Abstract
Background
Patients with multimorbidity who frequently contact the general practice, use emergency care or have unplanned hospitalisations, may benefit from a proactive integrated care intervention. General practitioners are not always aware of who these ‘high need’ patients are. Electronic medical records are a potential source to identify them.
Objectives
To find predictors of high care needs in general practice electronic medical records of patients with multimorbidity and assess their predictive value.
Methods
General practice electronic medical records of 245,065 patients with ≥2 chronic diseases were linked to hospital claims data. Probit regression analysis was conducted to predict i) having at least 12 general practice contacts per year, ii) emergency department visit(s), and iii) unplanned hospitalisation(s). Predictors were patients’ age, sex, morbidity, health services and medication use in the previous year.
Results
11% of multimorbid patients had ≥12 general practice contacts, which could be reliably predicted by the number of contacts in the previous year (PPV 42%). The model containing all predictors had only slightly better predictive value (PPV 44%). Emergency department visits and unplanned hospitalisations (12% and 7% of multimorbid patients, respectively) could be predicted less accurately (PPV 27% and 20%). Those with frequent contact with the general practice hardly overlapped with ED visitors (29%) or persons with unplanned hospitalisations (17%).
Conclusion
Among multimorbid populations various ‘high need’ groups exist. Patients with high needs for general practice care can be identified by their previous use of general practice care. To identify frequent ED visitors and persons with unplanned hospitalisations, additional information is needed.
Introduction
KEY MESSAGES
-
A minority of patients with multimorbidity have high care needs.
-
This study shows that multimorbid patients’ general practice records can be used to identify future frequent users of general practice care.
-
These frequent users are mainly not the same people as those with emergency care visits or unplanned hospitalisations.
Recent studies estimated that the high prevalence of multimorbidity among western populations will increase further in the coming years [Citation1–6]. This puts pressure on health systems, as the group of patients with multimorbidity, i.e. with two or more chronic diseases, uses health care services relatively frequently [Citation7–11]. However, there seems to be a subgroup within the whole group of multimorbid patients that uses health services very frequently [Citation8].
Patients who frequently use health services may benefit from a person-centred care approach, as high service use may reflect an increased need for (professional) care and support [Citation12,Citation13]. In this approach, general practitioners proactively invite these patients to assess and discuss their care needs. Based on these needs, they develop an integrated care plan [Citation12] that overcomes care fragmentation [Citation10]. This could improve patients’ care experiences and possibly also their functioning and wellbeing [Citation14].
To initiate a person-centred integrated care process, general practitioners (GPs) might benefit from support to identify ‘high need’ patients among their multimorbid patient populations. GPs’ electronic medical records (EMRs) may be used to identify such patients [Citation15]. We, therefore, explored whether high care needs could be predicted from EMR data of general practice patients with multimorbidity.
Methods
Study sample
We selected patients aged ≥ 18 years from the Nivel Primary Care database (Nivel-PCD) who had contact with their general practice (office visit, telephone consultation or home visit) for at least two chronic diseases as listed by O’Halloran et al. over the period 2011–2012 [Citation16]. To reduce the risk that we would miss patients because they had not been in contact with their general practice for these diseases for quite a while (for instance, patients whose conditions are monitored in secondary care), we examined visits for two years (2011–2012) rather than one.
Data
Data were derived from Nivel-PCD [Citation17] and the Dutch administrative hospital information system (DIS). Nivel-PCD holds data that are routinely recorded in about 500 general practices (about 10% of all Dutch general practices), including the number and type of GP contacts and health conditions presented during these contacts [Citation17], coded using the International Classification of Primary Care (ICPC) [Citation17,Citation18]. DIS holds reimbursement claims of all Dutch hospitals, recorded as diagnosis related groups (DRGs).
Data from Nivel-PCD and DIS were linked by a Trusted Third Party using a deterministic linkage method, based on a unique identifier. Data were anonymised to secure privacy of patients [Citation19].
