ABSTRACT
Interprofessional education is expected to promote collaborative practice and should therefore be included in health professionals’ curricula. Reports on interprofessional curricular development and its evaluation are rare. We therefore undertook a comprehensive quantitative and qualitative evaluation of a new, mandatory course on interprofessional collaboration for medical students during their third year of the Bachelor of Medicine study programme. The newly developed and implemented course spans over six weeks and was designed in a hybrid, flipped-classroom format. It incorporates experience- and case-based learning as well as interactions with other health professionals. Each student completes an eLearning and a clinical workshadowing individually before attending the – due to the pandemic – virtual live lectures. To assess quality and usefulness of teaching-learning formats and course structure to learn about interprofessional collaboration and to develop interprofessional competencies and identity, a quantitative and qualitative evaluation was performed with more than 280 medical students and 26 nurse educators from teaching hospitals using online surveys (open & closed-ended format). Data were analyzed descriptively and using content analysis processes. Students appreciated the flipped-classroom concept, the real-world case-based learning scenarios with interprofessional lecturer teams, and the possibility of an experience-based learning opportunity in the clinical setting including interaction with students and professionals from other health professions. Interprofessional identity did not change during the course. Evaluation data showed that the course is a promising approach for teaching-learning interprofessional competencies to medical students. The evaluation revealed three factors that determined the success of this course, namely, a flipped-classroom concept, the individual workshadowing of medical students with another health professional, mainly nurses, and live sessions with interprofessional teaching-learning teams. The course structure and teaching-learning methods showed potential and could serve as a template for interprofessional course development in other institutions and on other course topics.
Introduction
Interprofessional collaboration is essential to master the rapid increase in knowledge and the continuous specialization in health care [Citation1]. Interprofessional education, as defined by the World Health Organization (2010), occurs when two or more professions learn about, from and with one another to enable effective collaboration and improve health outcomes [Citation1,Citation2]. It is widely accepted that interprofessional education that is incorporated into the basic training of health professionals improves interprofessional collaboration [Citation2–4]. Recent reviews on interprofessional education unanimously report improved outcomes in students’ attitudes, perceptions of other professionals, and collaborative knowledge and skills [Citation5–11].
In practice, however, the integration of interprofessional education and the acquisition of interprofessional competencies remain challenging. The development and implementation of suitable teaching-learning formats and methods is necessary to promote students’ ability for interprofessional collaboration [Citation1,Citation3,Citation4]. The reporting of curricula development in interprofessional education and its evaluation is therefore necessary to develop evidence-based teaching-learning methods [Citation12].
Background
As part of a medical curriculum revision in 2019 for Bachelor students in Switzerland, interprofessional collaboration was defined as a key area for learning and was integrated into a new competency framework for medical students named PROFILES (Principal Relevant Objectives and Framework for Integrative Learning and Education in Switzerland), alongside areas such as palliative care and complementary therapies [Citation13]. In the same year, a Swiss interprofessional and interinstitutional working group developed interprofessional core competencies for interprofessional collaboration in health care, following an initiative from the Federal Office of Public Health. This working group recommended practice-based teaching-learning formats to develop interprofessional core competencies. Case-based online teaching-learning activities were considered less suitable; thus, a mix of both formats and methods were considered most desirable [Citation14].
Based on the new PROFILES competency framework and taking into account the working group recommendations, a new course on interprofessional practice covering the areas of palliative care and complementary therapies, was developed for the 6th semester of the Bachelor in Medicine program at the University of Zurich, Faculty of Medicine, in close collaboration with the Zurich University of Applied Sciences, School of Health Sciences. The areas of palliative care and complementary therapies were chosen since they present specialties with a high need for and commitment to interprofessional collaboration. In this paper, we report the evaluation of this newly developed, interprofessional course with a hybrid, flipped-classroom format for medical students.
Methods and materials
Research questions and design
The course evaluation was guided by the following research questions: (1) Does the quality of the teaching-learning formats used in the course support interprofessional education from medical students’ perspectives? (2) How do medical students and nurse educators perceive the usefulness of the workshadowing of medical students with a nurse or another health professional to learn about interprofessional collaboration? (3) What impact did the course have on medical students’ interprofessional identity?
To answer these questions, the course was evaluated with a cross-sectional survey using a combination of closed- and open-ended questions. Further, interprofessional identity of the medical students was assessed before and after the course.
Setting and participants
The course was implemented for the first time in the spring semester, from February to March 2021 as a mandatory course for 3rd year medical students. 380 enrolled medical students and 26 nurse educators participated in the course evaluation. Nurse educators are nurses responsible for nurses’ practical education in the teaching hospital. They collaborated with the faculty to provide on-site experience-based learning opportunities to medical students during the course. They were responsible for organizing and coordinating the medical students’ workshadowing with nurses on the units and served as a liaison between the faculty and the nurses on the unit whom medical students shadowed.
Course development and implementation
The course was developed in 2020 by an interprofessional group of lecturers from two universities with a background in medicine, nursing science, physiotherapy, and psychology. The aim was to create opportunity for medical students to learn about, and with other health professionals, interprofessional collaboration, palliative care, and complementary therapy.
