ABSTRACT
Clinical reasoning is the cornerstone to healthcare practice and teaching it appropriately is of utmost importance. Yet there is little formal training for clinical supervisors in supervising this reasoning process. Distance education provides interesting opportunities for continuous professional development of healthcare professionals. This mixed methods study aimed at gaining in-depth understanding about whether and how clinical teachers can develop complex pedagogical competencies through participation in a Massive Open Online Course on the supervision of clinical reasoning (MOOC SCR). Participants self-assed their clinical supervision skills before and after partaking in the MOOC SCR through the Maastricht Clinical Teachers Questionnaire. Item scores and the distribution of response proportions before and after participation were compared using paired t-tests and McNemar’s tests respectively. In parallel, the evolution of a subset of MOOC participants’ pedagogical practice and posture was explored via semi-structured interviews throughout and beyond their MOOC participation using simulated and personal situational recalls. The verbatim were analysed with standard thematic analysis. Quantitative and qualitative findings converged and their integration demonstrated that partaking in the MOOC SCR promoted the development of complex pedagogical competencies and reflexivity with the participants. This was quantitatively evidenced by significantly higher self-assessed supervision skills and corresponding attitudes after completing the MOOC. The qualitative data provided rich descriptions of how this progression in pedagogical practice and posture occurred in the field and how it was shaped by participants’ interaction with the MOOC’s content and their motivations to progress. Our findings provide evidence for the development of pedagogical skills and corresponding attitudes for the supervision of clinical reasoning through participation in the MOOC SCR and contribute to the literature body on the opportunities that distance learning provides for the development of pedagogical competencies. The extent to which the pedagogical underpinnings of the MOOC contributed to these developments remains to be determined.
Introduction
Clinical reasoning is central to healthcare practice. Yet, teaching and supervising it is complex as this process depends on the practitioners’ context and experience, partly results from automatic, implicit pattern recognition processes and implies a high cognitive load [Citation1,Citation2]. Between 7 and 28% of medical students encounter academic difficulties at some point in their curriculum [Citation3–6] and most of them encounter cognitive difficulties including difficulties in clinical reasoning [Citation7–11]. As most of these difficulties become apparent during clinical rotations, it is crucial to train clinical teachers in identifying and remediating them to facilitate the development of the learners’ competencies and ultimately ensure efficient clinical interventions and adequate patient care.
Distance learning has been increasingly integrated into medical education over the past two decades [Citation12–17]. In contrast with simply broadcasting electronic course material via the internet, online teaching encompasses a pedagogical approach and aspires to be flexible, engaging, interactive and learner-centered [Citation12,Citation18–20]. Massive Open Online Courses (MOOCs) on designated pedagogical platforms illustrate one way of online teaching in health professions education and are a class of online and mostly open-access courses that transmit content to large numbers of participants. They are usually several weeks long and ideally involve learners through videos, quizzes or peer interactions via forums, mutual assessments and individual or group assignments. Strong pedagogical foundations, active and authentic learning requiring reflection and a careful course design have additionally been reported as key ingredients for a MOOC’s effectiveness in the context of health professional’s continuous education [Citation21]. While the open access of MOOCs permits the registration of thousands of participants, usually only a fraction actually completes the course [Citation22,Citation23].
Striving for a continuous professional development as clinical teacher requires nurturing one’s knowledge base with clinical, medical, contextual and pedagogical knowledge [Citation24] and permits continuous improvement of clinical and pedagogical skills. In this context, MOOCs on topics such as the clinical reasoning process [Citation25,Citation26] or teaching and assessing clinical skills [Citation27–29] have been developed over the past years. These courses are particularly interesting as they deal with relevant issues encountered in the clinical context, thereby promoting the applicability of the learned concepts [Citation30,Citation31]. To contribute to the development of pedagogical competencies of the clinical teacher, the G3 de la francophonie (a consortium of three French-speaking universities – University of Geneva, Université de Montréal, and Free University of Brussels) supported the development of a MOOC on the supervision of clinical reasoning (MOOC SCR) in clinical settings. This MOOC proposes a conceptual framework for clinical reasoning supervision and trains participants in the practical use of methods for supervising this reasoning process and for implementing remediation strategies to difficulties encountered by their students. We hypothesized that participation in this MOOC allowed the development of complex pedagogical competencies such as the elaboration of teaching scripts [Citation24], the practice of supervision and the reflexivity of clinical teacher participants and their integration into participants’ practice and posture [Citation32,Citation33]. Such a professional development, further embodied through the development of a clinician-teacher professional identity, would allow learners to move beyond knowledge and skills (traits) towards attitudes and their incorporation into daily routines (states), a notion also described as ‘entrustment’ in the last level of Miller’s pyramid on learner assessment in health professions [Citation34,Citation35].
In the framework of coronavirus disease 2019 (COVID-19) related perturbations of medical education, numerous educational developments emerged, describing the adaptation of classroom and clinical teaching towards mainly online modalities [Citation20,Citation36–38]. This persisting context brought afore the need for shifting from a patching attitude of emergency remote teaching to a sustainable adaptation of study plans and continuing education programs [Citation20,Citation39–41]. Particularly in distance learning formats, there is an increasing need for a careful consideration of constructive pedagogical alignment [Citation42] and of relationships between and within teachers and learners [Citation20,Citation43,Citation44]. In this context, we here use the MOOC SCR and the analysis of nearly three years of participation to illustrate that carefully developed distance education can be used to develop complex pedagogical competencies and corresponding postures of participants. We build on our findings to illustrate important issues related to the supervision of clinical reasoning and discuss how distance teaching may promote the development of complex competencies.
Materials and methods
MOOC SCR objectives, modalities and pedagogical principles
Objectives - The main objectives of the MOOC SCR are to offer a conceptual framework and practical, relevant methods for supervising clinical reasoning, for implementing means of remediation of identified difficulties and for developing a reflexive stance on one’s practice as a teacher. The MOOC is aimed at health professionals who supervise pre- and/or post-graduate health professions’ students in different clinical settings (private practice, hospital, clinic) with a particular aim at medical doctors, as the situational videos and examples stem from their clinical context.
Modalities - The course is structured around eight modules, whose learning objectives are summarized in Supplementary File 1. Participants can start the course at any time and can take as much time as needed to complete it. This feature accommodates for possible differences in learner profiles, allowing participants to engage with the course content according to individual constraints and motivational drivers [Citation45]. The MOOC is held in French, and is available since January 2019 on two online platforms, namely Coursera [Citation46] and Edulib [Citation47].
Pedagogical foundations - The course is conceived in a learner-centered perspective reflecting an active, situated and self-directed vision of learning [Citation30,Citation31,Citation42,Citation48]. The different modules provide rich feedback and guidance for different learner needs through numerous interactive videos with simulated clinical supervision situations. The videos apply storytelling principles for the narration and were elaborated to resonate with participants’ practice. These practical cases are supplemented with short theoretical videos and extensive literature, provided at the end of each module, to integrate the theory.
Throughout the course, participants are prompted to analyze the presented situations and develop reflexive abilities [Citation49], thereby developing awareness of the competencies to be achieved. To anticipate for participants’ potential feeling of isolation in this online course, the MOOC aims at creating feelings of presence by keeping the same presenters intervening in the introductory and theoretical videos throughout the course. In addition, introductory videos are situated in the same clinical settings, in which a situational video would afterwards prompt participants to reflect on different steps of the supervision process. To minimize distractibility associated with distance learning, the course content is subdivided into short sub-units of generally less than five minutes. Furthermore, the expected duration for each activity is indicated. Finally, to contribute to the development of a community of practice, participants could interact with each other and with the teaching staff in online forums, during several online discussion periods as well as in dedicated workshops at medical education conferences of the société internationale francophone d’éducation médicale (SIFEM) and of the Association for Medical Education in Europe (AMEE).