Outcome measures
We included three types of health service use to reflect high care needs as outcome measures of the study, which were all measured in 2013:
High number of general practice contacts
A high number of general practice contacts (i.e. office visits, telephone consultations or home visits) was defined as ≥12 contacts with the general practice in 2013. The choice for the cut-off ≥12 contacts was rather arbitrary, as we could rely on only one previous study [Citation8], where it was found to characterise a subgroup of multimorbidity patients identified as ‘high users’. Therefore, we performed sensitivity analyses with cut-off values of 10 and 14 contacts.
Emergency department visit(s)
Emergency department visit(s) were defined as ≥1 contact(s) with an emergency department (ED) of a hospital in 2013.
Unplanned hospitalisation(s)
Unplanned hospitalisation(s) were defined as ≥1 unplanned hospitalisations in 2013. A hospitalisation was assumed to be unplanned if the admission date was the start date of the DRG.
Predictors
We selected relevant predictors that can be automatically retrieved from patients’ EMRs:
Demographic and disease characteristics
As demographics we included age and sex of the patient. Age at January 1st 2013 was divided into 5 categories: 18–49 years, 50–64 years, 65–74 years, 75–84 years, and 85 or older. Included disease characteristics were the (number of) chronic diseases for which the patient contacted the practice, and psychological symptoms/diseases, operationalised as ≥1 code(s) from the P-chapter of the ICPC. All were measured in 2011–2012.
Use of general practice care
We included the total number of contacts with the general practice per year also as a predictor, but for this purpose based on data from 2012. Furthermore, we included the total number of different medications, prescribed on Anatomical Therapeutical Classification (ATC)-3 level, and whether any psychotropic drugs (ATC-class N05/N06) had been prescribed. These predictors were based on registration data from 2012, as especially health care use in the year before the outcome measurement seemed relevant.
Statistics
In the first step, we performed Chi2 tests with each predictor and outcome variable. We then performed multivariate probit regression analysis for each outcome variable, including all significant predictors (Chi2 p < 0.05). We calculated marginal effects for each level of a predictor. We assessed model specification using the link test for model specification [Citation20] and predictive value using the area under the curve (AUC) and pseudo R2. We did not adjust the P-value for multiple testing, as we aimed to find the best predictive model and not to test specific hypotheses.
Ethical statement
GPs participating in Nivel-PCD are contractually obliged to inform their patients: (1) about their participation in Nivel-PCD, and (2) about the option to opt-out if patients object to inclusion of their data in the database. According to Dutch legislation, and under certain conditions, neither obtaining informed consent nor approval by a medical ethics committee is obligatory for this kind of observational study. This study has been approved by the governance bodies of Nivel-PCD (NZR-00318.024).
Results
Sample characteristics
Nivel-PCD included data from 789,332 patients aged ≥18 years during 2011–2012. Of these patients, 245,065 (31%) were defined as having multimorbidity, and were therefore included. Their background characteristics and healthcare use are described in . Compared to the non-multimorbid patients, they were older, more often female, and had more prescribed medications and GP contacts (Supplementary Table 1).
Table 1. Demographics, health related characteristics and health service use of persons with multimorbidity in 2012 (n = 245.065).
High care needs
11% of the multimorbid patients had ≥12 contacts with their general practice in 2013 (). As compared to the entire group of multimorbid patients, these patients were more often female and aged 65 or older. They also had more chronic diseases, more prescribed medications and were more often prescribed psychotropic drugs ().
Table 2. Use of health services in persons with multimorbidity in 2013.
12% of the patients visited the ED in 2013 (). They had more chronic diseases and prescribed medications than the entire group of multimorbid patients ().
7% of the patients had ≥1 unplanned hospitalisation in 2013 (). These patients were older than the entire group of multimorbid patients and had more chronic diseases and prescribed medications ().
