ABSTRACT
The provision of choice within interventions has been associated with increased motivation, engagement and interest, as well as improved clinical outcomes. Existing reviews are limited by their wide inclusion criteria or by not assessing behaviour change and mood outcomes. This review examines whether participant-driven choice-based interventions specifically are more likely to be enjoyed and accepted by participants compared to no-choice interventions, and whether this impacts on intervention outcomes in terms of behaviour change or mood. Forty-four randomised controlled trials were identified for inclusion. Random effects meta-analyses were performed for retention-related outcomes (drop-out, adherence and satisfaction), and aggregate behaviour change and mood outcomes. Choice-based interventions resulted in significantly less participant drop-out and increased adherence compared to interventions not offering choice. Results for the behaviour change and mood analyses were mixed. This meta-analytic review demonstrates that choice-based interventions may enhance participant retention and adherence, thus researchers and clinicians alike should consider the provision of choice when designing research and interventions. The evidence for the role of choice in behaviour change and mood is less convincing, and there is a need for more, higher quality research in this area.
Introduction
Individualised intervention design is an approach that takes into account individual needs and variability in terms of personal preference or relevance (Suhonen et al., Citation2008). Systematic and meta-analytic reviews have found that this type of intervention can have a range of positive outcomes compared to non-individualised interventions, including behavioural outcomes such as adherence to a care regimen, physical activity, and smoking; health outcomes such as skin health, functional health status and pain; and many more including knowledge, anxiety and confidence (Krebs et al., Citation2010; Lustria et al., Citation2013; Noar et al., Citation2007; Suhonen et al., Citation2008).
Choice interventions are a specific subset of individualised interventions, which differ slightly in that they allow participants to have an active role in determining an aspect of the treatment or intervention. This is contrasted with other individualised interventions which may provide a modified or tailored intervention based on some measured characteristic such as personality, motivation, or coping style. The element of active choice and thus increased control may have additional positive consequences for both the individual and the intervention efficacy.
The importance of choice
Control and autonomy are recognised as key factors in several behaviour change theories. According to self-determination theory (Deci & Ryan, Citation1980; Ryan & Deci, Citation2000), autonomy is one of the key components that underlies intrinsic motivation. This in turn can lead to other positive outcomes such as improved learning, task engagement, perceived competence, and better health (Deci & Ryan, Citation2012)). Similarly, the theory of planned behaviour identifies perceived control as a key factor driving behaviour (Ajzen, Citation1985). Several studies have demonstrated that both autonomy and perceived control are linked to wellbeing, positive mood and positive attitudes (Grob, Citation2000; Reis et al., Citation2000; Sheldon et al., Citation1996), as well as being an important component in behaviour change (Terry & O'Leary, Citation1995; Williams et al., Citation1998). Given that choice may increase both perceived control (Rotter, Citation1966; Staub, Citation2013) and autonomy (Dan-Cohen, Citation1992), it is possible that the very act of allowing choice can lead to changes in both behaviour and mood, regardless of what the choice is between. Indeed, choice has been found to increase feelings of personal control, motivation, and interest, even when choices appeared trivial or mundane (Cordova & Lepper, Citation1996; Swann Jr & Pittman, Citation1977).
A further potential benefit of providing choice in intervention design may be the increase in personal relevance and acceptability. In lay terms, not all people like the same things. Therefore, providing choice increases the likelihood that at least one of the options will be acceptable to the participant. Indeed, meta-analytic reviews have shown that both personal preference and choice leads to increased adherence and intervention satisfaction, as well as better clinical outcomes in terms of both medical and mental health (Lindhiem et al., Citation2014). When participants do not receive their treatment of choice, on the other hand, they may experience negative attitude or resentful demoralisation, leading to poorer motivation and adherence (Bowling & Rowe, Citation2005; Bradley, Citation1993; Torgerson et al., Citation1996). Relatedly, the restriction of choice may have negative consequences. For instance, restricting choice can lead to diminished learning and motivation (Deci et al., Citation1989; Seligman, Citation1975), as well as poorer adherence, decreased engagement, reduced tolerance for any inconvenience that may arise in a study setting, and increased dropout (Bradley, Citation1993, Citation1997; Brewin & Bradley, Citation1989; Feine et al., Citation1998; McPherson & Britton, Citation1999; McPherson et al., Citation1997).
While the above points to the many benefits of providing choice in intervention design, there is some evidence that choice may have no effect on motivation, engagement or attrition (Flowerday & Schraw, Citation2003; Flowerday et al., Citation2004; King et al., Citation2005), and some studies have found negative consequences of choice, including poorer decision making and poorer performance in subsequent tasks (Baumeister et al., Citation1998; Bruyneel et al., Citation2006; Gourville & Soman, Citation2005; Iyengar & Lepper, Citation2000; Schwartz, Citation2004; Vohs et al., Citation2004).
Given this mixed evidence, the present review seeks to provide an updated synthesis of this literature, extending previous reviews by considering both behavioural and mood outcomes. In order to provide a comprehensive review of the evidence we did not restrict trials according to specific diseases, patient groups or clinical contexts. Thus, we considered interventions in various forms, ranging from choice of treatment for depression or anxiety, to choice of physical activity in healthy adults, and from choice of cancer screening method in at-risk populations to choice of incentive for achieving a walking goal for sedentary or overweight adults. Further, this review addresses a significant limitation of previous reviews that have been confounded by the inclusion of heterogeneous study designs which either do not focus solely on choice itself, or do not compare with directly comparable no-choice interventions. For example, previous reviews such as Lindhiem et al. (Citation2014) and King et al. (Citation2005) include preference-based studies which do not involve active participant choice, as well as shared decision making which does include active choice, but is not necessarily the same as free, participant-driven choice. These reviews also include designs where those who refuse randomisation are provided with choice, and designs where choice is offered but those without strong preferences are randomised, both of which introduce the potential for systematic differences between choice and no-choice groups (i.e., the factors that may contribute to having (or not) a strong preference). Thus, whilst previous reviews do provide insight into the effect of receiving a preferred intervention, they are limited by the types of included studies, and cannot necessarily speak to the effect of choice. To our knowledge, no review to date has focused solely on fully randomised studies of participant-driven, active choice, compared with equivalent no-choice interventions. Here we apply stricter criteria focusing on studies where participants were fully randomised to choice and no-choice groups and made an active, independent choice. This will enable a higher degree of confidence that any observed benefits are due to this choice alone, and not impacted by other factors, such as the influence of the clinician or differences in participant characteristics.
Methods
Inclusion and exclusion criteria
Multiple inclusion criteria were applied to the systematic search. Firstly, only randomised controlled trials (RCTs) were included, as these are widely considered the gold standard of study design and are least susceptible to bias (Hariton & Locascio, Citation2018). This included both traditional RCTs, where participants are randomised to a choice group or two or more no-choice groups, and yoked designs in which participants are randomised to choice and no-choice groups, and then no-choice group participants are matched to a choice group participant. Alternatively, participants may be first matched and then randomised. Additionally, two-step RCTs such as Wennberg designs, where participants are firstly randomised to a choice or no-choice group, and then no-choice group participants are re-randomised to the various study interventions, whereas the choice group select their preference (Wennberg et al., Citation1993), were also included. Other designs that involve differential treatment based on participant preference were excluded. This included Brewin designs, in which randomisation takes place if there is no strong preference between groups, and those with a preference are given their choice (Brewin & Bradley, Citation1989). Rucker designs, which are similar to Wennberg designs but differ in that participants in the choice group who do not have strong preferences are re-randomised to the various intervention arms (Rücker, Citation1989), were also excluded. These types of design may result in systematic differences between those in the choice and those in the no-choice groups. Additionally, depending on how groups are analysed, these designs may result in a high proportion of participants not receiving their intended intervention. For instance, Ayre et al. (Citation2020) employed a Rucker design where 23% of those randomised to choice were undecided, and so were re-randomised to one of the two intervention arms. These participants were analysed as part of the choice group. Whilst retaining participants to their original randomly assigned allocation circumvents the issue of systematic differences between those in the choice and no-choice groups, given the proportion of participants who did not receive the intervention as intended, this study was excluded.
Secondly, the population was limited to adults aged 18 years and over, who were able to make an active choice regarding intervention content. As the focus of this review is on choice-based interventions, which differ in that they involve the participant playing an active role in individualising their intervention, only those interventions where the participants actively and consciously determined the content of the intervention were included. The primary element of the intervention had to be the provision of choice, and this had to be the only difference between the intervention and comparison groups. This was to ensure that results were not contaminated by other non-choice elements of the intervention. This included, for instance, studies where either the choice or no-choice group received extra elements of an intervention, or an additional option or condition. For example, Janevic et al. (Citation2003) included a usual care arm only for the no-choice participants (i.e., choice participants could not choose this option). This necessarily resulted in more differences between the groups than just choice. The aim of the choice arm had to be interventional. This was because studies that used choice as a control were unlikely to show any effect of choice as they were not designed to impact the outcomes, and therefore may bias the results of the review. Only studies that included a ‘no-choice’ comparison group were included, to determine whether giving participants an active role in determining the content of the intervention is more effective than not having that choice. Studies where participants believed they had a choice about the content of the intervention, but actually all participants received the same intervention, or both groups received preferred activities were included, provided that all those in the choice group believed they had chosen an aspect of their intervention, and those in the no-choice group believed they had not. Finally, studies had to report a retention-related (drop-out, satisfaction, or adherence), mood-related or behaviour change outcome.