The course is designed in a flipped-classroom format, which means that students acquire theoretical content individually through eLearning sessions (accounting for half of the course time), which is then elaborated in live sessions [Citation15,Citation16]. The entire course accounts for 1 ECTS (European Credit Transfer System, 1 ECTS corresponds to 20 units lasting 45 minutes each) and is spread over six weeks.
The course content is divided into three modules, that is, interprofessional collaboration, palliative care, and complementary therapy (). To ensure that all core competencies could be sufficiently addressed, the course content was mapped to the interprofessional core competencies, which include, for example, appreciation of other team members, joint decision-making, and communication skills in the interprofessional team [Citation14]. Learning objectives were defined at the course and module level, and harmonized with respective content and learning assessments, following constructive alignment rules [Citation17,Citation18]. As such, the course combines theoretical knowledge on interprofessional collaboration, experience-based learning with the acquisition of interprofessional core competencies during a workshadowing with other health professionals in clinical practice, and the case-based application of interprofessional collaboration within the areas of palliative care and complementary therapy.
Table 1. Course structure.
eLearning
The eLearning-sessions, which were especially created for this course, account for 40 to 60% of each module, and were implemented on the learning platform Open LMS, which is a dynamic Learning Management System that allows numerous useful options for user and course management [Citation19]. The eLearning sessions consist of a combination of short texts (mainly for definitions or theoretical knowledge), explanatory videos for more complex issues, expert discussions that allowed personal points of view, literature for further reading, and formative assessments that used multiple-choice questions with the possibility of repeated self-testing. According to the flipped-classroom concept, students need to complete the eLearning before attending live sessions and/or undertaking the workshadowing of another health professional in clinical practice. For the workshadowing, specific preparation- and follow-up learning assignments were included into the eLearning.
Live sessions
Live sessions of the course include experience-based learning during a half-day workshadowing session in clinical practice. The workshadowing session is spread out over the first five weeks of the course and accounts for one quarter of the total course time. Due to student schedules, it takes place on an afternoon in one out of ten teaching hospitals with a nurse or other health professional, such as a physiotherapist, a midwife, or an occupational therapist. It is combined with small-group reflections held during the last week of the course, which are moderated by Master students in nursing and physiotherapy from the partner University (Zurich University of Applied Sciences), who complete training in communication and group facilitation as part of their own curriculum.
In addition, case-based live sessions focus on interprofessional collaboration in palliative care and complementary therapy, which are facilitated by an interprofessional lecturer team, are delivered during the last week of the course. Real-life examples are used to enable medical students to gain experiences in collaborative practice and to develop skills. The aim is to promote the acquisition of interprofessional competencies in these two clinical fields through exchanges that incorporate various professional perspectives. To ensure discussions of case-examples in small student groups, the live-sessions are supplemented by virtual questions and perspectives of other health professions.
The course was implemented for the first time in Spring 2021 during the COVID-19 pandemic, which meant that live sessions (except for the workshadowing) were delivered in a virtual format. Each student completed the eLearning and the workshadowing individually before attending the virtual live lectures. Further course information is detailed in the supplementary material.
Recruitment and data collection processes
After completion of the course, all medical students enrolled in the course were invited to complete an online survey on EvaSys Zentrale Evaluation, Version 8.0, which is the web-based feedback automation platform for surveys [Citation20] used as the University’s official learning evaluation system. In addition, students completed a brief online survey after completion of each of the three eLearning sessions within the learning platform Open LMS [Citation19]. They were also asked to complete a validated measure assessing their interprofessional identity before and after completion of the entire course, which was programed on Unipark by Questback, version 2021, with an online link integrated into the eLearning or sent to students by email.
Nurse educators at teaching hospitals who coordinated the workshadowing placements were invited by personal email to complete a brief online survey, carried out on SurveyMonkey® by momentive.ai. They were reminded once.
Data collection instruments
Course content and methods with focus on workshadowing – student perspective
After completion of the course, an evaluation of the course was conducted using a combination of closed- and open-ended questions to assess students’ learning experience and outcomes on the overall course but also on the specific course modules (i.e., interprofessional collaboration, palliative care, complementary therapy). The online questionnaire consists of an adapted version of the existing course evaluation tool of the medical faculty. This evaluation form has a multidimensional structure and combines 42 closed-ended and 3 open-ended questions, of which 25 closed-end and all open-ended questions specific for the content of this evaluation were analyzed. It assesses, for example, overall satisfaction with the course, course design and competency development. In addition, course-specific items were added, which provided opportunities for feedback on the eLearning content and students’ experience with the live sessions, particularly the workshadowing, small group reflections, and case-based content [Citation21,Citation22]. The closed-ended items were rated using a 6-point numeric rating scale (1 = strongly disagree to 6 = strongly agree), except the question regarding the course duration (5-point numeric rating scale).
eLearning content and design – student perspectives
The eLearning was evaluated with an online questionnaire (11 closed- and 3 open-ended questions) focusing on domains such as content/comprehensibility, layout/design/time required for completion and the overall impression. Specified items were rated using a 10-point numeric rating scale (1 = strongly disagree to 10 = strongly agree). Surveys were included in the analysis if they had been completed before attending the live sessions. 9 closed- and all open-ended questions specific for the content of this evaluation were analyzed.