Overlap between high-need patient groups
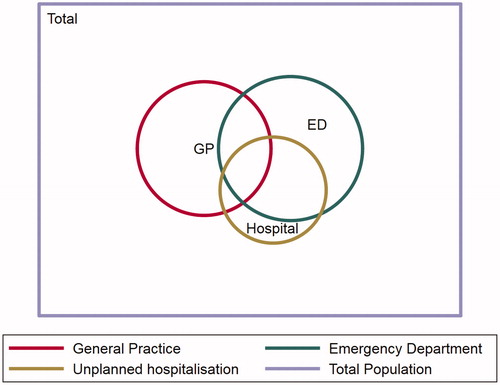
74% of the patients with unplanned hospitalisation(s) in 2013 also had ED visit(s) in the same year. The group of patients with frequent contact with the general practice appeared to be more distinct: only 29% of them had ED visit(s) and 17% had an unplanned hospitalisation(s) in the same year ().
Predicting high needs
High number of GP contacts
The strongest predictor was the number of contacts in the previous year (42% of those with ≥12 contacts in 2012 had ≥12 contacts in 2013). The next strongest predictor were three chronic diseases, stomach cancer, anaemia and heart failure; 33%, 33% and 28% of the patients with these diseases had ≥12 contacts, respectively. Furthermore, having 5 or more chronic diseases was a relatively strong predictor (22% had ≥12 contacts) (Supplementary Table 2(a)).
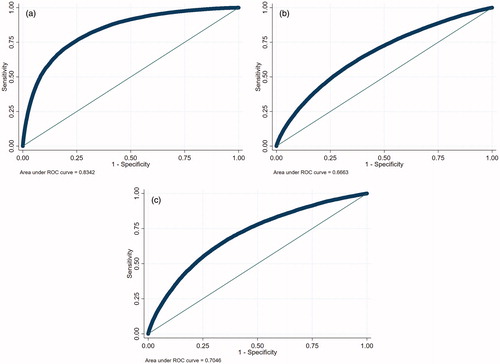
The multivariate probit model had an AUC of 0.83 (See ) and explained variance (R2) of 0.23. Model specification was adequate, as indicated by the non-significant linktest (p = .29). Only the number of GP contacts remained a strong predictor (Supplementary Table 2(a)). Using a predicted probability of 0.3 as a cut-off, the positive predictive value of the probit model was 44%, which is only slightly higher than the 42% using ≥12 contacts in the previous year as predictor. Sensitivity was 46% (Table 3(a)). Choosing a cut-off of 10 or 14 contacts did not lead to a better model (Supplementary Table 2(b,c)).
Emergency department visit(s)
The strongest predictor of having ≥1 ED visits in 2013 was having pancreatic, lung or haematologic cancer; 35%, 32% and 28% of these patients had an ED visit, respectively. Being 85 years or older and having ≥5 chronic diseases were the next strongest predictors (22% and 21% had ≥1 ED visits, respectively).
The multivariate probit model had an AUC of 0.66 (See ) and explained variance (r2) of 0.05. Model specification was inadequate (linktest hatsq p < 0.001). Results are shown in Supplementary Table 3). Using a predicted probability of 0.2 as a cut-off, the positive predictive value of the probit model was 27% and sensitivity was 26%.
Unplanned hospitalisation(s)
The strongest predictor of having ≥1 unplanned hospitalisations in 2013 was having pancreatic or lung cancer or heart failure (22%, 20% and 20% had an unplanned hospitalisation, respectively). Being 85 years or older was the next strongest predictors (15% had ≥1 unplanned hospitalisation).
The multivariate probit model had an AUC of 0.70 (See ) and explained variance (R2) of 0.07. Model specification was inadequate (linktest hatsq p < 0.001). Results are shown in Supplementary Table 4). Using a predicted probability of 0.15 as a cut-off, the positive predictive value of the probit model was 20% and sensitivity was 21%.