Study design
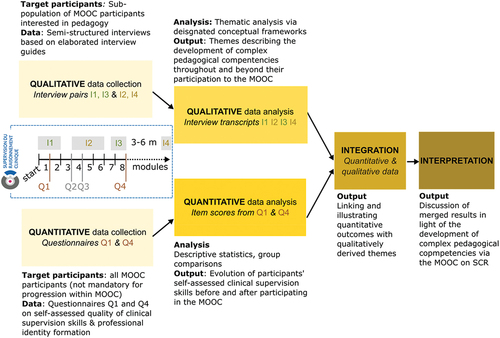
The present study aimed at understanding if and how MOOC SCR participation enabled the development of complex pedagogical competencies and a corresponding posture in clinical teachers. To address this two-fold objective, a convergent parallel mixed methods research approach was chosen [Citation50] and is reported according to the Good Reporting of Mixed Methods Study (GRAMMS) criteria [Citation51]. The quantitative arm aimed at assessing whether MOOC SCR participants improved their self-assessed clinical supervision skills after partaking in the course. The qualitative arm aimed at understanding the complex mechanisms underlying the development of those pedagogical competencies and corresponding attitudes. The study purpose was thus addressed by concurrently collecting and analyzing qualitative and quantitative data before merging results for triangulation, integration and interpretation (). The different datasets were equally important in addressing the research problem in an integrated way as they allowed to respond to the complementary aspects of ‘if’ and ‘how’ progression in pedagogical competencies and posture occurred through participation in the MOOC SCR.
Figure 1. Mixed methods research design: a parallel, convergent study design to gain in-depth understanding of how distance learning can promote the development of complex pedagogical competencies. Interview pair I1-I3 (green) focused on a simulated recording of a supervision, interview pair I2-I4 focused on a participant’s personal situational recall of a supervision situation. Questionnaire pair Q1-Q4 (brown) generated data about participants’ self-assessed clinical supervision skills before and after partaking in the MOOC. Questionnaire pair Q2-Q3 (grey) investigated the interaction between participants and the learning tools developed in the MOOC (analysis out of scope of the present work). MOOC SCR: Massive open online course on the supervision of clinical reasoning, I: interview, Q: questionnaire, m: months.
Quantitative study arm
Sampling and data collection
The quantitative arm of the study aimed at answering the research question ‘Do MOOC SCR participants self-assess their clinical supervision skills as higher after partaking in the MOOC SCR compared to before starting the MOOC?’. This was addressed by comparing the MOOC participants’ self-assessed clinical supervision skills before and after taking the MOOC SCR via two online questionnaires addressed to them at the beginning (Q1, end of module 1) and at completion (Q4, end of module 8) of the MOOC. Questionnaires Q2 and Q3 focused on the interaction between participants and the MOOC’s learning tools and are discussed in another contribution [Citation52]. All MOOC participants were voluntary and answering the questionnaires was not mandatory for progression within the MOOC. Likewise, responding to Q1 did not constrain participants to respond to the following questionnaires. Participants consented online to participate in the study before responding to the first question of Q1.
Data analysis
Self-assessed quality of participants’ clinical supervision skills
We compared the participants’ self-assessed clinical supervision skills before and after partaking in the MOOC SCR through the Maastricht Clinical Teaching Questionnaire (MCTQ), a valid and reliable instrument to assess clinical supervision skills [Citation53,Citation54]. This instrument has been used as a self-evaluation instrument (modified MCTQ, mMCTQ) to identify self-perceived training needs in clinical teachers [Citation55–57]. It aims at evaluating the quality of individual clinical teacher’s supervision through the dimensions of Role modeling, Coaching, Articulation, Exploration, and Learning environment (, dimensions 1–5).Qualitative [Citation58,Citation59] and quantitative [Citation60] evidence has suggested that excellent clinical teachers have a well-developed teacher identity in addition to their clinician identity. To explore the relationship between clinical reasoning supervision competencies and the development of a clinical teacher professional identity, we added questionnaire items on an additional dimension, Professional identity development (, dimension 6). All six dimensions require different pedagogical competencies and the questionnaire asked participants to self-assess their performance by indicating their agreement to 24 items distributed over these 6 dimensions on a four-point Likert scale [Citation61]. We chose a forced Likert scale to obtain a clear positioning from the participants, permitting the dynamic comparison of responses at the beginning and at the end respectively of their participation in the MOOC.
Table 1. Dimensions of clinical supervisions and corresponding teacher actions explored with questionnaires Q1 and Q4.
In the present study, the questionnaires were written and administrated in French (Supplementary File 2). For the purpose of this research article, they were translated to English by a native English speaker (Supplementary File 3).
Statistical analyses
We performed descriptive analyses of all mMCTQ items and computed the mean score and standard deviation obtained for each item as well as the distribution of each item’s responses on the Likert scale in Q1 and Q4. We assessed the differences between item scores in Q1 and Q4 using a paired t-test to consider the matched observations (same participants). For each item, we computed and reported the proportion of respondents that increased, maintained and decreased their agreement rating with each item’s statement between Q1 and Q4. We also computed the proportions of respondents that globally agreed (aggregating ratings for ‘Totally agree’ and ‘Partially agree’) and disagreed (aggregating ratings for ‘Totally disagree’ and ‘Partially disagree’) with each item’s statement in Q1 and Q4 and compared those proportions using McNemar’s test for paired nominal (‘agree’ vs. ‘disagree’) data.
Qualitative study arm
Sampling and data collection
The qualitative arm of the study consisted in answering the research question ‘How does partaking in the MOOC SCR enable the development of complex pedagogical competencies and corresponding postures in its participants?’. This was addressed through a longitudinal exploration of a selected subpopulation of MOOC participants’ progression in clinical teaching competencies during and beyond their participation in the MOOC (purposeful sampling). Those participants were recruited to participate in the MOOC SCR and the qualitative study arm by e-mail to a [nationality] community of practice of family medicine practitioners interested in pedagogy, of which one of this study’s authors, HM, is a member of.
The longitudinal exploration of their developing pedagogical competencies was achieved through a series of four semi-directed interviews held during (I1, I2, and I3) and after (I4) completion of the MOOC (). Participants gave verbal consent to participate during their first interview (I1). All interviews were guided by HM and conducted in French. The privileged contact with HM allowed for deep and authentic exchanges during the sequence of interviews, thereby generating an extremely rich set of qualitative data.
The interviews were organized in two pairs: the first pair of interviews (I1, at the start of the MOOC, and I3, at the end of the MOOC) focused on a video of a modelled supervision (same video in both interviews). The second pair of interviews (I2, between modules 3 and 6, and I4, between three and six months after completing the MOOC) centered on two distinct audio-taped supervisions of the participants themselves. Interviews were transcribed to generate French anonymized verbatim and selected quotes were translated to English for the purpose of this research article by a native English speaker.
Data analysis
Theoretical frameworks
We developed a coding grid for analyzing the participants’ development of pedagogical competencies throughout and beyond their participation in the MOOC SCR using theoretical frameworks about the development of a clinical teacher’s pedagogical competencies [Citation24] and dual professional identity [Citation11,Citation58,Citation60]. Indeed, physicians have a dual role in the clinical setting as they provide patient care (clinical role) while teaching trainees (supervising role) [Citation62,Citation63]. Considering that ‘excellence in clinical teaching is at the top of the pyramid of complexity and expertise’ [Citation24], efficient supervisors have to go beyond the development of knowledge and skills in clinical education [Citation64]. The search for excellence as a clinical teacher requires concurrently acquiring and organizing medical knowledge, knowledge about patients and contexts and pedagogical knowledge [Citation24]. The transformation of these different forms of knowledge and their integration into a supervisor’s teaching scripts [Citation24] mirror the development and enrichment of illness scripts [Citation65]. Combining the clinical and pedagogical reasoning processes allows a clinician to solve a patient’s problem using an appropriate illness script and to address a trainee’s need by referring to a relevant teaching script [Citation24] without being overburdened by the cognitive load this implies [Citation24,Citation66]. As good clinical teachers identify as clinicians and as teachers alike [Citation58–60,Citation67,Citation68], the development of this dual professional identity is thus of importance in light of clinical supervision competencies.