Workshadowing implementation – nurse educator perspectives
The self-developed, 10 questions for nurse educators at teaching hospitals assessed the quality of information received about the aim of the experience-based learning experience, the organization of the workshadowing, and the quality of the students’ preparation for the workshadowing. The items were rated using a 6-point numeric rating scale (1 = strongly disagree to 6 = strongly agree).
Interprofessional identity – student perspective
The validated Extended Professional Identity Scale (EPIS) was used to assess medical students’ perceptions regarding their interprofessional identity before and after completion of the course [Citation23] The EPIS is a 12-item self-rating scale that evaluates three dimensions of interprofessional identity, namely belonging (4 items, reflecting group loyalty), commitment (4 items, reflecting psychological group formation), and belief (4 items, reflecting attitudes towards other professions) [Citation24]. The dimensions are interrelated, but each one presents a distinct characteristic of the same construct. The items were rated using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree). The EPIS has been found to have a high internal validity, with a Cronbach’s alpha for the subscales of .79, .81 and .80, respectively and .89 for the overall scale. In our sample, the Cronbach’s alpha of the total EPIS score was .93. The EPIS was provided in the psychometrically validated English version, since a validated German version was not available at this time. Sufficient English language proficiency of the medical students was assumed, as they are expected to be able to read and appraise scientific papers in English during their studies.
Data analysis
Statistical analysis
The closed-ended questions from the overall course evaluation were analyzed quantitatively with Microsoft Office Excel, Version Windows 365. The closed-ended questions from the eLearning evaluation and the survey in teaching hospitals were analyzed quantitatively by using IBM® SPSS® Statistics, Release 26.0.0.0. Due to the skewed distribution of the scales and an assumed skewed distribution of values, medians, and interquartile ranges (IQR) were reported.
Qualitative analysis
Cleaned data from the open-ended questions were entered into NVivo® (QRS international), a qualitative software analysis, to aid the analysis process. The qualitative data were analyzed with ‘qualitative content analysis’ as described by Erlingsson & Brysiewicz [Citation25]. A content analysis of qualitative data contains a five-stage analysis process. At first, researchers familiarize themselves with the data, followed by the identification and condensation of meaning units. Then, codes were formed and assigned to meaning units, which was subsequently followed by the categorization of the codes. Finally, the final themes were formed based on the categorized codes. The analysis process was performed by a research assistant and a postdoctoral researcher who had not been involved in the course planning and organization. Interpretive meetings were held to agree on the findings structure (LV, AT, RN, CW).
Results
Out of the 318 enrolled medical students, 152 participated in and completed the general course evaluation (48% response rate). The results referring to research question 1 are shown in . Based on the median and IQR, the students were rather satisfied with the course (Median 4.0, IQR 2.0). A majority of students stated that the different teaching-learning formats complemented each other well (Median 5.0, IQR 1.0).
Table 2. Overall course evaluation – student perspective.
Interprofessional collaboration was very important topic to a majority of the students (Median 6.0, IQR 1.0). The interprofessional team of lecturers (Median 5.0, IQR 2.0) and the interprofessional facilitation of patient cases (Median 6.0, IQR 1.0) were rated as rather important.
In the following, we present the quantitative and qualitative findings according to the research questions, namely quality of eLearning design and teaching-learning content, usefulness of workshadowing and reflection, including organizational challenges, and impact on interprofessional identity.
Findings on eLearning design and teaching-learning content (research question 1)
The eLearning sessions of each module were evaluated by more than 280 medical students (). In general, the students stated that the content covered their expectations for the respective module (the median values ranged from 7.0 [IQR 3.0] to 8.0 [IQR 2.0] out of 10). They also indicated that the content built well on their prior knowledge (the median values ranged from 8.0 [IQR 3.0] to 9.0 [IQR 3.0]). After having completed the eLearning session, the students felt well-prepared for the live sessions of the respective module (the median values ranged from 7.0 [IQR 3.0] to 9.0 [IQR 3.0]).
Table 3. Evaluation of eLearning sessions for each module – student perspective.
The design/structure of the eLearning facilitated the understanding of the content (median values of 8.0 [IQR 3.0] out of 10). The students considered the digital media used in the eLearning sessions to be suitable for knowledge transfer (the median values ranged from 8.0 [IQR 2.0] to 8.5 [IQR 3.0]).
As shown in , 60–75% of the students considered the implementation of the content in an eLearning format to be optimal. A smaller group of 15–26% preferred the content to be delivered as a live event.