The exclusion criteria included populations where the choice was made by a caregiver, carer or other third party, such as studies involving adults with severe dementia or brain injury preventing the ability to make a choice, as in these cases the participant is not the one actively determining the content of the intervention. Children were excluded as evidence suggests that adults and children may respond differently to choice-based interventions (Patall et al., Citation2008). In terms of interventions, those using methods of individualisation that did not involve participant choice, such as those that assessed participant preference but did not involve active choice, and those that were individualised based on personality, stage of change, participant goals or as part of cognitive behavioural therapy or counselling were excluded. Further, studies where the choice was not explicit, or where it was judged that participants in the choice group were pressured to pick a particular option were excluded, as research has found that the effect of this is significantly different from those that allow autonomous choice (Moller et al., Citation2006). Conference papers, letters, editorials, protocols, unpublished studies and stand-alone abstracts were excluded. Studies not published in English and studies published in non-peer reviewed journals such as dissertations were also excluded. Reasons for excluding studies were recorded (Supplementary Appendix A).
Selection of studies
Comprehensive searches of the following databases were conducted to identify potentially eligible studies: Medline; Embase; PsycInfo and PsycArticles. Key search terms included terms relating to choice and individualisation, behaviour change and mood (see Supplementary Appendix B). The search was conducted for all databases from earliest records up 8th February 2021. Additionally, the reference lists of any relevant identified reviews and all included studies were searched for additional references.
Data collection and extraction
All search results were screened by title and abstract against the inclusion and exclusion criteria, for possible inclusion. Studies that appeared to satisfy the inclusion criteria based on the titles and abstracts, or where it was unclear, then underwent a full text screening. This was primarily done by one reviewer, however for studies where there was significant uncertainty (n = 24), inclusion was discussed with a second reviewer until a consensus was reached. A data extraction spreadsheet was used to extract and record information from each included study. This included basic study information, participant details, intervention and comparator details, information about the reported outcomes, and the results. This also included the definition of each reported outcome, to make it clear how all outcomes were assessed. Where given, study authors’ definitions of outcomes were used. Where this was not provided or ambiguous, for instance where multiple possible definitions of adherence were reported, the most appropriate was discussed and agreed between two reviewers.
Risk of bias
Risk of bias was assessed using the Cochrane Collaboration RoB2 tool (Sterne et al., Citation2019). Each study was assessed for bias related to the randomisation process, deviations from the intended intervention, missing outcome data, measurement of the outcome and selection of the reported result. Two assessors (SC, RJ) independently assessed risk of bias. Agreement between the two reviewers for each risk of bias domain and the overall risk domain ranged from 44% to 78%. All discrepancies were discussed until a consensus was reached.
Meta-analysis
Analyses were conducted using Review Manager software, version 5.4. A random effect model was used for all analyses due to the high degree of variability between studies (Borenstein et al., Citation2010). Meta-analyses were performed separately for the three main retention-related outcomes (drop-out, adherence, and satisfaction), as well as aggregate outcomes for ‘total mood change’ and ‘total behaviour change’ to assess the total effect. For instance, the total behaviour change analysis combined the different behaviour change outcomes. Similarly, the overall mood analysis included different forms of mood such as depression and anxiety. This approach was taken because there was no reason a-priori to expect that effects of choice may differ by behavioural or mood related outcome. Additionally, it was considered that whilst drop-out and adherence are commonly reported, individual behaviour change and mood outcomes are less so, and therefore creating aggregate outcomes would ensure sufficient numbers of studies contributing to the meta-analyses.
For continuous outcomes, the mean and standard deviation (SD) were extracted or calculated to determine the differences in post-intervention means (MDs) and 95% confidence intervals (CIs). Standardised mean differences (SMDs) were calculated where studies had used different methods of assessment (for example depression as measured using the Beck Depression Inventory, Hamilton Depression scale etc.). Final scores were used where available, however for five outcomes this was not reported, and change scores were used. Sensitivity analyses were conducted to assess whether there was any significant impact of combining change and final scores in analyses using SMDs. There were no significant differences between groups at baseline in the outcomes in all but two studies, for which baseline data was not reported. For dichotomous outcomes, the number of people with each outcome and the number of people per group were extracted, or calculated if percentages were reported instead, to calculate risk ratios with 95% CIs. All effect size calculations were performed by the lead author (SC) and checked by one or more study authors (KA and RJ) to ensure accuracy.
For studies where the different interventions comprising the choice and no-choice groups were reported separately, the data from the relevant separate interventions were pooled to make a single overall choice, and a single overall no-choice group. This is so that the overall effect of choice provision could be assessed regardless of the specific interventions, and to maximise the number of studies contributing to the analysis, accommodating for various reporting practices. If a study reported an additional trial arm that did not include choice or corresponding no-choice conditions, such as a no treatment or usual care condition, this arm was excluded to ensure that the interventions in each group matched, and thus the only difference between groups was the provision of choice. Given the lack of standardised time-point for outcome assessment in choice-based interventions, if multiple time-points were reported, the time-point closest to the end of the intervention was extracted. If the same study included two different measures of the same outcome, only the measure most commonly used by other studies was analysed, to avoid double counting of participants. Similarly, for the analysis of overall behaviour and mood, if a single study reported two relevant outcomes, for instance both anxiety and depression, or both physical activity and weight loss, the study’s primary outcome was selected. If both outcomes were listed as primary, or it was unclear, only the outcome with the most participants reporting was selected. If both outcomes reported the same number of participants, the outcome most commonly reported by other studies in the meta-analysis was extracted. Finally, if two scales of the same outcome measure differed in the direction, for instance if one scale increased with severity whilst the others decreased, the data were recalculated using methods from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., Citation2021). Where outcomes were not sufficiently reported for meta-analyses, authors were contacted to supply this information.
Cluster randomised studies were eligible for inclusion and were analysed according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., Citation2021), following the method of effective sample sizes, where possible. If there was insufficient detail reported in studies to carry out such adjustments, unadjusted values had to be used. In total, two cluster randomised trials were included, one of which underwent adjustment as described (Kitchener et al., Citation2016). The other could not be adjusted due to insufficient reporting (Castle et al., Citation2019).
Additionally, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria was used to assess the overall quality of each outcome for the primary analyses, taking into account risk of bias assessments, inconsistency caused by heterogeneity, imprecision, and indirectness, as well as provide estimates of anticipated absolute effects (Guyatt et al., Citation2011; Guyatt et al., Citation2008).
Sensitivity analyses
In addition to the sensitivity analyses of change scores described above, two additional exploratory sensitivity analyses were carried out. Firstly, it was noted that whilst the majority of the included studies had a physical or mental health focus, there were nine included studies that did not include a health-related population, intervention or context. It is possible that this difference in focus may impact the reported outcomes, therefore sensitivity analyses were also conducted to assess the impact of these studies on the overall results. Secondly, it was noted that a minority of studies included drug-related treatments, as opposed to behavioural or psychological treatments. Therefore, a second set of sensitivity analyses were conducted to assess the impact of removing studies using drug-related treatments. Sensitivity analyses can be found in Supplementary Appendix F–H.
Exploratory subgroup analyses
Whilst the main focus of this review is on the effect of the provision of choice in interventions, which would not be expected to vary depending on study characteristics such as the specific intervention or population, there is considerable variability in the types of studies regarding these features that warrant further investigation. To explore this, several post-hoc exploratory subgroup analyses were conducted, with the aim of aiding interpretation of the data. Firstly, data were sub-grouped by the specific behavioural change and mood outcomes. These are included in the main meta-analyses forest plots alongside the corresponding pooled aggregate outcomes; however the in-text emphasis remains on the aggregate outcomes. Additional exploratory subgroup analyses were carried out to investigate the effects of the different types of choice interventions, which have been coded into categories. These can be found in Supplementary Appendix I.
All raw data including sensitivity analyses and subgroup analyses, as well as the study protocol and completed data extraction tables for all included studies are available here: https://osf.io/b27jd/.
Results
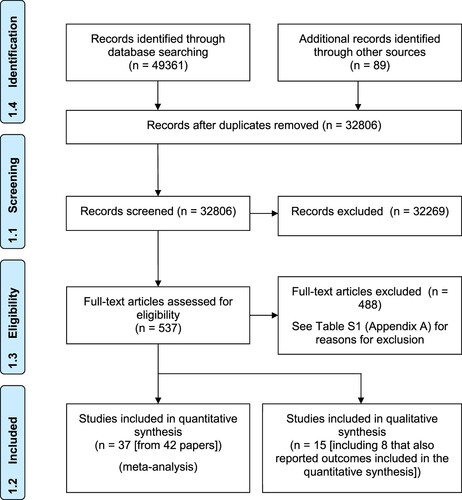
shows the PRISMA flow chart. The search retrieved a total of 49,361 results, and an additional 89 records were identified by screening reference lists of identified papers including literature reviews and systematic reviews, and through backwards citation searching. After removing duplicates, there were 32,806 references, of which 32,269 were excluded, and 537 underwent a full text screening. Of these, 488 were excluded. Overall, 44 studies were included from 49 papers. Thirty reported outcomes relating to retention, 17 reported outcomes relating to behaviour change, and 21 reported outcomes related to mood. Of the 44 included studies, 37 provided sufficient information for inclusion in the meta-analyses. Additionally, eight studies in the meta-analysis also reported other outcomes that could not be meta-analysed. Details of these 15 studies and outcomes can be found in Supplementary Appendix C.
