the survival studies and RSA studies showed a large degree of variation. A high methodological quality of all the studies included would have been desirable. Nevertheless, the quality of the survival studies and of the RSA studies showed only small effects on the association between migration and revision rate.
We should also take into account the fact that RSA only evaluates aseptic loosening. Although aseptic loosening is the foremost reason for failure, there are other failure mechanisms (e.g. infection, pain, and instability or pseudotumors in metal-on-metal total hip arthroplasty) which are not evaluated by RSA. RSA studies are therefore only the first step, after preclinical testing, in the phased introduction as proposed by both Faro and Huiskes and Malchau (CitationFaro and Huiskes 1992, CitationMalchau 1995, Citation2000). Several authors have pleaded for a phased evidence-based market introduction of new prostheses comparable to the introduction of new drugs to the consumer market (CitationMurray et al. 1995, CitationLiow and Murray 1997, CitationMuirhead-Allwood 1998, CitationMalchau 2000). During phase A, multiple single-center RSA studies should be performed to determine the safety of the THA regarding the risk of revision for aseptic loosening and wear. Thresholds for acceptable and unacceptable initial migration can be used for assessment of the new prosthesis (CitationMalchau 1995, Citation2000). Thus, the observed association in our study between early migration and long-term revision on shape-closed designed femoral stems can be adopted in phased evidence-based market introduction of new THAs. Given that the THA is safe, phase B studies must be conducted to evaluate the clinical performance of the THA regarding pain relief and functioning (clinical scores and patient-reported outcome measures (PROMS)) and to determine the rate of complications within a limited period that is feasible (e.g. severe adverse effects of the implant). Successful completion of phase B would allow introduction to the market and would herald phase C, where the performance of the THA must be monitored by post-marketing surveillance in national joint registries (CitationSchemitsch et al. 2010). This includes both the revision rate and patient evaluations using PROMS.
The Charnley Elite Plus stem is of special interest. This THA was introduced as successor to the well-established Charnley THA. It was assumed that small alterations in the design would enhance survival and patient outcome. However, early clinical studies gave conflicting findings, with some suggesting a similar outcome to that of the conventional Charnley stem, while others suggested a worse outcome (CitationKalairajah et al. 2004, CitationMakela et al. 2008). CitationHauptfleisch et al. (2006) found survival of 83% at 10 years, which was in accordance with their earlier predictions of high failure rates based on early RSA evaluation. These authors blamed the design of the Charnley Elite Plus for the poor survival. However, the cement used in that study was low-viscosity cement, and CitationDerbyshire et al. (2006) pointed out that the low-viscosity cement might also have been the reason for the poor survival (CitationDerbyshire et al. 2006). Our results suggest a similar reason: the pooled survival of the Charnley Elite Plus cemented with low-viscosity cement was far worse than the acceptable threshold. The same stem cemented with high-viscosity cement showed better survival, approaching the acceptable threshold. If the threshold of acceptable migration of the prosthesis had been known at the time the Charnley Elite Plus was introduced, it would have been classified as unacceptable after only 2 years of RSA follow-up. This example illustrates the clinical value of migration thresholds for early identification of THAs that have a high likelihood of failure at long-term follow-up. Moreover, this example highlights that not only design but also type of fixation should be taken into account when evaluating femoral stem survival. For the Charnley Elite Plus femoral stem, it was not only the design but also the fixation (low-viscosity or high-viscosity cement) that influenced both early migration and long-term survival. Labeling of femoral stems according to the PF (prosthesis and fixation) combination principle is therefore imperative.
Various authors and regulatory agencies recognize the potential of RSA (CitationKarrholm et al. 1994, CitationRyd et al. 1995, CitationMalchau 2000, CitationHauptfleisch et al. 2006). The NICE guidelines of 2003 require adequate long-term clinical data for hip prostheses and regard RSA as a promising technique that may be an early-warning indicator of expected poor long-term revision rates (NHS). Recently, the International Organization for Standardization (ISO) and the European Standards Working Group on Joint Replacement Implants published a standard protocol for early clinical studies that provides requirements for the clinical assessment of migration of orthopedic implants with RSA (ISO 16087:2013). The Dutch Orthopaedic Society now requires a phased introduction with mandatory RSA studies before any new THA is considered for introduction to the Dutch market (CitationSwierstra et al. 2011). In addition, new initiatives for increasing patient safety such as the Beyond Compliance Service not only support the stepwise introduction of new implants to the market, but also acknowledge the importance of training established surgeons how to use a new innovative design (the Beyond Compliance Advisory Group).