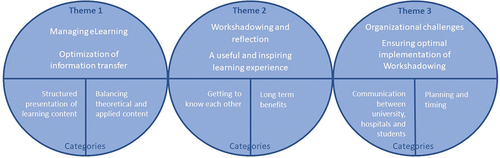
The results of the open-ended questions from the eLearning evaluation confirmed these quantitative results and showed that the medical students were overall satisfied with the presentation of the eLearning. Managing the eLearning was identified as one of the three themes from the qualitative analysis (see theme 1 in ). The program’s design, user-friendliness, and the diversity of applied digital media and learning content were considered attractive, as one student emphasized: ‘I find the overall design and use of online media for this course to be in general attractive’. Another said that ‘It was a very varied course with different types of questions and media used such as text, diagram, video’. The use of an illustrative pencast was found to be inspiring [Citation26]. The students expressed the wish for more video material to be integrated into the eLearning sessions: 'I found the video to start with very good! It motivated me and showed well how relevant collaborative practice is! More audio-visual media is desirable'.
Figure 2. Themes and categories on interprofessional collaboration content (eLearning and workshadowing) from open-ended questions.
The students identified room for improvement in connecting the theoretical content with practical examples. They wished more case-based examples that illustrate how the different but equally important principles of interprofessional collaboration come together and play out in real life. As one student stated, ‘I would have liked more information about concrete situations of interprofessional collaboration. For instance, when and how often an exchange is needed – is the handover sufficient, in which situations it is not?’ Specific examples of best practice were also suggested: ‘Case-based examples would be good, with elaboration on good interprofessional interaction practice’. The students appreciated when the text and assigned readings were brief and easy to read: ‘The publications used are quite complex, and sometimes the essence of the text gets lost because of that’.
Findings on the value of the workshadowing and reflection (research question 2)
The workshadowing was evaluated by the medical students (n = 152 statements) and the 26 nurse educators from the teaching hospitals. The quantitative results are presented in . The students considered the experience-based workshadowing to be a core teaching-learning activity in the course (Median 5.0, IQR 2.0 out of 6). However, the aim and purpose of the preparation and follow-up tasks remained somewhat unclear to the students (Median 3.0 [IQR 2.0] and Median 4.0 [IQR 3.0]). In contrast, the small group reflection was rated as useful consolidation of their experiences and observations made in practice (Median 5.0 [IQR 3.0]). The fact that the Master of Science in Nursing and Physiotherapy students facilitated these small group discussions was considered an enrichment (Median 5.0 [IQR 2.0]).
Table 4. Evaluation of the workshadowing by students and teaching hospitals.
The medical students felt that they had gained sufficient insights into other health professional, particularly nursing practice fields (Median 4.0 [IQR 3.0]). The opportunities to observe interprofessional collaboration itself were rated to be rather low (Median 2.0 [IQR 3.0]). A main reason was that workshadowings had to be scheduled in the afternoons due to student timetable restrictions. However, the supervision provided by the nurses who they shadowed, was rated as good (Median 5.0 [IQR 2.0]).
The qualitative findings from the open-ended questions showed that the workshadowing and small group reflections were perceived to be useful and inspiring learning experiences (see theme 2 in ). The students found it beneficial to meet different health professionals and considered their workshadowing experience to be very helpful in gaining an impression of the roles and activities of different health professionals: ‘What I liked most was the day in the hospital with the nursing staff. It showed me what the nurse is responsible for and how the organization works’. However, some students mentioned that they already had some prior knowledge of nurses’ tasks and thereby would have preferred to shadow another health professional: ‘Many of us have completed at least one nursing internship. Therefore, it would have been newer and accordingly more interesting to have met with, for instance, the physiotherapy [professionals]’.
From the nurse educators’ perspectives who coordinated the workshadowing in the teaching hospitals, the workshadowing was meaningful to promote interprofessional collaboration in practice. They were also positive towards students’ workshadowing with other health professionals: ‘Workshadowing is very interesting for medical students to get an insight into the work of, for instance, occupational therapists’. The teaching hospitals considered the early investment in interprofessional education to be beneficial for the cultivation of interprofessional collaboration: ‘Benefits are more likely in the long term, when obtained insights sustainably promote interprofessional collaboration’.
Findings on organizational challenges with workshadowing (research question 2)
The quantitative evaluation showed that the aim and purpose of the workshadowing were clear and understandable (Median 5.0, IQR 2.0). The preparation of students for their workshadowing was considered sufficient (Median 4.0, IQR 2.0). However, the flow of information was not always perfect, and the nurse educators would have preferred more timely communication and clarity about their responsibilities for students during their actual workshadowing (see theme 3 in ). Students found that health professionals were not always well-informed about the purpose and content of the workshadowing program. Another student said, ‘Better inform the professionals for what exactly we are coming for, so we can truly observe interprofessional collaboration’.
Due to the students’ restrictive timetable, with mandatory attendance in other classes in the morning, the workshadowing was planned mostly during the afternoon. Both the teaching hospitals and students considered workshadowing during the afternoon to be undesirable because interprofessional interactions, such as patient visits and interprofessional team meetings, occur less frequently during the afternoon. A student mentioned that ‘workshadowing in the afternoon is unfavorable because no handovers or visits by physicians take place, and the interprofessional collaboration could not be observed at all’.
Findings on interprofessional identity (research question 3)
The results on interprofessional identity obtained using the EPIS before (n = 274 students, response rate 86%) and after (n = 108 students, response rate 34%) the course, are shown in . Overall, the interprofessional identity was already high (Median 4.1, IQR 0.7 out of 5) before the course. The scores of the three subscales ‘interprofessional belonging’, ‘interprofessional commitment’ and ‘interprofessional belief’, were quite similar. After the course, the scores of each subscale and the total EPIS score remained unchanged or increased only slightly.