Study characteristics
Details of all included studies can be found in . There was a total of 46,729 participants across the 44 trials, of which 14,174 were randomised to choice-based interventions and 32,275 were randomised to no-choice interventions. Three studies (n = 280) did not report the number of participants randomly allocated to each study arm. The median sample size of the studies was 168 participants. There were 10 studies exclusively including participants with a physical health condition such as diabetes, cancer, and heart disease, and five studies including participants with specific mental health conditions including depression and anxiety. There were two studies that specifically studied populations with drug, alcohol or smoking problems, and two studying an overweight population. Eleven studies involved university students, three studies specifically focused on older adults, and another four studies included participants with a mean age of ≥65 years. Nine studies included women only, two studies included men only. Twenty-five studies were conducted in the USA, four in the UK, three in Canada, two each in Germany, Australia and Brazil, and one each in New Zealand, Italy, Belgium, the Netherlands, Israel, and Sweden.
Table 1. Details of included studies.
Intervention characteristics
Interventions varied significantly in terms of their content, duration, and the way in which the choice intervention was operationalised. Details of the interventions can be found in . The most common types of intervention included those offering a choice between programmes of the same class targeting specific behaviours or medical conditions (e.g., a group-based or individual heart disease management programme), those offering a choice between a different class of treatments (e.g., a psychotherapy or drug therapy), and those offering the choice of having something (e.g., a recording of a doctor’s consultation) or not. Other intervention types included those using a combination of choice types and choices between different incentives. Comparison groups were no-choice interventions. One study included a perceived no-choice, where participants were led to believe that they were randomly allocated to one of two interventions, when in fact they were allocated according to preference.
Design
There were three categories of study design. Firstly, standard RCT (n = 22 trials; resulting in a 2:1 participant allocation), secondly a two-step RCT (n = 10 trials) where participants were randomised to either a choice or no-choice condition, and those in the no-choice condition were further randomised to one of the various no-choice conditions (resulting in a 1:1 allocation). Lastly, a matched design, where participants were randomised to a choice or no-choice condition, and then participants in the no-choice group were yoked to a participant in the choice group, or participants were matched and then randomised (n = 12 trials).
Effects of the interventions
Retention-related outcomes
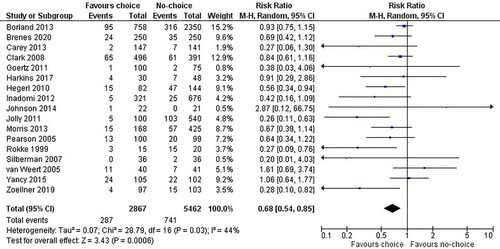
The most commonly reported retention-related outcome was drop-out. Of the 17 studies reporting this outcome, 14 favoured choice and 3 favoured no-choice (). Overall, the weighted point estimate significantly favoured choice with an effect size of RR = 0.68. The confidence interval ranged from 0.54 to 0.85, indicating that the true effect lies between a 46% to an 15% reduction in drop-out in the choice group. There were non-significant levels of heterogeneity. The quality of this evidence, according to the GRADE criteria, was low. Further details, and details of the anticipated absolute effects can be found in .
Table 2. GRADE evidence summary: Retention, behaviour change and mood.
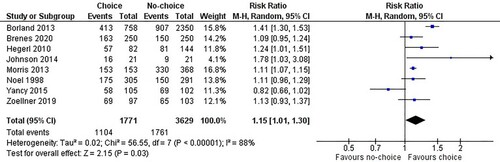
Eight studies reported adherence to the intervention at the end of the intervention (). Seven of these favoured choice interventions, and one favoured no-choice. The overall weighted point estimate significantly favoured choice with an effect size of RR = 1.15. The confidence interval ranged from 1.01 to 1.30, encompassing a true effect of between 1% and 30% increased adherence for participants in the choice group. Heterogeneity levels were very high, which was reflected in the very low GRADE quality rating ().
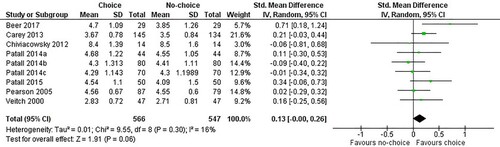
Nine studies also reported the outcome satisfaction, which was measured in terms of enjoyment or satisfaction (). Of these nine, six favoured choice, with the overall point estimate also favouring choice with a SMD of 0.13. The confidence interval ranged from 0.00 to 0.26, encompassing no differences between groups to a small positive effect. Heterogeneity levels were very low and non-significant, and the overall GRADE quality of the evidence was moderate, due to risk of bias ().
Figure 4. Satisfaction.
Notes: Beer et al., Citation2017: The intrinsic motivation inventory – enjoyment subscale; Carey et al., Citation2013: client satisfaction based on a 5-point likert scale; Chiviacowsky et al., Citation2012: single item regarding enjoyment; Patal et al., (Citation2014) Studies A–C and Patall & Leach, Citation2015: Interest-enjoyment subscale of the Intrinsic Motivation inventory; Pearson et al., Citation2005: patient satisfaction based on a 5-point likert scale; Veitch & Newsham, Citation2000: Environmental Satisfaction scale.
Behaviour change
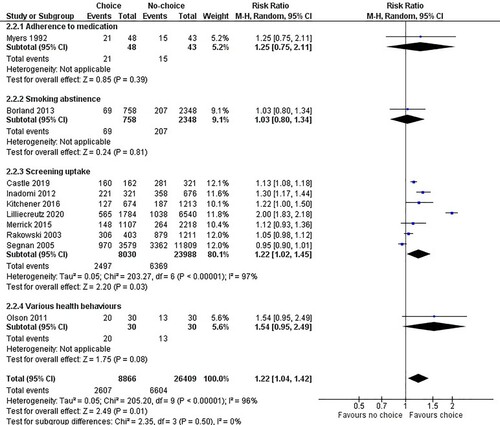
Due to the outcomes reported, separate meta-analyses were conducted for dichotomous (n = 10 trials) and continuous (n = 6 trials) behaviour change outcomes. In the dichotomous analysis, nine studies favoured choice (). Overall, the pooled point estimate significantly favoured choice, with a pooled effect size of RR = 1.22. The confidence interval ranged from 1.04 to 1.42, indicating that the true effect lies between a 4% to 42% increase in various healthy behaviours in the choice group. The quality of the evidence according to GRADE was very low, due to risk of bias, imprecision and heterogeneity ().
In the continuous behaviour change analysis (Supplementary Appendix D, Figure S1), three studies had point estimates favouring choice, and three favoured no-choice. The overall point estimate favoured choice but was close to the line of no effect (SMD 0.02), with the confidence intervals encompassing a small positive and very small negative effect (95% CI −0.16–0.20, p = .83). This evidence was rated as low quality due to risk of bias and significant heterogeneity (I2 = 57%; ).
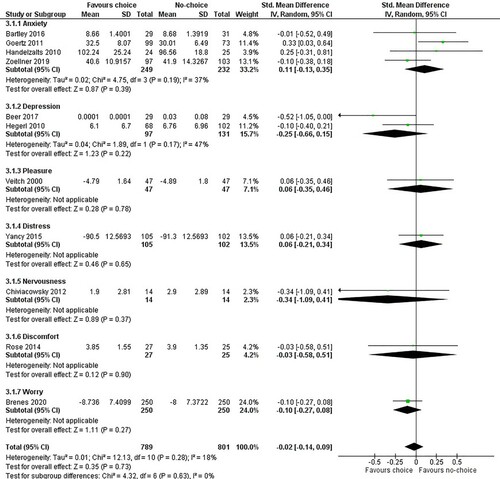
Mood
The analysis of the aggregate mood outcome included 11 studies, of which 7 favoured choice and 4 favoured no-choice (). Overall, the weighted point estimate favoured choice, but was very close to the line of no effect, with a SMD of −0.02. The confidence interval ranged from −0.14 to 0.09, indicating that the true effect lies between a very small positive and very small negative effect. The quality of the evidence for this outcome was low, due to risk of bias (). One of the included studies reported a mean and SD of 0 in the choice arm (Beer et al., Citation2017). A sensitivity analysis was conducted, removing this study to assess the effect of this study on the overall analysis (Supplementary Appendix E). Removal of this study resulted in a SMD of −0.01 (95% CI −0.11–0.09, p = .88).
Figure 6. Total mood.
Notes: Bartley et al. Citation2016: short-form State-Trait Anxiety Inventory; Beer et al., Citation2017: Profile of Mood States – Adolescent Inventory; Brenes et al., Citation2020: Penn State Worry Questionnaire-Abbreviated; Chiviacowsky et al., Citation2012: non-validated questionnaire; Goertz et al., Citation2011: State-Trait Anxiety Inventory – State; Handelzalts & Keinan, Citation2010: Sarason’s Test Anxiety; Hegerl et al., Citation2010: Hamilton Depression Rating Scale; Rose et al., Citation2014 A: aggregated likert scales for irritated, uncomfortable and unpleasant; Veitch & Newsham, Citation2000: non-validated questionnaire – pleasure subscale; Yancy et al., Citation2015: Impact of Weight on Quality of Life-Lite questionnaire – distress subscale; Zoellner et al., Citation2019: Spielberger State-Trait Anxiety Inventory.