Interview guides
We elaborated four interview guides using open questions related to the theoretical frameworks described above (Supplementary File 4). Each of the four interviews I1-I4 () was organized in three phases
an introductory phase, exploring the clinical and the teaching contexts of the participant as well as their expectations and needs in terms of training (I1) or their advancement in the MOOC and the difficulty of combining clinical and teaching activities (I2, I3, and I4)
an observatory phase, consisting in visualizing a video of a modelled supervision (I1 and I3, same video in both interviews) or in listening to a recorded supervision of the participant (I2 and I4, two distinct supervisions)
a debriefing and development phase, exploring the participant’s reaction to the observed supervision and their representations of how to evolve in their practice and of their teaching scripts
Thematic analysis
The qualitative arm aimed at identifying how partaking in the MOOC SCR contributed to the development of clinical reasoning supervision skills and corresponding attitudes. To understand the experiences and perceptions of the participating clinical supervisors, we used a phenomenological approach and performed thematic analysis as described by Braun and Clarke [Citation69]. We used both a deductive approach, using the coding grid developed through the conceptual frameworks presented above, and an inductive approach, permitting the elaboration of data-driven codes to enrich the analysis. Transcribed interviews were analyzed using coding software ATLAS.ti version 9 through an iterative coding process on a first transcript by three researchers (SW, HM, and MCA) to determine their alignment, and then by two pairs of researchers (SW/HM and SW/MCA) for all consecutive transcripts. All three authors first individually grouped the codes into categories that allowed defining main themes. Themes and categories were then refined based on discussions among them. The final themes and categories were described and illustrated with quotes illustrating the development of the participants’ pedagogical competencies.
Integration of qualitative and quantitative data and analyses
In order to provide a comprehensive understanding of the impact of distance teaching and its underlying mechanisms on the development of complex pedagogical competencies, this study provided integration of qualitative and quantitative data at multiple levels [Citation70]. At the level of the study design, the integration was materialized through the parallel convergent design allowing furthermore to triangulate the obtained data (). At the level of the study methods, the integration occurred by linking data collection and analysis methods through embedding [Citation70]. The connection of the quantitative and qualitative datasets occurred via participant sampling and by matching the explored dimensions in both arms through shared theoretical frameworks underpinning the mMCTQ, the interview guides and the coding grid for thematic analysis. At the level of data reporting and interpretation, integration occurred through merging: both datasets were parallelized to assess for confirmation, expansion or discordance. A narrative approach was used to describe the integrated data thematically [Citation70]. This multilevel integration of both study arms underpins this mixed methods study.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki and approved by the University of Geneva’s Committee for Ethical Research (authorization # 201901.01). Participants to the quantitative arm consented online to participate in the study before responding to the first question of Q1 via the institutional survey software LimeSurvey. The LimeSurvey databases are stored on the University’s central servers in compliance with the Swiss federal and cantonal legislation on data protection and could be accessed by MCA, AM, CP and HM. Database extracts consisted in text files, where each line represented the ratings of one participant. No participant identifier such as e-mail address, name, date of birth or any other, was attached to the line.
Participants to the qualitative arm gave verbal consent to participate in the qualitative research during their first interview (I1). HM knew the participants as described above, and conducted the interviews. AM and CP transcribed the interviews without knowing the interviewees and coded the participants from P01 to P08. Participants’ names did not appear anywhere in the transcribed files. No compensation was provided to participate in either arm of the study.
Results
Quantitative study arm
Sociodemographic characterization of MOOC participants
A total of 3734 persons registered to the MOOC on SCR on Coursera or EduLib between January 2019 and October 2021. Of those, 405 (10.85%) participated to Q1 (module 1), among which 48 (11.86%) also participated to Q4 (module 8), thus constituting the sample of participants of the quantitative arm of this study. The distribution of age classes and professions of those participants is summarized in .
Table 2. Sociodemographic characteristics of MOOC participants to the quantitative arm of the study. *: ambulatory and hospital settings. MOOC: Massive open online course, Q: questionnaire, NA: non-applicable.
Self-assessed clinical supervision skills
We used the self-assessed mMCTQ to measure participants’ perceptions of their clinical supervision skills and attitudes in six dimensions at the beginning (Q1) and at completion (Q4) of the MOOC SCR.
The mean score of all but two mMCTQ items increased between Q1 and Q4 indicating an increase in self-assessed supervision skills. The paired t-test revealed a statistically significantly increased score for items in the dimensions Role modelling, Coaching, Articulation, Exploration, and Professional Identity formation (). The majority of items (17/24) had a mean score of more than 3 out of 4 in Q1, indicating a rather strong initial agreement with the different items. This proportion increased to 24/24 items in Q4. These results suggest that the participants perceived a positive evolution of their role modelling (items 2 and 3) and coaching (items 6 and 7) competencies and increasingly perceived themselves as accompanying their students in becoming aware of and developing their clinical reasoning process (items 9, 10 and 12). In addition, participants demonstrated an increasingly developed professional identity as clinical teachers between starting and completing the MOOC (items 19, 21, 22 and 23); even though most items corresponding to this dimension exhibited the lowest mean score across dimensions in both Q1 and Q4.
Table 3. Mean scores for all questionnaire items in Q1 and Q4. Statistically significant increases are highlighted in yellow. Q: questionnaire, NS: non-significant, m: mean, std: standard deviation.
To provide insights into the change in rating frequency distributions underlying item scores in Q1 and Q4, we computed the proportion of respondents that increased, maintained and decreased their agreement rating with each item’s statement between Q1 and Q4 (Supplementary file 5). The majority of respondents maintained their agreement rating between Q1 and Q4. For all but three items, the proportion of respondents increasing their agreement with each item’s statement was greater than the proportion decreasing their agreement. We compared the proportion of respondents globally agreeing (aggregating ratings for ‘Totally agree’ and ‘Partially agree’) and disagreeing (aggregating ratings for ‘Totally disagree’ and ‘Partially disagree’) with each item’s statement in Q1 and in Q4 using McNemar’s test for paired nominal data (). The proportion of respondents agreeing with an item’s statement increased for all items except for those in the dimension Learning environment, where all respondents maintained agreement between Q1 and Q4. Likewise, the proportion of respondents disagreeing with an item’s s statement decreased. Those changes in proportions were significantly different for two items of the dimension Modelling, and for three items from the dimensions Coaching, Articulation and Professional Identity Development respectively.
Table 4. Comparison of proportions of respondents agreeing and disagreeing with each item’s statement in Q1 and Q4 using McNemar’s test for paired data. Na: McNemar’s test non-applicable since one proportion equal to 0. Q: questionnaire, NS: non-significant.
Qualitative study arm
Sociodemographic description of the participants of the qualitative arm of the study
The sociodemographic information of the qualitative study’s participants is summarized in . About one third of the members of the [nationality] community of practice interested in pedagogy (n = 8/25) agreed to participate in the qualitative study and participated in the first semi-directed interview (I1) at the start of the MOOC SCR. Among those, four (50%) participants pursued with the MOOC and participated in interviews I2 and I3. One participant did not terminate the MOOC and hence did not participate in the follow up interview (I4).
Table 5. Sociodemographic characteristics of MOOC participants to the qualitative arm of the study. MOOC: massive open online course, F: female, M: male, I: interview.
Thematic analysis
The qualitative arm of the study aimed at exploring the development of complex pedagogical competencies of a subsample of MOOC participants during their progression within the course and beyond through a series of semi-directed interviews (). The thematic analysis of the interviews’ contents allowed us to identify two main themes suggesting the development of competencies and posture:
A progression in pedagogical practice, evidenced by an increasingly precise and analytical pedagogy, consciously organized supervisions and a developed reflexivity about their own practice
A developed pedagogical attitude through an embodied dual clinician-teacher professional identity, illustrated by an increased feeling of legitimacy as supervisors, by the desire to share the gained competencies with their peers and by a demonstrated reflexivity about their pedagogical posture
Here, we present these findings based on the participants’ trajectories within the MOOC. We illustrate how the participants’ progression occurred in each particular context and how its extent and reach were shaped by their interaction with the course’s content, by their motivation to engage in the MOOC or by their previous experience in clinical supervision. The verbatim illustrating the developments of the different participants are referred to under the form of participant X – quote Y (PX-Y) and regrouped in Supplementary File 6.