Table 5. Student interprofessional identity (EPIS): Before and after the course.
Discussion
In this paper, we report the evaluation of a newly developed, hybrid flipped-classroom, course on interprofessional practice in health care for 3rd-year medical students. We found that the course format, which consisted of a general introduction to interprofessional collaboration coupled with hands-on experience collected during a half-day of workshadowing in clinical practice and case-based interprofessional teaching-learning on the topics of palliative care and complementary therapies, was feasible and acceptable to the medical students. Our comprehensive course evaluation was guided by three research questions focusing on the quality of teaching-learning methods, including eLearning formats, the usefulness of the workshadowing as a teaching-learning method to develop interprofessional competencies, and the impact of the course on their perception of interprofessional identity. This evaluation included different data sources and perspectives, showed that the students appreciated the flipped-classroom concept, the real-world case-based learning scenarios with interprofessional teaching teams, the possibility of an experience-based learning opportunity in the clinical setting, which was followed by small group reflections facilitated by Master students’ from nursing and physiotherapy. No effect on their interprofessional identity could be identified, which may likely be due to methodological limitations. Nonetheless, our findings suggest that a combination of theoretical content connected to narratives and clinical learning experiences, delivered by interprofessional lecture teams and co-facilitated by students from other health professions, provides a satisfactory and meaningful learning experience to medical students, and has the potential for effective interprofessional education. The implementation of such teaching-learning methods and interprofessional course structures within health professional education may therefore be increased and strengthened.
Course content, methods, and design
First, we evaluated the quality of teaching-learning methods and their potential to develop interprofessional competencies. We found that the use of a flipped-classroom format was perceived to be useful and beneficial for learning about interprofessional collaboration. Flipped-classroom concepts have recently received much attention within medical education and have been found to be particularly suitable to increase learners’ motivation, engagement, and task value [Citation27]. These findings support the use of a flipped-classroom format in interprofessional education. Providing parts of a complete course as a flexible option in terms of the time and place might overcome some of the challenges of interprofessional education, particularly with regard to a possible extension of the course to students from other health professions. Flexible solutions may be easier fitted into the different curricula and timetables of different faculties, schools and programs, and provide additional advantages to students’ individual learning preferences [Citation1,Citation28].
A variety of (multimedia) elements were included in the eLearning sessions, since different elements uphold learners’ engagement, attention, and satisfaction [Citation29–31]. The students appreciated this diversity, as indicated in our eLearning evaluation results. Our findings suggest that a mix of text-based elements, expert discussions, formative assessments, and additional resources, such as further reading, facilitates the understanding of the course content.
Throughout the entire course, we used several strategies that are known to facilitate learning, e.g., spacing (by using the flipped-classroom model and distributing content across several weeks), piquing curiosity (e.g., with practical examples close to students’ daily reality), and providing an opportunity for the self-control of progress (the self-assessment in eLearning modules and active recalling of knowledge in lectures) [Citation32–36]. Furthermore, the learning objectives, course content, and assessments were harmonized according to constructive alignment rules [Citation17,Citation18]. These measures have likely contributed to the students’ favorable course perception regarding the content, as seen in our evaluation results.
Teaching-learning interprofessional competencies rather than just transferring knowledge remains a challenge. The well-known Miller’s pyramid on assessing clinical skills and competencies proposes a 4-level framework to be used in medical education [Citation37]. This framework includes knowledge, competence, performance and action, which leads students from ‘knowing’ to ‘doing’, and is widely used to design teaching programs. Recently, it has been suggested to extend this pyramid with an additional level called ‘professional identity’ [Citation38]. Our approach to teaching-learning (inter)professional identity included interprofessional and interinstitutional lecturer teams during live sessions. The students indicated that they highly valued the in-action experience of the lecturers of different professional backgrounds, who demonstrated their own professional identity in interprofessional patient management by using case-based scenarios. In addition, they reported to appreciate the interactions with other health professionals, mostly nurses, during the workshadowing and the subsequent small group reflections. These findings support the existing evidence on using interprofessional simulation activities and the use of a case-based approach [Citation39,Citation40].
Workshadowing
Second, we investigated the usefulness of the workshadowing with a nurse or another health professional to learn about interprofessional collaboration. The students’ workshadowing of a nurse or other health professional was a highly valued and essential element of the course. This is in line with the finding of a systematic review [Citation41], which showed that even a short duration (of 2 to 10 hours) of clinically based interprofessional activity can be beneficial to improve interprofessional understanding and to develop interprofessional core competencies. Using an experience-based, reflective learning cycle [Citation21,Citation22] and involving interprofessional teams throughout the cycle was considered valuable by the medical students for their learning. Our results indicate that the clear communication of goals, expectations and tasks is important for students and clinical supervisors alike to ensure that the workshadowing is a beneficial learning experience for all involved parties.