Sensitivity analyses
Sensitivity analysis assessing the impact of non-health related studies on the overall results affected four outcomes: drop-out, adherence, satisfaction and mood. These sensitivity analyses demonstrated that there were minimal impacts on the point estimates and confidence intervals for drop-out, adherence, and mood (Supplementary Appendix F, Figures S3–S6). For the satisfaction outcome, the point estimate increased from 0.13 to 0.20, showing a slightly bigger positive effect of choice, and confidence intervals widened, suggesting a less precise estimate.
The impact of removing studies reporting change scores rather than final scores was also explored. This effected two outcomes: behaviour change and mood. The sensitivity analyses showed minimal impact on the point estimates and confidence intervals for both outcomes, with the behaviour change pooled estimate showing a slightly bigger effect favouring choice (SMD increasing from 0.02 to 0.07). The mood SMD also slightly increased from −0.02 to 0.02, indicating a slight shift from favouring choice to favouring no-choice, whilst remaining close to the line of no effect (Supplementary Appendix G, Figures S7–S8).
Studies employing a drug-related intervention contributed to four outcomes, including drop-out, adherence, behaviour change and mood. Sensitivity analyses removing these studies also showed minimal impacts on the point estimates for all outcomes, whilst confidence intervals became slightly wider, suggesting less precise estimates (Supplementary Appendix H, Figures S9–S12).
Exploratory subgroup analyses
Subgroup analyses by type of outcome are largely limited by small numbers of contributing studies. In terms of behaviour change, seven studies reported screening uptake and found that the point estimate significantly favoured choice (; RR 1.22, 95%CI 1.02–1.45, p = .03). Two studies each non-significantly favoured no-choice in terms of weight loss and steps walked, with point estimates close to the line of no effect (Supplementary Appendix D, Figure S1). Other behaviour change outcome domains were reported by single studies only, but show that for adherence to medication, smoking abstinence, calories consumed and various health behaviours there is a non-significant benefit of choice, whereas there was no benefit of choice seen for alcohol use (Figures 5 and S1). The most commonly reported mood outcome was anxiety (n = 4 trials), and subgroup analyses showed that for this outcome, there was a non-significant benefit of no-choice. Two studies reported depression, with the point estimate favouring choice but wide confidence intervals indicating a potential benefit of no-choice. The remainder of the outcomes are represented by single studies ().
Additional subgroup analyses explored the effects of intervention characteristics in terms of the different types of choice interventions (Supplementary Appendix I, Figures S13–S18). Six categories of choice types were defined: same class, different class, having versus not having, incentives, combination and other. Same class choice interventions, followed by different class choice interventions were the most frequently reported, both of which significantly favoured choice in terms of drop-out. Different class interventions also significantly favoured choice in terms of adherence. There were no other statistically significant differences between choice and no-choice groups for the remaining reported outcomes for same class or different class interventions. However, the pooled point estimates favoured choice for different class interventions measuring dichotomous behaviour change and mood, and for same class interventions measuring adherence, satisfaction and dichotomous behaviour change. Pooled point estimates for same class interventions non-significantly favoured no-choice for the continuous behaviour change and mood outcomes. Five interventions used a combination of choice types, which also non-significantly favoured choice in terms of satisfaction. Other outcomes were only reported by one of these studies. Two studies involved a choice of having versus not having something, and two studies involved a choice of incentives, with point estimates non-significantly favouring choice for all reported outcomes apart from continuous behaviour change. One study fell into the category ‘other’, and non-significantly favoured choice in terms of behaviour change.
Risk of bias
Risk of bias was assessed per outcome rather than for the overall study, and is reported for retention-related outcomes (drop-out, adherence and satisfaction), behaviour change (both continuous and dichotomous outcomes) and mood. This was to allow for aspects such as the amount of missing data, the method of measurement, and the definition of each specific outcome to be considered. The methodological quality of the studies varied; however, of the study outcomes included in the meta-analyses, the majority were given an overall rating of either some concerns (n = 39 outcomes) or high risk (n = 20 outcomes). Only two outcomes were judged as low risk in all domains. See for details of the risk of bias assessment per domain for all outcomes included in the meta-analyses. Supplementary Appendix J also includes the risk of bias details for the outcomes that could not be meta-analysed.
Table 3. Risk of bias ratings per outcome.
Discussion
This review is the first to assess retention-related, behaviour change and mood outcomes, whilst including only studies where the only difference between study arms was the provision of active, participant-driven choice, and whilst using strict criteria regarding the type of study design included. This allows for greater confidence that the findings of this review are due to the provision of choice alone rather than being influenced by other factors such as features of a specific intervention or the influence of the clinician. In doing so, this review aimed to firstly assess whether providing choice was acceptable to participants and impacted on participant retention, and secondly to assess whether choice-based interventions are more effective than no-choice interventions in terms of behaviour change and mood-related outcomes. The findings related to these aims are discussed below, as well as the limitations and implications of this review and areas for further research.
Effects of choice-based interventions
The review found that choice had a positive effect on drop-out and adherence to the intervention, with statistically significant effects favouring choice. Further, the analysis showed some potential positive effects on satisfaction, with the pooled point estimate favouring choice, however this was not statistically significant. When focusing on health-related studies only results were similar, with some minimal changes resulting in slightly less convincing effects for adherence and satisfaction, but still suggesting a benefit of choice. Overall, this supports previous review evidence which has demonstrated higher treatment satisfaction and completion rates in patients who either were involved in shared decision making, made the choice themselves or who received their preferred treatment compared to those who did not (Lindhiem et al., Citation2014).
The second objective of this review was to assess whether choice-based interventions were more effective than no-choice interventions in terms of commonly reported interventional outcomes such as behaviour change and mood. In doing so, this assesses whether giving participants choice translates to better outcomes. Results for the mood outcomes suggests that choice-based interventions may result in greater improvements in mood, although this evidence was not convincing. While point estimates tended to favour choice, confidence intervals were wide and were not statistically significant. It is unclear however, whether this is because the provision of choice makes no meaningful difference in terms of mood outcomes, or whether this is a result of sparse and divergent data making significant findings unlikely given considerable uncertainty. The behaviour change meta-analyses were more mixed. For instance, whilst the dichotomous behaviour change analysis significantly favoured choice, the overall behaviour change for continuous data showed minimal differences between the two intervention types. This suggests that whilst choice is beneficial in terms of participant retention and adherence, the effects of choice on behaviour change and mood were more limited.
It is interesting to note that whilst choice-based interventions improved participant retention and resulted in more adherent participants compared to the no-choice groups, this did not always translate to better outcomes, particularly in terms of behaviour change. Of the 16 meta-analysed studies reporting a behaviour change outcome, six also reported drop-out. Of these, five reported less drop-out in the choice-based group. However, of these five only three showed that the intervention resulted in better behaviour change outcomes in the choice group versus the control arm(s). Further, of the three studies favouring choice, for two studies the point estimates were very close to the line of no effect. This suggests, contrary to what might be expected, that better participant retention does not necessarily lead to better behaviour change outcomes. In fact, other research has similarly found that participant attrition may not impact study outcomes, including palliative treatment outcomes (Strömgren et al., Citation2005) and behaviour change outcomes such as the number of alcoholic drinks consumed (Kypri et al., Citation2020).
Adherence, on the other hand, has been associated with better outcomes in a number of behaviour change studies, showing that increased adherence is related to increased weight loss (Kaipainen et al., Citation2012; Murawski et al., Citation2009; Shapiro et al., Citation2012) and physical activity (Heesch et al., Citation2003), as well as outcomes such as greater reductions in disability and pain (Friedrich et al., Citation1998), whereas non-adherence is related to poorer outcomes such as decreases in health-related quality of life (Austin et al., Citation2012). When comparing behaviour change outcomes with adherence to intervention outcomes in this review however, conclusions are limited by the small number of contributing studies. Only two studies reported both adherence and behaviour change. Of these, one study showed that those in the choice arm were more adherent to the intervention, and also favoured choice in terms of the behaviour change outcome, although the point estimate was close to the line of no effect. The other study showed that those in the choice group were less adherent to the intervention, with poorer behaviour change outcomes compared with the no-choice group. The limited number of studies do not allow for firm conclusions at this time. Further studies of choice compared to no-choice interventions including both adherence related outcomes and behaviour change outcomes are needed to determine whether choice may be a mechanism through which adherence leads to greater behaviour change.
Exploratory analyses
Post-hoc analyses explored whether the effect of choice varied depending on either the specific behaviour change or mood outcome, or by the characteristics of the choice intervention in terms of the type of choice. In terms of behaviour change, these analyses suggest that providing choice significantly improves screening uptake, whilst other behaviour outcomes are limited by small numbers of studies and/or show no significant differences between groups. Mood analyses showed no significant differences between choice and no-choice groups for all outcome types, however, are similarly limited by small numbers of studies. All analyses had significant heterogeneity not explained by these subgroups, suggesting that differences between studies in behaviour change and mood outcomes are not explained by the specific type of outcome.