Progression in pedagogical practice
Analytical and focused pedagogy
During the first interview, participants often referred to their pedagogical skills as being based on intuition rather than on formal training (P01–1, P04–2, P08–1). The discussions about the video of a simulated supervision (I1) or reflections on their own practice (I2) also illustrated these non-analytical approaches through long and poorly structured discourses that contained little pedagogical jargon. On several occasions, participants failed to precisely identify the clinical reasoning problems exposed in the recorded supervisions (P04–1, P05–1, P08–2). The discussion of the same simulated supervision and the reflections on their own practice towards completion of the MOOC revealed enriched teaching scripts through a much more structured and analytical approach (P01–3) marked by explicit pedagogical terminology and key concepts adapted to the learners’ level (P04–3, P05–2). Despite this progress, one of those participants was not yet able to correctly diagnose a premature closure in her last supervision, showing the persistent progress margin (P04–4). One of the participants explicitly reported now assuming her intuition and using it as a basis for addressing encountered difficulties (P01–2). The participant that did not terminate the MOOC did not demonstrate an elaboration of her teaching scripts. In I3, she rather reported situations in which she re-experienced similar blockades with her students and described similar attempts to remedy them than the ones reported during I1 (P08–3).
Tools for and organization of efficient supervisions
At the beginning, participants did not seem to make use of particular methods to carry out efficient supervisions. They struggled to explicitly determine pedagogical objectives with and for their students (P04–5,6, P05–3, P08–4) and to address encountered clinical reasoning difficulties of their students in relevant ways (P01–4,5,6). Alongside the lack of methodological framework to identify and remedy the encountered clinical reasoning difficulties, they also referred to the tensions between the clinical and the teaching agendas as a barrier to carrying out efficient supervisions (P05–4, P04–7, P08–5,6). After participating in the MOOC, the same participants exposed clear strategies to organize their supervisions (P01–7, P04–8) and to address a clinical reasoning problem considering the context and the learner (P05–5, P04–9). They expressed satisfaction about how they managed to dissect encountered situations and determine pedagogical objectives for their students (P01–8,9). While some participants explicitly associated those pedagogical competencies with the MOOC (P05–6, P01–8,9), the participant that did not terminate the MOOC clearly expressed her status-quo concerning her pedagogical practice. She did not manage to operationalize her motivations to develop her supervision competencies due to work overload and difficulties to organize dedicated time to practice the encountered techniques (P08–7,8).
Demonstration of increased reflexivity about their own practice
After completing the MOOC, participants demonstrated increased reflexivity about their own practice. One participant exposed how the MOOC had enriched her practice with a variety of tools that she was eager to try out in order to build and elaborate teaching scripts (P01–10) and demonstrated reflexivity on the strengths and weaknesses of her own practice in light of the acquired tools (P01–11). She further reflected on how her increased pedagogical awareness had rendered recent supervisions highly interesting, thereby continually nurturing her practice (P01–12). Another participant reflected how the MOOC had helped her feel calmer and more structured in her supervisions (P04–10), and on how future recalls of the learnt concepts were going to enact periodic reflection on the evolution of her own practice (P04–11). A third participant reflected on the shortcomings of his past practice in light of the gained knowledge (P05–7) and on how the learnt concepts were going to shape his future practice (P05–8,9). While the participant who did not terminate the MOOC did not demonstrate evolved competencies, participation in the MOOC and in the interviews for this research project did stir up reflections on her practice (P08–9) and the challenges associated to the high cognitive burden of the daily work preventing mental availability to integrate the taught concepts (P08–10). Those difficulties, mainly caused by a lack of pedagogical practice and skills, hindered her reasoning in terms of teaching scripts, thereby impeding the parallel clinical and pedagogical reasoning processes. This in turn resulted in long, inefficient supervisions, overburdening her mentally and eventually causing her to abandon the MOOC.
A changing attitude through the embodiment of a dual clinician-teacher professional identity
Increased perceived legitimacy for the supervisor role
Feeling legitimate as clinical supervisor contributes to a professional identity as clinician and as teacher [Citation68]. Several participants shared the feeling of poor legitimacy as supervisors during the first interviews, mainly fueled by the lack of formal training in this role (P04–12, P05–10). Through their participation in the MOOC, some participants reported gained legitimacy and improved confidence as clinical supervisors through the acquired knowledge, tools and competencies (P05–11, P01–13). One participant yet reported a lack of confidence as clinical supervisor even though she recalled tools from the MOOC that she was eager to use in future supervision situations, demonstrating the integration of the taught concepts (P04–13). During the last interview, she eventually expressed satisfaction about how her handling of a recent supervision had been successful and satisfying for her (P04–14).
Eagerness to transmit and to share the gained expertise with colleagues
The development of the professional identity as a clinical teacher was also materialized by the desire to transmit the gained skills to colleagues [Citation60,Citation67]. Indeed, during the first interview, several participants voiced frustrations about the absence and non-harmonization of existing trainings in supervising clinical reasoning (P01–14, P08–11). After completing the MOOC, several participants expressed their desire to disseminate the acquired concepts (P01–15, P05–12, P08–12), demonstrating the eagerness to contribute to the development of pedagogical cultures in their departments.
Developed reflexivity about attitude as clinician and teacher
Finally, participants also demonstrated an increased reflexivity about their attitude and posture. One participant, who previously prioritized the clinical duty over the teaching duty, now demonstrated awareness about his pedagogical identity (P05–13) and reflected on the challenges associated with the role of the supervisor (P05–14). He valued the MOOC and the participation in this study as an opportunity to reflect on his practice, demonstrating professionalism and a changed attitude towards his job (P05–15). Another participant reflected on the parallel between the pedagogical and clinical reasoning and diagnoses processes (P01–16), demonstrating a deep integration of the concepts into her posture. She further exposed how the acquired competencies conferred her the necessary confidence and skills to supervise a future student with difficulties that was being referred to her specifically because of her pedagogical competencies (P01–17). Overall, the participant that did not terminate the MOOC evolved little in her posture: albeit characterized by a well-developed starting reflexivity on the complementarity of the clinical and the pedagogical identities (P08–13), this reflexivity remained confined by struggles in efficiently embodying this double role during the daily work (P08–14).
Factors influencing the extent and reach of the participants’ progression and change in attitude
Interaction with the MOOC’s content
We identified that the participants all interacted in their own way with the MOOC’s content. For instance, participant P01 demonstrated an in-depth appropriation of the course’s content, illustrated among others by her printing out different supervision tools and testing them with her students. She exposed the most prominent development in her practice (adoption of multiple concepts and tools from the MOOC and expressing satisfaction about their efficiency) and in her posture (paralleling clinical and pedagogical reasoning or being referred to for students with difficulties). Another participant, P04, went through the MOOC to the best of her abilities, trying to free enough time (2 or 3 h in a row) to actively engage with the content during each session, which she identified as a challenge. Her progression, while slowed down by a maternity leave, was neat in terms of pedagogical reasoning and supervision techniques but less prominent in terms of attitude, confidence and capacity to explicitly and correctly diagnose a particular pedagogical problem. A third participant, P05, displayed a more superficial interaction with the course’s content and did not completely integrate the different tools presented in the course, as evidenced by difficulties recalling them during the interviews. He progressed rapidly in series of shorter sessions (<1 h at a time) and reported visualizing most of the videos at an increased speed. However, he hailed the self-reflective questions at the end of each module as an important moment to take a step back and recognize what had been learnt and demonstrated a shift from clinically-centered to student-centered supervisions as he progressed within the MOOC. The fourth participant, P08, did not manage to terminate the MOOC due to overwork and the incapacity to periodically free time slots to dive into the course’s content. She did not demonstrate much progression in pedagogical practice or posture.
Motivation to engage and continue with the MOOC
Most participants exposed intrinsic motivations to start and continue the MOOC, such as the desire to learn and to improve one’s practice. This could be associated with a deeper acquisition of skills and corresponding pedagogical attitudes (i.e. P01). Participants also reported extrinsic motivations, such as the desire for recognition or legitimacy, which could be associated with a more superficial learning and a weaker progression in pedagogical competencies (i.e. P05). One participant, P04, suggested that the flexible schedule and the availability online were additional attractors of this MOOC. Most of the participants agreed that the series of interviews in the context of the qualitative study constituted another important motivational driver to regularly progress within the course’s content and to debrief on the encountered concepts.