Our findings show that there is room for improvement in scheduling the workshadowing part. Due to organizational constraints, the workshadowing took place in the afternoon, whereas interprofessional collaboration in hospitals, such as rounds, occurs mainly during the morning shift. Moreover, nurses provide more direct patient care in the morning than in the afternoon, which limits medical students’ opportunity to observe nurse-patient interactions. To improve opportunities for observing interprofessional collaboration and to improve students’ learning experience, workshadowing should be rescheduled to occur during morning shifts.
Interprofessional identity
Third, we investigated perceptions of medical students of their interprofessional identity before and after the course. Interprofessional identity as measured with the EPIS [Citation23] did not change to a statistically significant extent, which makes it difficult to assess the learning effect on the level of ‘professional identity’ of the Miller’s pyramid. However, these results need to be interpreted with caution. Interprofessional identity was rated high before attending the course. Since completing the questionnaire was voluntary and the response rate dropped from high (pre) to low (post), there might be a selection bias at play, with very motivated students interested in interprofessional practice being more likely to have completed the post-measurement. Further, a leniency effect cannot be excluded due to a social desirability bias or due to an idealization of interprofessional collaboration by the students. Lenient ratings have been described to occur more often when socially desirable responses are provided [Citation42].
It would be interesting to explore whether EPIS scores change over the course of the entire course of educational training of medical studies. Experiences during professional practice might shape and change the interprofessional identity in both – positive and negative – ways, as suggested by van Duin et al. [Citation43]. It has been previously reported that interprofessional identity in nursing, medical and further health professional students decreases during their studies [Citation44]. However, in Tong et al.’ study, the interprofessional identity did not decrease if students were in (high quality) contact with students from other health professions, confirming the need to provide sufficient opportunities for interprofessional education early on. Research does indeed indicate that interprofessional education might be most effective when interactions between students of different health professions occur [Citation45–47]. Since social factors enhance the interprofessional education experience for learners, ample opportunities for both formal and informal interactions between health professions should be provided [Citation48]. Our course included some components during which different health professionals interacted, such as the workshadowing and reflection part. Further, it would be of interest if sequential courses on interprofessional collaboration or more opportunities for interprofessional teaching-learning might change EPIS.
Limitations
Our evaluation uses observational data, and has several limitations. First, we used established, but – with the exception of EPIS – not psychometrically tested instruments. Second, only approximately half of the participating medical students completed the overall course evaluation, which may limit the generalizability of the results. Nonetheless, the response rate was higher than the usual 30% observed in course evaluations of the same faculty and can therefore be considered somewhat satisfactory.
Only approximately 40% of students who completed the EPIS before the course also completed the post-course assessment. Thus, a potential selection bias limits the interpretability of our pre-post evaluation of interprofessional competencies. Further, the EPIS was provided in English, which is the validated form. Since the majority of students are not native English speakers misunderstanding of items cannot be excluded.
The primary focus of the program was on medical students, extension of this course to students of other health professions would be a great opportunity to allow interprofessional peer-to-peer interaction for the students.
Despite these limitations, our evaluation provides initial, data-based insights into the impact of an interprofessional course on medical students’ learning experiences and interprofessional competencies. Using both quantitative and qualitative data, our findings indicate that the course was useful and beneficial, enabling students to experience interprofessional learning and to develop interprofessional competencies.
Conclusion
We reported the evaluation of a newly developed course on interprofessional collaboration for medical students, which not only focused on interprofessional practice as a content area but also applied interprofessional teaching-learning to other required content domains, namely, palliative care and complementary therapies. We found that the use of a hybrid flipped-classroom format that combined eLearning sessions with – due to the pandemic – virtual live sessions and clinical learning opportunities is promising for teaching-learning interprofessional competencies. The use of case- and experience-based teaching-learning methods during live and clinical sessions was valued by the students, who perceived them as useful to their own learning, both in relation to interprofessional practice, professional roles, and application to interprofessional patient management.
Our findings have several implications for practice and research. We suggest the following key elements for the implementation of interprofessional education in practice. First, a flipped-classroom concept should be used to allow flexible scheduling for students of different faculties or schools. Second, experience-based learning should be provided with a workshadowing. Third, interprofessional teaching teams are necessary to facilitate the knowledge transfer to case-based learning in live sessions. The inclusion of students from other health professions, such as nursing, physiotherapy, or midwifery in all parts of the course, is desirable. Considering research implications, more data-based insights into the benefits of such courses on interprofessional competencies, including perspectives from different health professional students included in the course, are needed.
Authors’ contributions
All authors participated in the development and implementation of the course. MR, JL, AT, RN, DB and CW developed the course-specific items for the overall course evaluation, and AT, CW and RN developed the questionnaire to evaluate the eLearning sessions and teaching hospitals’ experience. AT and MR analyzed the quantitative evaluation data. MH analyzed the EPIS data. The qualitative data from all questionnaires were analyzed by LV and RN. AT, LV, and RN co-wrote the manuscript. CW, DB, AF, EF, JL, MH, and MR critically reviewed the manuscript for important intellectual content. All authors have reviewed the drafts of the manuscript and have approved the final version.