Discussion
Main findings
To support GPs in identifying multimorbid patients who may benefit from proactive person-centred integrated care, we analysed data from the general practice EMRs of almost 250,000 patients. The group of multimorbid patients with frequent general practice contacts appears to be distinct from the groups with ED visits or unplanned hospitalisations. The first group could be identified from the number of general practice contacts in the previous year, whereas the other two groups could not be identified reliably from data available in general practice EMRs.
Strengths and limitations
We included a large, well-defined and unselected sample of multimorbid patients. DIS holds claims data from all Dutch hospitals and demographic characteristics of patients in Nivel PCD are similar to the Dutch general population. Because both data sources are used for reimbursement with health insurance companies, they are likely complete. It is unlikely that we missed important chronic diseases, as we included morbidity registered for two years. Both databases could contain typos or incorrect coding, but it is unlikely that these were made selectively.
We may have missed some contacts related to diabetes, COPD or cardiovascular disease, as in the Netherlands management of these diseases within primary care is financed by bundled payment contracts, so they may not be registered separately in patients’ EMRs. In addition, we could not determine whether use of health services may have been (partially) avoidable. We wish to emphasise that with this study we solely aimed to help GPs identify multimorbid patients with high care needs, and not to make any inferences about underlying causes or interventions to meet these needs.
Another limitation is that the cut-off of ≥12 GP contacts was not based on previous literature. Sensitivity analyses, however, showed that results are similar when a cut-off of ≥10 or ≥14 is applied.
Interpretation in relation to existing literature
Predictors of high needs for general practice care
A previous cross-sectional study among multimorbid patients also found that women and older patients were more likely to have a high number of GP contacts [Citation8]. Chronic conditions were not a sigificant predictor [Citation8]. Another cross-sectional study among older patients found that women, those older than 85 and those prescribed a high number of medications were more likely to have frequent GP visits, whereas the Charlson Comorbidity Index did not predict frequent visits [Citation21]. These studies did not include prior healthcare use as a predictor.
Predictors of high needs for emergency and unplanned inpatient care
Predictors of ED visits and unplanned hospitalisations have not been studied previously among multimorbid patients, but a recent study in ED visitors with chronic diseases found that the number of previous ED visits was the most important predictor of future ED visits [Citation22]. A systematic review of risk prediction models for emergency hospital admissions among the general population reported that all models that had good model discrimination included indicators of prior healthcare utilisation, multimorbidity or polypharmacy, and named medical diagnoses or prescribed medications [Citation11]. Brief risk-prediction instruments for adverse healthcare outcomes among elderly frequently included medical comorbidities and age [Citation23].
Implications
To identify multimorbid patients with high general practice needs, their number of general practice contacts in the previous year is sufficient. GPs may be able to generate this information themselves or ask an IT specialist to develop software. GPs could then consider inviting these patients to explore and assess their needs and plan effective actions to improve patients' quality of life and health. As such, our results could also have important implications for patients with high care needs, who may benefit from such a proactive person-centred approach. Furthermore, it seems likely that such an approach is also beneficial for the health care system and society as a whole, as being able to manage high need patients more proactively may result in more efficient use of resources.
A second important finding of this study is that GPs have different groups of high-need patients among their multimorbid patient populations: the group who frequently contacts the general practice is largely distinctive from the group with ED visits of unplanned hospitalisations. To identify the latter two proactively, data from general practice EMRs alone seem insufficient. Additional patient-reported or hospital registration data may likely be needed [Citation24,Citation25]. Besides, care management of these groups may also be different from those with high general practice needs. This should be taken into account when designing and evaluating proactive integrated care interventions for multimorbid patients.
Conclusion
Multimorbid patients with high care needs can partly be identified from their EMR data. This holds in particular for patients who frequently contact the general practice. To identify patients with a high risk of using emergency care, additional data, either reported by patients or registered in hospitals, may be necessary.
Supplementary Tables 1-4
Download MS Word (67.9 KB)Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- van Oostrom SH , Gijsen R , Stirbu I , et al. Time trends in prevalence of chronic diseases and multimorbidity not only due to aging: data from general practices and health surveys. PLoS One. 2016;11(8):e0160264.