Experience in supervision at MOOC start
While all participants displayed some type of progression in their pedagogical competencies, novice supervisors (for instance P04 or P05, ) appeared to start from a lower level of competencies and their progression most markedly occurred in their practice and less in their posture. Experienced supervisors on the other hand started the MOOC with a well-developed reflexivity on the importance of pedagogy in medical education (for instance P01 or P08, ). Their respective progression however was impacted by their trajectory within the MOOC: while P01 impressively internalized the MOOCs concepts and further developed her pedagogical practice and her professional identity as clinician and as teacher, P08, who did not terminate the MOOC, did not demonstrate the same type of progression.
Integration of qualitative and quantitative data
The integration of quantitative and qualitative data allowed us to gain an in-depth understanding of the impact and underlying mechanisms of the MOOC SCR on the development of complex pedagogical competencies. The quantitative data, stemming from all MOOC participants, suggested a moderate but generalized increase in self-reported supervision skills across explored dimensions. This result was further underpinned by a significant increase in the proportion of respondents agreeing with items between Q1 and Q4. The qualitative data, stemming from a purposefully sampled sub-population of MOOC participants, illustrated how this progression occurred in practice in different contexts and particularly, how its extent and reach were shaped by their interaction with the course’s content, their motivational drivers or their previous experience in clinical supervision. The integration of both results enabled an expanded understanding of the phenomenon at study and is hereunder presented using a narrative approach that describes the results thematically [Citation70].
Progression in pedagogical practice
Numerous items from the mMCTQ demonstrated improvement in self-assessed clinical supervision skills between starting and completing the MOO, which aligned with the witnessed progression in pedagogical competencies of the interview participants. More specifically, the questionnaire results demonstrated improved perceptions of participants’ mastery of supervision techniques and pedagogical concepts (items 10, 12, 14, 19, 22 and 23), which was very well reflected in the qualitative interviews, through an increasingly focused and analytical pedagogy and expressed satisfaction about the usage of different tools. Similarly, questionnaire respondents reported an improved perception of their abilities to adjust their teaching to their trainees’ level (item 6), a competency that was also demonstrated by the participants during the interviews. The participants to the qualitative arm also demonstrated an increased reflexivity concerning their own practice, which was reflected in the questionnaire results through role modelling items and professional identity development items.
Embodied dual clinician-teacher professional identity
The interviews of the qualitative arm revealed the development of a clinical teacher professional identity and the corresponding attitude among participants. Legitimacy in the role of a clinical teacher emerged to be a very important aspect, which was fuelled by gain in self-confidence with regards to teaching and supervising. Improved self-confidence about the gained competencies as clinical teacher was reflected in some of the assertive mMCTQ items (I create sufficient opportunities, I provide relevant feedback). Another component of the developing professional identity as clinical teacher was sharing with colleagues and contributing to a community of practice. While participants to the qualitative arm reported eagerness to transmit the learnt concepts, they did not explicitly describe contributions to establishing pedagogical standards in their workplace. Similarly, the score of the corresponding item in the mMCTQ (item 20) was among those, whose score was relatively low in Q1 and increased little in Q4. The development of the professional identity was also associated to an increased reflexivity about participants’ posture as clinical teachers during the interviews. Also, the mMCTQ revealed how participants may perceive themselves increasingly as clinical teachers, as demonstrated by an improved perception of their ability to focus on their students’ needs during supervisions, rather than remaining with the clinical agenda (items 22, 23, 24).
This integration of qualitative and quantitative datasets allowed to demonstrate either confirmation or expansion of our understanding of the studied concepts and grounds our findings and catalyses their impact.
Discussion
In the aftermath of a COVID-19-enforced rapid and massive implementation of distance teaching [Citation36–38], numerous calls emerged to take the lessons learnt and promote sustainable and efficient distance education of health care professionals [Citation20,Citation39–41,Citation71]. In this framework, we analyzed the qualitative and quantitative data issued from nearly three years of participation to the MOOC SCR to explore whether and how distance education can promote the development of complex pedagogical competencies in clinical teachers. The findings from both quantitative and qualitative study arms demonstrate convergence and show that MOOC participants developed their supervision skills and corresponding attitudes throughout and beyond the course. The integration of both study arm analyses underpinned and enriched those findings and further allowed to comprehensively describe how those developments occurred. In this discussion, we build on those integrated results and discuss the complexity of the targeted competencies and the challenges associated with teaching them. We underline the relationship between the development of those competencies and the embodiment of a dual professional identity as clinical teachers. We then discuss challenges and opportunities of distance teaching for promoting the development of complex pedagogical competencies and conclude with our study’s strengths and limitations.
Complexity of supervising clinical reasoning
Our study results demonstrate the complexity of clinical supervision competencies and of using them in relevant ways in the clinical setting. Our findings corroborate similar observations in the literature that illustrate how efficient and relevant supervisions of clinical reasoning require knowledge, skills and attitudes that go beyond the correction of a wrong diagnosis, the sharing of illness scripts with trainees of providing feedback after a clinical encounter [Citation24,Citation63,Citation72–74]. In particular, a growing body of literature argues that developing expertise in clinical teaching occurs through the elaboration and practicing of teaching scripts that guide supervisors’ pedagogical reasoning process during supervision situations [Citation24,Citation72,Citation75]. Such teaching scripts, in analogy to illness scripts for clinical reasoning, guide supervisors through establishing pedagogical diagnoses and issuing pedagogical prescriptions for their trainees. The joint application of both script theories eases the cognitive burden of this parallel reasoning process and permits high quality care of both the learner and the patient without overloading working memory [Citation24,Citation66,Citation72]. While the MOOC aimed at developing awareness about and promoting this parallel reasoning process, the results of our study show that participants that managed to engage in the parallel reasoning process demonstrated excellent supervision skills and expressed satisfaction about their supervisions, which can in part be attributed to the fact that they were easier for them, with less cognitive load.
Co-construction of pedagogical competencies and a clinical teacher professional identity
Our longitudinal study allowed exploring the progressive development of the participants’ pedagogical attitudes throughout and beyond their participation in the MOOC. The quantitative findings suggested that at course completion, participants generally felt more competent across all dimensions related to clinical teacher performance, including their professional identity as clinical teachers. The qualitative results enriched those findings by illustrating how the degree of improved pedagogical practice (‘better’ teaching) was intimately linked to the extent of the evolved posture as clinical teachers (‘better’ attitude). This co-construction of pedagogical competencies and professional identity on the path towards excellence as clinical teachers is congruent with works by Starr et al. [Citation58], Steinert et al. [Citation76] and others [Citation59,Citation68]. As the development of supervision skills improved participants’ practice, their self-confidence in establishing pedagogical diagnoses and issuing pedagogical prescriptions improved. This increased self-confidence in turn improves clinical teachers’ perceived capabilities to teach, engendering satisfaction, external recognition and often, the desire to share their expertise and develop those competencies in others. Those internal and external elements have been associated with a strong teacher identity in health care professionals [Citation58,Citation60,Citation77,Citation78]. Indicators for the development or presence of a professional identity situate practitioners at the apex of the pyramid assessing medical competence by demonstrating not only excellent medical skills but also the corresponding and necessary professional attitude [Citation35]. Given the co-construction of pedagogical competencies and professional identity, faculty development initiatives promoting the acquisition of teaching skills and competencies may therefore focus in parallel on the awakening or strengthening of clinical teacher’s professional identity [Citation76,Citation79,Citation80].