Ethics approval and consent to participate
The research has been conducted according to the national guidelines and regulations for research with humans [Citation49]. The Cantonal Ethics Committee Zurich waived the need for ethics approval (BASEC-No Req-2021–00131). The surveys reported here were irrevocably anonymous and conducted on a voluntary basis. In accordance with Swiss regulation and ethical guidance, participants were informed that completion and return of the online survey is taken as informed consent. Therefore, there was no need for formal collection of informed consent.
Availability of data and materials
Parts of the data come from the university standardized evaluation of teaching curricula where a data sharing in an open access repository is not foreseen. Data can be provided from the corresponding author upon specific, reasonable request.
Supplemental Material
Download MS Word (26.4 KB)Acknowledgments
The authors would like to thank Matthew Kerry-Kerry Krause, Heidi Bruderer Enzler and Eva Thürlimann for their assistance in data analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10872981.2023.2198177
References
- Health Professions Network Nursing & Midwidery Human Resources for Health. Framework for action on interprofessional education and collaborative practice. 2010. Available from: https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice
- Hammick M, Freeth D, Koppel I, et al. A best evidence systematic review of interprofessional education: BEME Guide 9. Med Teach. 2007 Oct;29(98):735–12. DOI:10.1080/01421590701682576.
- Buring SM, Bhushan A, Brazeau G, et al. Keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educ. Jul 10 2009;73(4):60. DOI:10.5688/aj730460.
- Buring SM, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. Jul 10 2009;73(4):59. DOI:10.5688/aj730459.
- Spaulding EM, Marvel FA, Jacob E, et al. Interprofessional education and collaboration among healthcare students and professionals: a systematic review and call for action. J Interprof Care. 2021 Jul-Aug;35(4):612–621. DOI:10.1080/13561820.2019.1697214.
- Berger-Estilita J, Fuchs A, Hahn M, et al. Attitudes towards interprofessional education in the medical curriculum: a systematic review of the literature. BMC Med Educ. Aug 6 2020;20(1):254. DOI:10.1186/s12909-020-02176-4.
- Dyess AL, Brown JS, Brown ND, et al. Impact of interprofessional education on students of the health professions: a systematic review. J Educ Eval Health Prof. 2019;16:33.
- Guraya SY, Barr H. The effectiveness of interprofessional education in healthcare: a systematic review and meta-analysis. Kaohsiung J Med Sci. 2018 Mar;34(3):160–165. DOI:10.1016/j.kjms.2017.12.009.
- Lairamore C, Morris D, Schichtl R, et al. Impact of team composition on student perceptions of interprofessional teamwork: a 6-year cohort study. J Interprof Care. 2018 Mar;32(2):143–150. DOI:10.1080/13561820.2017.1366895.
- Reeves S, Fletcher S, Barr H, et al. A BEME systematic review of the effects of interprofessional education: bEME Guide No. 39. Med Teach. 2016 Jul;38(7):656–668. DOI:10.3109/0142159X.2016.1173663.
- Murdoch NL, Epp S, Vinek J. Teaching and learning activities to educate nursing students for interprofessional collaboration: a scoping review. J Interprof Care. 2017 Nov;31(6):744–753. DOI:10.1080/13561820.2017.1356807.
- Fox L, Onders R, Hermansen-Kobulnicky CJ, et al. Teaching interprofessional teamwork skills to health professional students: a scoping review. J Interprof Care. 2018 Mar;32(2):127–135. DOI:10.1080/13561820.2017.1399868.
- Michaud PA, Jucker-Kupper P. The profiles working G. The “Profiles” document: a modern revision of the objectives of undergraduate medical studies in Switzerland. Swiss Med Wkly. 2016;146:w14270.
- Huber M, Spiegel-Steinmann B, Schwärzler P, et al. Kompetenzen zur interprofessionellen Zusammenarbeit und geeignete Unterrichtsformate Forschungsberichte des Bundesamtes für Gesundheit BAG. 2019.
- Young TP, Bailey CJ, Guptill M, et al. The flipped classroom: a modality for mixed asynchronous and synchronous learning in a residency program. West J Emerg Med. 2014 Nov;15(7):938–944. DOI:10.5811/westjem.2014.10.23515.
- Belfi LM, Bartolotta RJ, Giambrone AE, et al. “Flipping” the introductory clerkship in radiology: impact on medical student performance and perceptions. Acad Radiol. 2015 Jun;22(6):794–801. DOI:10.1016/j.acra.2014.11.003.
- Biggs J. Enhancing teaching through constructive alignment. Higher Educ. 1996;32(3):347–364.
- Biggs J, Tang C. Teaching for quality learning at university. 4th ed. Maidenhead: Society for research into higher Education & Open University Press; 2011.
- Open LMS. Open LMS. 2022. [cited 10January2022]. Available from: https://www.openlms.net/
- EvaSysZentrale Evaluation. Version 8.0. 2021. Available from: https://evasys.de/evasys/
- Stanton F, Grant J. Approaches to experiential learning, course delivery and validation in medicine. A background document. Med Educ. 1999 Apr;33(4):282–297. DOI:10.1046/j.1365-2923.1999.00272.x.
- Husebø SE, Dieckmann P, Rystedt H, et al. The relationship between facilitators’ questions and the level of reflection in postsimulation debriefing. Simul Healthc. 2013;8(3):135–142.