- Cassell A , Edwards D , Harshfield A , et al. The epidemiology of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2018;68(669):e245–e251. Apr
- Harrison C , Henderson J , Miller G , et al. The prevalence of diagnosed chronic conditions and multimorbidity in Australia: a method for estimating population prevalence from general practice patient encounter data. PLoS One. 2017;12(3):e0172935
- Weston C , Gilkes A , Durbaba S , et al. Long term condition morbidity in English general practice: a cross-sectional study using three composite morbidity measures. BMC Fam Pract. 2016;17(1):166 Nov 29
- King DE , Xiang J , Pilkerton CS. Multimorbidity trends in United States Adults, 1988–2014. J Am Board Fam Med. 2018;31(4):503–513.
- Violan C , Foguet-Boreu Q , Flores-Mateo G , et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9(7):e102149.
- McPhail SM. Multimorbidity in chronic disease: impact on health care resources and costs. Risk Manag Healthc Policy. 2016;9:143–156.
- Hopman P , Heins MJ , Korevaar JC , et al. Health care utilization of patients with multiple chronic diseases in the Netherlands: differences and underlying factors. Eur J Intern Med. 2016;35:44–50.
- Giannouchos TV , Kum HC , Foster MJ , et al. Characteristics and predictors of adult frequent emergency department users in the United States: a systematic literature review. J Eval Clin Pract. 2019;25(3):420–433.
- Huntley A , Lasserson D , Wye L , et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open. 2014;4(5):e004746.
- Wallace E , Stuart E , Vaughan N , et al. Risk prediction models to predict emergency hospital admission in community-dwelling adults: a systematic review. Med Care. 2014;52(8):751–765.
- Oliver DD. Oliver A manifesto for multimorbidity. Br Med J. 2018;360:k1044.
- Rijken M , van Kerkhof M , Dekker J , et al. Comorbidity of chronic diseases: effects of disease pairs on physical and mental functioning. Qual Life Res. 2005;14(1):45–55.
- Davy C , Bleasel J , Liu H , et al. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015;15:194
- Goldstein BA , Navar AM , Pencina MJ , et al. Opportunities and challenges in developing risk prediction models with electronic health records data: a systematic review. J Am Med Inform Assoc. 2017;24(1):198–208.
- O'Halloran J , Miller GC , Britt H. Defining chronic conditions for primary care with ICPC-2. Fam Pract. 2004;21(4):381–386.
- Nivel. Nivel Primary Care Database. [cited 2020 October 22]; https://nivel.nl/en/nivel-primary-care-database.
- Lamberts H, Wood M. ICPC. International classification of primary care. Oxford: Oxford University Press; 1987.
- Kuchinke W , Ohmann C , Verheij RA , et al. A standardised graphic method for describing data privacy frameworks in primary care research using a flexible zone model. Int J Med Inform. 2014;83(12):941–957.
- Pregibon D. Goodness of link tests for generalized linear models. J R Stat Soc Ser C Appl Stat. 1980;29(1):15–24.
- Hu T , Dattani ND , Cox KA , et al. Effect of comorbidities and medications on frequency of primary care visits among older patients. Can Fam Physician. 2017;63:45–50.
- Chiu YM , Vanasse A , Courteau J , et al. Persistent frequent emergency department users with chronic conditions: a population-based cohort study. PLoS One. 2020;15(2):e0229022.
- O'Caoimh R , Cornally N , Weathers E , et al. Risk prediction in the community: a systematic review of case-finding instruments that predict adverse healthcare outcomes in community-dwelling older adults. Maturitas. 2015;82(1):3–21.
- Jayanti A , Foden P , Wearden A , et al. Illness beliefs in end stage renal disease and associations with self-care modality choice. PLoS One. 2016;11(7):e0154299.
- Lowe R , Porter A , Snooks H , et al. The association between illness representation profiles and use of unscheduled urgent and emergency health care services. Br J Health Psychol. 2011;16(4):862–879.