In conclusion, 2-year early migration of shape-closed design femoral stems is associated with 10-year revision for aseptic stem loosening. The proposed migration thresholds provide insight into the failure mechanism of shape-closed femoral stems. Too few RSA study and survival study combinations for force-closed and uncemented stem designs were found to give meaningful recommendations on the predictive value of early migration for aseptic revision of these designs. If more RSA migration studies are performed, the value of early migration profiles of these designs will be possible.
Supplementary data
Appendix is available at Acta’s website (www.actaorthop.org), identification number 7633.
IORT_A_1043832_SM1622.pdf
Download PDF (467.9 KB)RGN, BGP, and ERV conceived the study. SM provided methodological input and MF provided statistical input during the conceptual phase of the study. JWP designed the search strategy for the literature search. PV, BGP, MJN, and JJ performed the study selection and matching procedure. PV and JJ appraised the quality of the literature and performed the data extraction. MF and BGP analyzed the data. PV, BGP, ERV, and RGN wrote the initial draft of the manuscript. MF and SM ensured the accuracy of the data and analysis. BGP and MF wrote the Appendix. Critical revision of the manuscript was done by all the authors.
We thank the Atlantic Innovation Fund (Atlantic Canada Opportunities Agency; contract number 191933), the Dutch Arthritis Association (project number LLP13; 08-1-300), and the European Information and Communication Technologies Community Seventh Framework Programme (FP7/2007-2013; grant agreement number 248693) for providing funding for this study. The Atlantic Innovation Fund, the Dutch Arthritis Association, and the European Information and Communication Technologies Community Seventh Framework Programme did not take part in the design or performance of the study; in the collection, management, analysis, or interpretation of the data; or in preparation, review, or approval of the manuscript.
Statistical code and dataset are available from the corresponding author upon request. R code for the analysis described in the Appendix is available from one of the authors (e-mail [email protected]).
- Adam F, Pape D, Johann S, Kohn D. Postoperative migration of cementless titanium hip-stems. Clinical study with Roentgen Stereometric Analysis (RSA). J Bone Joint Surg Br 2004; 86-B: 377-37e.
- AJR. Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2013: https://aoanjrr.dmac.adelaide.edu.au/nl/annual-reports-2013.
- Aldinger P R, Breusch S J, Lukoschek M, Mau H, Ewerbeck V, Thomsen M. A ten- to 15-year follow-up of the cementless Spotorno stem. J Bone Joint Surg Br 2003a; 85 (2): 209-14.
- Aldinger P R, Thomsen M, Mau H, Ewerbeck V, Breusch S J. Cementless Spotorno tapered titanium stems: excellent 10-15-year survival in 141 young patients. Acta Orthop Scand 2003b; 74 (3): 253-8.
- Alfaro-Adrian J, Gill H S, Murray D W. Cement migration after THR. A comparison of Charnley Elite and Exeter femoral stems using RSA. J Bone Joint Surg Br 1999; 81 (1): 130-4.
- Alfaro-Adrian J, Gill HS, Murray DW. Should total hip arthroplasty femoral components be designed to subside? A radiostereometric analysis study of the Charnley Elite and Exeter stems. J Arthroplasty 2001; 16 (5): 598-606.
- Badhe N P, Quinnell R C, Howard P W. The uncemented Bi-Contact total hip arthroplasty. J Arthroplasty 2002; 17 (7): 896-901.
- Badhe S, Livesley P. Early polyethylene wear and osteolysis with ABG acetabular cups (7- to 12-year follow-up). Int Orthop 2006; 30 (1): 31-4.
- The Beyond Compliance Advisory Group. http://www.beyondcompliance.org.uk.
- Bulstrode CJ, Murray DW, Carr AJ, Pynsent PB, Carter SR. Designer hips. BMJ 1993; 306 (6880): 732-3.
- Canales C V, Panisello Sebastia J J, et al. Ten-year follow-up of an anatomical hydroxyapatite-coated total hip prosthesis. Int Orthop 2006; 30 (2): 84-90.