Distance learning: the importance of participant motivation and engagement for the development of complex competencies
Our results reveal how different learner profiles interacted in various ways with the learning material and environment and suggest that the corresponding behavioral engagement impacted the breadth and reach of the participants’ learning. Poellhuber et al. described different participant profiles and interaction patterns with learning material based on participants’ traces within a MOOC and mapped them onto a continuum of behavioral engagement that reflected their performance in test results [Citation81]. While generalizing those findings to ‘good interaction with course content causes good learning’ may be stretched as numerous factors account for the depth and quality of the learning, there is general agreement that active learner engagement favors high quality learning [Citation42,Citation82]. Being actively engaged in a course reflects commitment and motivation and is facilitated by contextual, relevant learning experiences with which participants identify [Citation31,Citation82,Citation83]. These considerations may be particularly important 1) in distance education, where drop-out rates are high [Citation22,Citation23], and 2) for the development of complex competencies as opposed to acquiring declarative knowledge. The authenticity of the MOOC SCR, through the numerous situational videos, self-reflective prompts and self-evaluation quizzes, allowed participants to deeply relate to and engage with the learning material [Citation52]. Participants were also engaged through possibilities to exchange about their practice: while the openness of the MOOC provided the opportunity to individualize the time and depth of the learning experience, the opportunity to discuss and engage in feedback via the online discussion boards, dedicated workshops at medical education conferences or via the series of interviews may have contributed to keeping participants committed. Engaging in feedback has been extensively described as promoting high quality learning in medical education [Citation30,Citation84,Citation85]. Likewise, belonging to a community of teachers facilitates exchanges with peers and has been described as one of seven elements of the teacher identity [Citation58], which we identified as co-developing alongside complex pedagogical competencies. Creating the feeling of belonging to a community of practice by providing opportunities for engaging in feedback between teachers and participants may hence be of importance for the development of complex pedagogical competencies in clinical teachers, particularly in distance education.
Limitations
We conducted a mixed-methods study, which allowed compiling a rich and nuanced understanding of the development of complex pedagogical competencies through the MOOC SCR. While we employed rich and complementary methods to assess those developments using self-assessment, simulated recalls (video of simulated supervision) and real situational recalls (participants’ recorded supervisions), our study also has limitations. First, the study sample size in both arms is small. The small quantitative sample resulted from a large drop in participants between Q1 and Q4. This may in part be explained by the low completion rates observed with MOOCs (generally less than 10% [Citation22,Citation23]) and by the fact that many MOOC SCR participants appeared to take months to complete the course. The qualitative sample, albeit small, was composed of participants with very different trajectories. This favored a privileged and in-depth interaction with these participants and permitted a profound understanding of their progression and motives, which may have been more difficult to achieve with larger numbers of participants. The diversity and richness of the qualitative data could further allow identifying patterns and potentiate transferability of our results [Citation86]. Second, the qualitative arm’s study population stems from a single care setting – family medicine ambulatory practitioners. Future research investigating the development of supervision skills in other disciplines may therefore be warranted to enhance transferability or generalization. Third, the quantitative data was obtained from self-reported data, which might be divergent from real practice [Citation87] and on a modified version of the mMCTQ through addition of items on professional identity formation, which we did not validate psychometrically. However, we compared self-reported responses to the same items between the beginning and the end of the MOOC, a comparison that should be less vulnerable to these biases. Fourth, the quantitative findings could suffer from ceiling effects, in particular items from the dimension Learning environment of the mMCTQ, which did not increase in score between Q1 and Q4. While high initial item scores may have prevented substantial increases of the scores in Q4, this dimension has already been scoring very high in previous studies using the MCTQ or mMCTQ [Citation53,Citation54]. This dimension may therefore be inherently less discriminant for assessing clinical supervision skills. In addition, we compared response proportions of respondents globally agreeing and globally disagreeing using McNemar’s test for paired nominal data. Those computations do not suffer from ceiling effects and support our findings. Fifth, we used a forced Likert scale without neutral option, which may impede comparability with literature as the original MCTQ used a 5-point Likert scale. However, as we used the test to compare results within our study population to assess progression, this bias may be less important. For those latter limitations, it is noteworthy to stress that none withstanding potential limitation of the survey itself, the usage of a validated instrument like the MCTQ/mMCTQ strengthens our work and increases its potential impact, as it allows to situate it in existing literature and thus contribute to advance the research on clinical teaching.
Conclusion: how can distance teaching promote the development of complex pedagogical competencies?
In this study, we used validated references frameworks for the data analyses, allowing to position our work within the existing body of literature. Our qualitative results were largely congruent with the quantitative findings and allowed identifying two main themes and six sub-themes corresponding to all participants’ progression in practice and posture as clinical teachers. While the evaluation of pedagogical competencies remains rare in healthcare settings, we here provide a privileged access to clinical teachers’ perceptions of the development of those competencies and of their congruent professional identity as clinical teachers. We thereby contribute significantly to raising awareness about the importance of those competencies and attitudes, while providing evidence on their development through distance learning.
Taken together, our findings suggest that distance learning can be used to promote the development of complex pedagogical competencies in clinical teachers. It is however key to appraise those results in a larger context, as evidenced through the importance of participant commitment, their interaction with the course’s content and their integration into a community of practice. As such, the extent to which the pedagogical principles underpinning this MOOC contributed to those developments remains unclear. In the context of massification of online and distance education, it would be highly valuable to understand which design principles should be retained and could potentially be reused in similar and in different educational activities, in line with calls for sustainable and resilient teaching formats [Citation71]. Further analyses of how the different pedagogical choices of the MOOC SCR promoted the development of complex pedagogical competencies in clinical teachers would therefore be highly interesting.
Authors’ contributions
HM, NCF, CP, and MCA conceived the study. HM conducted participant interviews. CP and AM transcribed the interviews. SW, HM and MCA performed thematic analysis of the qualitative data. SW, HM, AM analyzed the quantitative data. CP, BC, HM, MCA, and SW discussed the results. SW produced figures and tables and wrote the manuscript. All authors reviewed the final manuscript.
Supplemental Material
Download MS Word (64.1 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10872981.2023.2265163
Additional information
Funding
References
- Eva KW. What every teacher needs to know about clinical reasoning. Med Educ. 2005;39(1):98–17. doi: 10.1111/j.1365-2929.2004.01972.x
- Durning S, Artino AR Jr, Pangaro L, et al. Context and clinical reasoning: understanding the perspective of the expert’s voice. Med Educ. 2011;45(9):927–938. doi: 10.1111/j.1365-2923.2011.04053.x
- Szumacher E, Catton P, Jones GA, et al. Helping learners in difficulty – the incidence and effectiveness of remedial programmes of the medical radiation sciences programme at university of Toronto and the Michener institute for applied sciences, Toronto, Ontario, Canada. Ann Acad Med Singap. 2007;36(9):725–734. doi: 10.47102/annals-acadmedsg.V36N9p725
- Yao DC, Wright SM. National survey of internal medicine residency program directors regarding problem residents. J Am Med Assoc. 2000;284(9):1099–1104. doi: 10.1001/jama.284.9.1099
- Schwind CJ, Williams RG, Boehler ML, et al. Do individual attendings’ post-rotation performance ratings detect residents’ clinical performance deficiencies? Acad Med. 2004;79(5):453–457. doi: 10.1097/00001888-200405000-00016
- Audétat MC, Dory M, Nendaz M, et al. What is so difficult about managing clinical reasoning difficulties? Med Educ. 2012;46(2):216–227. doi: 10.1111/j.1365-2923.2011.04151.x
- Smith CS, Stevens NG, Servis M. A general framework for approaching residents in difficulty. Fam Med. 2007;39(5):331–336.