As with the type of outcome, exploratory analyses of the type of choice intervention used suggested that the different types of choice are not significantly different from each other in terms of their effects on the included outcomes. For instance, for outcomes with significant heterogeneity, such as adherence and behaviour change, this was not accounted for by these subgroup analyses. Therefore, the results from this review suggests that whilst choice interventions are more effective than no-choice interventions for some outcomes, the way in which the choice is given, in terms of type of choice, does not matter.
Limitations
Several difficulties were encountered when carrying out this review and meta-analyses. The studies that were included were very heterogeneous in terms of the specific intervention, population, outcomes used, and time-points reported. Traditionally, such diverse studies would not be meta-analysed together, however as one of the aims of this review was to explore the effect of choice on the selected outcomes, regardless of the specific intervention and population, to see whether there was an overall effect of choice, this method was judged to be appropriate. In order to minimise the effects of heterogeneous studies on the analyses, the inclusion criteria were kept strict, particularly with respect to the choice intervention. Whilst the goal of this was to ensure studies were as comparable as possible, it does limit this review’s ability to consider only the specific type of study design that was included, whilst a number of alternative designs have been and are being used, such as preference-based studies, or those where the interventions available to participants differ depending on group assignment.
Further, all but two of the included outcomes were judged as having some concerns regarding risk of bias, or high risk of bias, therefore reducing confidence and adding a degree of uncertainty to the results of the analyses. One of the main challenges for this type of study as regards the risk of bias is the fact that participant blinding is not possible, coupled with the fact that many outcomes are self-reported by participants, leading to potential bias due to expectations surrounding the provision of choice. Participants may be more likely to rate an intervention more favourably if they have had an active role in determining the specific content of their intervention, compared to being assigned an intervention. This may be because having an active role in their intervention content may not only increase autonomy, but also lead to a sense of responsibility and accountability, increasing the likelihood of positive appraisals. Thus, it is possible that by their very nature, choice-based interventions introduce bias in this way; or indeed that may be the ‘active ingredient’ that enables choice to enhance or influence such outcomes.
There were also methodological limitations, including that this review was not pre-registered. However, the protocol and raw data have been made available at the OSF link. Further, we were unable to have an independent second screener at the title-abstract and full text screening stage. Due to the size of the search this was not feasible, however a second screener was involved in discussions where there was uncertainty regarding a particular paper, which increased the certainty that all relevant papers were included. The size of the search also meant that use of a search filter for outcomes was necessary. Despite the use of filters, the search remained very large and so we are confident that the majority of eligible studies were identified. However, we acknowledge that the use of such filters may increase the risk of missing potentially eligible studies.
Lastly, whilst this review did briefly consider the effects of different types of choice interventions, other features of choice, such as the number of choice opportunities and the number of choice options per opportunity, were not considered. An in-depth exploration of these features was beyond the scope of this review, but they could be valuable areas of enquiry in the future.
Implications
This review accomplishes several things. Firstly, it addresses a gap in the current literature, by taking an often-ill-defined area with multiple relevant terms, and synthesising it, bringing together the existing evidence for this type of intervention, in terms of retention-related, mood, and behaviour change outcomes. This now allows researchers seeking to conduct research in this area to understand what has and has not been done. As such, this enables an informed choice regarding intervention design, and identification of the designs used in their own field, to enable more comparable studies to be carried out and allow for greater confidence in future reviews.
Secondly, this review confirms and strengthens previous review findings that choice may lead to improved retention-related outcomes. Our findings suggest that researchers may want to consider the inclusion of a choice-based intervention arm, particularly if there are concerns regarding participant retention, adherence or satisfaction. According to an audit of 151 RCTs, only 56% of studies achieved their target sample size, with a median retention rate of 89% (Walters et al., Citation2017). Failure to recruit or retain participants results in uncertain findings and squandered research funds, as well as both researcher and participant time. Similarly, poor adherence can result in an inability to fully evaluate intervention efficacy, further contributing to uncertainty in findings. The consequences of greater participant satisfaction are also important, with implications for relationships between the research and public communities, as well as potentially impacting outcomes in a number of research contexts, including both behavioural (Fodor et al., Citation2020) and clinical (Peyrot & Rubin, Citation2009). Thus, the provision of choice may not only improve these outcomes, but may in turn have several important implications for both intervention efficacy, and the confidence that can be placed in the conclusions drawn.
Finally, this review has also identified areas where evidence is lacking, and further research is required. For instance, the heterogeneity between different study designs has also resulted in a very small number of studies specifically investigating comparable populations and specific outcomes, making comparisons difficult and based on a small number of studies, indicating a general need for more research in this area to build up the evidence base. Further, this review has highlighted the lack of high-quality studies with sufficiently powered sample sizes. Thus, future work should look to address this by carrying out appropriate power calculations, and minimising potential bias where possible by adhering to practices such as publication of study protocols and clear and transparent reporting in study papers. Further, there was heterogeneity in the time-point for outcome assessment across the studies, resulting in time-points ranging from immediately post-intervention, to 18 months, with an average of 12 weeks from the end of the intervention. Thus, the results of this review speak to the relatively short terms effects of choice, and future work could expand on this by investigating the long-term effects of choice-based interventions.
Conclusions
This review demonstrated that the choice-based interventions currently being carried out by researchers vary greatly in terms of participants, settings, and several factors relating to the provision of choice itself. However, despite this variation, there is good evidence that choice-based interventions improve retention-related outcomes. They lead to a reduction in participant drop-out, increased adherence, and may be liked by participants more than no-choice interventions. Whilst there remains some uncertainty in regard to whether choice-based interventions are more effective than no-choice interventions in terms of both behaviour change and mood outcomes, there are reasons to believe that the provision of choice may be beneficial in these contexts. However, more evidence is needed.
Authors contributions
SC, KA and KV designed the review. SC, KA and RJ contributed to the systematic searches and data extraction processes. SC drafted the first draft of the manuscript. All authors contributed to the final version of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All available data including the study protocol, completed data extraction tables for all included studies, and raw data including sensitivity analyses and subgroup analyses are available here: https://osf.io/b27jd/.
Additional information
Funding
References
- Ajzen, I. (1985). From intentions to actions: A theory of planned behavior. In Action control (pp. 11–39). Springer, Berlin, Heidelberg.
- Austin, S., Qu, H., & Shewchuk, R. M. (2012). Association between adherence to physical activity guidelines and health-related quality of life among individuals with physician-diagnosed arthritis. Quality of Life Research, 21(8), 1347–1357. https://doi.org/https://doi.org/10.1007/s11136-011-0046-x
- Ayre, J., Cvejic, E., Bonner, C., Turner, R. M., Walter, S. D., & McCaffery, K. J. (2020). Effects of health literacy, screening, and participant choice on action plans for reducing unhealthy snacking in Australia: A randomised controlled trial. PLoS Medicine, 17(11), e1003409. https://doi.org/https://doi.org/10.1371/journal.pmed.1003409
- Bartley, H., Faasse, K., Horne, R., & Petrie, K. J. (2016). You can't always get what you want: The influence of choice on nocebo and placebo responding. Annals of Behavioral Medicine, 50(3), 445–451. https://doi.org/https://doi.org/10.1007/s12160-016-9772-1
- Baumeister, R. F., Bratslavsky, E., Muraven, M., & Tice, D. M. (1998). Ego depletion: Is the active self a limited resource?. Journal оf Personality and Social Psychology, 74(5), 1252–1265. https://doi.org/https://doi.org/10.1037/0022-3514.74.5.1252
- Beer, N. J., Dimmock, J. A., Jackson, B., & Guelfi, K. J. (2017). Providing choice in exercise influences food intake at the subsequent meal. Medicine & Science in Sports & Exercise, 49(10), 2110–2118. https://doi.org/https://doi.org/10.1249/MSS.0000000000001330
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. https://doi.org/https://doi.org/10.1002/jrsm.12
- Borland, R., Balmford, J., & Benda, P. (2013). Population-level effects of automated smoking cessation help programs: A randomized controlled trial. Addiction, 108(3), 618–628. https://doi.org/https://doi.org/10.1111/j.1360-0443.2012.04091.x
- Bowling, A., & Rowe, G. (2005). “You decide doctor”. What do patient preference arms in clinical trials really mean? Journal of Epidemiology and Community Health, 59(11), 914–915. https://doi.org/https://doi.org/10.1136/jech.2005.035261
- Bradley, C. (1993). Designing medical and educational intervention studies: A review of some alternatives to conventional randomized controlled trials. Diabetes Care, 16(2), 509–518. https://doi.org/https://doi.org/10.2337/diacare.16.2.509
- Bradley, C. (1997). Psychological issues in clinical trial design. The Irish Journal of Psychology, 18(1), 67–87. https://doi.org/https://doi.org/10.1080/03033910.1997.10558130
- Brenes, G. A., Divers, J., Miller, M. E., Anderson, A., Hargis, G., & Danhauer, S. C. (2020). Comparison of cognitive-behavioral therapy and yoga for the treatment of late-life worry: A randomized preference trial. Depression and Anxiety, 37(12), 1194–1207. https://doi.org/https://doi.org/10.1002/da.23107
- Brewin, C. R., & Bradley, C. (1989). Patient preferences and randomised clinical trials. BMJ: British Medical Journal, 299(6694), 313. https://doi.org/https://doi.org/10.1136/bmj.299.6694.313
- Brown, J. A., Fowler, S. L., Rasinski, H. M., Rose, J. P., & Geers, A. L. (2013). Choice as a moderator of placebo expectation effects: Additional support from two experiments. Basic and Applied Social Psychology, 35(5), 436–444. https://doi.org/https://doi.org/10.1080/01973533.2013.803968
- Bruyneel, S., Dewitte, S., Vohs, K. D., & Warlop, L. (2006). Repeated choosing increases susceptibility to affective product features. International Journal of Research in Marketing, 23(2), 215–225. https://doi.org/https://doi.org/10.1016/j.ijresmar.2005.12.002
- Carey, K. B., DeMartini, K. S., Prince, M. A., Luteran, C., & Carey, M. P. (2013). Effects of choice on intervention outcomes for college students sanctioned for campus alcohol policy violations. Psychology of Addictive Behaviors, 27(3), 596–603. https://doi.org/https://doi.org/10.1037/a0030333
- Castle, P. E., Silva, V. R., Consolaro, M. E., Kienen, N., Bittencourt, L., Peloso, S. M., Partridge, E. E., Pierz, A., Dartibale, C. B., Uchimura, N. S., & Scarinci, I. C. (2019). Participation in cervical screening by self-collection, Pap, or a choice of either in Brazil. Cancer Prevention Research, 12(3), 159–170. https://doi.org/https://doi.org/10.1158/1940-6207.
