Figures & data
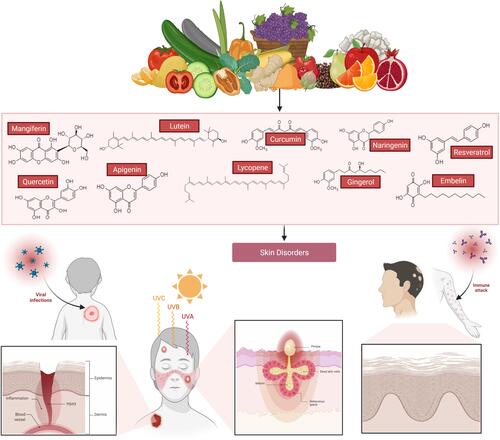
Figure 1 Skin anatomy in health. The skin structure is mainly divided into the epidermis, dermis, and subcutaneous/hypodermis. The epidermis is further divided into the stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale. The epidermis contains specialized cells, such as Langerhans cells (LCs), CD8+ T-cells, melanocytes, and others. Although skin appendages (hair, hair follicles, sweat glands, and sebaceous glands) are the main entry points for microorganisms, they are useful in transportation (from outside to inside and vice versa), prevention from mechanical damage, keeping skin dry, regulating temperature changes, protecting from ultraviolet light, and other. The dermis is the place where the majority of skin immunological interventions take place. The dermis is composed of fibroblasts, tissue-resident T-cells (TRM; including CD4+ T-cells [Th1, Th2, and Th17 cells] CD8+ T-cells, γδT cells, NKT cells), dendritic cells (including plasmacytoid DCs, tissue-resident DCs), tissue-resident macrophages, mast cells and others, and dense extracellular matrix (ECM). ECM is composed of collagen and elastin fibres, which occupies the extracellular space. The ECM provides a basement structure for the blood vessels, lymphatic vessel, and neurons through which transportation of immune cells and sensory functions are carried out, respectively. Beneath the dermis, a fatty layer which protects the host is the subcutaneous layer, also called subcutaneous adipose tissue. Along with the dermis, the subcutaneous layer also harbors a variety of immune cells, including T-cells, B-cells, macrophages, and others, and thus is collectively called the stromal vascular fraction (SVF). Despite immune cells function, adipocytes tissue secretes several bioactive proteins, collectively called adipokines (such as leptin, resistin, and adiponectin). These adipokines have various functions, including metabolic, inflammation, coagulation, vascular homeostasis, and others. Besides adipokines, adipocytes also secrete other molecules, such as IL-6, TGF-β, IGF-1, and others. Dermal DCs and LCs, which carry self/non-self-antigens (from PAMPs or DAMPs), migrate to lymph nodes and become antigen-presenting cells and present the antigens to the lymph node resident T-cells. The antigen-experienced T-cells differentiated into T-helper cells and migrate to the injured skin scite. Similarly, B-cells produce antibodies against self/non-self-antigens. The stratum corneum is the outermost layer (10–30 µm) in the skin, which is formed majorly from dead keratinocytes (also called denucleated keratinocytes; corneocytes), intracellular lipids (providing the hydrophobic nature to the skin), and others. The stratum lucidum is a very thin layer of dead cells in the skin after the stratum corneum that can appear as a translucent layer under a microscope. The stratum granulosumis composed of 3–5 layers of cells, which are composed of dark clumps of cytoplasmic granules. The stratum spinosum,also known as the prickle cell layer, originated from the keratinocytes that were differentiated and moved from the stratum basale. The stratum basale is a single layer of undifferentiated keratinocytes, which is the source of the stratum spinosum, and composed of melanocytes (Pigment melanin secreting cells). More information on skin anatomy can be found in excellent reviews.Citation3,Citation10,Citation11,Citation210 Created with BioRender.com.
