Abstract
In a state ravaged by suicide and a mental health crisis, this study sought to mitigate impacts of adverse childhood experiences (ACEs) and depressive and anxiety symptomology in high school students in a rural Montana community. Through a seven-week, twice weekly intervention of trauma-informed yoga, participants experienced statistically significant reductions in anxiety (GAD-7) and increases in Strengths and Difficulties (SDQ-11) overall scores and some subscales; noteworthy improvements were also present in depressive symptomatology (PHQ-A), salivary cortisol levels, and sleep duration. Importantly, participant qualitative feedback indicated significant benefits in focus, relaxation, and overall well-being. Further research is needed to imply generalizability and should include a larger, more diverse sample as well as utilization of control groups and an examination of academic and behavioral impacts at the school level.
A child’s mental health is just as important as their physical health and deserves the same quality of support. No one would feel embarrassed about seeking help for their child if they broke their arm—and we really should be equally ready to support a child coping with emotional difficulties. —Kate Middleton
Introduction
It is imperative that schools create time to ensure the safety, health, and well-being of students (Noddings, Citation2005). However, current legislation forces public school teachers and administrators to focus their energies on students meeting standardized measures of academic progress and proficiency against state and national standards for accountability purposes. To ensure adequate instructional time for tested subjects like mathematics and reading, enrichment activities like music and art classes, and often even recess, are cut from the schedule (Walker, Citation2014). In the hyper-scheduled and over-tested lives of our K-12 students and teachers, an emphasis on educating the whole child is often left wanting.
The purpose of this project was to find a purposeful and efficient way to integrate student well-being and mental health practices in a rural school district in Montana without detracting from instructional time. Through the lens of community-based participatory research, the research team developed a meaningful and productive relationship with the school district and key community members. This ensured the success and longevity of an intervention designed to target students with histories of traumatic exposure in a community deeply impacted by stigmatization of mental health care, substance abuse, and the suicide epidemic.
Project significance
This research aimed to improve chronic stress-related behavioral and mental health outcomes for adolescents in rural Montana through the application of a school-based intervention: trauma-informed yoga. Given the prevalence of suicide and mental health issues in rural Montana (Montana Department of Public Health & Human Services, Citation2018), this project was designed to help mitigate the impact of contributing factors (i.e., stress and trauma) by providing coping strategies (such as breathing, meditation, and mindfulness) through yoga for adolescents. These coping strategies are intended to improve overall mental health and behavioral outcomes, which may ultimately lead to reduced suicide rates. This study sought to evaluate the implementation of an innovative intervention that will ultimately promote positive development in school-aged children concurrently with providing rural access to novel interventions.
Context: The rural mental health crisis
Montana is a state in a true mental health crisis. It has consistently ranked in the top five states with highest suicide rates in the nation, based on recent reports from the Centers for Disease Control and Prevention (CDC, Citation2020). Nearly a fifth, or 19.5% of Montana adults, report being diagnosed with depression, compared to 17.4% of all U.S. adults (Substance Abuse & Mental Health Services Administration, Citation2015). Based on the 2015 and 2016 National Survey on Drug Use and Health (NSDUH) estimates, nearly 8% of Montana adults suffer from major depressive episodes, compared to 6.7% of all U.S. adults (Substance Abuse & Mental Health Services Administration, Citation2017). Depression and mental illness are not only present in adults in Montana, but these issues also impact youth as well.
A longitudinal study from 2010 to 2014 indicated that 39.1% of Montana adolescents aged 12–17 sought treatment for a major depressive episode at some point during the study (Montana Adolescent Substance Abuse Facts, Citation2015; Montana Department of Health & Human Services, Citation2016). Higher than national average prevalence of mental illness likely contributes to Montana’s suicide rate that is nearly double that of the U.S. (American Foundation for Suicide Prevention, Citation2017). For example, the rate of youth suicides (ages 11–17) in Montana is more than double the rate of youth suicides nationally, and 74% of those suicides presented with warning signs. Factors, including scarcity of treatment resources, long distances to existing care, and stigma of mental illness and its care, are also likely contributors to these higher suicide rates (Kaiser Family Foundation, Citation2016). Importantly, in the county in which this project took place, the 2019 Youth Risk Behavior Survey indicated that 39% of high schoolers experienced severe depression symptoms, 20% made a concrete suicide plan, and 16% attempted suicide (Montana Office of Public Instruction, Citation2019). Because of these alarming statistics, this project sought to directly address several factors of youth mental health through the promotion of healthy stress management and targeted improvement of indicators of depression and anxiety using trauma-informed yoga. Understanding how rurality is a key factor in this project further informed the study’s approaches.
Rural mental health care access disparities
Rural America has unique challenges in accessing quality mental health care. Many barriers exist, including a lack of mental health care providers, geographic isolation leading to inability to access providers, cost, stigma around mental illness, and even weather (many Montanans are unable to travel any considerable distance for the majority of the year due to deep snowpack and lack of highway snow plowing to healthcare provider locations) (Kaiser Family Foundation, Citation2016). To illustrate the rural nature of the state, 44% of Montana’s population is classified as rural or frontier, meaning they are some of the smallest and most geographically isolated areas in America (National Center for Frontier Communities, Citation2018; National Network of Libraries of Medicine, Citation2020). Therefore, innovative mental health delivery methods are desperately needed for not only rural Montanans, but other geographically isolated areas in our nation. Specifically, intervening with adolescents in the school setting is indicated in the context of rurality and limited mental health care access, particularly for children that have been exposed to adverse experiences.
Adverse childhood experiences
The linchpin around which this study revolves are adverse childhood experiences. In a seminal study involving 17,000 participants, Felitti and his team (Citation1998) discovered a strong correlation between negative adult health outcomes and adverse childhood experiences (ACEs), such as physical and emotional abuse, neglect, and/or household dysfunction (Felitti et al., Citation1998). Of its study participants, 64% had at least one ACE, and as the number of ACEs one experienced increased, so did their negative health outcomes (Felitti et al., Citation1998). This study prompted the genesis of many others involving ACEs and their impacts on both children’s and adults’ mental and physical health, as well as behavioral and academic outcomes. For example, a study by Carrey, Butter, Persinger, and Bialik (Citation1995) found that abused children, when compared with a reference group, scored lower on verbal and full-scale IQ batteries. Furthermore, these scores were inversely related to the severity of the abuse they had suffered and supports the hypothesis that abuse, and therefore certain types of trauma, can inhibit cognitive function (Carrey et al., Citation1995). Adverse childhood experiences not only impact an individual’s mental and physical health, but it significantly impairs cognitive function, leading to an increased academic achievement gap between traumatized youth and those who have not suffered trauma. Therefore, it is imperative to address these issues at the school level to support children academically, socially, and emotionally and mitigate the issues of childhood adversity.
Rural ACEs
Rurality presents a unique challenge to those who experience ACEs. While adverse experiences can happen anywhere geographically, fewer resources and social supports are available in geographically isolated areas. Further, poverty and low educational attainment also tend to be concentrated in rural locations, placing children in more vulnerable situations without needed resources (Lukens, Citation2017). The 2011–2012 National Survey of Children’s Health found that rural children were more likely to experience ACEs than urban children due to the likelihood of an impoverished lifestyle and lack of public resources (Lukens, Citation2017; U.S. Department of Health & Human Services, Citation2015). Additionally, in a recent study, Talbot, Szlosek, and Ziller (Citation2016) found that while the prevalence of ACEs was comparable in rural and urban adults, roughly a quarter of rural adults had a high ACE score (4+ ACEs).