- Capello W N, D’Antonio J A, Feinberg J R, Manley M T, Naughton M. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty 2008; 23 (7 Suppl): 39-43.
- Castoldi F, Rossi R, La Russa M, Sibelli P, Rossi P, Ranawat A S. Ten-year survivorship of the Anatomique Benoist Girard I total hip arthroplasty. J Arthroplasty 2007; 22 (3): 363-8.
- Chen F S, Di Cesare P E, Kale A A, et al. Results of cemented metal-backed acetabular components: a 10-year-average follow-up study. J Arthroplasty 1998; 13 (8): 867-73.
- Chiu K H, Shen W Y, Tsui H F, Chan K M. Experience with primary Exeter total hip arthroplasty in patients with small femurs - Review at average follow-up period of 6 years. J Arthroplasty 1997; 12 (3): 267-72.
- Chiu K H, Shen W Y, Cheung K W, Tsui H F. Primary Exeter total hip arthroplasty in patients with small femurs: a minimal of 10 years follow-up. J Arthroplasty 2005; 20 (3): 275-81.
- de Kam D C, Klarenbeek R L, Gardeniers J W, Veth R P, Schreurs B W. The medium-term results of the cemented Exeter femoral component in patients under 40 years of age. J Bone Joint Surg Br 2008; 90 (11): 1417-21.
- Derbyshire B, Porter ML. Re: the premature failure of the Charnley Elite-Plus stem: a confirmation of RSA predictions. J Bone Joint Surg Br 2006; 88 (12): 1676; author reply -7.
- Derbyshire B, Porter M L. A study of the Elite Plus femoral component using radiostereometric analysis. J Bone Joint Surg Br 2007; 89 (6): 730-5.
- Digas G, Thanner J, Anderberg C, Karrholm J. Fluoride-containing acrylic bone cement in total hip arthroplasty. Randomized evaluation of 97 stems using radiostereometry and dual-energy X-ray absorptiometry. J Arthroplasty 2005; 20 (6): 784-92.
- Digas G, Karrholm J, Thanner J. Addition of fluoride to acrylic bone cement does not improve fixation of a total hip arthroplasty stem. Clin Orthop Relat Res 2006; 448: 58-66.
- Eingartner C, Volkmann R, Winter E, et al. Results of an uncemented straight femoral shaft prosthesis after 9 years of follow-up. J Arthroplasty 2000; 15 (4): 440-7.
- Eingartner C, Heigele T, Dieter J, Winter E, Weise K. Long-term results with the BiCONTACT system--aspects to investigate and to learn from. Int Orthop 2003; 27 Suppl 1: S11-5.
- Epinette J A, Manley M T. Uncemented stems in hip replacement--hydroxyapatite or plain porous: does it matter? Based on a prospective study of HA Omnifit stems at 15-years minimum follow-up. Hip Int 2008; 18 (2): 69-74.
- Espehaug B, Havelin L I, Engesaeter L B, Vollset S E, Langeland N. Early revision among 12,179 hip prostheses - A comparison of 10 different brands reported to the Norwegian Arthroplasty Register, 1987-1993. Acta Orthop Scand 1995; 66 (6): 487-93.
- Faro L M, Huiskes R. Quality assurance of joint replacement. Legal regulation and medical judgement. Acta Orthop Scand Suppl 1992; 250: 1-33.
- Fiocco M, Putter H, van Houwelingen J C. Meta-analysis of pairs of survival curves under heterogeneity: a Poisson correlated gamma-frailty approach. Stat Med 2009a; 28 (30): 3782-97.
- Fiocco M, Putter H, Van Houwelingen J C. A new serially correlated gamma-frailty process for longitudinal count data. Biostatistics 2009b; 10 (2): 245-57.
- Fiocco M, Stijnen T, Putter H. Meta-analysis of time-to-event outcomes using a hazard-based approach: Comparison with other models, robustness and meta-regression. Computational Statistics and Data Analysis 2012; 56 (5): 1028-37.
- Gallo J, Langova K, Havranek V, Cechova I. Poor survival of ABG I hip prosthesis in younger patients. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2008; 152 (1): 163-8.