- Reinders JJ, Lycklama ANM, Der Schans Cp V, et al. The development and psychometric evaluation of an interprofessional identity measure: extended Professional Identity Scale (EPIS). J Interprof Care. 2020;3(2020):1–13.
- Reinders JJ, Krijnen WP, Goldschmidt AM, et al. Changing dominance in mixed profession groups: putting theory into practice. Eur J Work Organ Psychol. 2018;27(3):375–386.
- Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med. 2017;7(3):93–99.
- Lehrvideo Interprofessionelle Zusammenarbeit im Gesundheitswesen. [cited 20October2021]. Available from: https://youtu.be/DeoUv8IME8M. youtube.com.
- Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017 Jun;51(6):585–597. DOI:10.1111/medu.13272.
- Tucker K, Wakefield A, Boggis C, et al. Learning together: clinical skills teaching for medical and nursing students. Med Educ. 2003 Jul;37(7):630–637. DOI:10.1046/j.1365-2923.2003.01558.x.
- Cook DA, Dupras DM. A practical guide to developing effective web-based learning. J Gen Intern Med. 2004 Jun;19(6):698–707. DOI:10.1111/j.1525-1497.2004.30029.x.
- Santer DM, Michaelsen VE, Erkonen WE, et al. A comparison of educational interventions. Multimedia textbook, standard lecture, and printed textbook. Arch Pediatr Adolesc Med. 1995 Mar;149(3):297–302. DOI:10.1001/archpedi.1995.02170150077014.
- Bell DS, Fonarow GC, Hays RD, et al. Self-study from web-based and printed guideline materials. A randomized, controlled trial among resident physicians. Ann internal med. Jun 20 2000;132(12):938–946.
- Kramár EA, Babayan AH, Gavin CF, et al. Synaptic evidence for the efficacy of spaced learning. Proc Natl Acad Sci U S A. 2012;109(13):5121.
- Halamish V, Madmon I, Moed A. Motivation to Learn. Exp Psychol. 2019 Sep;66(5):319–330. DOI:10.1027/1618-3169/a000455.
- Larsen DP, Butler AC, Roediger Iii HL Repeated testing improves long-term retention relative to repeated study: a randomised controlled trial. 10.1111/j.1365-2923.2009.03518.x. Med Educ. 2009;43(12):1174–1181. doi:https://doi.org/10.1111/j.1365-2923.2009.03518.x
- Gruber MJ, Gelman BD, Ranganath C. States of curiosity modulate hippocampus-dependent learning via the dopaminergic circuit. Neuron. Oct 22 2014;84(2):486–496.
- Larsen DP, Dornan T. Quizzes and conversations: exploring the role of retrieval in medical education. Med Educ. 2013;47(12):1236–1241.
- Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9):S63–7.
- Cruess RL, Cruess SR, Steinert Y. Amending miller’s pyramid to include professional identity formation. Acad Med. 2016;91(2):180–185.
- Marion-Martins AD, Pinho DLM. Interprofessional simulation effects for healthcare students: a systematic review and meta-analysis. Nurse Educ Today. 2020 Nov;94:104568. DOI:10.1016/j.nedt.2020.104568.
- Visser CLF, Ket JCF, Croiset G, et al. Perceptions of residents, medical and nursing students about Interprofessional education: a systematic review of the quantitative and qualitative literature. BMC Med Educ. May 3 2017;17(1):77. DOI:10.1186/s12909-017-0909-0.
- Brack P, Shields N. Short duration clinically-based interprofessional shadowing and patient review activities may have a role in preparing health professional students to practice collaboratively: a systematic literature review. J Interprof Care. 2019;33(5):446–455.
- Cheng KHC, Hui CH, Cascio WF. Leniency Bias in Performance Ratings: the Big-Five Correlates. Front Psychol. 2017;8:521.
- van Duin TS, de Carvalho Filho MA, Pype PF, et al. Junior doctors’ experiences with interprofessional collaboration: wandering the landscape. Med Educ. 2022;56(4):418–431.
- Tong R, Roberts LD, Brewer M, et al. Quality of contact counts: the development of interprofessional identity in first year students. Nurse Educ Today. 2020;86:104328.
- van Diggele C, Roberts C, Burgess A, et al. Interprofessional education: tips for design and implementation. BMC Med Educ. 2020;20(2):455.
- Hall LW, Zierler BK. Interprofessional education and practice Guide No. 1: developing faculty to effectively facilitate interprofessional education. J Interprof Care. 2015;29(1):3–7.
- Omar H, Khan S, Haneline M, et al. Attitudes of dental and chiropractic students towards a shared learning programme-An interprofessional learning model. Eur J Dent Educ. 2021 Aug;25(3):592–599. DOI:10.1111/eje.12636.
- Nash A, Hoy A. Terminal care in the community–an evaluation of residential workshops for general practitioner/district nurse teams. Palliat Med. 1993;7(1):5–17.
- Swiss Academy of Medical Sciences. Research with human subjects: a manual for practitioners. 2 ed. Bern: Swiss Academy of Medical Sciences; 2015.