In the Montanan county in which this study took place, the 2019 Community Health Survey indicated a widespread prevalence of high ACE scores (a score of 4 or greater): 23.8% of men and 19.9% of women reported high ACE scores, and 38.2% of those respondents were in the 18–39 year age range (J. Wilcox, personal communication, September 30, 2019). Of these survey responses, the most commonly occurring ACE in this county reported was emotional abuse (42.2%); the next most-often occurring ACEs were tightly clustered and included household substance abuse (28.4%), parental separation or divorce (26.8%), household mental illness (24.7%) and physical abuse (22.8%) (J. Wilcox, personal communication, September 30, 2019). Given that nearly half of respondents suffered from emotional abuse and nearly a quarter suffered from other forms of abuse, it is abundantly clear that this population is in dire need of efforts to mitigate childhood ACEs during adolescence. Purposefully integrating mental health interventions in the public school setting in rural areas offers an accessible opportunity to address ACEs, especially when access to mental health care agencies is less available in frontier areas (Kaiser Family Foundation, Citation2016).
Partnership processes: Community-based participatory research
To increase access to mental health care and mitigate high school students’ issues surrounding adverse childhood experiences (or other less severe challenges to their mental health and equilibrium), the principal investigator developed a partnership with a school system and a local yoga studio within a rural Montana community using a community-based participatory approach. Israel, Schulz, Parker, and Becker (Citation2001) define community-based participatory research (CBPR) as “focusing on social, structural, and physical environmental inequities through active involvement of community members, organizational representatives, and researchers in all aspects of the research process” (p. 182). Instead of implementing the project from a researcher-centered approach, a CBPR approach was utilized to purposefully situate the community stakeholders at the center of the study. This method provides an opportunity for stakeholders to contribute to their own purposes, questions, and aims for the study instead of the researcher implementing their personal research agenda upon the community. As opposed to traditional research approaches, CBPR is founded upon shared ownership of the research process and products along with shared decision making (Faridi, Grunbaum, Gray, Franks, & Simoes, Citation2007). In summary, CBPR “recognizes the importance of involving members of a study population as active and equal participants, in all phases of the research project, if the research process is to be a means of facilitating change” (Holkup, Tripp-Reimer, Salois, & Weinert, Citation2004, para. 3). This change occurs when stakeholders contribute “their expertise to enhance understanding of a given phenomenon and integrate the knowledge gained with action to benefit the community involved” (Israel et al., Citation2003, p. 1).
After forging initial relationships with the school district and community partners, to continue to grow trust and the relationship with the school district, the principal investigator (PI) facilitated additional community relationships that support the school district. The principal investigator joined the local community wellness/resilience committee that focuses on suicide prevention and de-stigmatization of mental health care; this participation led to the PI receiving an invitation to join the school district’s suicide, intervention, and response to treatment committee. From these committees, a community advisory board (CAB) was formed from various members of the school district (co-principals, district level administrator, physical education teacher, and school nurse) and community agencies (the county’s health department director and community health coordinator from the local hospital). Community advisory boards are often lauded as a positive, formalized mechanism for ensuring equitable community representation in research studies (Newman et al., Citation2011).
A participant observation framework was used by the PI throughout the intervention for the purpose of engaging with all participants and instructors. This process included active participation in each session of yoga. This framework was based on Hammer et al. (Citation2017) who stated “Participant observation can provide depth and context to observations and help minimize mistaken assumptions routinely made based on observations from a distance” (p. 441). Although participant observation is more often used in cultural and anthropological research contexts (Fletcher et al., Citation2013), it is also gaining momentum as an accepted approach for community-based participatory research. The framework is beneficial in providing a lens through which wide-ranging sociocultural factors in community-identified issues can be explored more broadly (Horowitz, Robinson, & Seifer, Citation2009). These strong CPBR structures supported and ultimately led to a grant from the National Institutes of Health (NIH), which funded this study (NIH award no. P20GM104417).
Given the current challenges due to COVID-19, it is important to note that according to Saul (Citation2013) collective trauma has a way of forging strong bonds between those who experience it. While the coronavirus crisis is still ongoing at the time of this manuscript’s creation, it began in the midst of the intervention period. Despite the difficulties this pandemic created, the sense of community and support between the PI and CAB has noticeably strengthened.
Intervention design: Trauma-informed yoga
Bessel van der Kolk (Citation2014) asserts that chronically traumatized individuals hold trauma within their physical bodies, which may take the form of migraines, muscle spasms, or fibromyalgia. While medication can be prescribed for these various ailments, researchers posit that movement and somatic experiencing (a focus on using the body to heal trauma) may work to mitigate the impacts of trauma in the body without medication (Levine, Citation1997; van der Kolk, Citation2014). Further complicating the physical ailments related to trauma is alexithymia, which, according to van der Kolk (Citation2014), is “the technical term for not being able to identify what is going on inside oneself” (p. 274). A cultivation of a yoga practice is one way to reconnect with one’s physical and emotional sensations to foster a sense of self-awareness and emotional regulation which also assist with processing complex trauma; this awareness leads to improved interoception, or discovering the body’s internal rhythms while simultaneously benefiting one’s proprioception, or awareness of connection to one’s self, others, and their environment (Malchiodi & Perry, Citation2020). One study showed that a 20-week yoga intervention for chronically traumatized adult women increased activity in the insula and medial prefrontal cortex areas of the brain, both of which are responsible for self-regulation (van der Kolk, Citation2014). Moreover, yoga has shown to improve heart rate variability in traumatized individuals, which is used as an indicator for the health of the autonomic nervous system (van der Kolk, Citation2014). When an individual has been traumatized, the autonomic nervous system creates “arousal in both body and brain” and leads to poor heart rate variability, indicating a negative stress response in the individual (van der Kolk, Citation2014, p. 269).
Although limited research exists on children and yoga, recent studies suggest that yoga and mindfulness can greatly benefit all students, especially for those that have suffered traumatizing experiences (Cook-Cottone, Talebkhah et al., Citation2017; Emerson & Hopper, Citation2011; Spinazzola, Rhodes, Emerson, Earle, & Monroe, Citation2011; van der Kolk, Citation2014). These studies have drawn positive relationships between physical yoga practices and academic gains along with a decrease in cortisol levels. Middle school students also have improvements in stress, sleep, and academic performance after participating in yoga (Butzer, van Over, Noggle Taylor, & Khalsa, Citation2015; Khalsa, Hickey-Schultz, Cohen, Steiner, & Cope, Citation2012). Other studies on yoga have reported positive mental health outcomes in measures of resilience, anger, anxiety, stress, depression and fatigue as well as physical health improvements such as flexibility, strength, and weight loss (Khalsa et al., Citation2012). Additionally, yoga has also been linked to improvements in test anxiety, work habits, academic performance, emotional intelligence, and cooperation (Butzer et al., Citation2015; Khalsa et al., Citation2012).
Burke-Harris (Citation2018) reveals one of the keys to reversing the physiological and psychological impacts of childhood adversity is exercise along with relaxation techniques like meditation. Providing a trauma-informed yoga-based practice can help students create a space where they “feel safe enough for learning to occur” (Cook-Cottone et al., Citation2017, p. 218). Further, exercise causes the release of a protein called brain-derived neurotrophic factor, which is paramount for learning and memory in the brain hippocampus and prefrontal cortex (Ratey, Citation2008). Yoga has been shown to increase GABA levels in the brain, which are lower in survivors of post-traumatic stress disorder (Ratey, Citation2008). Spinazzola cites Hölzel et al. (Citation2011) in asserting that “mindful meditation has also been shown to increase brain gray matter concentration, which is involved in learning, memory, emotion regulation, self-referential processing, and perspective taking” (p. 433). As noted by the research above, yoga as a form of physical exercise has the capability to improve learning and academic outcomes for youth.
Traditionally, trauma-informed yoga follows a “hatha” style practice, which can be used as an umbrella term for yoga practiced in Western cultures. Hatha yoga is comprised of “asanas” (static poses), “pranayama” (breathing practice), and “vinyasa” (dynamic sequences of asanas/poses). Given that the participants in the current study were in a regularly scheduled strength training physical education class, we wanted to challenge them with a “power vinyasa” practice. Power vinyasa is a strength-focused practice that links movement to deep, measured breathing by combining sequences of poses with long holds and balance work (Buscko & Rychlik, Citation2006, p. 168).