![Figure 1 Skin anatomy in health. The skin structure is mainly divided into the epidermis, dermis, and subcutaneous/hypodermis. The epidermis is further divided into the stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale. The epidermis contains specialized cells, such as Langerhans cells (LCs), CD8+ T-cells, melanocytes, and others. Although skin appendages (hair, hair follicles, sweat glands, and sebaceous glands) are the main entry points for microorganisms, they are useful in transportation (from outside to inside and vice versa), prevention from mechanical damage, keeping skin dry, regulating temperature changes, protecting from ultraviolet light, and other. The dermis is the place where the majority of skin immunological interventions take place. The dermis is composed of fibroblasts, tissue-resident T-cells (TRM; including CD4+ T-cells [Th1, Th2, and Th17 cells] CD8+ T-cells, γδT cells, NKT cells), dendritic cells (including plasmacytoid DCs, tissue-resident DCs), tissue-resident macrophages, mast cells and others, and dense extracellular matrix (ECM). ECM is composed of collagen and elastin fibres, which occupies the extracellular space. The ECM provides a basement structure for the blood vessels, lymphatic vessel, and neurons through which transportation of immune cells and sensory functions are carried out, respectively. Beneath the dermis, a fatty layer which protects the host is the subcutaneous layer, also called subcutaneous adipose tissue. Along with the dermis, the subcutaneous layer also harbors a variety of immune cells, including T-cells, B-cells, macrophages, and others, and thus is collectively called the stromal vascular fraction (SVF). Despite immune cells function, adipocytes tissue secretes several bioactive proteins, collectively called adipokines (such as leptin, resistin, and adiponectin). These adipokines have various functions, including metabolic, inflammation, coagulation, vascular homeostasis, and others. Besides adipokines, adipocytes also secrete other molecules, such as IL-6, TGF-β, IGF-1, and others. Dermal DCs and LCs, which carry self/non-self-antigens (from PAMPs or DAMPs), migrate to lymph nodes and become antigen-presenting cells and present the antigens to the lymph node resident T-cells. The antigen-experienced T-cells differentiated into T-helper cells and migrate to the injured skin scite. Similarly, B-cells produce antibodies against self/non-self-antigens. The stratum corneum is the outermost layer (10–30 µm) in the skin, which is formed majorly from dead keratinocytes (also called denucleated keratinocytes; corneocytes), intracellular lipids (providing the hydrophobic nature to the skin), and others. The stratum lucidum is a very thin layer of dead cells in the skin after the stratum corneum that can appear as a translucent layer under a microscope. The stratum granulosumis composed of 3–5 layers of cells, which are composed of dark clumps of cytoplasmic granules. The stratum spinosum,also known as the prickle cell layer, originated from the keratinocytes that were differentiated and moved from the stratum basale. The stratum basale is a single layer of undifferentiated keratinocytes, which is the source of the stratum spinosum, and composed of melanocytes (Pigment melanin secreting cells). More information on skin anatomy can be found in excellent reviews.Citation3,Citation10,Citation11,Citation210 Created with BioRender.com.](/cms/asset/559442ea-73ce-4d6b-9b3a-da9279cca201/dddt_a_12298327_f0001_c.jpg)
Table 1 List of Skin Diseases or Disorders
Figure 2 Innate and acquired immune systems interactions in cutaneous bacterial infection. Disruption in the aforementioned barrier leads directly to occasional infections. In reaction to bacteria infringing the epithelial barrier, keratinocytes will produce chemokines, antimicrobial peptides, and cytokine,s which leads to an increase in leukocyte extravasation stimulating the migration into the skin and guiding these cells via chemotactic gradients. Dendritic cells convey bacterial antigens to naïve and central T-cells, contributing to pathogen-specific cells being activated producing CD4 and CD8 T-cells which increased targeting of innate responses. Created with BioRender.com.
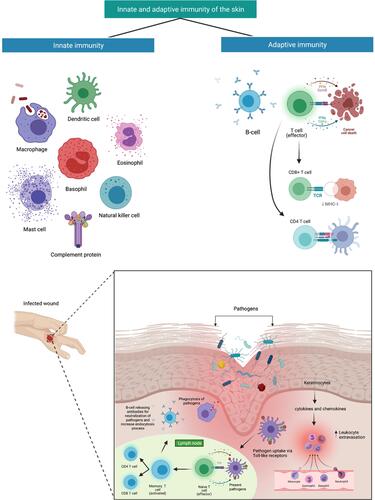
Figure 3 Chemical structure and source of natural products reported against skin disorders. Created with BioRender.com.
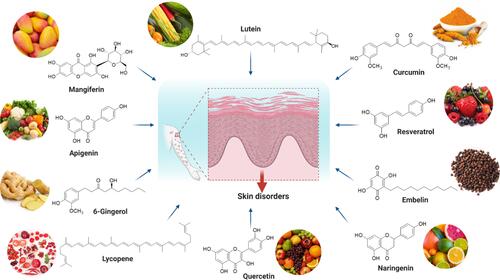
Figure 4 Effect of mangiferin against skin disorders and its mechanism of action. Mangiferin possessed a wide spectrum of pharmacological and biological properties, including antioxidant, chemoprotective, and anti-inflammatory properties. Besides, it can also inhibit elastase and collagenase can also help to preserve the skin and prevent wrinkles. Mangiferin has the ability to suppress CD68 activity, a key macrophage biomarker linked to dermatitis. Created with BioRender.com.
