Abstract
Hepatocellular carcinoma (HCC), the third leading cause of cancer-related death worldwide, is a disease of immune microenvironment. Chronic Hepatitis B virus (HBV) infection, also an immune-related disease, is the major etiological factor for HCC especially in Asia. As an immune regulator, which has pleiotropic activities on T cells, nature killer cells and dendritic cells and so on, the efficacy of thymalfasin on HCC patients has been proven by several pilot studies as an adjuvant therapy. Combination of thymalfasin significantly improved survival and prolonged the time to tumor recurrence in patients who received transcatheter arterial chemoembolization after tumor resection. An improvement in patients’ immunity has also been demonstrated. However, there is no large-scale randomized controlled study so far in resectable HCC patients. To confirm the role of thymalfasin adjuvant therapy in patients with HBV-related HCC after curative resection, a large-scale multicenter randomized controlled trial has been planned in China to investigate the effect of thymalfasin (1.6 mg twice a week for 12 months) on 2-year recurrence-free survival rate and tumor immune microenvironment. Here is the first announcement of the study protocol (ClinialTrials.gov Identifier: NCT02281266).
1. Introduction
1.1 Hepatocellular carcinoma and tumor immune microenvironment
Globally, hepatocellular carcinoma (HCC) is the sixth most common neoplasm and the third most frequent cause of cancer death Citation[1]. The prevalence of HCC is higher in Asia compare to Western countries with half of the disease burden being borne in China Citation[2].
Hepatitis B virus (HBV) and hepatitis C virus infection, alcohol liver disease, non-alcoholic fatty liver disease are the major etiological factors of HCC. In East Asia and Africa, > 80% of HCCs are attributed to HBV infection or exposure to aflatoxin. Globally, > 50% of HCC patients and almost all pediatrics patients are accompanied with active HBV infection Citation[3].
For patients without cirrhosis and in the very early stage of HCC, surgical resection is the treatment of choice. For patients with cirrhosis, resection still benefits the patients with small tumor, without portal hypertension and with normal total bilirubin level. But the 5-year recurrence rate after resection is as high as 70% because the underlying chronic liver disease continues to put the patient at risk of the development of new carcinoma Citation[2]. Because the higher numbers of young people have HBV-related HCC and milder cirrhosis stage, hepatectomy is much common in Asian countries compared to Western countries Citation[2]. Transarterial chemoembolization (TACE) is optimal choice for the intermediate-stage patients. For patients who have either failed TACE or who present with more advanced HCC, sorafenib is now considered the first-line treatment Citation[2].
Accumulating evidence has demonstrated that tumor microenvironment plays an important role in the development or progression of this lethal disease. It is now clear that the local immune system plays a dual role in HCC: it can not only suppress tumor formation and outgrowth but also promote tumor progression either by selecting for tumor cells more fit to survival in immunocompetent host or by establishing conditions within the tumor milieu that facilitate tumor outgrowth. The balance between antitumor and pro-tumor factors located in the tumor microenvironment is important for patient outcome – a balance toward pro-tumor factors indicated weak antitumor activities and poor outcome and vice versa. Multiple mechanisms underlining the tumor evasion from immune surveillance was demonstrated including loss of tumor antigen, by establishing an immunosuppressive state within the tumor microenvironment by recruiting suppressive cells regulatory T cells (Treg cells) and myeloid-derived suppressive cells; by secreting suppressive cytokines IL-10 and TGF-β; by expressing the negative costimulatory molecules CTLA-4, PD-1, PD-L1 and B7-H3 and by consuming IL-2, a cytokine that is essential for maintaining cytotoxic T-lymphocyte function Citation[4]. The immunotherapeutic strategy based on overcoming barriers within the microenvironment, briefly by enhancing antitumor power in combination with attenuating pro-tumor strength, was widely accepted. Until now, several immunotherapeutic studies demonstrated promising results in HCC. Moreover, immunotherapeutic treatment after hepatectomy may improve patient outcome by effectively killing residual cancer cells or tiny lesion of recurrence Citation[4].
1.2 Thymalfasin
Thymalfasin, often referred to in medical literature as thymosin-α1 or Tα1, is a peptide that has been evaluated for its immunomodulatory activities and related therapeutic potential in several conditions and diseases, including cancer (such as HCC, lung cancer and melanoma), infectious disease (sepsis, infections after bone marrow transplant, lung infections including chronic obstructive pulmonary disorder, severe acute respiratory syndrome, hepatitis B or C and HIV) and improvement in elderly immunocompromised patients (e.g., for enhancement of response to vaccines).