Trauma-informed yoga is distinctive from a traditional yoga practice in a variety of ways. Most importantly, the yoga instructor must be very knowledgeable regarding both the physiological and psychological impacts of trauma for those who are participating in each session. The knowledge will then guide the instructor in relation to intentional, trauma-informed choices which could positively or negatively impact participants. For example, certain props such as a strap, could create a trigger for those who may relate a strap to some form of past restraint. The instructor should also be aware of poses that could inadvertently serve as trigger either due to the naming/instructions provided for the pose or the actual physical position. An example would be language including “binding hands behind one’s back or performing ‘corpse pose.’” The actual physical positions include any that could be interpreted as sexually suggestive (such as downward dog, straddle splits, etc.) (Emerson & Hooper, Citation2011). Additionally, a trauma-informed yoga instructor must be constantly aware of these potential triggers and support participants in teaching them to listen to their body. Finally, a trauma-informed yoga instructor should also focus on enhancing participant knowledge to help them understand how yoga can support healing a dysregulated stress response/nervous system (Cook-Cottone et al., Citation2017; Emerson & Hopper, Citation2011).
Through slow, controlled movements that are paired with breath, this “yogic breathing” (or deep, diaphragmatic breath) forces participants to focus on their breathing and poses as a moving meditation and work together to address the embodied, physical effects of trauma; a plethora of research exists to support that practicing yoga and this intentional breath work is beneficial to emotion regulation, decreased rumination, stress management, and quality of life while concurrently treating traumatic stress disorders, insomnia, anxiety, and depression (Salmon, Lush, Jablonski, & Sephton, Citation2009). Additionally, the rhythmic and repetitive motions that a trauma-informed yoga practice involves are shown to help regulate a dysregulated stress response, bringing practitioners into the present moment. They are designed to “restore and entrain the rhythmicity of biological functions that are often disrupted during periods of stress” (Salmon et al., Citation2009, p. 62). The empirical evidence thus far supports the use of yoga toward improving mental and physical health outcomes for traumatized youth; therefore, these evidence-based benefits following a yoga session suggest that trauma-informed yoga could be an important complementary treatment for children with a history of ACEs to support overall well-being and academic success (Salmon et al., Citation2009).
Intervention framework
Consistent with established yoga interventions for mental and physical health outcomes for adolescents, the program used the framework designed by the “Yogis in Service Trauma-Informed Yoga” (YIS-TIY) approach () (Cook-Cottone et al., Citation2017). During course sessions, a certified yoga instructor led mindfulness/yoga practice sessions that highlight deep breathing, mindful movement, and cultivation of emotional regulation and stress relief. Each session began with goal or intention-setting for each individual, a brief time for reflection prior to the practice, intentional breathing followed by the physical practice, and ended with a meditative reflection intended to calm the central nervous system. Each student was also asked to write a journal reflection at the conclusion of each session to record changes in mood, thought patterns, or physical sensations. At the end of the 8-week intervention period, students were also asked to respond to an open-ended survey to share whether/how they found the mindfulness/yoga practice helpful in regulating emotions, behaviors, thoughts, and/or perceived academic outcomes.
Table 1. Conceptual framework for trauma-informed yoga intervention (Cook-Cottone, Talebkhah, et al., Citation2017).
Research aims
As a pilot study, this research held two primary objectives:
Aim 1: Foster a partnership with a rural Montana school district and test the feasibility of implementing a trauma-informed yoga intervention.
Aim 2: Collect preliminary data for the intervention (surveys, journal entries, and cortisol levels) to assess how the intervention related to changes in youth mental and physical health (e.g., behavioral, social, emotional, and physical functioning).
For this pilot study, feedback was gathered from the school district, teachers, and students from the focus group via conversations and email communications to determine the level of burden from the various assessment instruments and participation in the pilot. Retention and satisfaction of participants, as measured by survey instrumentation and participation rates from year one indicated the feasibility of an ongoing partnership with the school district. Because this pilot was a feasibility study, no control group was utilized, and the focus of the project was to examine pre and post survey results and cortisol levels.
Methods
Innovative methodology
This research relied upon a novel, rarely implemented intervention of a trauma-informed yoga intervention in the public school setting to promote positive youth development. Traditionally, trauma-informed practices in school settings involve educationally-focused interventions, like Social Emotional Learning curricula or referral to special education programs (Burke-Harris, Citation2018; Collaborative for Academic, Social and Emotional Learning, Citation2020). The authors of this manuscript posit that intervening with adolescent mental and physical health must be a multidisciplinary approach, and that root causes of health issues stemming from outside the educational environment cannot be addressed solely through educational interventions. Additionally, this study engaged collaborative partnerships with a rural Montana school district, community businesses (yoga studios), and public health organizations for this study’s promotion and recruitment. Given that district and school administration have requested the PI’s continued assistance with program evaluation, data analysis, and further implementation and expansion of this study, this project supports the collaborative approach of CBPR and community-identified needs.
In the winter of 2020, this pilot study was implemented in a rural high school in Montana. Although designed to be eight weeks, this intervention was forced to be truncated at seven weeks due to the global coronavirus pandemic and mandatory school closures. In this seven-week intervention, 18 high school participants completed a 45-minute trauma-informed yoga session with a certified yoga instructor twice a week during their regularly scheduled physical education class. Students completed pre-surveys that indicated adverse childhood experience scores, anxiety scores, depressive symptomatology scores, and strengths and difficulties scores. Teachers and parents also completed pre-surveys regarding the participants’ strengths and difficulties as well; however, the survey response rates were very low with both teachers and parents, thus invalidating results. Salivary cortisol was collected pre- (during week 1, prior to the initial session) and mid-intervention (at week 4) to determine if participants’ stress levels were impacted by the intervention; post-intervention cortisol was unable to be collected in week 8 due to school closures from the coronavirus crisis.
Qualitative data were collected through reflective journals that participants were asked to utilize after each session, and students were given the latitude to write whatever they desired after their final pose. Additional qualitative data were gathered by the graduate assistant from observations for each intervention session, and a final survey was given to participants that allowed for open response feedback on elements of the study they liked or disliked.
After students volunteered for program participation, to establish a baseline for participants, students were given the ACE screening instrument and pre-surveys (outlined below) and then began the eight-week intervention. Because of this unexpected closure, students completed post surveys online during week 8 while they were sheltered in place at home. Participants were offered a $25 gift card incentive to complete their surveys, and the physical education teacher also made it a requirement of their class. As a result, 16 out of 19 of the participants completed all post-survey measures.
Salivary cortisol samples were deidentified (using a code key system) before analysis by the Center for American Indian and Rural Health Equity Translational Biomarkers Core Lab at MSU. Testing utilized the Abcam (ab154996) cortisol in vitro competitive ELISA (Enzyme-Linked Immunosorbent Assay) kit designed for the accurate quantitative measurement of cortisol in saliva (sensitivity 0.12 ng/mL). Comparisons using paired t-tests between pre and post-surveys were utilized to determine changes in cortisol and sleep duration following the intervention, and any changes in cortisol levels and sleep duration pre and mid-intervention were analyzed to assess any trends in stress reduction and improved rest. outlines the various validated measures utilized in this study to assess participant outcomes.
Table 2. Assessment measures.
Sample
Eighteen students at a small, rural high school in Montana volunteered to participate in this study. The analytical sample includes 16 students who completed both the pre and post measures; one student opted not to participate in the study, and another moved during the study period. Students who opted out of the study were still required to participate in the yoga exercises, per the physical education teacher’s instructions, but did not provide data for the study. Students who did not self-select this physical education class in their schedule were excluded from the study. The majority of participants identified as white (n = 14) and male (n = 14 males); as this was a strength training class, students self-select this elective, explaining the prevalence of male participants. The majority of students (89%) attended at least 10 sessions and four students attended every session. Among our sample, 21% of our participants had a moderate ACE score (an ACE score of 2–3), while 50% had a high ACE score (of 4 or more ACEs). Descriptive statistics for the full sample on the outcome measures are provided in .