- Chiviacowsky, S., Wulf, G., Lewthwaite, R., & Campos, T. (2012). Motor learning benefits of self-controlled practice in persons with Parkinson’s disease. Gait & Posture, 35(4), 601–605. https://doi.org/https://doi.org/10.1016/j.gaitpost.2011.12.003
- Clark, N. M., Janz, N. K., Dodge, J. A., Mosca, L., Lin, X., Long, Q., … Liang, J. (2008). The effect of patient choice of intervention on health outcomes. Contemporary Clinical Trials, 29(5), 679–686. https://doi.org/https://doi.org/10.1016/j.cct.2008.04.002
- Cordova, D. I., & Lepper, M. R. (1996). Intrinsic motivation and the process of learning: Beneficial effects of contextualization, personalization, and choice. Journal of Educational Psychology, 88(4), 715. https://doi.org/https://doi.org/10.1037/0022-0663.88.4.715
- Dan-Cohen, M. (1992). Conceptions of choice and conceptions of autonomy. Ethics, 102(2), 221–243. https://doi.org/https://doi.org/10.1086/293394
- Deci, E. L., Connell, J. P., & Ryan, R. M. (1989). Self-determination in a work organization. Journal of Applied Psychology, 74(4), 580. https://doi.org/https://doi.org/10.1037/0021-9010.74.4.580
- Deci, E. L., & Ryan, R. M. (1980). Self-determination theory: When mind mediates behavior. The Journal of Mind and Behavior, 1(1), 33–43.
- Deci, E. L., & Ryan, R. M.. (2012). Motivation, personality, and development within embedded social contexts: An overview of self-determination theory. In R. M. Ryan (Ed.), The Oxford Handbook of Human Motivation (pp. 85–107). Oxford: University Press.
- Feine, J. S., Awad, M. A., & Lund, J. P. (1998). The impact of patient preference on the design and interpretation of clinical trials. Community Dentistry and Oral Epidemiology, 26(1), 70–74. https://doi.org/https://doi.org/10.1111/j.1600-0528.1998.tb02086.x
- Flowerday, T., & Schraw, G. (2003). Effect of choice on cognitive and affective engagement. The Journal of Educational Research, 96(4), 207–215. https://doi.org/https://doi.org/10.1080/00220670309598810
- Flowerday, T., Schraw, G., & Stevens, J. (2004). The role of choice and interest in reader engagement. The Journal of Experimental Education, 72(2), 93–114. https://doi.org/https://doi.org/10.3200/JEXE.72.2.93-114
- Fodor, M. C., Grekin, E. R., Beatty, J. R., McGoron, L., & Ondersma, S. J. (2020). Participant Satisfaction with computer-delivered intervention components and its relation to alcohol outcomes. Substance Use & Misuse, 55(14), 2332–2340. https://doi.org/https://doi.org/10.1080/10826084.2020.1811343
- Friedrich, M., Gittler, G., Halberstadt, Y., Cermak, T., & Heiller, I. (1998). Combined exercise and motivation program: Effect on the compliance and level of disability of patients with chronic low back pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 79(5), 475–487. https://doi.org/https://doi.org/10.1016/S0003-9993(98)90059-4
- Goertz, W., Dominick, K., Heussen, N., & vom Dahl, J. (2011). Music in the cath lab: Who should select it? Clinical Research in Cardiology, 100(5), 395–402. https://doi.org/https://doi.org/10.1007/s00392-010-0256-1
- Gourville, J. T., & Soman, D. (2005). Overchoice and assortment type: When and why variety backfires. Marketing Science, 24(3), 382–395. https://doi.org/https://doi.org/10.1287/mksc.1040.0109
- Grob, A.. (2000). Perceived control and subjective well-being across nations and across the life span. In E. Diener & E. Suh (Eds.), Culture and Subjective Well-Being (pp. 319–339). Cambridge, MA: MIT Press.
- Guyatt, G., Oxman, A. D., Akl, E. A., Kunz, R., Vist, G., Brozek, J., … Debeer, H. (2011). GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology, 64(4), 383–394. https://doi.org/https://doi.org/10.1016/j.jclinepi.2010.04.026
- Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., & Schünemann, H. J. (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. Bmj, 336(7650), 924–926. https://doi.org/https://doi.org/10.1136/bmj.39489.470347.AD
- Hack, T. F., Pickles, T., Bultz, B. D., Ruether, J. D., & Degner, L. F. (2007). Impact of providing audiotapes of primary treatment consultations to men with prostate cancer: A multi-site, randomized, controlled trial. Psycho-Oncology, 16(6), 543–552. https://doi.org/https://doi.org/10.1002/pon.1094
- Hack, T. F., Pickles, T., Bultz, B. D., Ruether, J. D., Weir, L. M., Degner, L. F., & Mackey, J. R. (2003). Impact of providing audiotapes of primary adjuvant treatment consultations to women with breast cancer: A multisite, randomized, controlled trial. Journal of Clinical Oncology, 21(22), 4138–4144. https://doi.org/https://doi.org/10.1200/JCO.2003.12.155
- Handelzalts, J. E., & Keinan, G. (2010). The effect of choice between test anxiety treatment options on treatment outcomes. Psychotherapy Research, 20(1), 100–112. https://doi.org/https://doi.org/10.1080/10503300903121106
- Hariton, E., & Locascio, J. J. (2018). Randomised controlled trials—The gold standard for effectiveness research. BJOG: An International Journal of Obstetrics and Gynaecology, 125(13), 1716. https://doi.org/https://doi.org/10.1111/1471-0528.15199
- Harkins, K. A., Kullgren, J. T., Bellamy, S. L., Karlawish, J., & Glanz, K. (2017). A trial of financial and social incentives to increase older adults’ walking. American Journal of Preventive Medicine, 52(5), e123–e130. https://doi.org/https://doi.org/10.1016/j.amepre.2016.11.011
- Heesch, K., Mâsse, L., Dunn, A., Frankowski, R., & Mullen, P. D. (2003). Does adherence to a lifestyle physical activity intervention predict changes in physical activity? Journal of Behavioral Medicine, 26(4), 333–348. https://doi.org/https://doi.org/10.1023/A:1024205011001
- Hegerl, U., Hautzinger, M., Mergl, R., Kohnen, R., Schutze, M., Scheunemann, W., … Henkel, V. (2010). Effects of pharmacotherapy and psychotherapy in depressed primary-care patients: A randomized, controlled trial including a patients’ choice arm. International Journal of Neuropsychopharmacology, 13(1), 31–44. https://doi.org/https://doi.org/10.1017/S1461145709000224
- Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., & Welch, V.. (2021). Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
- Inadomi, J. M., Vijan, S., Janz, N. K., Fagerlin, A., Thomas, J. P., Lin, Y. V., … Hayward, R. A. (2012). Adherence to colorectal cancer screening: A randomized clinical trial of competing strategies. Archives of Internal Medicine, 172(7), 575–582. https://doi.org/https://doi.org/10.1001/archinternmed.2012.332
- Iyengar, S. S., & Lepper, M. R. (2000). When choice is demotivating: Can one desire too much of a good thing? Journal of Personality and Social Psychology, 79(6), 995. https://doi.org/https://doi.org/10.1037/0022-3514.79.6.995
- Janevic, M. R., Janz, N. K., Dodge, J. A., Lin, X., Pan, W., Sinco, B. R., & Clark, N. M. (2003). The role of choice in health education intervention trials: A review and case study. Social Science & Medicine, 56(7), 1581–1594. https://doi.org/https://doi.org/10.1016/S0277-9536(02)00158-2
- Johnson, L. D., Wehby, J. H., Symons, F. J., Moore, T. C., Maggin, D. M., & Sutherland, K. S. (2014). An analysis of preference relative to teacher implementation of intervention. The Journal of Special Education, 48(3), 214–224. https://doi.org/https://doi.org/10.1177/0022466913475872
- Jolly, K., Lewis, A., Beach, J., Denley, J., Adab, P., Deeks, J. J., … Aveyard, P. (2011). Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: Lighten up randomised controlled trial. BMJ, 343(nov03 2), d6500. https://doi.org/https://doi.org/10.1136/bmj.d6500
- Kaipainen, K., Payne, C. R., & Wansink, B. (2012). Mindless eating challenge: Retention, weight outcomes, and barriers for changes in a public web-based healthy eating and weight loss program. Journal of Medical Internet Research, 14(6), e168. https://doi.org/https://doi.org/10.2196/jmir.2218
- King, M., Nazareth, I., Lampe, F., Bower, P., Chandler, M., Morou, M., … Lai, R. (2005). Impact of participant and physician intervention preferences on randomized trials: A systematic review. Jama, 293(9), 1089–1099. https://doi.org/https://doi.org/10.1001/jama.293.9.1089
- Kitchener, H. C., Gittins, M., Rivero-Arias, O., Tsiachristas, A., Cruickshank, M., Gray, A., … Roberts, C. (2016). A cluster randomised trial of strategies to increase cervical screening uptake at first invitation (STRATEGIC). Health Technology Assessment (Winchester, England), 20(68), 1–138. https://doi.org/https://doi.org/10.3310/hta20680
- Krebs, P., Prochaska, J., & Rossi, J. (2010). A meta-analysis of computer-tailored interventions for health behavior change. Preventive Medicine, 51(3-4), 214–221. https://doi.org/https://doi.org/10.1016/j.ypmed.2010.06.004
- Kypri, K., Bowe, S. J., Karlsson, N., & McCambridge, J. (2020). Enrolment-latency in randomized behavior change trials: Individual participant data meta-analysis showed association with attrition but not effect-size. Journal of Clinical Epidemiology, 118, 55–59. https://doi.org/https://doi.org/10.1016/j.jclinepi.2019.09.019