- Garellick G, Malchau H, Regner H, Herberts P. The Charnley versus the Spectron hip prosthesis: radiographic evaluation of a randomized, prospective study of 2 different hip implants. J Arthroplasty 1999; 14 (4): 414-25.
- Garellick G, Malchau H, Herberts P. Survival of hip replacements. A comparison of a randomized trial and a registry. Clin Orthop Relat Res 2000; (375): 157-67.
- Gill H S, Alfaro-Adrian J, Alfaro-Adrian C, McLardy-Smith P, Murray D W. The effect of anteversion on femoral component stability assessed by radiostereometric analysis. J Arthroplasty 2002; 17 (8): 997-1005.
- Glyn-Jones S, Hicks J, Alfaro-Adrian J, Gill H S, McLardy-Smith P, Murray D W. The influence of cement viscosity on the early migration of a tapered polished femoral stem. Int Orthop 2003; 27 (6): 362-5.
- Glyn-Jones S, Alfaro-Adrian J, Murray D W, Gill H S. The influence of surgical approach on cemented stem stability: an RSA study. Clin Orthop Relat Res 2006; 448: 87-91.
- Grant P, Aamodt A, Falch J A, Nordsletten L. Differences in stability and bone remodeling between a customized uncemented hydroxyapatite coated and a standard cemented femoral stem A randomized study with use of radiostereometry and bone densitometry. J Orthop Res 2005; 23 (6): 1280-5.
- Grewal R, Rimmer M, Freeman M. Early migration of prostheses related to long-term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg Br 1992; 74 (2): 239-42.
- Guther D, Pap G, Bamert P, Eggli S. [Long-term results with the cemetless CLS stem in hip replacement]. Z Orthop Ihre Grenzgeb 2003; 141 (3): 309-15.
- Hallan G, Lie S A, Furnes O, Engesaeter L B, Vollset S E, Havelin L I. Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br 2007; 89 (12): 1574-80.
- Hauptfleisch J, Glyn-Jones S, Beard D J, Gill H S, Murray D W. The premature failure of the Charnley Elite-Plus stem: a confirmation of RSA predictions. J Bone Joint Surg Br 2006; 88 (2): 179-83.
- Havelin L I, Engesaeter L B, Espehaug B, Furnes O, Lie S A, Vollset S E. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71 (4): 337-53.
- Herrera A, Canales V, Anderson J, Garcia-Araujo C, Murcia-Mazon A, Tonino A J. Seven to 10 years followup of an anatomic hip prosthesis: an international study. Clin Orthop Relat Res 2004; (423): 129-37.
- Hook S, Moulder E, Yates P J, Burston B J, Whitley E, Bannister G C. The Exeter Universal stem: a minimum ten-year review from an independent centre. J Bone Joint Surg Br 2006; 88 (12): 1584-90.
- Hozack W J, Rothman R H, Eng K, Mesa J. Primary cementless hip arthroplasty with a titanium plasma sprayed prosthesis. Clin Orthop Relat Res 1996; (333): 217-25.
- Huiskes R, Verdonschot N, Nivbrant B. Migration, stem shape, and surface finish in cemented total hip arthroplasty. Clin Orthop Relat Res 1998; (355): 103-12.
- ISO. Implants for surgery -Roentgen stereophotogrammetric analysis for the assessment of migration of orthopaedic implants (16087:2013): http://www.iso.org/iso/home/store/catalogue_tc/catalogue_detail.htm?csnumber=55662.
- Issack P S, Botero H G, Hiebert R N, et al. Sixteen-year follow-up of the cemented spectron femoral stem for hip arthroplasty. J Arthroplasty 2003; 18 (7): 925-30.
- Iwase T, Wingstrand I, Persson B M, Kesteris U, Hasegawa Y, Wingstrand H. The ScanHip total hip arthroplasty: radiographic assessment of 72 hips after 10 years. Acta Orthop Scand 2002; 73 (1): 54-9.
- Jacobsson S A, Ivarsson I, Djerf K, Wahlstrom O. Stem loosening more common with ITH than Lubinus prosthesis - a 5-year clinical and radiographic follow-up of 142 patients. Acta Orthop Scand 1995; 66 (5): 425-31.