Table 3. Descriptive statistics of sample (n = 16), pre-yoga intervention (T1).
Measures
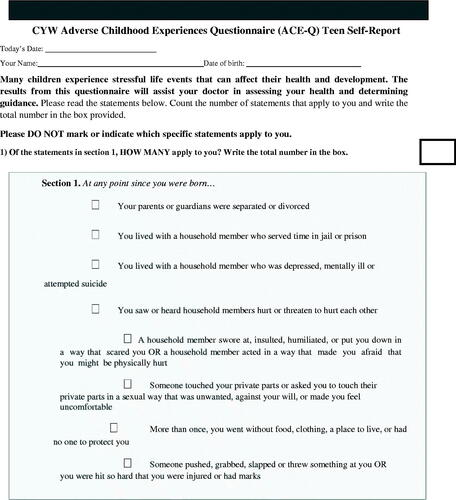
Adverse childhood experiences
The Center for Youth Wellness ACE-Q Teen self-report is a 19-item survey that is broken into two subscales; the first subscale measures traditional adverse childhood experiences (on a scale of 0–10) while the second quantifies events that are hypothesized to be correlated to a dysregulated stress response on a scale of 0–9 (i.e., toxic stress caused by discrimination, bullying, unsafe housing, etc.) (Bucci et al., Citation2015). For the purposes of this study, only the first subscale for adverse childhood experiences was utilized in calculating ACE scores. ACE scores ranged 0–10, with a mean of 3.78 and a standard deviation of 2.9. Thirty-seven percent of students were categorized as having a low ACE score (a score of 0–1), 21% had a moderate ACE score (a score of 2–3), and 42% were categorized as having a high ACE score (a score of 4–10).
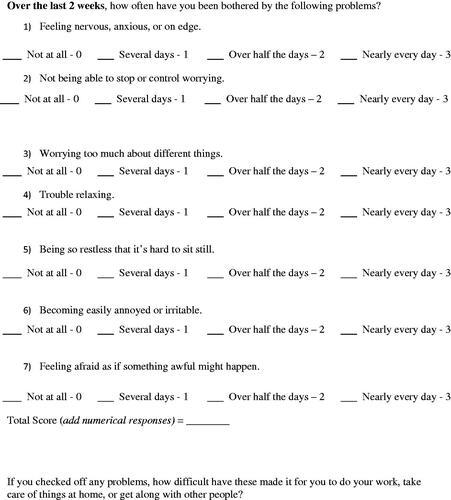
Adolescent anxiety
The Generalized Anxiety Disorder Scale (GAD-7) (Spitzer, Kroenke, Williams, & Löwe, Citation2006) is a seven-item practical self-report anxiety questionnaire where participants are asked how often, during the last two weeks, they have been bothered by each of the seven core symptoms of generalized anxiety disorder. Response options are “not at all,” “several days,” “more than half the days,” and “nearly every day,” scored as 0, 1, 2, and 3 respectively. Therefore, GAD-7 scores range from 0 to 21, with scores of >5, >10, and >15 representing mild, moderate, and severe anxiety symptom levels. In this study, the GAD-7 demonstrated high internal consistency (Cronbach’s alpha of 0.88) for the sample in this study. The GAD-7 has also shown strong reliability (0.85) and validity (73.3%) in prior research (Rutter & Brown, Citation2017).
Adolescent depressive symptoms
The Patient Health Questionnaire for Depressive Symptomology for Adolescents (PHQ-A) (Johnson, Harris, Spitzer, & Williams, Citation2002) is a self-report nine-item instrument to assess symptoms of depression among adolescents at study onset. Participants were asked to indicate how often they have been bothered by eight possible problems or symptoms over the last two weeks (e.g., “feeling down, depressed, or hopeless,” “feeling tired or having little energy,” and “feeling bad about yourself, or that you are a failure, or have let yourself or your family down”). Each item was rated 0 (not at all), 1 (several days), 2 (more than half the days), or 3 (nearly every day), and items were summed to obtain scale scores. Internal consistency for this scale was high (Cronbach’s alpha = 0.73) in the sample. The PHQ-A has also demonstrated strong reliability (0.875) (Bian, Li, Duan, & Wu, Citation2011).
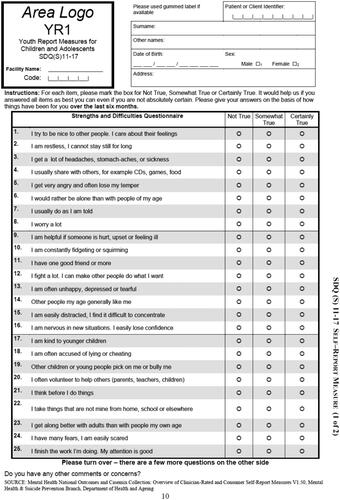
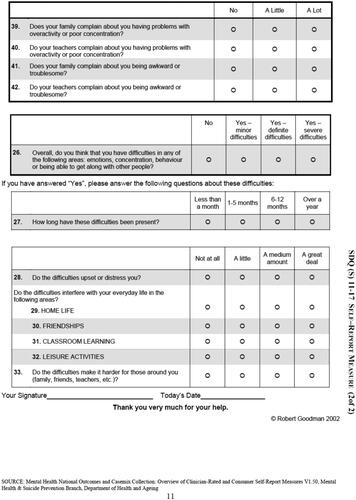
Adolescent strengths and difficulties
The Strengths and Difficulties Questionnaire for ages 11–17 (SDQ Self-Report 11–17) (Goodman, Citation1997) is a self-report questionnaire with 25 items that comprise the following five scales: emotional symptoms scale, conduct problem scale, hyperactivity scale, peer problem scale, and prosocial scale. The responses to items include “not true,” “somewhat true,” and “certainly true.” For each of the five scales, a participant’s score can range from 0–10 if all five items were completed. Scale scores can be prorated if at least three items were completed. A total difficulties score can be calculated from summing the emotion symptoms scale, conduct problem scale, hyperactivity scale, and peer problem scale. Reliability and validity vary according to respondent type and age of child self-reporting. Cronbach’s alpha for the five scales in the student form was 0.73. Copies of each instrument are included in the Appendix of this paper.
Analytical methods
To assess changes pre-and post-intervention, we used descriptive statistics and also examined differences in means between pre-intervention (T1) and post-intervention (T2) scores among the 16 students who completed the measures at both time points using a paired samples t-test or a Wilcoxon signed rank test with continuity correction for non-normal distributions. These analytical methods enabled us to assess changes in academic, social, and emotional functioning of adolescent participants. In addition, descriptive statistics were utilized to compare pre-and mid-intervention cortisol levels. As discussed above, post-intervention cortisol levels were not obtained due to coronavirus-mandated school closures.
Next, to determine any relationships between individual ACE scores and outcomes from the intervention, analyses of covariance (ANCOVA) following treatment completion was used to evaluate whether there were significant post-treatment differences in student-reported symptoms between children with low (0–1), moderate (2–3), and high (4+) ACE scores, with pre-intervention student-reported symptoms and attendance rate as the covariates. The outcome measures used in these analyses were GAD-7, PHQ-A, SDQ, and the SDQ subscales. ANCOVA is the clearest and most straightforward analysis to address each of the analytic goals.
Results
Despite the myriad challenges presented by external factors beyond the research team’s control, results of the study were very promising. There were marked improvements between pre- and post-survey data on participant anxiety and depression scales, as well as areas of improvement in their strengths and difficulties perceptions.