- Le, Q. A., Doctor, J. N., Zoellner, L. A., & Feeny, N. C. (2014). Cost-effectiveness of prolonged exposure therapy versus pharmacotherapy and treatment choice in posttraumatic stress disorder (the optimizing PTSD treatment trial): A doubly randomized preference trial. The Journal of Clinical Psychiatry, 75(3), 222–230. https://doi.org/https://doi.org/10.4088/JCP.13m08719
- Liang, P. S., Wheat, C. L., Abhat, A., Brenner, A. T., Fagerlin, A., Hayward, R. A., … Inadomi, J. M. (2016). Adherence to competing strategies for colorectal cancer screening over 3 years. American Journal of Gastroenterology, 111(1), 105–114. https://doi.org/https://doi.org/10.1038/ajg.2015.367
- Lilliecreutz, C., Karlsson, H., & Spetz Holm, A.-C. (2020). Participation in interventions and recommended follow-up for non-attendees in cervical cancer screening-taking the women’s own preferred test method into account—A Swedish randomised controlled trial. Plos One, 15(7), e0235202. https://doi.org/https://doi.org/10.1371/journal.pone.0235202
- Lindhiem, O., Bennett, C. B., Trentacosta, C. J., & McLear, C. (2014). Client preferences affect treatment satisfaction, completion, and clinical outcome: A meta-analysis. Clinical Psychology Review, 34(6), 506–517. https://doi.org/https://doi.org/10.1016/j.cpr.2014.06.002
- Lustria, M. L. A., Noar, S. M., Cortese, J., Van Stee, S. K., Glueckauf, R. L., & Lee, J. (2013). A meta-analysis of web-delivered tailored health behavior change interventions: corrigendum. Journal of Health Communication, 18(11), 1397. https://doi.org/https://doi.org/10.1080/10810730.2013.852950
- McPherson, K., & Britton, A. (1999). The impact of patient treatment preferences on the interpretation of randomised controlled trials. European Journal of Cancer, 35(11), 1598–1602. https://doi.org/https://doi.org/10.1016/S0959-8049(99)00196-3
- McPherson, K., Britton, A. R., & Wennberg, J. E. (1997). Are randomized controlled trials controlled? Patient preferences and unblind trials. Journal of the Royal Society of Medicine, 90(12), 652–656. https://doi.org/https://doi.org/10.1177/014107689709001205
- McVay, M. A., Voils, C. I., Coffman, C. J., Geiselman, P. J., Kolotkin, R. L., Mayer, S. B., … Yancy Jr, W. S. (2014). Factors associated with choice of a low-fat or low-carbohydrate diet during a behavioral weight loss intervention. Appetite, 83, 117–124. https://doi.org/https://doi.org/10.1016/j.appet.2014.08.023
- McVay, M. A., Voils, C. I., Geiselman, P. J., Smith, V. A., Coffman, C. J., Mayer, S., & Yancy Jr, W. S. (2016). Food preferences and weight change during low-fat and low-carbohydrate diets. Appetite, 103, 336–343. https://doi.org/https://doi.org/10.1016/j.appet.2016.04.035
- Mergl, R., Henkel, V., Allgaier, A. K., Kramer, D., Hautzinger, M., Kohnen, R., … Hegerl, U. (2011). Are treatment preferences relevant in response to serotonergic antidepressants and cognitive-behavioral therapy in depressed primary care patients? Results from a randomized controlled trial including a patients’. choice arm. Psychotherapy & Psychosomatics, 80(1), 39–47. https://doi.org/https://doi.org/10.1159/000318772
- Merrick, E. L., Hodgkin, D., Horgan, C. M., Lorenz, L. S., Panas, L., Ritter, G. A., … Nefussy, R. A. (2015). Testing novel patient financial incentives to increase breast cancer screening. American Journal of Managed Care, 21(11), 771–779.
- Moller, A. C., Deci, E. L., & Ryan, R. M. (2006). Choice and ego-depletion: The moderating role of autonomy. Personality and Social Psychology Bulletin, 32(8), 1024–1036. https://doi.org/https://doi.org/10.1177/0146167206288008
- Morris, M., Edwards, P., Doyle, P., & Maconochie, N. (2013). Women in an infertility survey responded more by mail but preferred a choice: Randomized controlled trial. Journal of Clinical Epidemiology, 66(2), 226–235. https://doi.org/https://doi.org/10.1016/j.jclinepi.2012.10.003
- Murawski, M. E., Milsom, V. A., Ross, K. M., Rickel, K. A., DeBraganza, N., Gibbons, L. M., & Perri, M. G. (2009). Problem solving, treatment adherence, and weight-loss outcome among women participating in lifestyle treatment for obesity. Eating Behaviors, 10(3), 146–151. https://doi.org/https://doi.org/10.1016/j.eatbeh.2009.03.005
- Myers, E. D., & Branthwaite, A. (1992). Out-patient compliance with antidepressant medication. British Journal of Psychiatry, 160(1), 83–86. https://doi.org/https://doi.org/10.1192/bjp.160.1.83
- Noar, S. M., Benac, C. N., & Harris, M. S. (2007). Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin, 133(4), 673–693. https://doi.org/https://doi.org/10.1037/0033-2909.133.4.673
- Noël, P. H., Larme, A. C., Meyer, J., Marsh, G., Correa, A., & Pugh, J. A. (1998). Patient choice in diabetes education curriculum: Nutritional versus standard content for type 2 diabetes. Diabetes Care, 21(6), 896–901. https://doi.org/https://doi.org/10.2337/diacare.21.6.896
- Olson, R., Schmidt, S., Winkler, C., & Wipfli, B. (2011). The effects of target behavior choice and self-management skills training on compliance with behavioral self-monitoring. American Journal of Health Promotion, 25(5), 319–324. https://doi.org/https://doi.org/10.4278/ajhp.090421-QUAN-143
- Patall, E. A., Cooper, H., & Robinson, J. C. (2008). The effects of choice on intrinsic motivation and related outcomes: A meta-analysis of research findings. Psychological Bulletin, 134(2), 270–300. https://doi.org/https://doi.org/10.1037/0033-2909.134.2.270
- Patall, E. A., & Leach, J. K. (2015). The role of choice provision in academic dishonesty. Contemporary Educational Psychology, 42, 97–110. https://doi.org/https://doi.org/10.1016/j.cedpsych.2015.06.004
- Patall, E. A., Sylvester, B. J., & Han, C.-w. (2014). The role of competence in the effects of choice on motivation. Journal of Experimental Social Psychology, 50, 27–44. https://doi.org/https://doi.org/10.1016/j.jesp.2013.09.002
- Pearson, S., Maddern, G. J., & Hewett, P. (2005). Interacting effects of preoperative information and patient choice in adaptation to colonoscopy. Diseases of the Colon & Rectum, 48(11), 2047–2054. https://doi.org/https://doi.org/10.1007/s10350-005-0172-z
- Peyrot, M., & Rubin, R. R. (2009). How does treatment satisfaction work?: Modeling determinants of treatment satisfaction and preference. Diabetes Care, 32(8), 1411–1417. https://doi.org/https://doi.org/10.2337/dc08-2256
- Rakowski, W., Lipkus, I. M., Clark, M. A., Rimer, B. K., Ehrich, B., Lyna, P. R., & Kornguth, P. J. (2003). Reminder letter, tailored stepped-care, and self-choice comparison for repeat mammography. American Journal of Preventive Medicine, 25(4), 308–314. https://doi.org/https://doi.org/10.1016/S0749-3797(03)00215-0
- Raposo, S., Hogan, C. L., Barnes, J. T., Chemudupati, T., & Carstensen, L. L. (2020). Leveraging goals to incentivize healthful behaviors across adulthood. Psychology and Aging, 36(1), 57–68. https://doi.org/https://doi.org/10.1037/pag0000428
- Reis, H. T., Sheldon, K. M., Gable, S. L., Roscoe, J., & Ryan, R. M. (2000). Daily well-being: The role of autonomy, competence, and relatedness. Personality and Social Psychology Bulletin, 26(4), 419–435. https://doi.org/https://doi.org/10.1177/0146167200266002
- Rokke, P. D., Tomhave, J. A., & Jocic, Z. (1999). The role of client choice and target selection in self-management therapy for depression in older adults. Psychology and Aging, 14(1), 155–169. https://doi.org/https://doi.org/10.1037/0882-7974.14.1.155
- Rose, J. P., Geers, A. L., Fowler, S. L., & Rasinski, H. M. (2014). Choice-making, expectations, and treatment positivity: How and when choosing shapes aversive experiences. Journal of Behavioral Decision Making, 27(1), 1–10. https://doi.org/https://doi.org/10.1002/bdm.1775
- Rose, J. P., Geers, A. L., Rasinski, H. M., & Fowler, S. L. (2012). Choice and placebo expectation effects in the context of pain analgesia [Erratum appears in J Behav Med. 2012 Dec;35(6):674]. Journal of Behavioral Medicine, 35(4), 462–470. https://doi.org/https://doi.org/10.1007/s10865-011-9374-0
- Rotter, J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General and Applied, 80(1), 1. https://doi.org/https://doi.org/10.1037/h0092976
- Rotton, J., & Shats, M. (1996). Effects of state humor, expectancies, and choice on postsurgical mood and self-medication: A field experiment. Journal of Applied Social Psychology, 26(20), 1775–1794. https://doi.org/https://doi.org/10.1111/j.1559-1816.1996.tb00097.x
- Rücker, G. (1989). A two-stage trial design for testing treatment, self-selection and treatment preference effects. Statistics in Medicine, 8(4), 477–485. https://doi.org/https://doi.org/10.1002/sim.4780080411
- Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68. https://doi.org/https://doi.org/10.1037/0003-066X.55.1.68
- Schwartz, B. (2004). The paradox of choice: Why more is less.