- Hicks PJ, Cox SM, Espey EL, et al. To the point: medical education reviews—dealing with student difficulties in the clinical setting. Am J Obstet Gynecol. 2005;193(6):1915–1922. doi: 10.1016/j.ajog.2005.08.012
- Hunt D, Carline J, Tonesk X, et al. Types of problem students encountered by clinical teachers on clerkships. Med Educ. 1989;23(1):14–18. doi: 10.1111/j.1365-2923.1989.tb00806.x
- Schmidt HG, Mamede S. How to improve the teaching of clinical reasoning: a narrative review and a proposal. Med Educ. 2015;49(10):961–973. doi: 10.1111/medu.12775
- Audétat MC, Laurin S, Dory M, et al. Diagnosis and management of clinical reasoning difficulties: part I. Clinical reasoning supervision and educational diagnosis. Med Teach. 2017;39(8):792–796. doi: 10.1080/0142159X.2017.1331033
- Ellaway R, Masters K. AMEE Guide 32: e-learning in medical education part 1: learning, teaching and assessment. Med Teach. 2008;30(5):455–473. doi: 10.1080/01421590802108331
- Masters K, Ellaway R. E-learning in medical education guide 32 part 2: technology, management and design. Med Teach. 2008;30(5):474–489. doi: 10.1080/01421590802108349
- Masters K, Ellaway RH, Topps D, et al. Mobile technologies in medical education: AMEE guide No. 105. Med Teach. 2016;38(6):537–549. doi: 10.3109/0142159X.2016.1141190
- George PP, Papachristou N, Belisario JM, et al. Online eLearning for undergraduates in health professions: a systematic review of the impact on knowledge, skills, attitudes and satisfaction. J Glob Health. 2014;4(1). doi: 10.7189/jogh.04.010406
- Moule P, Ward R, Lockyer L. Nursing and healthcare students’ experiences and use of e‐learning in higher education. J Adv Nurs. 2010;66(12):2785–2795. doi: 10.1111/j.1365-2648.2010.05453.x
- Pettersson F, Olofsson AD. Implementing distance teaching at a large scale in medical education: a struggle between dominant and non-dominant teaching activities. Educ Inf Technol. 2015;20(2):359–380. doi: 10.1007/s10639-013-9289-1
- Saiyad S, Virk A, Mahajan R, et al. Online teaching in medical training: establishing good online teaching practices from cumulative experience. Int J App Basic Med Res. 2020;10(3):149. doi: 10.4103/ijabmr.IJABMR_358_20
- Anderson J, McCormick R. Ten Pedagogic principles for e-learning. In: McCluskey A, editor. Policy and Innovation in Education. Quality Criteria. Brussels: European Schoolne; 2005. p. 10–15.
- Rossettini G, Turolla A, Gudjonsdottir B, et al. Digital entry-level education in physiotherapy: a commentary to Inform post-COVID-19 future directions. Med Sci Educator. 2021;31(6):2071–2083. doi: 10.1007/s40670-021-01439-z
- Longhini J, Rossettini G, Palese A. Massive open online courses for nurses’ and healthcare professionals’ continuous education: a scoping review. Int Nurs Rev. 2021;68(1):108–121. doi: 10.1111/inr.12649
- Jordan K. Initial trends in enrolment and completion of massive open online courses. Int Rev Res Open Distributed Learning. 2014;15(1):133–160. doi: 10.19173/irrodl.v15i1.1651
- Wang W, Guo L, He L, et al. Effects of social-interactive engagement on the dropout ratio in online learning: insights from MOOC. Behav Inf Technol. 2019;38(6):621–636. doi: 10.1080/0144929X.2018.1549595
- Irby DM. Excellence in clinical teaching: knowledge transformation and development required. Med Educ. 2014;48(8):776–784. doi: 10.1111/medu.12507
- Caire Fon N, Poellhuber B, Audétat MC, et al. Les Massive Open Online Course (MOOC) sont-ils une méthode utile en pédagogie médicale? Éléments de réponse avec l’exemple du MOOC-Processus de raisonnement clinique. Pédagogie Médicale. 2017;18(2):47–50. doi: 10.1051/pmed/2018001
- Caire Fon N, Audétat MC, Bertrand ME, et al. Processus de raisonnement clinique [MOOC Edulib]; n.d. Available from: https://cours.edulib.org/courses/course-v1:UMontreal+PRC.5+A2018/about.
- Santen S. Enseigner et évaluer les capacités cliniques [MOOC Coursera]; n.d. 2021. Available from: https://www.coursera.org/learn/clinical-skills?ranMID=40328&ranEAID=SAyYsTvLiGQ&ranSiteID=SAyYsTvLiGQ-bRoyLfGGneHv47GJR_pC.A&siteID=SAyYsTvLiGQ-bRoyLfGGneHv47GJR_pC.A&utm_content=10&utm_medium=partners&utm_source=linkshare&utm_campaign=SAyYsTvLiGQ.
- Rodrigues V. Clinical Supervision: Teaching And Facilitating Learning [MOOC Future Learn]; n.d. Available from: https://www.futurelearn.com/courses/clinical-supervision-teaching-facilitating.
- Nash R Clinical Supervision For Health Professionals [MOOC Future Learn]; n.d. Available from: https://www.futurelearn.com/courses/clinical-supervision-health.
- Harden RM, Laidlaw JM. Be FAIR to students: four principles that lead to more effective learning. Med Teach. 2013;35(1):27–31. doi: 10.3109/0142159X.2012.732717
- Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE guide No. 63. Med Teach. 2012;34(2):e102–e115.
- Grossman R, Salas E. The transfer of training: what really matters. Int J Train Dev. 2011;15(2):103–120. doi: 10.1111/j.1468-2419.2011.00373.x
- Yelon SL, Ford JK, Anderson WA. Twelve tips for increasing transfer of training from faculty development programs. Med Teach. 2014;36(11):945–950. doi: 10.3109/0142159X.2014.929098
- Ten Cate O, Carraccio C, Damodaran A, et al. Entrustment decision making: extending Miller’s pyramid. Acad Med. 2021;96(2):199–204. doi: 10.1097/ACM.0000000000003800
- Cruess RL, Cruess SR, Steinert Y. Amending Miller’s pyramid to include professional identity formation. Acad Med. 2016;91(2):180–185. doi: 10.1097/ACM.0000000000000913
- Daniel M, Gordon M, Patricio M, et al. An update on developments in medical education in response to the COVID-19 pandemic: a BEME scoping review: BEME guide No. 64. Med Teach. 2021;43(3):253–271. doi: 10.1080/0142159X.2020.1864310
- Stojan J, Haas M, Thammasitboon S, et al. Online learning developments in undergraduate medical education in response to the COVID-19 pandemic: a BEME systematic review: BEME guide No. 69. Med Teach. 2022;44(2):109–129. doi: 10.1080/0142159X.2021.1992373
- Bastos RA, Carvalho DRS, Brandão CFS, et al. Solutions, enablers and barriers to online learning in clinical medical education during the first year of the COVID-19 pandemic: a rapid review. Med Teach. 2022;44(2):187–195. doi: 10.1080/0142159X.2021.1973979
- Pelaccia T, Demeester A, Charlin B, et al. Le déploiement de la formation à distance au sein des facultés de médecine dans le contexte de la crise sanitaire liée à la COVID-19: et après? Pédagogie Médicale. 2020;21(4):173–174. doi: 10.1051/pmed/2020055
- Brady AK, Pradhan D. Learning without borders: asynchronous and distance learning in the age of COVID-19 and beyond. ATS Scholar. 2020;1(3):233–242. doi: 10.34197/ats-scholar.2020-0046PS
- Watson A, McKinnon T, Prior SD, et al. COVID-19: time for a bold new strategy for medical education. Med Educ Online. 2020;25(1):1764741. doi: 10.1080/10872981.2020.1764741
- Biggs J, Tang C. Teaching for quality learning at university. UK: McGraw-Hill Education; 2011.
- Jacquinot G. Apprivoiser la distance et supprimer l’absence ? ou les défis de la formation à distance. Revue Française de Pédagogie. 1993;102(1):55–67. doi: 10.3406/rfp.1993.1305
- Peraya D. Un regard critique sur les concepts de médiatisation et médiation: nouvelles pratiques, nouvelle modélisation. Les Enjeux de l’information et de la communication. 2008;9(2). https://lesenjeux.univ-grenoble-alpes.fr/2008/supplement-a/12-un-regard-critique-sur-les-concepts-de-mediatisation-et-mediation-nouvelles-pratiques-nouvelle-modelisation/
- Carré P, Wright GM, Wadowska DW. Motifs et dynamique d’engagement en formation. Éducation permanente. Mol Cell Endocrinol. 1998;136(2):119–131. doi: 10.1016/s0303-7207(97)00220-7
- Audetat MC, Nendaz M, Caire Fon N, et al. Supervision du raisonnement clinique [MOOC Coursera]; n.d. Available from: https://www.coursera.org/learn/supervision-raisonnement-clinique.
- Audetat MC, Nendaz M, Caire Fon N, et al. Supervision du raisonnement clinique [MOOC Edulib]; n.d. Available from: https://cours.edulib.org/courses/course-v1:UMontreal+SRC-2.1+P2018/about.
- Harden RM, Sowden S, Dunn WR. Educational strategies in curriculum development: the SPICES model. Med Educ. 1984;18(4):284–297. doi: 10.1111/j.1365-2923.1984.tb01024.x
- Sandars J. The use of reflection in medical education: AMEE guide No. 44. Med Teach. 2009;31(8):685–695. doi: 10.1080/01421590903050374
- Creswell JW, Clark VLP. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage publications; 2017.