Promising changes in depressive symptomology
There were no statistically significant differences between depressive symptomatology among participants before or after this intervention. However, 75% of students noted an improvement in depressive symptoms; mean scores between pre- and post-surveys were reduced by 35.8%. The post-survey indicated an increase in “no” depressive symptoms by 49% over pre-survey responses and also showed a 40% reduction in mild depression symptoms and a 16% reduction in moderate symptoms among participants. The Wilcoxon signed rank test with continuity correction for the non-normal distribution of PHQ-A change scores indicated no significant difference between pretest and post-test scores in our analytic sample (V = 71, p = 0.0783).
Across outcomes, the ANCOVAS indicated that the post-test means, adjusted for pretest scores and attendance rate, did not significantly differ between the three ACE groups of low (0–1), moderate (2–3), and high (4+).
Statistically significant reductions in anxiety
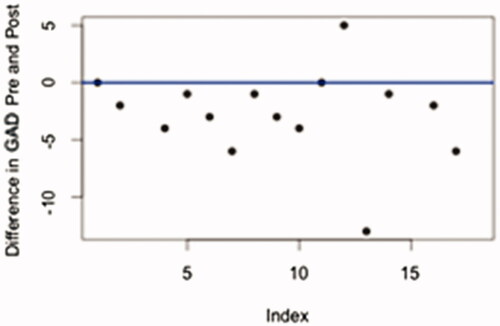
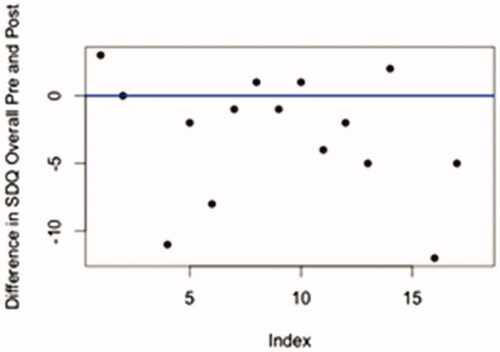
This scale indicated statistically significant improvements after participants were exposed to the intervention. Mean scores were reduced by 45.1%, and 81% of students reported improvements in their anxiety levels after the intervention. At the conclusion of the study, 27% more students reported only minimal anxiety (the lowest level on this scale) than at its outset; 4% of students reported a reduction in mild anxiety, 10% reported reduction in moderate anxiety symptoms, and 10% reported a reduction in severe symptomatology. The results from the pretest (M = 7.33, SD = 5.44) and post-test (M = 4.20, SD = 5.36) Generalized Anxiety Disorder Scale (GAD-7) indicate that the yoga intervention resulted in an reduction in anxiety symptoms, t(14) = 2.702, p = .017. A simple difference plot for the GAD-7 () provides visual evidence that the majority of observations had a higher GAD score at baseline than post-intervention.
Improvement in overall student perceptions of personal strengths and challenges; variability in subscales
Overall student self-reported SDQ scores indicated statistically significant improvements at the conclusion of the study. Teacher and parent SDQ outcomes were not completed by many participants and therefore have been excluded from the results of this study. Overall mean scores were reduced by 12.8% after the trauma-informed yoga practice, and 63% of students reported improvements in their perceptions of personal strengths and challenges. Further, the proportion of overall scores in the “normal” range increased by 14% and scores in the “abnormal” range decreased by 19% after the intervention. There was also a significant decrease in the overall self-reported strengths and difficulties after the intervention (M = 20.47, SD = 7.33) compared to pre-intervention (M = 23.72, SD = 7.48), t(14) = 2.492, p = .026. shows that the majority of observations had a lower SDQ overall score post-intervention than at baseline.
Figure 2. SDQ overall simple difference plot. Note. Points below the blue line indicate observations where baseline was greater than post-intervention, that is where (post—pre) is negative.
Subscale scores were more variable in their outcomes. The emotional subscale reported statistically significant reductions in emotional difficulties with a 29.4% reduction in mean scores and 63% of respondents reporting improvement in emotional functioning. The results from the pretest (M = 3.33, SD = 2.03) and post-test (M = 2.33, SD = 2.13) SDQ Emotional Symptoms Scale indicate that the yoga intervention resulted in an reduction in emotional symptoms, t(14) = 2.385, p = .032. The conduct subscale did not indicate any significant changes statistically, but mean scores were reduced by 16% on the post-survey with 44% of students self-reporting an improvement in their conduct. The hyperactivity scale also did not show any significant changes, with only minor reductions in mean scores (3.8%), but 50% of respondents reported an improvement in their hyperactivity levels. Lastly, the impact scores of participants (how much these difficulties impacted their everyday lives) were statistically significantly improved after the intervention, showing a 48.2% reduction in mean scores, and 44% of respondents reporting improvements.
Interestingly, subscale scores that showed a decline after the intervention both focused on interpersonal difficulties: the peer problems and prosocial scales. A Wilcoxon signed rank test with continuity correction for the non-normal distribution of this peer problem scale indicated a significant increase in the peer problems after the intervention (M = 2.73, SD = 1.83) compared to pre-intervention (M = 1.67, SD = 1.24), V = 25, p-value = .047. The prosocial subscale did not show statistically significant differences; while there was a 10.1% decrease in mean scores after the study, 56% of respondents noted a decline in their overall prosocial behaviors. Results for each outcome of interest are provided in .
Table 4. Pre/post difference in means for outcomes.
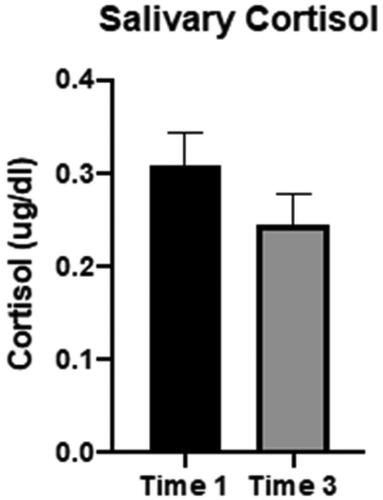
Marked decreases in cortisol levels and improvement in participant sleep
Salivary cortisol assays were assessed using the Abcam (ab154996) cortisol in vitro competitive ELISA (Enzyme-Linked Immunosorbent Assay) kit designed for the accurate quantitative measurement of cortisol in saliva (sensitivity 0.12 ng/mL). Comparisons using paired t-tests between pre and mid-intervention time periods showed marked decreases in cortisol levels in participants and nearly statistically significant improvements in participant sleep duration (p = 0.06) from pre- to mid-intervention. While these do not exhibit truly statistically significant differences, it is important to note that these levels occurred only after 4 weeks of the intervention and do not reflect final cortisol levels after a full intervention cycle, as these could not be collected due to the pandemic-related school closures.
displays the differences in salivary cortisol levels from pre-intervention to mid-intervention. displays the descriptive statistics regarding the salivary cortisol levels from pre to mid-intervention. Lastly, displays the descriptive differences in participant sleep duration from pre to mid-intervention.
Table 5. Pre/mid-intervention difference in means for salivary cortisol (salivary cortisol levels (ug/dL).
Table 6. Pre/mid-intervention difference in means for previous night’s sleep duration.
Unique difficulties and score variability of participants
Along with the quantitative analysis, qualitative results also provided data to gain additional insight into participant perspectives regarding the impact of the trauma-informed intervention. According to Patton (Citation2015), qualitative inquiry provides a lens through which individuals “perspectives and experiences” can be understood (p. 12). Qualitative comments provided by some students on the SDQ proved to be helpful in determining areas of unique difficulties among participants. For example, some of the comments in the pre-survey included the following:
-Have been struggling with Depression and on medication and going to counsiling (sic).
-Taking Anti-depressants and counseling; Most of these have nothing to with my stress levels.
-Sure I do stress but I have diagnosed ADHD, anxiety and depression (sic), so those just make those answers. [M]y land lord (sic) whom I consider a granfather (sic) died on [date redacted for privacy).