- Scott, R. G., Edwards, J. T., Fritschi, L., Foster, N. M., Mendelson, R. M., & Forbes, G. M. (2004). Community-based screening by colonoscopy or computed tomographic colonography in asymptomatic average-risk subjects. American Journal of Gastroenterology, 99(6), 1145–1151. https://doi.org/https://doi.org/10.1111/j.1572-0241.2004.30253.x
- Segnan, N., Senore, C., Andreoni, B., Arrigoni, A., Bisanti, L., Cardelli, A., … Group-Italy, S. W. (2005). Randomized trial of different screening strategies for colorectal cancer: Patient response and detection rates. Journal of the National Cancer Institute, 97(5), 347–357. https://doi.org/https://doi.org/10.1093/jnci/dji050
- Seligman, M. E.. (1975). Helplessness: On Depression, Development and Death. San Francisco: W. H. Freeman.
- Senore, C., Armaroli, P., Silvani, M., Andreoni, B., Bisanti, L., Marai, L., … Segnan, N. (2010). Comparing different strategies for colorectal cancer screening in Italy: Predictors of patients’ participation. American Journal of Gastroenterology, 105(1), 188–198. https://doi.org/https://doi.org/10.1038/ajg.2009.583
- Shapiro, J. R., Koro, T., Doran, N., Thompson, S., Sallis, J. F., Calfas, K., & Patrick, K. (2012). Text4Diet: A randomized controlled study using text messaging for weight loss behaviors. Preventive Medicine, 55(5), 412–417. https://doi.org/https://doi.org/10.1016/j.ypmed.2012.08.011
- Sheldon, K. M., Ryan, R., & Reis, H. T. (1996). What makes for a good day? Competence and autonomy in the day and in the person. Personality and Social Psychology Bulletin, 22(12), 1270–1279. https://doi.org/https://doi.org/10.1177/01461672962212007
- Silberman, J. (2007). Positive intervention self-selection: Developing models of what works for whom. International Coaching Psychology Review, 2(1), 70–77.
- Staub, E. (2013). Development and maintenance of prosocial behavior: International perspectives on positive morality (Vol. 31). Springer Science & Business Media.
- Sterne, J. A., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., … Eldridge, S. M. (2019). Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. https://doi.org/https://doi.org/10.1136/bmj.l4898
- Strömgren, A. S., Sjogren, P., Goldschmidt, D., Petersen, M. A., Pedersen, L., Hoermann, L., & Groenvold, M. (2005). A longitudinal study of palliative care: Patient-evaluated outcome and impact of attrition. Cancer: Interdisciplinary International Journal of the American Cancer Society, 103(8), 1747–1755. https://doi.org/https://doi.org/10.1002/cncr.20958
- Suhonen, R., Välimäki, M., & Leino-Kilpi, H. (2008). A review of outcomes of individualised nursing interventions on adult patients. Journal of Clinical Nursing, 17(7), 843–860. https://doi.org/https://doi.org/10.1111/j.1365-2702.2007.01979.x
- Swann Jr, W. B., & Pittman, T. S. (1977). Initiating play activity of children: The moderating influence of verbal cues on intrinsic motivation. Child Development, 48(3), 1128–1132. https://doi.org/https://doi.org/10.2307/1128374.
- Terry, D. J., & O'Leary, J. E. (1995). The theory of planned behaviour: The effects of perceived behavioural control and self-efficacy. British Journal of Social Psychology, 34(2), 199–220. https://doi.org/https://doi.org/10.1111/j.2044-8309.1995.tb01058.x
- Torgerson, D. J., Klaber-Moffett, J., & Russell, I. T. (1996). Patient preferences in randomised trials: Threat or opportunity? Journal of Health Services & Research Policy, 1(4), 194–197. https://doi.org/https://doi.org/10.1177/135581969600100403
- van Weert, E., Hoekstra-Weebers, J., Grol, B., Otter, R., Arendzen, H. J., Postema, K., … van der Schans, C. (2005). A multidimensional cancer rehabilitation program for cancer survivors: Effectiveness on health-related quality of life. Journal of Psychosomatic Research, 58(6), 485–496. https://doi.org/https://doi.org/10.1016/j.jpsychores.2005.02.008
- Veitch, J. A., & Newsham, G. R. (1998). Experimental investigations of lighting quality, preferences and control effects on task performance and energy efficiency: Experiment 2 primary analyses. Institute for Research in Construction.
- Veitch, J. A., & Newsham, G. R. (2000). Exercised control, lighting choices, and energy use: An office simulation experiment. Journal of Environmental Psychology, 20(3), 219–237. https://doi.org/https://doi.org/10.1006/jevp.1999.0169
- Vohs, K., Baumeister, R., Twenge, J., Schmeichel, B., Tice, D., & Crocker, J. (2004). Decision fatigue: Choices influence self-regulatory resources. Unpublished manuscript.
- Wallston, K. A., Smith, R. P., King, J. E., Smith, M., Rye, P., & Burish, T. (1991). Desire for control and choice of antiemetic treatment for cancer chemotherapy. Western Journal of Nursing Research, 13(1), 12–29. https://doi.org/https://doi.org/10.1177/019394599101300102
- Walters, S. J., dos Anjos Henriques-Cadby, I. B., Bortolami, O., Flight, L., Hind, D., Jacques, R. M., … Surtees, M. (2017). Recruitment and retention of participants in randomised controlled trials: A review of trials funded and published by the United Kingdom health technology assessment programme. BMJ Open, 7(3), e015276. https://doi.org/https://doi.org/10.1136/bmjopen-2016-015276
- Wennberg, J. E., Barry, M. J., Fowler, F. J., & Mulley, A. (1993). Outcomes research, PORTs, and health care reform. Annals of the New York Academy of Sciences, 703(1), 52–62. https://doi.org/https://doi.org/10.1111/j.1749-6632.1993.tb26335.x
- Williams, G. C., Freedman, Z. R., & Deci, E. L. (1998). Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21(10), 1644–1651. https://doi.org/https://doi.org/10.2337/diacare.21.10.1644
- Yancy, W. S., Mayer, S. B., Coffman, C. J., Smith, V. A., Kolotkin, R. L., Geiselman, P. J., … Voils, C. I. (2015). Effect of allowing choice of diet on weight loss: A randomized trial. [Summary for patients in Ann Intern Med. 2015 Jun 16;162(12):I-22; PMID: 26075773]. Annals of Internal Medicine, 162(12), 805–814. https://doi.org/https://doi.org/10.7326/M14-2358
- Zoellner, L. A., Roy-Byrne, P. P., Mavissakalian, M., & Feeny, N. C. (2019). Doubly randomized preference trial of prolonged exposure versus sertraline for treatment of PTSD. American Journal of Psychiatry, 176(4), 287–296. https://doi.org/https://doi.org/10.1176/appi.ajp.2018.17090995