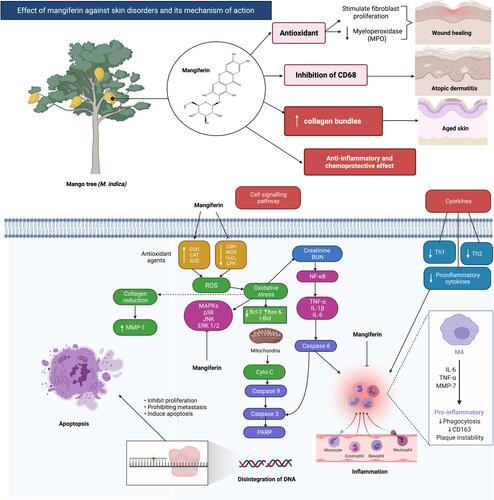
Table 2 Overall Mechanism of Action for Natural Products Against Skin Disorders
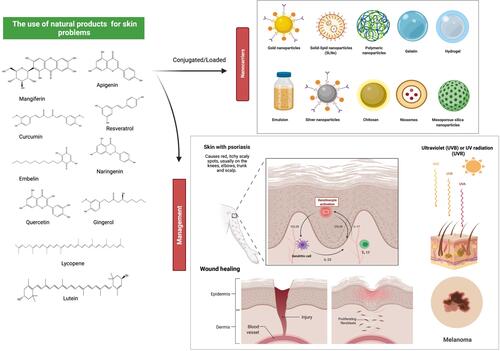
Figure 5 Overview of the mechanisms of action of natural products reported to treat/management of skin disorders. Mangiferin, lutein, curcumin, resveratrol, embelin, naringenin, quercetin, lycopene, gingerol, and apigenin are natural products that are commonly used in the treatment of various skin disorders. Through various pathways, these natural products can aid in wound healing, protect against tumor development due to oxidative damage, prevent further progression of wrinkles from prolonged UV exposure, and reduce atopic dermatitis skin lesion growth. Created with BioRender.com.
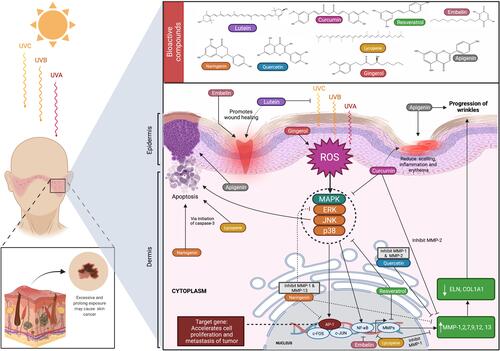
Figure 6 Targets of inflammatory skin diseases. Inflammation is an innate response of the body’s initial response against any insults (damage or infection). The hyperimmune response is the seeding point for several inflammatory skin diseases, including autoimmune diseases. The loss of self-tolerance in the skin sequentially develop as autoimmune diseases. Therefore, targeting excess inflammation would serve as a best strategy to restore the skin homeostasis. Several established targets in inflammatory diseases, such as innate immune system, co-stimulation, downstream pathways, adaptive immune system (including T- and B-cells), and others. Created with BioRender.com.
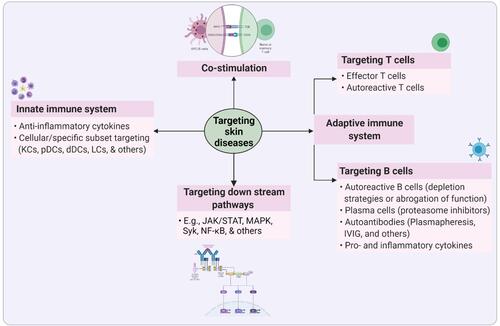
Table 3 Computed Physicochemical Properties of Natural Products Reported Against Skin Disorders
Figure 7 Effects of natural products on numerous skin conditions and possible drug delivery system. Nanocarriers are currently being used as a vehicle to deliver natural products to specific targeted regions in a regulated manner, as well as to overcome some of the drawbacks pertaining to the free compounds, such as poor bioavailability and rapid degradation. Natural products, along with innovative delivery systems, are a very promising area for future drug discovery against skin problems. For example, naringenin is a good candidate as an anti-psoriatic treatment as it inhibits over-expression of interleukin and ameliorated psoriasis and reduces transepidermal water loss. Resveratrol has protection against the main factor affecting non-melanoma skin cancer, which is UVB exposure by reducing COX-2 levels. Some other bioactive substances also exhibited a similar mode of action against various skin conditions including wound healing. Created with BioRender.com.