These responses, shared with school faculty and administration, provided important insights for participants so that further support could be offered to these students.
Comments from the post-SDQ were also useful in determining potential reasons for variability in scores from the pre-SDQ. Example comments included, the most noteworthy of which being the final statement:
-I believe this study will show that yoga has relaxed me and made me less stressed.
-My great grandma has kidney cancer. That is why there are difficulties.
-Isolation due to COVID-19 may have an effect on the answers to many of the questions.
Increased Interoception
Participants in the study were also provided an opportunity to share their thoughts through reflective journals. Several entries seem to support the concept of an increase in interoception both during the sessions and more broadly. During the sessions, there were multiple entries which indicated an awareness of feelings, both positive and negative. Students used words such as “tired” and “stressed” to indicate their feelings at the beginning of sessions. For example, one participant stated “I’m super tired and sore have little energy feel so much better” while another student stated “relieved a lot of stress and feeling myself become more flexible.” The majority of participants used words such as “calm” or “relaxed” to indicate how they felt upon completing each session. Examples of journal entries noting feeling of calm and/or relaxed include the following:
I learn more yoga things and it helps me calm down.
I thought this was dumb and a waste of time, but as we got started I enjoyed it, I feel a little relaxed.
I feel really calm and relaxed. I didn’t think I would like it but it was good.
I enjoyed today’s session. It was relaxing.
Feel very calm.
I feel very relaxed, my mind is calm and it is nice.
From a broader perspective, one student noted that “I’m more awake for what’s happening in life” while another student stated “I had a really bad week, but now I feel good and I was able to forget.” Finally, one student stated “I was very relaxed after this, it helped to clear my mind, I am growing to appreciate yoga more and more.” Along with the benefits expressed by participants in relation to feeling more relaxed, the qualitative results also suggest that they were able to “cultivate sensory awareness” which could also positively impact their ability to foster emotional regulation (van der Kolk, Citation2014, p. 275). Overall, the reflective journal entries indicated that students felt much calmer and relaxed after each yoga session.
Improved Perceptions of Well-Being
In addition to reflective journals, students provided feedback through an informal survey to ascertain program strengths and challenges. General themes from this feedback included improved perceptions of physical health and overall well-being, reductions in stress, and improvements in academic focus and relaxation. The themes reflect a “wellness model” of heath which emphasizes “self-healing” along with an emphasis on “mental and social well-being” in addition to complete physical health (Edlin & Golanty, Citation2019, p. 5). The journal responses support an overall sense of well-being which aligns with positive emotions and life satisfaction. Below, provides sample student responses from this survey.
Table 7. Sample student survey responses.
Interestingly, the majority of the students preferred meditation over the physical practice, which the team found surprising given that this intervention took place in a strength training class; this indicates that students found it to be more beneficial and deserves to be given more attention and time in future iterations of this study. Additionally, some students noted that they did not like writing in their reflective journals at the conclusion of each session, and others shared that they did not feel any change or difference resulting from the practice, citing that they wanted more of a physical challenge. Other than these outlying comments, however, students generally communicated to have enjoyed and received benefits from this intervention.
Outcomes of CBPR process
Due to the positive results from this intervention, the community and school district has communicated a desire to continue this research in a larger follow-up study; one administrator shared the following noteworthy take-aways resulting from the study in an email communication:
-We can get parent permissions and can conduct screening in the socio-emotional domain.
- We can participate in really, really cool research that can tell us meaningful things about what might improve mental health indicators for our kids
-The people working together on it (names redacted for confidentiality) are all really, really fine people who work together well and truly care about (name of town redacted for privacy)’s kids.
-Yoga is cool and the trauma-informed version appears to be good for student well-being.
-Students are likely to embrace being involved in future studies and feel they're part of something important.
-Other stakeholders among our staff, families and community like it.
Discussion
Results from this study were positive when analyzed descriptively, quantitatively, and qualitatively. As summarized above, there were statistically significant declines in anxiety symptomatology, overall strengths and difficulties scores, and the emotional symptoms SDQ subscale. While not statistically significant, marked improvements were also indicated in depressive symptomatology, cortisol levels, and sleep duration among participants.
A statistically significant increase in peer problems and prosocial SDQ subscales was reported following this intervention. We hypothesize that, to account for these increased difficulties, participants may have cultivated a deeper sense of interoception as a result of their involvement in the study. Bessel van der Kolk (Citation2014) asserts that it is critical for those recovering from trauma to cultivate sensory awareness or interoception as opposed to going through each day in a numbing type of experience. According to van der Kolk (Citation2014), participation in yoga can provide a space to focus attention on the sensory experience of breathing along with making “connections between your emotions and your body” (p. 275). Although this mind-body connection long term is beneficial, the initial awareness can be challenging to negotiate. For some participants, the awareness of their emotions (as opposed to a sense of numbness) could then have resulted in an increased awareness of emotions (both positive and negative) toward their peers. This could indicate the need for an enhanced SEL curriculum to support students in learning how to positively navigate conflict with their peers. Another possible rationale for the findings could also correspond with the increased stress due to COVID-19.
Implications
Together, the quantitative and qualitative findings provide evidence of the feasibility and potential of a trauma-informed yoga intervention in a rural context. Brackett (Citation2019) asserts that “anxiety disorders are the most common mental illness in the U.S., affecting 25% of children between 13 and 18 years old….[and] Depression is the leading cause of disability worldwide” (p. 3). The mental health epidemic present in our nation, but especially in rural adolescents, can no longer be ignored. Additionally, 20% of American’s youth experiences a mental illness, and over 50% of all seventeen-year-olds report having either experienced trauma directly or indirectly (Brackett, Citation2019). Brackett further postulates that by “failing to recognize trauma’s effects on learning, educators risk compounding the trauma and jeopardizing students’ prospects in school” (Citation2019, p. 192).
Further, in a recent study of 22,000 teenagers nationally about how they feel in school, 77% of respondents replied with negative terms like “tired,” “bored,” and “stressed.” American teenagers also lead the world in violence, binge drinking, marijuana use, and obesity (Brackett, Citation2019, p. 14, 191). These unhealthy coping strategies place an unnecessary burden on the nation’s economy, both in terms of a productive workforce, healthcare costs, and the nation’s judiciary and prison systems (Bellis et al., Citation2019). In order to mitigate the impacts of childhood adversity and mental illness, we must confront these issues head-on in the context of our K-12 public schools.
Based on this study’s outcomes, integrating a trauma-informed yoga intervention into a physical education curriculum and/or regular education classroom may be indicated. We hypothesize that in addition to improved mental and behavioral health outcomes, students (and classroom teachers) may experience an improvement of classroom/school climate and culture, therefore additionally remedying common classroom management issues frequently addressed by teachers (Butzer, Bury, Telles, & Khalsa, Citation2016). Furthermore, we believe that an inclusion of a trauma-informed yoga practice into a school setting has the potential to improve academic achievement, particularly by those with a high incidence of adverse childhood experiences. Although this aspect of the study has yet to be fully researched and validated, other studies suggest this possibility (Butzer et al., Citation2015).
Perhaps what should be considered most importantly, however, is the feedback from the students who participated in this study. It sends a powerful message when rural high school students, who initially exhibited great reluctance in participating in yoga in their strength-training class, share that “everyone should do yoga” at the study’s conclusion. While the improvements in mental and behavioral health are significant, the fact that these high school students, most of whom have high ACE scores, found true benefits from the practice, is an indication that there is power in this practice. The research team has great hope that trauma-informed yoga could provide a low-cost, high-reward intervention when applied thoughtfully and purposefully in the public school context, especially for at-risk and rural students.