The basis for effectiveness in these conditions is its multiple effects on immunological responsiveness. Thymalfasin has a number of immunomodulating activities, resulting from activation of Toll-like receptor Citation[5] in dendritic and other immune system cells Citation[6,7] resulting in augmentation T helper 1 (Th1) function, natural killer (NK) cell activity and increased antibody response to T-cell-dependent antigens Citation[8].
Thymalfasin has also been shown to increase expression of proteins on the surface of virally infected or tumor cells, including those that mediate antigen presentation such as MHC class I, MHC class II and β-2 microglobulin Citation[9], as well as tumor-specific antigens Citation[10,11].
Importantly, thymalfasin acts without overstimulation of cytokine production and is generally well tolerated; it has an excellent safety profile and does not appear to induce the side effects and toxicities commonly associated with agents in this class such as IFN and IL-2, such as influenza-like symptoms or hematologic toxicities.
1.3 Rationale: the potential role of thymalfasin in HBV-related HCC
Based on the immunomodulating activity of thymalfasin, it is expected to be of benefit for use after hepatic resection, or in combination with either sorafenib or TACE, with no addition of toxicity.
A pilot study determined that the addition of thymalfasin to TACE led to a significant increase in survival (82 vs 41%; p < 0.05) and immune parameters (CD8 cytotoxic T cells and NK cells) Citation[12]. Another study demonstrated that the addition of thymalfasin provided a significant increase in survival compared to historical controls at 6, 9 and 12 months after TACE (91, 88 and 78% compared to 77, 58 and 46%, respectively; p < 0.05) Citation[13,14]. Cheng et al. evaluated the addition of thymalfasin to TACE after tumor resection or partial hepatectomy in a study of 57 subjects with HCC Citation[15,16]. The addition of thymalfasin significantly improved survival (10 vs 7 months; p = 0.002) and delayed the time to tumor recurrence (p = 0.039) in these subjects. Cheng et al. also evaluated the addition of thymalfasin plus lamivudine combination therapy after tumor resection or partial hepatectomy in a study of 81 subjects with HBV infection and HCC Citation[17-19]. In this study, the addition of thymalfasin/lamivudine combination treatment also resulted in statistically significant increases in time to tumor recurrence (10 vs 6.5 months; p = 0.0032) and median survival time (12.5 vs 6 months; p = 0.0023), as well as increases in HBV-DNA clearance (100 vs 4%; p = 0.0000) and HBeAg seroconversion (73 vs 7.5%; p < 0.05). The study by Gish et al. also showed an improvement in response to TACE with the addition of thymalfasin Citation[20]; in 25 unresectable HCC patients randomized to TACE with or without thymalfasin, the addition of thymalfasin led to an improvement in response (57 vs 46%; not significant) and an medial overall survival (OS) (110 vs 57 weeks; not significant).
For advanced HCC patients treated with sorafenib, Gu et al. found that thymalfasin combination therapy also improved the patients’ immunity (CD3+, CD4+, CD4+/CD8, CD16+/CD56+, etc.) and survival outcome (median time to progression from 2.8 to 3.8 months, OS from 6 to 6.6 months) Citation[21].
However, thymalfasin adjuvant therapy in resectable HCC patients has not been researched in a large-scale study. Hence, a multicenter, randomized, observation-controlled clinical trial has been planned in China, to evaluate the efficacy and safety of thymalfasin adjuvant therapy in patients with HBV-related HCC after curative resection.
2. Patients
It has been planned to include 360 patients with resectable HCC and currently HBsAg-positive and/or HBV-DNA positive from six teaching hospitals in China.
2.1 Inclusion criteria
Inclusion criteria during screening period (perioperative period) includes:
life expectance ≥ 3 months;
patients with hepatitis B history and currently HBsAg-positive and/or HBV-DNA positive;
patients who have undergo hepatic curative resection;
tumor feature a) with cancer embolus, b) a solitary nodule measuring between 3 and 8 cm or 2 nodules, a total combined measurement between 3 and 8 cm;
East Cooperative Oncology Group performance score of 0 – 2;
Child–Pugh score A; and
signed informed consent.
Inclusion criteria at baseline (4 weeks after surgery) includes:
no documented evidence of disease recurrence with computed tomography (CT) scan and CT angiography;
Child-Pugh score A; and
hematological test WBC > 3.5 × 109/l, RBC > 30%, PLT > 50,000/UL, NEU > 1.0 × 109/l, Cr < 1.5 mg/dl.