- Johnsson R, Franzen H, Nilsson L T. Combined survivorship and multivariate analyses of revisions in 799 hip prostheses. A 10- to 20-year review of mechanical loosening. J Bone Joint Surg Br 1994; 76 (3): 439-43.
- Kalairajah Y, Azurza K, Molloy S, Hulme C, Cronin M, Drabu K J. Is the Charnley evolution working? A five-year outcome study. Acta Orthop Belg 2004; 70 (4): 315-21.
- Kale A A, Della Valle C J, Frankel V H, Stuchin S A, Zuckerman J D, Di Cesare P E. Hip arthroplasty with a collared straight cobalt-chrome femoral stem using second-generation cementing technique - A 10-year-average follow-up study. J Arthroplasty 2000; 15 (2): 187-93.
- Karrholm J, Snorrason F. Subsidence, tip, and hump micromovements of noncoated ribbed femoral prostheses. Clin Orthop Relat Res 1993; (287): 50-60.
- Karrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br 1994; 76 (6): 912-7.
- Kim Y H, Kim J S, Yoon S H. Long-term survivorship of the Charnley Elite Plus femoral component in young patients. J Bone Joint Surg Br 2007; 89 (4): 449-54.
- Lee G Y, Srivastava A, D’Lima D D, Pulido P A, Colwell C WJr. Hydroxyapatite-coated femoral stem survivorship at 10 years. J Arthroplasty 2005; 20 (7 Suppl 3): 57-62.
- Lewthwaite S C, Squires B, Gie G A, Timperley A J, Ling R S M. The Exeter (TM) Universal hip in patients 50 years or younger at 10-17 years’ followup. Clin Orthop Relat Res 2008; 466 (2): 324-31.
- Liow R Y, Murray D W. Which primary total knee replacement? A review of currently available TKR in the United Kingdom. Ann R Coll Surg Engl 1997; 79 (5): 335-40.
- Makela K, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older: results of the 12 most common cemented implants followed for 25 years in the Finnish Arthroplasty Register. J Bone Joint Surg Br 2008; 90B (12): 1562-9.
- Malchau H. On the importance of stepwise introduction of new hip implant technology: assessment of total hip replacement using clinical evaluation, radiostereometry, digitised radiography and a national hip registry. Ortopedisk kirurgi 1995.
- Malchau H. Introducing new technology: a stepwise algorithm. Spine (Phila Pa 1976) 2000; 25 (3): 285.
- Manley M T, Capello W N, D’Antonio J A, Edidin A A, Geesink R G T. Fixation of acetabular cups without cement in total hip arthroplasty - A comparison of three different implant surfaces at a minimum duration of follow-up of five years. J Bone Joint Surg Am 1998; 80A (8): 1175-85.
- McCombe P, Williams S A. A comparison of polyethylene wear rates between cemented and cementless cups. A prospective, randomised trial. J Bone Joint Surg Br 2004; 86 (3): 344-9.
- McCulloch P, Altman D G, Campbell W B, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009; 374 (9695): 1105-12.
- McLaughlin J R, Lee K R. Total hip arthroplasty with an uncemented femoral component - Excellent results at ten-year follow-up. J Bone Joint Surg Br 1997; 79B (6): 900-7.
- McLaughlin J R, Lee K R. Total hip arthroplasty in young patients. 8- to 13-year results using an uncemented stem. Clin Orthop Relat Res 2000; (373): 153-63.
- McLaughlin J R, Lee K R. The outcome of total hip replacement in obese and non-obese patients at 10-to 18-years. J Bone Joint Surg Br 2006; 88B (10): 1286-92.
- McLaughlin J R, Lee K R. Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am 2008; 90 (6): 1290-6.
- Min B W, Song K S, Bae K C, Cho C H, Kang C H, Kim S Y. The effect of stem alignment on results of total hip arthroplasty with a cementless tapered-wedge femoral component. J Arthroplasty 2008; 23 (3): 418-23.
- Mjoberg B, Selvik G, Hansson L I, Rosenqvist R, Onnerfalt R. Mechanical loosening of total hip prostheses. A radiographic and roentgen stereophotogrammetric study. J Bone Joint Surg Br 1986; 68 (5): 770-4.