Study limitations
As alluded to previously, there were limitations to this study, both in design and also extenuating circumstances. While the research team hoped to have enough of a sample size to analyze statistical significance, only one physical education teacher was willing to share his class time for this study; as a result, we had a small sample of 16 students as participants (out of a class of 20 students total). This was a nonrandom sample, as students self-selected to participate in the intervention. Selection bias prohibits us from making causal claims about the efficacy of the yoga intervention. This sample was ethnically homogenous (all were white), and only two students were female, so our sample was heavily skewed toward males. Additionally, attendance for the intervention was inconsistent among several participants (with an average intervention participation rate across all participants of 80%), which inevitably impacted study results, but also makes our findings more conservative. Poor school attendance is often related to the incidence of adverse childhood experiences (Blodgett & Lanigan, Citation2018).
Regarding the intervention, the research team was unable to secure a single yoga teacher for every session of the intervention, so two teachers were used each week of the intervention, which introduces the possibility of variability of results based on different teachers’ styles. As mentioned earlier, our study was also truncated due to the mandated school closures from COVID-19, so participants only completed seven rather than the scheduled eight weeks of the intervention. Moreover, because of these closures, a final cortisol collection was unable to occur, and post-surveys were disseminated online for students to complete while at home; because of these limitations, only 16 out of 18 participants completed the post-surveys, further limiting our results. It is also highly likely that the external stressors caused by the pandemic may artificially deflate post-survey scores or underestimate improvements (one participant actually noted this in one of his post-survey comments). Additionally, the research team has concerns regarding potential survey bias for students who scored high on the suicidal ideation question on the Patient Health Questionnaire for Adolescents. These students, per medical guidance from the PHQ-A, were pulled the same day of the pre-survey to assess immediate risk by the school nurse (which is the medical/psychological recommendation), but this action may have influenced those students to not answer in such a way that they would be “called out” (or parents notified) on their PHQ-A post-survey.
Lastly, parent and teacher participation with one of the survey measures (the Strengths and Difficulties Questionnaire for ages 11–17) was uneven, at best. Despite classroom supply money being offered as an incentive for teachers, many pre-surveys were not completed until four weeks into the intervention, so these results are likely skewed; we received only seven teacher post-surveys on students, which is likely the result of teachers moving instruction online in the midst of school closures. Additionally, parent participation was poor: three completed pre-surveys, five completed post-surveys, and only two completed both a pre-and post-survey for their child. As a result, teacher and parent surveys are inconclusive. In future research, efforts need to be made by the research team to further incentivize both teacher and parent participation to increase engagement and participation to gather critical data from relevant adults in participants’ lives.
Conclusions
Although the positive behavioral and physical health outcomes of this study are evident based on reductions in salivary cortisol levels, depression, and anxiety scales, additional research is needed to assess efficacy and substantiate generalizability to a broader population. Therefore, future research should have a larger sample size and a control group to determine greater statistical significance and feasibility of implementing this intervention in a larger context. Further, while variations of this pilot study have taken place at the middle and upper elementary levels in another state, this specific research design must be tested across multiple grade levels to assess efficacy across various age groups. Similarly, there is a pressing need to expand this study to more diverse student populations, as the sample for this study was not only small but very racially/ethnically homogenous. Furthermore, there is an opportunity to share this intervention with indigenous communities both in Montana and beyond, as historical and generational trauma are ever-present in these areas (Bird et al., Citation2016; Duran, Citation2006; Walters et al., Citation2011).
Ethics Statement
The Institutional Review Board of Montana State University has approved the research outlined in this manuscript.
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Additional information
Funding
References
- American Foundation for Suicide Prevention. (2017). Suicide: Montana 2017 facts & figures. https://dphhs.mt.gov/assets/suicideprevention/SuicideinMontana.pdf
- Bian, C., Li, C., Duan, Q., & Wu, H. (2011). Reliability and validity of patient health questionnaire: Depressive syndrome module for outpatients. Scientific Research and Essays, 6(2), 278–282.
- Bird, S., Held, S., McCormick, A., Hallett, J., Martin, C., & Trottier, C. (2016). The Impact of historical and current loss on chronic illness: Perceptions of crow (apsáalooke) people. International Journal of Indigenous Health, 11(1), 198–210. doi:10.18357/ijih111201614993
- Bellis, M., Hughes, K., Ford, K., Rodriguez, G., Sethi, D., & Passmore, J. (2019). Life course health consequences and associated costs of adverse childhood experiences across Europe and North America: A systematic review and meta-analysis. The Lancet Public Health, 4(10), e517–528. doi:10.1016/S2468-2667(19)30145-8
- Blodgett, C., & Lanigan, J. D. (2018). The association between adverse childhood experience (ACE) and school success in elementary school children. School Psychology Quarterly : The Official Journal of the Division of School Psychology, American Psychological Association, 33(1), 137–146. doi:10.1037/spq0000256
- Brackett, M. (2019). Permission to feel. New York, NY: Celadon Books.
- Bucci, M., Gutiérrez, W., Koita, K., Purewal, S., Silvério, M. B., & Harris, N. (2015). Center for youth wellness ACE-questionnaire user guide. San Francisco, CA: Center for Youth Wellness.
- Burke Harris, N., & Renschler, T. (2015). Center for Youth Wellness ACE-Questionnaire (CYW ACE-Q Child, Teen, Teen SR). Center for Youth Wellness. San Francisco, CA.
- Burke-Harris, N. (2018). The Deepest well: Healing the long-term effects of childhood adversity. New York, NY: Houghton Mifflin Harcourt.
- Buscko, K., & Rychlik, R. (2006). Changes of the maximal muscle torque in women training power yoga (ashtanga vinyasa). Human Movement, 7(2), 168–177.
- Butzer, B., Bury, D., Telles, S., & Khalsa, S. B. S. (2016). Implementing yoga within the school curriculum: A scientific rationale for improving social-emotional learning and positive student outcomes. Journal of Children’s Services, 11(1), 3–24. doi:10.1108/JCS-10-2014-0044
- Butzer, B., van Over, M., Noggle Taylor, J., & Khalsa, S. (2015). Yoga may mitigate decreases in high school grades. Evidence-Based Complementary and Alternative Medicine, 2015, 1–8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4546979/.
- Carrey, N., Butter, H., Persinger, M., & Bialik, R. (1995). Physiological and cognitive correlates of child abuse. Journal of the American Academy of Child and Adolescent Psychiatry, 34(8), 1067–1075. doi:10.1097/00004583-199508000-00017
- Collaborative for Academic, Social and Emotional Learning (2020). Reunite, renew and thrive: Social and emotional learning (SEL) roadmap for reopening school. https://casel.org/wp-content/uploads/2020/07/SEL-ROADMAP.pdf.
- Cook-Cottone, C., Talebkhah, K., Guyker, W., & Keddie, E. (2017). Mindfulness and yoga in schools. New York, NY: Springer Publishing.
- Cook-Cottone, C., LaVigne, M., Guyker, W., Travers, L., Lemish, E., & Elenson, P. (2017). Trauma-informed yoga: An embodied, cognitive-relational framework. International Journal of Complementary Medicine, 9(1), 00091. https://medcraveonline.com/IJCAM/IJCAM-09-00284.pdf
- Centers for Disease Control and Prevention (CDC) (2020). Suicide mortality by state. https://www.cdc.gov/nchs/pressroom/sosmap/suicide-mortality/suicide.htm.
- Duran, E. (2006). Healing the soul wound: Counseling with American Indians and other Native people. New York, NY: Teachers College Press.
- Edlin, G., & Golanty, E. (2019). Health & wellness (13th ed.). Burlington, MA: Jones and Bartlett Learning.
- Emerson, D., & Hopper, E. (2011). Overcoming trauma through yoga: Reclaiming your body. Berkeley, CA: North Atlantic Books.
- Faridi, Z., Grunbaum, J., Gray, B., Franks, A., & Simoes, E. (2007). Community-based participatory research: Necessary next steps. Preventing Chronic Disease, 4, A70. http://www.cdc.gov/pcd/issues/2007/jul/06_0182.htm.