2.2 Exclusion criteria
Any anticancer therapy prior to the liver surgery procedure, including liver transplant, TACE, image-guided tumor ablation, radiotherapy, chemotherapy, molecular targeted therapy and immunotherapy and so on.
Patients taking the hepatotoxic drug or immunosuppressant drug.
Invasion of portal vascular and its first branch, hepatic duct and its first branch, inferior vena cava and hepatic vein.
Organ transplant recipient.
Extrahepatic organs and lymph node metastasis.
Prior treatment with immunomodulator (e.g., IFN, thymalfasin) or traditional Chinese medicine within 30 days prior to randomization.
Know postoperative complications (e.g., infection, bleeding, bile leak) at baseline.
3. Investigational product
About 1.6 mg thymalfasin (ZADAXIN®, SciClone) is planned to be given twice a week for 12 months subcutaneously.
4. Study design
The patients with HCC who are eligible for the inclusion/exclusion criteria will be randomly assigned to either the treatment arm (with thymalfasin adjuvant therapy) or the observational arm (without thymalfasin adjuvant therapy) at the radio of 1:1 at 4 weeks after curative resection ().
Figure 1. Illustration showing the study design. Subjects will be randomized into treatment arm (with 1.6 mg thymalfasin, twice a week, for 52 weeks) or observational arm at 4 weeks (± 7 days) after curative resection.
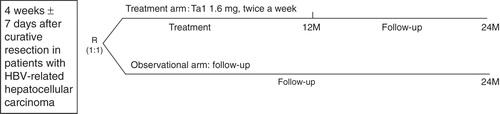
The patients in the treatment arm will be administered with thymalfasin for 12 months, followed by 12 months observation.
The patients in the observational arm will be followed up for 2 years periodically, without thymalfasin therapy.
HBV-DNA positive patients should be treated by antiviral agents. Entecavir is recommended.
The patients’ baseline HCC tissues and adjacent tissues will be collected in selected sites for immune microenvironment assay. If the patient experiences reoperation due to recurrence, resected tissues will also be collected.
5. Study end points
5.1 Efficacy end points
The primary end point of this study is recurrence-free survival (RFS) in the patients with thymalfasin adjuvant therapy versus the patients without thymalfasin adjuvant therapy after curative resection at 2-year.
The second end points include: 1-year and 2-year OS; 1-year RFS and mean recurrence time.
Immune microenvironment assay will explore T cells (CD3, CD4, CD8), Treg cell (FoxP3), Th17 cell (IL-17), NK cell (CD56), NEU (CD66b), Mφ (CD68), DC (CD1a, CD83) and MVD (CD31), and so on.
5.2 Safety objective
To assess the safety and tolerability of thymalfasin adjuvant therapy in patients with HBV-related HCC, adverse events, severe adverse events, laboratory values and vital signs and electrocardiogram; over time data will be collected.
6. Statistical analysis and sample size
RFS and OS will be summarized by treatment group using Kaplan–Meier methods. The primary test for differences in RFS between the two treatment arms will be based on a two-sided stratified log-rank test with a 0.05 significance level.
With the assumption of the 2-year RFS of 50% in the control arm and 65% in the treatment arm, the required sample size is 157 per arm with a two-sided 5% significance level and 80% power. Considering the dropout of 15%, 360 patients (180 patients per arm) will need to be enrolled.
7. Ethics approval
This study has been approved by the Ethic Committee of Zhongshan hospital, Fudan University (approval number B2014-052).
8. Trial registration information
This study has been registered in ClinicalTrials.gov. The Identifier is NCT02281266.
9. Expert opinion
HCC, the third leading cause of cancer-related death worldwide, is a disease of immune microenvironment. Chronic HBV infection, also an immune-related disease, is the major etiological factor for HCC especially in Asia. As an immune regulator, which has pleiotropic activities on T cells NK cell, dendritic cell and so on, the efficacy of thymalfasin on HCC patients has been proved by several pilot studies as an adjuvant therapy. Combination of thymalfasin significantly improved survival and prolonged the time to tumor recurrence in patients who received TACE after tumor resection. An improvement in patients’ immunity has also been showed. However, there is no large-scale randomized controlled study so far in resectable HCC patients. To confirm the role of thymalfasin adjuvant therapy in patients with HBV-related HCC after curative resection, a large-scale, multicenter, randomized controlled trial has been planned in China, to investigate the effect of thymalfasin (1.6 mg twice a week for 12 months) on 2-year RFS rate and tumor immune microenvironment. Here is the first announcement of the study protocol (ClinialTrials.gov Identifier: NCT02281266).