- O’Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy. 2008;13(2):92–98. doi: 10.1258/jhsrp.2007.007074
- Peltier C, Campion B, Wurth S, et al. Intentions pédagogiques et perceptions d’un dispositif de formation médiatisée : analyse de réception médiatique d’un MOOC à visée professionnalisante. Revue Internationale des Technologies en Pédagogie Universitaire. 2023;20(1):35–55. doi: 10.18162/ritpu-2023-v20n1-03
- Boerboom TBB, Dolmand DHJM, Jaarsma D, et al. Exploring the validity and reliability of a questionnaire for evaluating veterinary clinical teachers’ supervisory skills during clinical rotations. Med Teach. 2011;33(2):e84–e91. doi: 10.3109/0142159X.2011.536277
- Stalmeijer RE, Dolmans DHJM, Wolfhagen IHAP, et al. The Maastricht clinical teaching questionnaire (MCTQ) as a valid and reliable instrument for the evaluation of clinical teachers. Acad Med. 2010;85(11):1732–1738. doi: 10.1097/ACM.0b013e3181f554d6
- Boerboom TBB, Jaarsma D, Dolmans DHJM, et al. Peer group reflection helps clinical teachers to critically reflect on their teaching. Med Teach. 2011;33(11):e615–e623. doi: 10.3109/0142159X.2011.610840
- Bearman M, Tai J, Kent F, et al. What should we teach the teachers? Identifying the learning priorities of clinical supervisors. Adv Health Sci Educ. 2018;23(1):29–41. doi: 10.1007/s10459-017-9772-3
- Audetat Voirol M-C, Cerutti B, Rieder A, et al. Perceptions of clinical supervision in ambulatory settings: do supervisee and supervisors see eye to eye? Creative Educ. 2020;11(3):297–306. doi: 10.4236/ce.2020.113023
- Starr S, Ferguson WJ, Haley H-L, et al. Community preceptorsʼ views of their identities as teachers. Acad Med. 2003;78(8):820–825. doi: 10.1097/00001888-200308000-00017
- Audétat M-C, Grégoire G, Fernandez N, et al. From intuition to professionalization: a qualitative study about the development of teacher identity in internal medicine senior residents. Int J Health Promot Educ. 2017;1(1):5–12. doi: 10.17267/2594-7907ijhe.v1i1.1234
- Starr S, Haley H-L, Mazor KM, et al. Initial testing of an instrument to measure teacher identity in physicians. Teach Learn Med. 2006;18(2):117–125. doi: 10.1207/s15328015tlm1802_5
- Nadler JT, Weston R, Voyles EC. Stuck in the middle: the use and interpretation of mid-points in items on questionnaires. J Gen Psychol. 2015;142(2):71–89. doi: 10.1080/00221309.2014.994590
- Ramani S, Leinster S. AMEE Guide no. 34: teaching in the clinical environment. Med Teach. 2008;30(4):347–364. doi: 10.1080/01421590802061613
- Kilminster S, Cottrell D, Grant J, et al. AMEE guide No. 27: effective educational and clinical supervision. Med Teach. 2007;29(1):2–19. doi: 10.1080/01421590701210907
- Higgs J, Mcallister L. Being a clinical educator. Adv Health Sci Educ. 2007;12(2):187–200. doi: 10.1007/s10459-005-5491-2
- Charlin B, Boshuizen HPA, Custers EJ, et al. Scripts and clinical reasoning. Med Educ. 2007;41(12):1178–1184. doi: 10.1111/j.1365-2923.2007.02924.x
- Muller-Juge V, Pereira Miozzari AC, Rieder A, et al. A medical student in private practice for a 1-month clerkship: a qualitative exploration of the challenges for primary care clinical teachers. Adv Med Educ Pract. 2018;9:17. doi: 10.2147/AMEP.S145449
- de Carvalho-Filho MA, Tio RA, Steinert Y. Twelve tips for implementing a community of practice for faculty development. Med Teach. 2020;42(2):143–149. doi: 10.1080/0142159X.2018.1552782
- Stone S, Ellers B, Holmes D, et al. Identifying oneself as a teacher: the perceptions of preceptors. Med Educ. 2002;36(2):180–185. doi: 10.1046/j.1365-2923.2002.01064.x
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa
- Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–2156. doi: 10.1111/1475-6773.12117
- Quintana RM, Fortman J, DeVaney J. Advancing an approach of resilient design for learning by designing for extensibility, flexibility, and redundancy. In: Thurston TN, Lundstrom K, and González C, editors Resilient pedagogy: practical teaching strategies to overcome distance, disruption, and distraction. Utah State University; 2021. p. 77–92.
- Côté L, Bordage G. Content and conceptual frameworks of preceptor feedback related to residents’ educational needs. Acad Med. 2012;87(9):1274–1281. doi: 10.1097/ACM.0b013e3182623073
- Pereira Miozzari AC, Rieder AR, Sader J, et al. Clinicians or teachers–why not both? Expanding the comfort zone of Swiss clinical teachers in private practice. Swiss Med Wkly. 2020.
- Lubarsky S, Dory V, Audétat M-C, et al. Using script theory to cultivate illness script formation and clinical reasoning in health professions education. Can Med Educ J. 2015;6(2):e61–e70. doi: 10.36834/cmej.36631
- Moghadami M, Amini M, Moghadami M, et al. Teaching clinical reasoning to undergraduate medical students by illness script method: a randomized controlled trial. BMC Med Educ. 2021;21(1):1–7. doi: 10.1186/s12909-021-02522-0
- Steinert Y, O’Sullivan PS, Irby DM. Strengthening teachers’ professional identities through faculty development. Acad Med. 2019;94(7):963–968. doi: 10.1097/ACM.0000000000002695
- Steinert Y, Macdonald ME. Why physicians teach: giving back by paying it forward. Med Educ. 2015;49(8):773–782. doi: 10.1111/medu.12782
- Hu WC, Thistlethwaite JE, Weller J, et al. ‘It was serendipity’: a qualitative study of academic careers in medical education. Med Educ. 2015;49(11):1124–1136. doi: 10.1111/medu.12822
- Sternszus R, Boudreau JD, Cruess RL, et al. Clinical teachers’ perceptions of their role in professional identity formation. Acad Med. 2020;95(10):1594–1599. doi: 10.1097/ACM.0000000000003369
- van Lankveld T, Thampy H, Cantillon P, et al. Supporting a teacher identity in health professions education: AMEE guide No. 132. Med Teach. 2021;43(2):124–136. doi: 10.1080/0142159X.2020.1838463
- Poellhuber B, Roy N, Bouchoucha I. Understanding participant’s behaviour in massively open online courses. Int Rev Res Open Distributed Learning. 2019;20(1). doi: 10.19173/irrodl.v20i1.3709
- Harden RM, Laidlaw JM. Essential skills for a medical teacher: an introduction to teaching and learning in medicine. Elsevier Health Sciences: 2020. doi: 10.33029/9704-5958-4-2021-KLN-1-376
- Jia M, Gong D, Luo J, et al. Who can benefit more from massive open online courses? A prospective cohort study. Nurse Educ Today. 2019;76:96–102. doi: 10.1016/j.nedt.2019.02.004
- Teunissen PW, Stapel DA, van der Vleuten C, et al. Who wants feedback? An investigation of the variables influencing residents’ feedback-seeking behavior in relation to night shifts. Acad Med. 2009;84(7):910–917. doi: 10.1097/ACM.0b013e3181a858ad
- Ramani S, Krackov SK. Twelve tips for giving feedback effectively in the clinical environment. Med Teach. 2012;34(10):787–791. doi: 10.3109/0142159X.2012.684916
- Albarello L. Choisir l’étude de cas comme méthode de recherche. In: De Boeck, editor. Méthodes en sciences humaines. De Boeck; 2011. p. 144.
- Norman G, Norcini J, Bordage G. Competency-based education: milestones or millstones? J Grad Med Educ. 2014;6(1):1–6. doi: 10.4300/JGME-D-13-00445.1