- Mjoberg B, Franzen H, Selvik G. Early detection of prosthetic-hip loosening. Comparison of low- and high-viscosity bone cement. Acta Orthop Scand 1990; 61 (3): 273-4.
- Muirhead-Allwood S K. Lessons of a hip failure. BMJ 1998; 316 (7132): 644.
- Murray D W, Carr A J, Bulstrode C J. Which primary total hip replacement? J Bone Joint Surg Br 1995; 77 (4): 520-7.
- Myers G J C, Morgan D, O’Dwyer K. Exeter-Ogee total hip replacement using the Hardinge approach; the ten to twelve year results. Hip Int 2008; 18 (1): 35-9.
- Nelissen R G, Garling E H, Valstar E R. Influence of cement viscosity and cement mantle thickness on migration of the Exeter total hip prosthesis. J Arthroplasty 2005; 20 (4): 521-8.
- Nelissen R G, Pijls B G, Karrholm J, Malchau H, Nieuwenhuijse M J, Valstar E R. RSA and registries: the quest for phased introduction of new implants. J Bone Joint Surg Am 2011; 93 Suppl 3: 62-5.
- NHS. National Institute for Clinical Excellence. Guidance on the selection of prostheses for primary total hip replacement. : http://www.nice.org.uk/nicemedia/pdf/Guidance_on_the_selection_of_hip_prostheses.pdf.
- Nieuwenhuijse M J, Valstar E R, Kaptein B L, Nelissen R G. Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups. Results from ten years of follow-up with roentgen stereophotogrammetric analysis (RSA). J Bone Joint Surg Am 2012; 94 (10): 874-80.
- Nivbrant B, Karrholm J, Soderlund P. Increased migration of the SHP prosthesis: radiostereometric comparison with the Lubinus SP2 design in 40 cases. Acta Orthop Scand 1999; 70 (6): 569-77.
- Nivbrant B, Karrholm J, Rohrl S, Hassander H, Wesslen B. Bone cement with reduced proportion of monomer in total hip arthroplasty: preclinical evaluation and randomized study of 47 cases with 5 years’ follow-up. Acta Orthop Scand 2001; 72 (6): 572-84.
- NJR. New Zealand National Joint Registry Annual Report 2012 (fourteen year report): http://www.nzoa.org.nz/nz-joint-registry.
- Nordsletten L, Aamodt A, Benum P, Grant P. The Unique customized prosthesis (UCP) is more stable than the cemented Elite Plus femoral stem. A randomized prospective study with radiostereometric one year follow up. J Bone Joint Surg Br 2004; 86-B: 401-40d.
- Ochs U, Eingartner C, Volkmann R, et al. >Prospective long-term follow-up of the cementless bicontact hip stem with plasmapore coating. Z Orthop Unfall 2007; 145 Suppl 1: S3-8.
- Ohnsorge J A, Davis J, Maus U, Saklak M, Weisskopf M, Wirtz D C. >Early polyethylene wear and excessive acetabular granuloma in an uncemented HA-coated total hip arthroplasty--midterm results of a prospective study. HSS J 2006; 2 (2): 114-20.
- Olofsson K, Digas G, Karrholm J. Influence of design variations on early migration of a cemented stem in THA. Clin Orthop Relat Res 2006; 448: 67-72.
- Oosterbos C J, Rahmy A I, Tonino A J. Hydroxyapatite coated hip prosthesis followed up for 5 years. Int Orthop 2001; 25 (1): 17-21.
- Oosterbos C J, Rahmy A I, Tonino A J, Witpeerd W. High survival rate of hydroxyapatite-coated hip prostheses: 100 consecutive hips followed for 10 years. Acta Orthop Scand 2004; 75 (2): 127-33.
- Parvizi J, Sharkey P F, Hozack W J, Orzoco F, Bissett G A, Rothman R H. Prospective matched-pair analysis of hydroxyapatite-coated and uncoated femoral stems in total hip arthroplasty. A concise follow-up of a previous report. J Bone Joint Surg Am 2004; 86-A (4): 783-6.
- Pijls B G, Dekkers O M, Middeldorp S, Valstar E R, van der Heide H J, Van der Linden-Van der Zwaag H M, Nelissen R G. AQUILA: assessment of quality in lower limb arthroplasty. An expert Delphi consensus for total knee and total hip arthroplasty. BMC Musculoskelet Disord 2011; 12: 173.