Acknowledgment
S-J Qiu and Z-G Zhou have equally contributed to this work.
Declaration of interest
This paper is part of a supplemental issue, sponsored by SciClone. The sponsor of this trial is Liver Cancer Institute, Zhongshan hospital and Fudan University. All authors made substantial contribution to the study design and protocol generation. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents, received or pending, or royalties.
Notes
Bibliography
- World Health Organization. International agency for research on cancer. GLOBOCAN. 2012. Available from: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx
- El-Serag HB. Hepatocellular Carcinoma. N Engl J Med 2011;365:1118-12
- Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012;379:1245-55
- Sawada Y, Ofuji K, Sakai M, et al. Immunotherapy for hepatocellular carcinoma: Current status and future perspectives[M]. INTECH Open Access Publisher, Rijeka,Croatia; 2013
- Romani L, Bistoni F, Gaziano R, et al. Thymosin alpha 1 activates dendritic cells for antifungal Th1 resistance through toll-like receptor signaling. Blood 2004;103(11):4232-9
- Romani L, Bistoni F, Perruccio K, et al. Thymosin alpha1 activates dendritic cell tryptophan catabolism and establishes a regulatory environment for balance of inflammation and tolerance. Blood 2006;108(7):2265-74
- Romani L, Bistoni F, Montagnoli C, et al. Thymsoin alpha 1: an endogenous regulator of inflammation, immunity, and tolerance. Ann N Y Acad Sci 2007;1112:326-38
- Romani L, Moretti S, Fallarino F, et al. Jack of all trades: thymosin alpha 1 and its pleiotropy. Ann N Y Acad Sci 2012;1269:1-6
- Giuliani C, Napolitano G, Mastino A, et al. Thymosin-alpha1 regulates MHC class I expression in FRTL-5 cells at transcriptional level. Eur J Immunol 2000;30(3):778-86
- SinibaldiVallebona P, Pierimarchi P, Moroni G, et al. Thymalfasin up-regulates tumor antigen expression in colorectal cancer cells. XXXth Meet Int Soc Oncodevel Biol Med 2002
- Garaci E, Pica F, Serafino A, et al. Thymosin alpha 1 and cancer: action on immune effector and tumor target cells. Ann N Y Acad Sci 2012;1269:11-18
- Stefanini GF, Foschi FG, Castelli E, et al. Alpha-1-thymosin and transcatheter arterial chemoembolization in hepatocellular carcinoma patients: a preliminary experience. Hepatogastroenterology 1998;45:209-15
- Zhang WJ. Transcatheter arterial chemotherapy and embolization plus thymosin alpha 1 for treatment of hepatocellular carcinoma. J Gastroenterol Hepatol 2004;15:A401
- Li ZS. HCC patients treated with TACE combined with thymalfasin: one year follow up. Paper presented at: Shanghai International Oncology Conference; 2001
- Cheng S, Wu M, Chen H, et al. Combination transcatheter hepatic arterial chemoembolization with thymosin alpha 1 on recurrence prevention of hepatocellular carcinoma. Hepatogastroenterology 2004;51:1445-7
- Cheng S, Wu M, Chen H, et al. Transcatheter hepatic arterial chemoembolization and thymosin in postoperative treatment of hepatocellular carcinoma. Chinese J Oncol 2004;26(5):305-7
- Cheng S, Wu M, Chen H, et al. Anti-viral therapy using lamivudine and thymosin is helpful to prevent recurrence in hepatocellular carcinoma with coexisting active hepatitis B. Chinese J Oncol 2005;27(2):114-16
- Cheng S, Ding G, Shi J, et al. Role of antivirus therapy in treatment of hepatocellular carcinoma with chronic hepatitis B infection. Chinese-Ger J Clin Oncol 2005;4(6):330-3
- Cheng S, Wu M, Chen H, et al. Antiviral therapy using lamivudine and thymosin alpha 1 for hepatocellular carcinoma coexisting with chronic hepatitis B infection. Hepatogastroenterology 2006;53:249-52
- Gish RG, Gordon SC, Nelson D, et al. A randomized controlled trial of thymalfasin plus transarterial chemoembolization for unresectable hepatocellular carcinoma. Hepatol Int 2009;3(3):480-9
- Gu X, Jiang Z, Yang M. Efficacy of sorafenib with thymosin α1 for patients with advanced hepatocellular carcinoma [J]. Jiangsu Med J 2010;21:004