- Felitti, V., Anda, R., Nordenberg, D., Williamson, D., Spitz, A., Edwards, V., … Marks, J. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14(4), 245–258. doi:10.1016/S0749-3797(98)00017-8
- Fletcher, F., Hibbert, A., Robertson, F., & Asselin, J. (2013). Needs and readiness assessments: Tools for promoting community-university engagement with Aboriginal communities. Gateways: International Journal of Community Research and Engagement, 6, 131–149. doi:10.5130/ijcre.v6i1.3219
- Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 38(5), 581–586. doi:10.1111/j.1469-7610.1997.tb01545.x
- Hammer, B., Fletcher, F., & Hibbert, A. (2017). Participant observation: Enhancing the impact measurement in community based participatory research. The Qualitative Report, 22(2), 439–455. doi:10.46743/2160-3715/2017.2553
- Holkup, P., Tripp-Reimer, T., Salois, E., & Weinert, C. (2004). Community-based participatory research: An approach to intervention research with a Native American community. ANS. Advances in Nursing Science, 27(3), 162–175. doi:10.1097/00012272-200407000-00002
- Hölzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M., Gard, T., & Lazar, S. W. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry research, 191(1), 36–43. doi:10.1016/j.pscychresns.2010.08.006
- Horowitz, C., Robinson, M., & Seifer, S. (2009). Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation, 119, 2633–2642. http://circ.ahajournals.org/
- Israel, B., Schulz, A., Parker, E., & Becker, A. (2001). Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Education for Health (Abingdon, England), 14(2), 182–197. doi:10.1080/13576280110051055
- Israel, B., Schulz, A., Parker, E., Becker, A., Allen III, A., & Guzman, J. (2003). Critical issues in developing and following community-based participatory research principles. In Community-based participatory research for health (pp. 53–76). San Francisco, CA: Jossey-Bass.
- Johnson, J., Harris, E., Spitzer, R., & Williams, J. (2002). The Patient health questionnaire for adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 30(3), 196–204. doi:10.1016/S1054-139X(01)00333-0
- Kaiser Family Foundation. (2016). Mental health care health professional shortage areas (HPSAs) 2016. https://www.kff.org/other/state-indicator/mental-health-care-health-professional-shortage-areas-hpsas.
- Khalsa, S. B., Hickey-Schultz, L., Cohen, D., Steiner, N., & Cope, S. (2012). Evaluation of the mental health benefits of yoga in a secondary school: A preliminary randomized controlled trial. The Journal of Behavioral Health Services and Research, 39(1), 80–90. https://www.ncbi.nlm.nih.gov/pubmed/21647811.
- Levine, P. (1997). Waking the tiger: Healing trauma- the innate capacity to transform overwhelming experiences. Berkeley, CA: North Atlantic Books.
- Lukens, J. (2017, September 20). Confronting adverse childhood experiences to improve rural kids’ lifelong health. Rural Health Information Hub: The Rural Monitor. Retrieved from https://www.ruralhealthinfo.org/rural-monitor/adverse-childhood-experiences/
- Malchiodi, C., & Perry, C. (2020). Rhythms and regulation: Innovative approaches to brain and body during a time of immobilization. Paper presented at the Annual Trauma Research Foundation Conference, Boston, MA.
- Montana Adolescent Substance Abuse Facts. (2015). HHS office of adolescent health. Retrieved from https://www.hhs.gov/ash/oah/facts-and-stats/national-and-state-data-sheets/adolescents-and-substance-abuse/montana/index.html
- Montana Department of Public Health and Human Services. (2016). 2016 Suicide mortality review team report. Retrieved from https://www.sprc.org/sites/default/files/resource-program/2016%20Montana%20Suicide%20Mortality%20Review%20Report.pdf
- Montana Department of Public Health and Human Services. (2018). Suicide in Montana: Facts, figures, and formulas for prevention. https://dphhs.mt.gov/Portals/85/suicideprevention/SuicideinMontana.pdf
- Montana Office of Public Instruction. (2019). Park County, Montana Youth Risk Behavior Survey. Helena, MT: Montana Office of Public Instruction.
- National Center for Frontier Communities. (2018). Defining the frontier. Retrieved from http://frontierus.org/
- National Network of Libraries of Medicine. (2020). General facts: Montana. https://nnlm.gov/pnr/about/montana.
- Newman, S., Andrews, J., Magwood, G., Jenkins, C., Cox, M., & Williamson, D. (2011). Community advisory boards in community-based participatory research: A synthesis of best processes. Preventing Chronic Disease, 8(3), A70.
- Noddings, N. (2005). What does it mean to educate the whole child? Educational Leadership, 63(1), 8–13.
- Patton, M. (2015). Qualitative research and evaluation methods (4th ed.). Thousand Oaks, CA: SAGE.
- Ratey, J. J. (2008). SPARK: The revolutionary new science of exercise and the brain. New York, NY: Little, Brown and Company.
- Rutter, L. A., & Brown, T. A. (2017). Psychometric properties of the generalized anxiety disorder scale-7 (GAD-7) in outpatients with anxiety and mood disorders. Journal of Psychopathology and Behavioral Assessment, 39(1), 140–146. doi:10.1007/s10862-016-9571-9
- Saul, J. (2013). Collective trauma, collective healing: Promoting community resilience in the aftermath of disaster. New York, NY: Routledge.
- Salmon, P., Lush, E., Jablonski, M., & Sephton, S. (2009). Yoga and mindfulness: Clinical aspects of an ancient mind/body practice. Science Dir5ect, 16, 59–72. doi:10.1016/j.cbpra.2008.07.002
- Spinazzola, J., Rhodes, A., Emerson, D., Earle, E., & Monroe, K. (2011). Application of yoga in residential treatment of traumatized youth. Journal of the American Psychiatric Nurses Association, 17(6), 431–444. doi:10.1177/1078390311418359
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi:10.1001/archinte.166.10.1092
- Substance Abuse and Mental Health Services Administration. (2015). Behavioral health barometer: Montana, 2015. https://www.samhsa.gov/data/sites/default/files/2015_Montana_BHBarometer.pdf
- Substance Abuse and Mental Health Services Administration. (2017). 2015–2016 NSDUH state prevalence estimates. Retrieved from https://www.samhsa.gov/data/report/2015-2016-nsduh-state-estimates-substance-use-and-mental-disorders.
- Talbot, J., Szlosek, D., & Ziller, E. (2016). Adverse childhood experiences in rural and urban contexts. Portland, ME: Maine Rural Health Research Center: Research and Policy Brief (PB-64). https://muskie.usm.maine.edu/Publications/rural/Adverse-Childhood-Experiences-Rural.pdf
- U.S. Department of Health and Human Services: Health Resources and Services Administration, Maternal and Child Health Bureau. (2015). The health and well-being of children in rural areas: A portrait of the nation, 2011–2012. Rockville, MD: Author. https://mchb.hrsa.gov/nsch/2011-12/rural-health/pdf/rh_2015_book.pdf#page=51
- van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. New York: Viking.
- Walker, T. (2014). The testing obsession and the disappearing curriculum. http://neatoday.org/2014/09/02/the-testing-obsession-and-the-disappearing-curriculum-2/
- Walters, K., Mohammed, S., Evans-Campbell, T., Beltrán, R., Chae, D., & Duran, B. (2011). Bodies don’t just tell stories, they tell histories: Embodiment of historical trauma among American Indians and Alaska natives. Du Bois Review: Social Science Research on Race, 8(1), 179–189. doi:10.1017/S1742058X1100018X
Appendices
Appendix A: Center for Youth Wellness ACE-Q survey (Burke-Harris & Renschler, 2015)
Note: A toxic stress questionnaire is also a part of this instrument but was not included in this study.
Appendix B: Generalized Anxiety Disorder 7-item (GAD-7) scale (Spitzer et al., Citation2006)
Appendix C: Patient Health Questionnaire for Adolescents (Johnson, Johnson et al., Citation2002)