- Pijls B G, Nieuwenhuijse M J, Fiocco M, Plevier J W, Middeldorp S, Nelissen R G, Valstar E R. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survivalstudies. Acta Orthop Scand 2012a; 83 (6): 583-91.
- Pijls B G, Valstar E R, Nouta K A, Plevier J W, Fiocco M, Middeldorp S, Nelissen R G. Early migration of tibial components is associated with late revision: a systematic review and meta-analysis of 21,000 knee arthroplasties. Acta Orthop Scand 2012b; 83 (6): 614-24.
- Pivec R, Johnson A J, Mears S C, Mont M A. Hip arthroplasty. Lancet 2012; 380 (9855): 1768-77.
- Poon P C, Rennie J, Gray D H. Review of total hip replacement. The Middlemore Hospital experience, 1980-1991. N Z Med J 2001; 114 (1133): 254-6.
- Purtill J J, Rothman R H, Hozack W J, Sharkey P F. Total hip arthroplasty using two different cementless tapered stems. Clin Orthop Relat Res 2001; (393): 121-7.
- Putter H, Fiocco M, Stijnen T. Meta-analysis of diagnostic test accuracy studies with multiple thresholds using survival methods. Biom J 2010; 52 (1): 95-110.
- Rogers A, Kulkarni R, Downes E M. The ABG hydroxyapatite-coated hip prosthesis: one hundred consecutive operations with average 6-year follow-up. J Arthroplasty 2003; 18 (5): 619-25.
- Ryd L, Albrektsson B E, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br 1995; 77 (3): 377-83.
- Savilahti S, Myllyneva I, Lindholm T S, Pajamaki K J, Nevalainen J, Laippala P. Clinical outcome and survival of Link RS total hip prosthesis. J Bone Joint Surg Br 1995; 77 (3): 369-73.
- Schemitsch E H, Bhandari M, Boden S D, et al. The evidence-based approach in bringing new orthopaedic devices to market. J Bone Joint Surg Am 2010; 92 (4): 1030-7.
- Schramm M, Keck F, Hohmann D, Pitto R P. Total hip arthroplasty using an uncemented femoral component with taper design: outcome at 10-year follow-up. Arch Orthop Trauma Surg 2000; 120 (7-8): 407-12.
- Schreiner U, Scheller G, Herbig J, Jani L. Mid-term results of the cementless CLS stem. A 7- to 11-year follow-up study. Arch Orthop Trauma Surg 2001; 121 (6): 321-4.
- SHAR. Swedish Hip Arthroplasty Registry Report 2011: http://www.shpr.se/en/Publications/DocumentsReports.aspx.
- Sheth U, Nguyen N A, Gaines S, Bhandari M, Mehlman C T, Klein G. New orthopedic devices and the FDA. J Long Term Eff Med Implants. 2009; 19 (3): 173-84.
- Siebold R, Scheller G, Schreiner U, Jani L. [Long-term results with the cement-free Spotorno CLS shaft]. Orthopade 2001; 30 (5): 317-22.
- Soballe K, Christensen F. Calcar resorption after total hip arthroplasty. J Arthroplasty 1988; 3 (2): 103-7.
- Soballe K, Christensen F, Luxhoj T. Hip replacement in obese patients. Acta Orthop Scand 1987a; 58 (3): 223-5.
- Soballe K, Olsen N J, Ejsted R, Christensen F, Luxhoj T. Revision of the uncemented hip prosthesis. Acta Orthop Scand 1987b; 58 (6): 630-3.
- Spotorno L, Romagnoli S, Ivaldo N, et al. The CLS system. Theoretical concept and results. Acta Orthop Belg 1993; 59 Suppl 1: 144-8.
- Stefansdottir A, Franzen H, Johnsson R, Ornstein E, Sundberg M. Movement pattern of the Exeter femoral stem; a radiostereometric analysis of 22 primary hip arthroplasties followed for 5 years. Acta Orthop Scand 2004; 75 (4): 408-14.
- Steimer O, Adam F, Johann S, Pape D. [Primary stability of cementless implanted hip stems made of titanium alloy with metaphyseal fixation. A prospective clinical Roentgen-Stereometry-Analysis (RSA) study]. Z Orthop Ihre Grenzgeb 2006; 144 (6): 587-93.
- Strom H, Mallmin H, Milbrink J, Petren-Mallmin M, Nivbrant B, Kolstad K. The cone hip stem: a prospective study of 13 patients followed for 5 years with RSA. Acta Orthop Scand 2003; 74 (5): 525-30.
- Strom H, Kolstad K, Mallmin H, Sahlstedt B, Milbrink J. Comparison of the uncemented Cone and the cemented Bimetric hip prosthesis in young patients with osteoarthritis: an RSA, clinical and radiographic study. Acta Orthop Scand 2006; 77 (1): 71-8.
- Swierstra B A, Vervest A M, Walenkamp G H, et al. Dutch guideline on total hip prosthesis. Acta Orthop Scand 2011; 82 (5): 567-76.
- Tarasevicius S, Kesteris U, Robertsson O, Smailys A, Janusonis V, Wingstrand H. Introduction of total hip arthroplasty in Lithuania: results from the first 10 years. Acta Orthop Scand 2007; 78 (4): 454-7.
- Thanner J, Freij-Larsson C, Karrholm J, Malchau H, Wesslen B. Evaluation of Boneloc. Chemical and mechanical properties, and a randomized clinical study of 30 total hip arthroplasties. Acta Orthop Scand 1995; 66 (3): 207-14.
- Thien T M, Ahnfelt L, Eriksson M, Stromberg C, Karrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem - A prospective randomized comparison using radiostereometry. Acta Orthop Scand 2007; 78 (6): 730-8.
- Tonino A J, Rahmy A I. The hydroxyapatite-ABG hip system: 5- to 7-year results from an international multicentre study. The International ABG Study Group. J Arthroplasty 2000; 15 (3): 274-82.
- Vochteloo A J, Pijls B G, van der Heide H J. Sutures v staples. Let’s add three other studies. BMJ 2010; 340: c2627.
- Volkmann R, Eingartner C, Winter E, Weise K, Weller S. Midterm results in 500 titanium alloy straight femoral stem prostheses-cemented and cementless technique. Eur J Ortho Surg Traumatol 1998; 8 (3): 133-9.
- von Schewelov T, Sanzen L, Onsten I, Carlsson A. Catastrophic failure of an uncemented acetabular component due to high wear and osteolysis - An analysis of 154 Omnifit prostheses with mean 6-year follow-up. Acta Orthop Scand 2004; 75 (3): 283-94.
- Weise K, Eingartner C, Winter E. [Cemented versus uncemented hip replacement--rational decision making using the BiCONTACT total hip system]. Zentralbl Chir 2003; 128 (1): 46-52.
- Williams H D, Browne G, Gie G A, Ling R S, Timperley A J, Wendover N A. The Exeter universal cemented femoral component at 8 to 12 years. A study of the first 325 hips. J Bone Joint Surg Br 2002; 84 (3): 324-34.
- Wingstrand I, Persson B M, Wingstrand H. Total hip replacement with second generation cementing technique and the monobloc ScanHip: a 10-year follow-up. Int Orthop 2002; 26 (2): 69-71.
- Wykman A, Lundberg A. Subsidence of porous coated noncemented femoral components in total hip arthroplasty. A roentgen stereophotogrammetric analysis. J Arthroplasty 1992; 7 (2): 197-200.
- Wykman A, Selvik G, Goldie I. Subsidence of the femoral component in the noncemented total hip. A roentgen stereophotogrammetric analysis. Acta Orthop Scand 1988; 59 (6): 635-7.
- Wykman A, Olsson E, Axdorph G, Goldie I. Total hip arthroplasty. A comparison between cemented and press-fit noncemented fixation. J Arthroplasty 1991; 6 (1): 19-29.
- Yoo J J, Kim Y M, Yoon K S, Koo K H, Song W S, Kim H J. Alumina-on-alumina total hip arthroplasty. A five-year minimum follow-up study. J Bone Joint Surg Am 2005; 87 (3): 530-5.
- Young L, Duckett S, Dunn A. The use of the cemented Exeter Universal femoral stem in a District General Hospital: a minimum ten-year follow-up. J Bone Joint Surg Br 2009; 91 (2): 170-5.
